Abstract
A precise diagnosis of diastolic dysfunction is often difficult and requires invasive techniques to determine left ventricular volume, relaxation, and compliance properties. At this current point of time there is no single non-invasive index available to adequately reflect diastolic function, perhaps because of the numerous factors that can alter diastolic function. In most clinical settings, diastolic function is estimated using Doppler echocardiography. Cardiac magnetic resonance imaging (CMRI) is yet another emerging modality for diastolic function analysis. Here we present a comprehensive review of the various parameters used to assess diastolic function as part of diagnosis of clinical syndrome “Heart failure with preserved ejection fraction (HFPEF)”.
Keywords: Diastolic dysfunction, HFPEF, HFNEF, echocardiography
Introduction
A precise diagnosis of diastolic dysfunction is often difficult and requires invasive techniques to determine left ventricular (LV) volume, relaxation, and compliance properties. At this current point of time there is no single non-invasive index available to adequately reflect diastolic function, perhaps because of the numerous factors that can alter diastolic function. The criterion standard for demonstrating LV diastolic dysfunction is cardiac catheterization to obtain pressure-volume curves to measure the rate of pressure decay during isovolumic relaxation [1]. However, this measurement is imperfect because of the additional effect of trans-myocardial pressure on the left ventricle; routine invasive cardiac catheterization is also not feasible. In most clinical settings, diastolic function is estimated using Doppler echocardiography. Cardiac magnetic resonance imaging(CMRI) is yet another emerging modality for diastolic function analysis. Several studies have compared the Doppler echocardiography and CMRI, and suggest favourable inter-modality agreement. Here we present a comprehensive review of the various parameters used to assess diastolic function as part of diagnosis of clinical syndrome “Heart failure with preserved ejection fraction (HFPEF)”.
Heart failure with preserved ejection fraction
Three obligatory conditions need to be satisfied to diagnose HFPEF:
1. Signs and symptoms of heart failure
Clinical signs and symptoms are similar to systolic heart failure. Interestingly, symptoms of dyspnoea correlate better with HFPEF than with reduced ejection fraction (HFREF), and people with reduced EF may even have better exercise capacity than patients with normal EF and diastolic dysfunction [2-4]. Pulmonary congestion, peripheral oedema, and abdominal bloating may also occur as the result of hepatic congestion[5-8].
2. Normal or mildly abnormal systolic function
Although preserved LVEF is one of the main diagnostic criteria of HFPEF, there is no consensus on a specific cut-off value. The National Heart, Lung, and Blood Institute’s Framingham Heart Study [9] used an LVEF > 50% as cut-off for normal or mildly abnormal systolic LV function and this cut-off value has meanwhile been used or proposed by others [10,11].
3. Diastolic dysfunction
Diastolic dysfunction is characterised by abnormalities in LV relaxation, filling, distensibility, and stiffness. A detail discussion on assessment follows.
Invasive assessment of LV diastolic function
Invasively acquired evidence of diastolic dysfunction for abnormal LV relaxation, filling, diastolic distensibility, and diastolic stiffness is considered as definite evidence of HFPEF.
LV relaxation is measured as time constant of LV relaxation; tau (τ), a measure of the rate of LV relaxation. Diastolic dysfunction is present when τ > 48 ms [12].
LV diastolic distensibility refers to the position on a pressure-volume plot of the LV diastolic pressure-volume relation. When LV end-diastolic pressure or pulmonary capillary wedge pressure is elevated in the presence of a normal LVEDVI, LV end-diastolic distensibility is considered to be reduced.
LV stiffness refers to a change in diastolic LV pressure relative to diastolic LV volume (dP/dV) and equals the slope of the diastolic LV pressure-volume relation. It is measured as diastolic LV stiffness modulus (b).
LV compliance is the inverse of LV stiffness (dV/dP).
Echocardiography
Cardiac catheterization has now largely been replaced by echocardiography to assess diastolic function. The initial techniques, such as mitral valve inflow pulsed-wave Doppler, are dependent on loading conditions, systolic function, and heart rate; but recent methods are load independent and have improved assessment of diastolic dysfunction to a great extent (Figure 3) [13].
Figure 3.
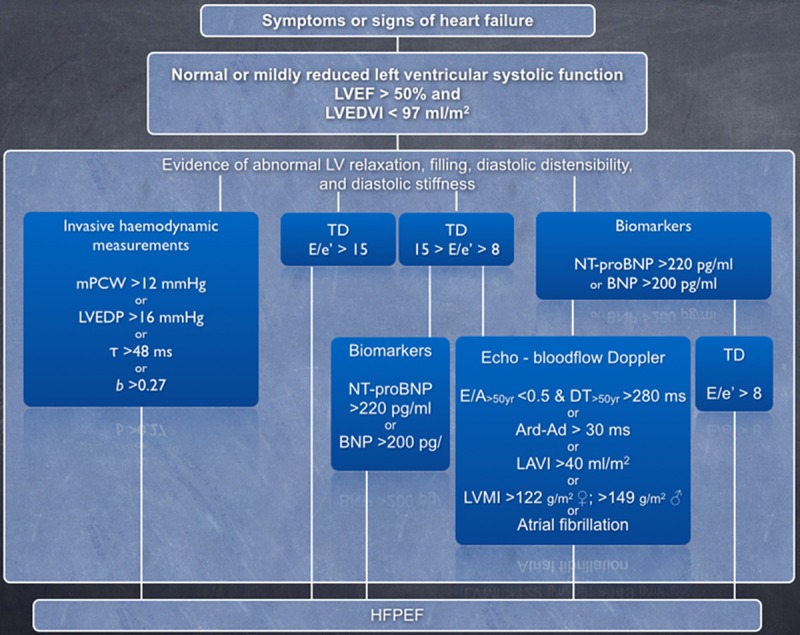
How to diagnose diastolic heart failure: a consensus statement on the diagnosis of HFPEF by the Heart Failure and Echocardiography Associations of the European Society of Cardiology [12]. LVEDVI: left ventricular end-diastolic volume index; mPCW: mean pulmonary capillary wedge pressure; LVEDP: left ventricular end-diastolic pressure; τ: time constant of left ventricular relaxation; b: constant of left ventricular chamber stiffness; TD: tissue Doppler; E: early mitral valve flow velocity; e’: early myocardial velocity at mitral annulus; NT-proBNP: N-terminal-pro brain natriuretic peptide; BNP: brain natriuretic peptide; E/A: ratio of early (E) to late (A) mitral valve flow velocity; DT: deceleration time; LVMI: left ventricular mass index; LAVI: left atrial volume index; Ard: duration of reverse pulmonary vein atrial systole flow; Ad: duration of mitral valve atrial wave flow.
Mitral inflow
Pulsed-wave Doppler is performed in the apical 4-chamber view to obtain mitral inflow velocities. Diastole is described as having 4 phases:
1. Isovolumic relaxation (IVRT); the time between aortic valve closure and mitral valve opening.
2. Rapid early filling; assessed by peak early filling/mitral inflow velocity (E).
3. Diastasis.
4. Late filling, from atrial contraction.
Isovolumic relaxation corresponds to initiation of relaxation when both the aortic valve and mitral valve are closed, measured by assessing the mitral inflow and LV outflow simultaneously by continuous waved Doppler.
When the LV pressure falls below the left atrial (LA) pressure, the mitral valve opens and the early rapid filling phase begins. The peak early filling velocity is termed “E wave”, which is recorded with the deceleration time (DT) from peak to baseline at the end of the E wave. The LV pressure gradually increases until the LV and LA pressure has equalised. At this point the early filling phase finishes and diastasis phase begins. There is essentially no net flow during the diastasis phase. The late filling phase occurs with atrial contraction and is represented by the measured A wave. In a healthy individual the E wave is bigger than A with a ratio of at least > 1. This ratio is reduced to< 1 in impaired relaxation when E wave shortens and LV filling becomes more dependent on stronger atrial contraction, i.e. the larger A wave. As the disease progresses and the relaxation is delayed further, there is an increased resting left atrial pressure which causes the filling pattern to appear normal as E/A becomes > 1. This phenomenon is termed as pseudonormalization. Progressively, the DT shortens due to flow into the noncompliant ventricle and the atrial contribution to filling is attenuated due to the early, rapid rise in left ventricular pressure. This restrictive filling pattern is characterized by very high E/A ratio (≥ 2), decreased IVRT, and decreased DT. A restrictive filling pattern is associated with a poor prognosis, especially if it persists after preload reduction. Likewise, restrictive filling pattern associated with acute myocardial infarction indicates an increased risk for heart failure, unfavourable LV remodelling, and increased cardiovascular mortality, irrespective of EF.
The normal values for these measurements are age dependent; E and E/A ratio decrease while IVRT, DT, and A velocity increase with age [14]. The normal values for Doppler-derived diastolic measurements are given in Table 1. Other factors also affect mitral inflow, including heart rate, rhythm, PR interval, cardiac output, mitral annular size, LA function, and more importantly, preload.
Table 1.
| Measurement | Age group (y) | |||
|---|---|---|---|---|
|
| ||||
| 16-20 | 21-40 | 41-60 | > 60 | |
| IVRT (ms) | 50 ± 9 (32-68) | 67 ± 8 (51-83) | 74 ± 7 (60-88) | 87 ± 7 (73-101) |
| E/A ratio | 1.88 ± 0.45 (0.98-2.78) | 1.53 ± 0.40 (0.73-2.33) | 1.28 ± 0.25 (0.78-1.78) | 0.96 ± 0.18 (0.6-1.32) |
| DT (ms) | 142 ± 19 (104-180) | 166 ± 14 (138-194) | 181 ± 19 (143-219) | 200 ± 29 (142-258) |
| A duration (ms) | 113 ± 17 (79-147) | 127 ± 13 (101-153) | 133 ± 13 (107-159) | 138 ± 19 (100-176) |
| PV S/D ratio | 0.82 ± 0.18 (0.46-1.18) | 0.98 ± 0.32 (0.34-1.62) | 1.21 ± 0.2 (0.81-1.61) | 1.39 ± 0.47 (0.45-2.33) |
| PV Ar (cm/s) | 16 ± 10 (1-36) | 21 ± 8 (5-37) | 23 ± 3 (17-29) | 25 ± 9 (11-39) |
| PV Ar duration (ms) | 66 ± 39 (1-144) | 96 ± 33 (30-162) | 112 ± 15 (82-142) | 113 ± 30 (53-173) |
| Septal e’ (cm/s) | 14.9 ± 2.4 (10.1-19.7) | 15.5 ± 2.7 (10.1-20.9) | 12.2 ± 2.3 (7.6-16.8) | 10.4 ± 2.1 (6.2-14.6) |
| Septal e’/a’ ratio | 2.4 | 1.6 ± 0.5 (0.6-2.6) | 1.1 ± 0.3 (0.5-1.7) | 0.85 ± 0.2 (0.45-1.25) |
| Lateral e’ (cm/s) | 20.6 ± 3.8 (13-28.2) | 19.8 ± 2.9 (14-25.6) | 16.1 ± 2.3 (11.5-20.7) | 12.9 ± 3.5 (5.9-19.9) |
| Lateral e’/a’ ratio | 3.1 | 1.9 ± 0.6 (0.7-3.1) | 1.5 ± 0.5 (0.5-2.5) | 0.9 ± 0.4 (0.1-1.7) |
Data are expressed as mean ± SD (95% confidence interval). Note that for e’ velocity in subjects aged 16 to 20 years, values overlap with those for subjects aged 21 to 40 years. This is because e’ increases progressively with age in children and adolescents. Therefore, the e’ velocity is higher in a normal 20-year-old than in a normal 16-year-old, which results in a somewhat lower average e’ value when subjects aged 16 to 20 years are considered.
Valsalva manoeuvre
The Valsalva manoeuvre helps to differentiate normal from pseudonormal mitral inflow patterns. In a healthy individual with normal mitral inflow, both E and A velocity will decrease with valsalva manoeuvre and the ratio will remain unchanged, with prolongation of DT. In myocardial disease, a decrease of ≥ 50% in the E/A ratio is highly specific for increased LV filling pressures [15].
Left atrial volume
LA enlargement is an excellent marker of the diastolic dysfunction chronicity as well as a predictor of adverse cardiovascular events (Figure 1) [16,17]. LA volume index ≥ 34 mL/m2 has been suggested to as an independent predictor of death, heart failure, atrial fibrillation, and ischemic stroke [18]. LA dilation can help discriminate normal from pseudonormal LV filling [19]. Other conditions causing significant LA enlargement in the absence of diastolic dysfunction include bradycardia, atrial flutter, fibrillation, significant mitral valve disease, anaemia and other high-output states.
Figure 1.
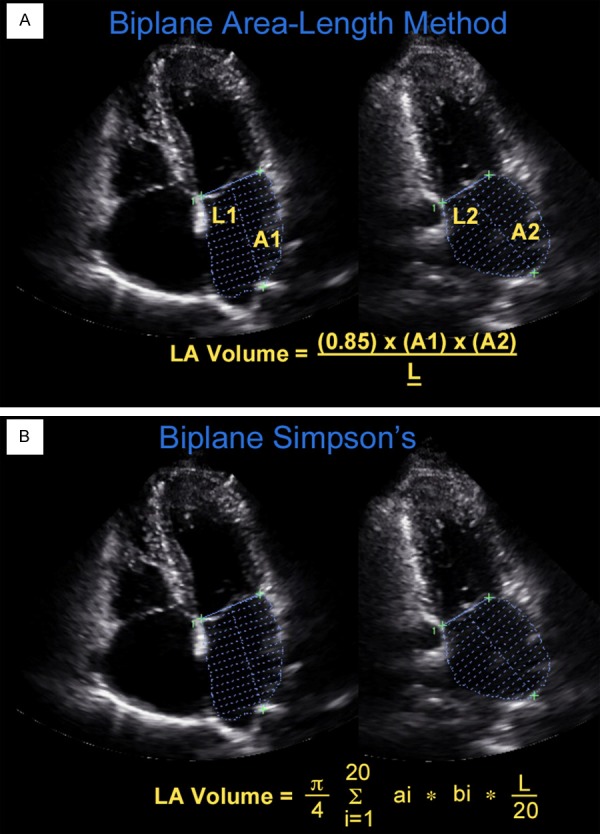
Biplane methods to calculate LA volume (A) Biplane area length, A1 = left atrial (LA) area, 4-chamber view; A2 = LA area, 2-chamber view; L1 and L2: length from midplane of mitral annulus to superior LA, L = LA length, L1 or L2 whichever is shorter; (B) Biplane Simpson’s where the volume of the LA is calculated as the sum of the volume of each individual disc.
Pulmonary venous flow
Pulsed-wave Doppler of pulmonary venous flow measuring peak systolic (S), peak anterograde diastolic (D), and peak atrial reversal (Ar) velocities in apical 4-chamber view, is an important tool for diastolic function assessment. There are two systolic velocities (S1 and S2), mostly noticeable when there is a prolonged PR interval, because S1 is related to atrial relaxation. S2 should be used to compute the ratio of peak systolic to peak diastolic velocity.
Ar velocity, and duration are influenced by LV late diastolic pressures, atrial preload, and LA contractility [20]. Although the S/D ratio and Ar velocities increase with older age, Ar velocities of more than 35 cm/s are very suggestive of increased LV end-diastolic pressure (LVEDP).
The Ar-A duration difference is age independent and can differentiate patients with abnormal LV relaxation and normal filling pressures from those with elevated LVEDPs. Although many patients with abnormal relaxation (reduced E/A) will have normal LVEDP, the isolated increase in LVEDP is the first hemodynamic abnormality seen in diastolic dysfunction and is reflected by an Ar-A duration > 30 milliseconds [21].
Assessment of LV mass
Although not a diagnostic criterion for HFPEF, increased LV mass provides supportive evidence. In patients with diastolic heart failure, concentric hypertrophy (increased mass and relative wall thickness), or remodelling (normal mass but increased relative wall thickness), can be observed. In contrast, eccentric LV hypertrophy is usually present in patients with low EFs. Because of the high prevalence of hypertension, especially in the older population, LV hypertrophy is common, and hypertensive heart disease is the most common abnormality leading to diastolic heart failure.
The ASE-recommended formula for estimation of LV mass from LV linear dimensions is based on modelling the LV as a prolate ellipse of revolution [22]:
LV mass = 0.8 × {1.04[(LVIDd + PWTd + SWTd)3 − (LVIDd)3]} + 0.6 g
where PWTd and SWTd are posterior wall thickness at end diastole and septal wall thickness at end diastole, respectively. This formula is appropriate for evaluating pa-tients without major distortions of LV geometry (e.g. patients with hypertension). Because this formula requires cubing primary measur-ements, even small errors in these measurements are magnified.
The most commonly used 2D methods for measuring LV mass are based on the area-length formula and the truncated ellipsoid model [23]. In the presence of extensive regional wall-motion abnormalities (e.g., MI), the biplane Simpson’s method may be used. The Normal values for LV mass differ between men and women even when indexed for BSA. Reference limits and partition values of left ventricular mass and geometry (LV mass/BSA, g/m2) as per ASE recommendations[22] are:
1. Linear Method: 43-95 in women, 49-115 in men.
2. 2D Method: 44-88 in women, 50-102 in men.
Colour M-mode velocity propagation
Colour M-mode and tissue Doppler imaging are less load dependent. Colour flow mapping with M-mode can differentiate normal from restrictive physiology. It measures the slowing of mitral-to-apical flow propagation due to intra-ventricular flow disturbance, suggestive of LV diastolic dysfunction.
Flow propagation velocity (Vp) is the rate of inflow from the mitral annulus to the apex, and can be measured during early filling. A Vp > 50 cm/s is considered normal [24,25]. Mitral E velocity to Vp ratio has been shown to be directly proportional to LA pressure, making it a useful parameter to predict elevated filling pressures [24]. An E/Vp ratio ≥ 1.5 is associated with elevated LA pressure and has been shown to be a strong predictor of in-hospital heart failure, and survival [26].
In most patients with depressed EFs, multiple echocardiographic signs of impaired LV diastolic function are present, and Vp is often redundant as a means to identify diastolic dysfunction. However, in this population, should other Doppler indices appear inconclusive, Vp can provide useful information for the prediction of LV filling pressures, and E/Vp ≥ 2.5 predicts PCWP > 15 mm Hg with reasonable accuracy [27]. However, care should be taken while interpreting Vp in people with preserved LVEF and abnormal filling pressures. It has been suggested that LV systolic performance may play a key role in generating a much faster Vp, especially in patients with relatively better LV systolic performance[28].
Tissue Doppler imaging
Tissue Doppler imaging (TDI) is a sensitive and load-independent measure of LV relaxation and should be part on any standard echocardiographic examination. Pulsed-wave TDI performed in the apical view measures mitral annular velocities including systolic, early diastolic(e’), and late diastolic (a’) annular velocities.
An e’ velocity is affected by changes in LV relaxation, preload, systolic function, and LV pressure. Most patients with e’ (lateral)< 8.5 cm/s or e’ (septal)< 8 cm/s have impaired myocardial relaxation [21,29]. However, for the most reliable conclusions, it is important to determine whether e’ is less than the mean minus 2 standard deviations of the age group to which the patient belongs (Table 1).
The ratio of mitral inflow E velocity and annular e’ velocity (E/e’) has been shown to predict LV filling pressures without being influenced by the effect of LV relaxation on peak E velocity. It has been consistently shown to correlate well with the invasive diastolic pressure measurements independent of LVEF [27,30-37]. The Heart Failure and Echocardiography Associations of the European Society of Cardiology propose an E/e’ ratio< 8 as consistent with normal LV filling pressure while a ratio > 15 suggestive of increased filling pressures, based on pulsed Doppler measurements and on averaged velocities of lateral and septal mitral annulus (Figure 4). When the value is between 8 and 15, other echocardiographic indices should be used. For the assessment of global LV diastolic function, it is recommended to acquire and measure tissue Doppler signals at least at the septal and lateral sides of the mitral annulus and their average, given the influence of regional function on these velocities and time intervals [27,38]. This is becomes particularly important in the presence of regional LV dysfunction.
Figure 4.
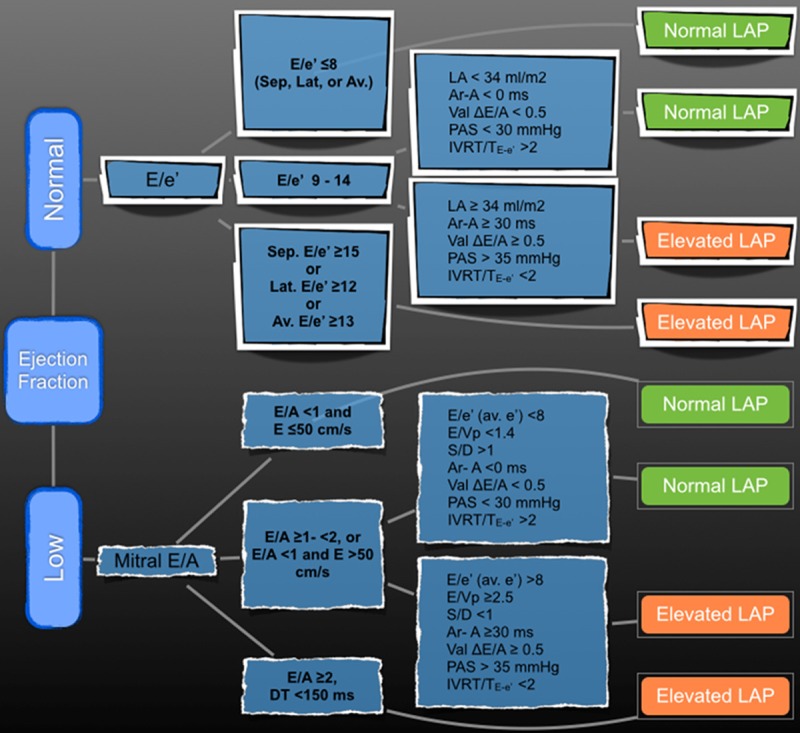
Diagnostic algorithm for the estimation of LV filling pressures [21,29]. LA: left atrium; Val: Valsalva; e’: early myocardial velocity at mitral annulus; E: early mitral valve inflow velocity; A: late mitral valve inflow velocity; DT: deceleration time of E velocity; IVRT: isovolumic relaxation; Ar-A: peak pulmonary venous atrial reversal velocity duration; PAS: pulmonary artery pressure; S: peak systolic pulmonary venous velocity; D: peak anterograde diastolic pulmonary venous velocity; LAP: left atrial pressure.
Age has been found to be a strong factor affecting the e’ velocity and E/e’ ratio. As age increases, the e’ velocity decreases; and the a’ velocity and E/e’ ratio increase [39]. E/e’ ratio is also affected by annular calcification, mitral valve disease, and constrictive pericarditis [40]. It is preferable to use the average e’ velocity obtained from the septal and lateral sides of the mitral annulus for the prediction of LV filling pressures as mentioned above. Because septal e’ is usually lower than lateral e’ velocity, the E/e’ ratio using septal signals is usually higher than the ratio derived by lateral e’, and different cut-off values should be applied on the basis of LVEF, as well as e’ location.
Speckle-tracking echocardiography
Speckle-tracking is another new technology in the field of echocardiography to assess LV function. Speckle-tracking evaluates myocardial deformation and assesses LV torsion dynamics by assessing twist and untwist magnitude and rates [41]. The speckles function as natural acoustic markers that can be tracked from frame to frame, and velocity and strain are obtained by automated measurement of distance between speckles. These measures were previously only possible with the use of CMRI with tissue tagging, but complexity and cost limit this methodology to research protocols.
Limitations of this technique include the dependence on 2-dimensional (2D) image quality and frame rates, difficulty of selection of image plane, and the reproducibility and variability of measurements from ventricles with different geometries [42].
Strain and strain rate
Myocardial deformation is expressed as strain, which can be either fractional or percentage, and strain rates. Systolic strain represents percentage short-ening in the long axis and percentage radial thickening in the short axis, lengthening and thickening strains assigned positive values and shortening and thinning strains negative values.
Similarly, the strain rate represents the speed with which this deformation occurs. Myocardial strain and strain rate is an excellent measure to quantify the regional wall function.
A number of studies suggest that myocardial strain and strain rate may provide unique information regarding diastolic function. This incudes the quantification of post-systolic myocardial strain as a measure of post-ejection shortening in ischemic myocardium [43] and regional diastolic strain rate, which can be used to evaluate diastolic stiffness during stunning and infarction [44,45]. There is evidence in an animal model that segmental early diastolic strain rate correlates with the degree of interstitial fibrosis [44].
Few studies have shown a significant relation between segmental and global early diastolic strain rate and the time constant of LV relaxation[46,47]. Wang et al. in this study [47] combined global myocardial strain rate during the isovolumetric relaxation period (by speckle tracking) and transmitral flow velocities, and showed that the mitral E velocity/global myocardial strain rate ratio predicted LV filling pressure in patients in whom the E/e’ ratio was inconclusive, i.e. 8 to 15, and was more accurate than E/e’ in patients with normal EFs and those with regional dysfunction.
LV torsion
During the systole phase of cardiac cycle, the base rotates in a clockwise direction when viewed from the apex, whilst the apex rotates counter clockwise causing the ventricle to twist. This is followed by rapid untwisting during diastole which causes a suction effect contributing to ventricular filling. Association of this phenomenon, termed as LV torsion, with early LV filling has been confirmed both in animals and humans [48,49].
The LV torsion dynamics studied in normal people suggests this complex phenomenon is directly related to myocardial muscle fibre orientation [50,51]. The multi-layered fibre arrangements in longitudinal, circumferential and spiral directions cause the heart to contract in a twisting motion during systole and untwisting during diastole. Untwisting starts in late systole but mostly occurs during the isovolumetric relaxation period and is largely finished at the time of mitral valve opening [52]. Diastolic untwist represents elastic recoil due to the release of restoring forces that have been generated during the preceding systole, contributing to LV filling through suction generation. If the negative pressure suction due to this untwisting motion during diastole is reduced due to impaired LV torsion, early diastolic LV filling may be compromised and ultimately despite a normal ejection fraction leading to symptoms of heart failure (HFPEF), elevated filling pressures, and left atrial (LA) hypertrophy. These symptoms in particular dyspnoea increases on exertion and is one of the early occurrences in diastolic heart failure. This may be because the rapid untwisting of left ventricle becomes particularly important during the exercise when due to rapid heart rate a more efficient LV filling is required and when failure to do so may lead to symptoms of dyspnoea [53]. It has been postulated that abnormalities in LV torsion post exercise can predict reduced exercise tolerance in people with HFPEF [54]. Interestingly, diastolic dysf-unction associated with normal aging does not appear to be due to a reduction in diastolic untwist [55], which can be a useful consideration when distinguishing between pathological ad physiological processes related to diastolic dysfunction in elderly people.
LV torsion magnitude and rates can be calculated by using speckle-tracking echocardiography as the difference between basal and apical rotation measured in LV short-axis images. Measurements of LV torsional dynamics are not recommended for routine clinical use at this point of time and additional studies are needed to define their potential clinical app-ications.
Grading diastolic dysfunction
Management strategies may vary depending on the severity of diastolic dysfunction [56]. It can be categorised into 4 grades based on the echocardiographic findings (Figure 2) [21,29]:
Figure 2.
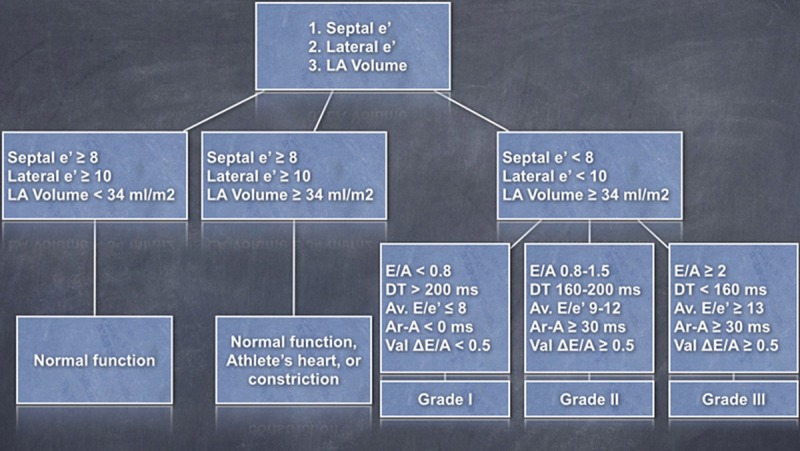
Scheme for grading diastolic dysfunction [21,29]. Av: Average; LA: left atrium; Val: Valsalva; e’: early myocardial velocity at mitral annulus; E: early mitral valve inflow velocity; A: late mitral valve inflow velocity; DT: deceleration time of E velocity; Ar-A: peak pulmonary venous atrial reversal velocity duration.
Grade I diastolic dysfunction: Impaired relaxation. There is no evidence of increased filling pressures at rest. This stage is characterized by a reduction in early diastolic mitral flow velocity (E) and an increase in late diastolic filling(A). The E/A ratio is reduced (< 0.8) with the prolongation of DT (> 200 ms) and IVRT (≥ 100 ms) [57]. The S wave is dominant in the pulmonary venous inflow tracing (S > D). Annular e’ is< 8 cm/s. The Ar-A duration is< 30 milliseconds and E/e’ of ≥ 8 (septal and lateral), indicating normal filling pressure at this stage.
These patients have reduced diastolic reserve that can be uncovered by stress testing. However, care should be taken when interpreting E/A ratio since a reduced mitral E/A ratio in the presence of normal annular tissue Doppler velocities can be seen in volume-depleted normal subjects.
Grade II diastolic dysfunction: Pseudonormal filling pattern. It represents impaired myocardial relaxation with mild to moderate elevation of LV filling pressures. In these patients, the mitral inflow resembles a normal pattern due to elevated LA pressure causing increased E wave, hence a normal E/A ratio (0.8 to 1.5), with normal DT. The E/A ratio decreases by ≥ 50% during the Valsalva manoeuvre. There is decreased LV compliance and increased LA pressure at rest [58]. The D wave in the pulmonary venous inflow tracing will be dominant (S/D ratio< 1). Ar velocity > 30 cm/s and E/e’ (average) ratio is increased (9-12, may be even greater). Annular e’ is< 8 cm/s.
In some patients LV end-diastolic pressure is the only pressure that is increased (i.e., mean LA pressure is normal) and is recognized by Ar-A duration ≥ 30 milliseconds.
Grade III to IV diastolic dysfunction: Restrictive LV filling. There is impaired relaxation with markedly elevated filling pressures. Left ventricular compliance is also severely impaired. The restrictive pattern is characterised by an increased E/A ratio ≥ 2) and shortening of the IVRT (≥ 60 ms) and DT (< 160 milliseconds). The average E/e’ >13, or septal E/e’ is ≥ 15. The S wave in the pulmonary venous inflow is markedly reduced or absent. Systolic filling fraction ≥ 40%.
Restrictive LV filling pattern is only observed in 10% of cases of HFPEF [59]. LV filling may revert to impaired relaxation with successful therapy in some patients. The irreversible or fixed restrictive filling abnormality is termed as grade IV diastolic dysfunction, and represents a high risk for cardiac morbidity and mortality. However, grade IV dysfunction should not be determined by a single examination and requires serial studies after treatment is optimized.
Differentiating pseudonormal phase form normal
1. Valsalva manoeuvre: reversal of E/A ratio in pseudonormal phase, but not in a normal person.
2. Reduced mitral annulus e’ velocity on TDI and increased E/e’.
3. Dominant D wave on pulmonary venous Doppler with prolonged Ar-A duration.
4. Reduced propagation velocity of mitral in-flow towards the apex using colour M-mode, and increased E/Vp ratio.
5. Impaired systolic LV function suggests concomitant diastolic dysfunction.
6. LV hypertrophy is again suggestive of diastolic dysfunction.
7. LA dilation also supports the diagnosis of diastolic dysfunction.
Normal values of echocardiographic parameters
Age is a primary consideration when defining normal values of mitral inflow velocities and time intervals (Table 1). It may represent a slowing of myocardial relaxation with age, which predisposes older individuals to the development of diastolic heart failure.
It should be noted that apart from the diastolic function and filling pressure, a number of other variables can affect mitral inflow. These factors include heart rate and rhythm, PR interval, cardiac output, mitral annular size, and LA function.
Diagnosis by CMRI
Cardiac MRI is not affected by the body habitus and other factors limiting views on echocardiography. It can measure blood flow velocities at any location and has the ability to and analysis of myocardial strain and torsion recovery rate by placement of myocardial tag markers.
Phase-contrast CMRI allows trans-mitral and pulmonary vein flow assessments similar to Doppler echocardiography [60]. It can also be used to inspect myocardial tissue velocity. The E/e’ ratio measured with CMRI has been shown to be comparable to that of TDI readings [61].
Gradient echo CMRI uses radiofrequency pulses gated to the electrocardiogram, which permits imaging at multiple phases of the cardiac cycle so that a cine display can be generated. This allows for accurate and reproducible quantitative assessment of chamber dimensions and systolic function. From multiple short-axis images of LV volume during diastole, global ventricular filling can be analysed.
CMRI tagging is a technique by which a radio-frequency pulse is applied to LV myocardium in the form of grid lines and allows accurate analysis of diastolic strain and 3D motion (including rotation and torsion) of the heart [62]. The deformations are measured using units of strain (percentage S) or torsion (degree).
Influence of atrial fibrillation on diastolic function assessment
Atrial fibrillation (AF) causes loss of A wave (no atrial systole) and a beat to beat variation in LV filling and ejection. It is recommended that measurements taken in AF be averaged over at least 5 cardiac cycles.
The E/e’ ratio remains a useful tool in the assessment of HFPEF in the presence of AF. A cut-off of 13 carries sensitivity of 81.8% and specificity of 89.5% in elderly patients with permanent, nonvalvular atrial fibrillation [63], and E/e’ > 15 is suggested an independent predictor of mortality [64].
Pulmonary venous flow patterns may also be useful in AF. A deceleration time of the D-wave > 220 ms has been shown to predict mean pulmonary capillary wedge pressure ≥ 12 mm Hg with 100% sensitivity and specificity [65].
Diastolic stress test
Many patients with diastolic dysfunction have symptoms mainly with exertion, because of the rise in filling pressures that is needed to maintain adequate LV filling and stroke volume. Therefore, it is useful to evaluate LV filling pressure with exercise. The test is most useful in patients with unexplained exertional dyspnoea who have mild diastolic dysfunction and normal filling pressures at rest.
In healthy individuals with normal myocardial relaxation, E and e’ velocities increase proportionally, hence the E/e’ ratio remains unchanged or is reduced [66]. However, in patients with impaired myocardial relaxation, the increase in e’ with exercise is much less than that of mitral E velocity, leading to an increased E/e’ ratio [67]. This E/e’ ratio correlates with invasively measured LVDP during exercise and can be used to reliably identify patients with elevated LVDP during exercise and reduced exercise capacity [68]. In addition, mitral DT decreases slightly in normal individuals with exercise, but shortens > 50 ms in patients with a marked elevation of filling pressures.
As mentioned before, the change in E/e’ ratio on exercise is mainly due to changes in mitral E velocity in patients with abnormal diastolic function. The E velocity increases with exertion and stays increased for a few minutes after the termination of exercise, whereas e’ velocity remains unchanged at baseline, exercise, and recovery. Therefore, E and e’ velocities can be recorded after exercise, after 2D images have been obtained for wall motion analysis. The delayed recording of Doppler velocities has an added advantage of being able to avoid the merging of E and A waves that occurs at faster heart rates. A recent study suggests that diastolic stress test can be a clinically significant tool to predict subsequent cardiovascular hospitalization in a small group of patients who present with exertional dyspnoea and normal filling pressures at rest, but demonstrate an increase of E/e’ on exercise [69].
Conclusion
Assessment of HEPEF is complex and has clinical and prognostic implications. A variety of tools are available to accurately predict the diastolic function and LV filling pressure amongst which a transthoracic echocardiogram remains the investigation of choice. It is non invasive, cost effective, and if used appropriately can help diagnose or rule out HFPEF with a sensitivity and specificity comparable to that of invasive measures or modalities like cardiac MRI. Advances in its diagnostic algorithms will allow better and timely diagnosis of this syndrome with potential benefits to the clinical outcomes, e.g. morbidity and prognosis.
Disclosure of conflict of interest
None to declare.
References
- 1.van Kraaij DJ, van Pol PE, Ruiters AW, de Swart JB, Lips DJ, Lencer N, Doevendans PA. Diagnosing diastolic heart failure. Eur J Heart Fail. 2002;4:419–430. doi: 10.1016/s1388-9842(02)00020-x. [DOI] [PubMed] [Google Scholar]
- 2.Kitzman DW. Exercise intolerance. Prog Cardiovasc Dis. 2005;47:367–379. doi: 10.1016/j.pcad.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 3.Little WC, Kitzman DW, Cheng CP. Diastolic dysfunction as a cause of exercise intolerance. Heart Fail Rev. 2000;5:301–306. doi: 10.1023/a:1026503028065. [DOI] [PubMed] [Google Scholar]
- 4.Brubaker PH, Marburger CT, Morgan TM, Fray B, Kitzman DW. Exercise responses of elderly patients with diastolic versus systolic heart failure. Med Sci Sports Exerc. 2003;35:1477–1485. doi: 10.1249/01.MSS.0000084416.71232.EA. [DOI] [PubMed] [Google Scholar]
- 5.Kitzman DW, Daniel KR. Diastolic heart failure in the elderly. Clin Geriatr Med. 2007;23:83–106. doi: 10.1016/j.cger.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 6.Rich MW. Heart failure in older adults. Med Clin North Am. 2006;90:863–885. xi. doi: 10.1016/j.mcna.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 7.Beattie S. Heart failure with preserved LV function: pathophysiology, clinical presentation, treatment, and nursing implications. J Cardiovasc Nurs. 2000;14:24–37. doi: 10.1097/00005082-200007000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Asrar ul Haq M, Wong C. Heart failure with preserved myocardial contractility: understanding the pathophysiology. European Journal of Health. 2013;2013 [Google Scholar]
- 9.Vasan RS, Levy D. Defining diastolic heart failure: a call for standardized diagnostic criteria. Circulation. 2000;101:2118–2121. doi: 10.1161/01.cir.101.17.2118. [DOI] [PubMed] [Google Scholar]
- 10.Zile MR, Gaasch WH, Carroll JD, Feldman MD, Aurigemma GP, Schaer GL, Ghali JK, Liebson PR. Heart failure with a normal ejection fraction: is measurement of diastolic function necessary to make the diagnosis of diastolic heart failure? Circulation. 2001;104:779–782. doi: 10.1161/hc3201.094226. [DOI] [PubMed] [Google Scholar]
- 11.Yturralde RF, Gaasch WH. Diagnostic criteria for diastolic heart failure. Prog Cardiovasc Dis. 2005;47:314–319. doi: 10.1016/j.pcad.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Paulus WJ, Tschope C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE, Marino P, Smiseth OA, De Keulenaer G, Leite-Moreira AF, Borbely A, Edes I, Handoko ML, Heymans S, Pezzali N, Pieske B, Dickstein K, Fraser AG, Brutsaert DL. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J. 2007;28:2539–2550. doi: 10.1093/eurheartj/ehm037. [DOI] [PubMed] [Google Scholar]
- 13.Appleton CP, Firstenberg MS, Garcia MJ, Thomas JD. The echo-Doppler evaluation of left ventricular diastolic function. A current perspective. Cardiol Clin. 2000;18:513–546. ix. doi: 10.1016/s0733-8651(05)70159-4. [DOI] [PubMed] [Google Scholar]
- 14.Klein AL, Burstow DJ, Tajik AJ, Zachariah PK, Bailey KR, Seward JB. Effects of age on left ventricular dimensions and filling dynamics in 117 normal persons. Mayo Clin Proc. 1994;69:212–224. doi: 10.1016/s0025-6196(12)61059-3. [DOI] [PubMed] [Google Scholar]
- 15.Hurrell DG, Nishimura RA, Ilstrup DM, Appleton CP. Utility of preload alteration in assessment of left ventricular filling pressure by Doppler echocardiography: a simultaneous catheterization and Doppler echocardiographic study. J Am Coll Cardiol. 1997;30:459–467. doi: 10.1016/s0735-1097(97)00184-8. [DOI] [PubMed] [Google Scholar]
- 16.Takemoto Y, Barnes ME, Seward JB, Lester SJ, Appleton CA, Gersh BJ, Bailey KR, Tsang TS. Usefulness of left atrial volume in predicting first congestive heart failure in patients > or = 65 years of age with well-preserved left ventricular systolic function. Am J Cardiol. 2005;96:832–836. doi: 10.1016/j.amjcard.2005.05.031. [DOI] [PubMed] [Google Scholar]
- 17.Tsang TS, Barnes ME, Gersh BJ, Takemoto Y, Rosales AG, Bailey KR, Seward JB. Prediction of risk for first age-related cardiovascular events in an elderly population: the incremental value of echocardiography. J Am Coll Cardiol. 2003;42:1199–1205. doi: 10.1016/s0735-1097(03)00943-4. [DOI] [PubMed] [Google Scholar]
- 18.Abhayaratna WP, Seward JB, Appleton CP, Douglas PS, Oh JK, Tajik AJ, Tsang TS. Left atrial size: physiologic determinants and clinical applications. J Am Coll Cardiol. 2006;47:2357–2363. doi: 10.1016/j.jacc.2006.02.048. [DOI] [PubMed] [Google Scholar]
- 19.De Castro S, Caselli S, Di Angelantonio E, Del Colle S, Mirabelli F, Marcantonio A, Puccio D, Santini D, Pandian NG. Relation of left atrial maximal volume measured by real-time 3D echocardiography to demographic, clinical, and Doppler variables. Am J Cardiol. 2008;101:1347–1352. doi: 10.1016/j.amjcard.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 20.Keren G, Bier A, Sherez J, Miura D, Keefe D, LeJemtel T. Atrial contraction is an important determinant of pulmonary venous flow. J Am Coll Cardiol. 1986;7:693–695. doi: 10.1016/s0735-1097(86)80482-x. [DOI] [PubMed] [Google Scholar]
- 21.Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelista A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009;22:107–133. doi: 10.1016/j.echo.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 22.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ Chamber Quantification Writing Group; American Society of Echocardiography’s Guidelines and Standards Committee; European Association of Echocardiography. Recommendations for Chamber Quantification: A Report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, Developed in Conjunction with the European Association of Echocardiography, a Branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 23.Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardio-grams. J Am Soc Echocardiogr. 1989;2:358–367. doi: 10.1016/s0894-7317(89)80014-8. [DOI] [PubMed] [Google Scholar]
- 24.Garcia MJ, Ares MA, Asher C, Rodriguez L, Vandervoort P, Thomas JD. An index of early left ventricular filling that combined with pulsed Doppler peak E velocity may estimate capillary wedge pressure. J Am Coll Cardiol. 1997;29:448–454. doi: 10.1016/s0735-1097(96)00496-2. [DOI] [PubMed] [Google Scholar]
- 25.Takatsuji H, Mikami T, Urasawa K, Teranishi J, Onozuka H, Takagi C, Makita Y, Matsuo H, Kusuoka H, Kitabatake A. A new approach for evaluation of left ventricular diastolic function: spatial and temporal analysis of left ventricular filling flow propagation by color M-mode Doppler echocardiography. J Am Coll Cardiol. 1996;27:365–371. doi: 10.1016/0735-1097(96)81240-x. [DOI] [PubMed] [Google Scholar]
- 26.Moller JE, Sondergaard E, Seward JB, Appleton CP, Egstrup K. Ratio of left ventricular peak E-wave velocity to flow propagation velocity assessed by color M-mode Doppler echocardiography in first myocardial infarction: prognostic and clinical implications. J Am Coll Cardiol. 2000;35:363–370. doi: 10.1016/s0735-1097(99)00575-6. [DOI] [PubMed] [Google Scholar]
- 27.Rivas-Gotz C, Manolios M, Thohan V, Nagueh SF. Impact of left ventricular ejection fraction on estimation of left ventricular filling pressures using tissue Doppler and flow propagation velocity. Am J Cardiol. 2003;91:780–784. doi: 10.1016/s0002-9149(02)03433-1. [DOI] [PubMed] [Google Scholar]
- 28.Ohte N, Narita H, Akita S, Kurokawa K, Hayano J, Kimura G. Striking effect of left ventricular systolic performance on propagation velocity of left ventricular early diastolic filling flow. J Am Soc Echocardiogr. 2001;14:1070–1074. doi: 10.1067/mje.2001.114136. [DOI] [PubMed] [Google Scholar]
- 29.Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelisa A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009;10:165–193. doi: 10.1093/ejechocard/jep007. [DOI] [PubMed] [Google Scholar]
- 30.Nagueh SF, Lakkis NM, Middleton KJ, Spencer WH 3rd, Zoghbi WA, Quinones MA. Doppler estimation of left ventricular filling pressures in patients with hypertrophic cardiomyopathy. Circulation. 1999;99:254–261. doi: 10.1161/01.cir.99.2.254. [DOI] [PubMed] [Google Scholar]
- 31.Nagueh SF, Mikati I, Kopelen HA, Middleton KJ, Quinones MA, Zoghbi WA. Doppler estimation of left ventricular filling pressure in sinus tachycardia. A new application of tissue doppler imaging. Circulation. 1998;98:1644–1650. doi: 10.1161/01.cir.98.16.1644. [DOI] [PubMed] [Google Scholar]
- 32.Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, Tajik AJ. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: A comparative simultaneous Doppler-catheterization study. Circulation. 2000;102:1788–1794. doi: 10.1161/01.cir.102.15.1788. [DOI] [PubMed] [Google Scholar]
- 33.Sundereswaran L, Nagueh SF, Vardan S, Middleton KJ, Zoghbi WA, Quinones MA, Torre-Amione G. Estimation of left and right ventricular filling pressures after heart transplantation by tissue Doppler imaging. Am J Cardiol. 1998;82:352–357. doi: 10.1016/s0002-9149(98)00346-4. [DOI] [PubMed] [Google Scholar]
- 34.Sohn DW, Song JM, Zo JH, Chai IH, Kim HS, Chun HG, Kim HC. Mitral annulus velocity in the evaluation of left ventricular diastolic function in atrial fibrillation. J Am Soc Echocardiogr. 1999;12:927–931. doi: 10.1016/s0894-7317(99)70145-8. [DOI] [PubMed] [Google Scholar]
- 35.Kim YJ, Sohn DW. Mitral annulus velocity in the estimation of left ventricular filling pressure: prospective study in 200 patients. J Am Soc Echocardiogr. 2000;13:980–985. doi: 10.1067/mje.2000.107156. [DOI] [PubMed] [Google Scholar]
- 36.Dokainish H, Zoghbi WA, Lakkis NM, Al-Bakshy F, Dhir M, Quinones MA, Nagueh SF. Optimal noninvasive assessment of left ventricular filling pressures: a comparison of tissue Doppler echocardiography and B-type natriuretic peptide in patients with pulmonary artery catheters. Circulation. 2004;109:2432–2439. doi: 10.1161/01.CIR.0000127882.58426.7A. [DOI] [PubMed] [Google Scholar]
- 37.Bruch C, Grude M, Muller J, Breithardt G, Wichter T. Usefulness of tissue Doppler imaging for estimation of left ventricular filling pressures in patients with systolic and diastolic heart failure. Am J Cardiol. 2005;95:892–895. doi: 10.1016/j.amjcard.2004.12.017. [DOI] [PubMed] [Google Scholar]
- 38.Nagueh SF, Rao L, Soto J, Middleton KJ, Khoury DS. Haemodynamic insights into the effects of ischaemia and cycle length on tissue Doppler-derived mitral annulus diastolic velocities. Clin Sci (Lond) 2004;106:147–154. doi: 10.1042/CS20030204. [DOI] [PubMed] [Google Scholar]
- 39.De Sutter J, De Backer J, Van de Veire N, Velghe A, De Buyzere M, Gillebert TC. Effects of age, gender, and left ventricular mass on septal mitral annulus velocity (E’) and the ratio of transmitral early peak velocity to E’ (E/E’) Am J Cardiol. 2005;95:1020–1023. doi: 10.1016/j.amjcard.2005.01.021. [DOI] [PubMed] [Google Scholar]
- 40.Ha JW, Oh JK, Ling LH, Nishimura RA, Seward JB, Tajik AJ. Annulus paradoxus: transmitral flow velocity to mitral annular velocity ratio is inversely proportional to pulmonary capillary wedge pressure in patients with constrictive pericarditis. Circulation. 2001;104:976–978. doi: 10.1161/hc3401.095705. [DOI] [PubMed] [Google Scholar]
- 41.Notomi Y, Lysyansky P, Setser RM, Shiota T, Popovic ZB, Martin-Miklovic MG, Weaver JA, Oryszak SJ, Greenberg NL, White RD, Thomas JD. Measurement of Ventricular Torsion by Two-Dimensional Ultrasound Speckle Tracking Imaging. J Am Coll Cardiol. 2005;45:2034–2041. doi: 10.1016/j.jacc.2005.02.082. [DOI] [PubMed] [Google Scholar]
- 42.Geyer H, Caracciolo G, Abe H, Wilansky S, Carerj S, Gentile F, Nesser HJ, Khandheria B, Narula J, Sengupta PP. Assessment of myocardial mechanics using speckle tracking echocardiography: fundamentals and clinical applications. J Am Soc Echocardiogr. 2010;23:351–369. doi: 10.1016/j.echo.2010.02.015. quiz 453-355. [DOI] [PubMed] [Google Scholar]
- 43.Voigt JU, Exner B, Schmiedehausen K, Huch-zermeyer C, Reulbach U, Nixdorff U, Platsch G, Kuwert T, Daniel WG, Flachskampf FA. Strain-rate imaging during dobutamine stress echocardiography provides objective evidence of inducible ischemia. Circulation. 2003;107:2120–2126. doi: 10.1161/01.CIR.0000065249.69988.AA. [DOI] [PubMed] [Google Scholar]
- 44.Park TH, Nagueh SF, Khoury DS, Kopelen HA, Akrivakis S, Nasser K, Ren G, Frangogiannis NG. Impact of myocardial structure and function postinfarction on diastolic strain measurements: implications for assessment of myocardial viability. Am J Physiol Heart Circ Physiol. 2006;290:H724–731. doi: 10.1152/ajpheart.00714.2005. [DOI] [PubMed] [Google Scholar]
- 45.Pislaru C, Bruce CJ, Anagnostopoulos PC, Allen JL, Seward JB, Pellikka PA, Ritman EL, Greenleaf JF. Ultrasound strain imaging of altered myocardial stiffness: stunned versus infarcted reperfused myocardium. Circulation. 2004;109:2905–2910. doi: 10.1161/01.CIR.0000129311.73402.EF. [DOI] [PubMed] [Google Scholar]
- 46.Kato T, Noda A, Izawa H, Nishizawa T, Somura F, Yamada A, Nagata K, Iwase M, Nakao A, Yokota M. Myocardial velocity gradient as a noninvasively determined index of left ventricular diastolic dysfunction in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. 2003;42:278–285. doi: 10.1016/s0735-1097(03)00573-4. [DOI] [PubMed] [Google Scholar]
- 47.Wang J, Khoury DS, Thohan V, Torre-Amione G, Nagueh SF. Global diastolic strain rate for the assessment of left ventricular relaxation and filling pressures. Circulation. 2007;115:1376–1383. doi: 10.1161/CIRCULATIONAHA.106.662882. [DOI] [PubMed] [Google Scholar]
- 48.Notomi Y, Popovic ZB, Yamada H, Wallick DW, Martin MG, Oryszak SJ, Shiota T, Greenberg NL, Thomas JD. Ventricular untwisting: a temporal link between left ventricular relaxation and suction. Am J Physiol Heart Circ Physiol. 2008;294:H505–513. doi: 10.1152/ajpheart.00975.2007. [DOI] [PubMed] [Google Scholar]
- 49.Burns AT, La Gerche A, Prior DL, MacIsaac AI. Left ventricular untwisting is an important determinant of early diastolic function. J Am Coll Cardiol Imaqinq. 2009;2:709–16. doi: 10.1016/j.jcmg.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 50.Greenbaum RA, Ho SY, Gibson DG, Becker AE, Anderson RH. Left ventricular fibre architecture in man. Br Heart J. 1981;45:248–263. doi: 10.1136/hrt.45.3.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ingels NB Jr, Hansen DE, Daughters GT 2nd, Stinson EB, Alderman EL, Miller DC. Relation between longitudinal, circumferential, and oblique shortening and torsional deformation in the left ventricle of the transplanted human heart. Circ Res. 1989;64:915–927. doi: 10.1161/01.res.64.5.915. [DOI] [PubMed] [Google Scholar]
- 52.Rademakers FE, Buchalter MB, Rogers WJ, Zerhouni EA, Weisfeldt ML, Weiss JL, Shapiro EP. Dissociation between left ventricular untwisting and filling. Accentuation by catecholamines. Circulation. 1992;85:1572–1581. doi: 10.1161/01.cir.85.4.1572. [DOI] [PubMed] [Google Scholar]
- 53.Notomi Y, Martin-Miklovic MG, Oryszak SJ, Shiota T, Deserranno D, Popovic ZB, Garcia MJ, Greenberg NL, Thomas JD. Enhanced ventricular untwisting during exercise: a mechanistic manifestation of elastic recoil described by Doppler tissue imaging. Circulation. 2006;113:2524–2533. doi: 10.1161/CIRCULATIONAHA.105.596502. [DOI] [PubMed] [Google Scholar]
- 54.Asrar ul Haq M, Mutha V, Lin T, Profitis K, Tuer Z, Lim K, Hare DL, Wong C. Left ventricular torsional dynamics post exercise for LV diastolic function assessment. Cardiovasc Ultrasound. 2014;12:8. doi: 10.1186/1476-7120-12-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hees PS, Fleg JL, Dong SJ, Shapiro EP. MRI and echocardiographic assessment of the diastolic dysfunction of normal aging: altered LV pressure decline or load? Am J Physiol Heart Circ Physiol. 2004;286:H782–788. doi: 10.1152/ajpheart.01092.2002. [DOI] [PubMed] [Google Scholar]
- 56.Haq MA, Wong C, Mutha V, Anavekar N, Lim K, Barlis P, Hare DL. Therapeutic interventions for heart failure with preserved ejection fraction: A summary of current evidence. World J Cardiol. 2014;6:67–76. doi: 10.4330/wjc.v6.i2.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Khouri SJ, Maly GT, Suh DD, Walsh TE. A practical approach to the echocardiographic evaluation of diastolic function. J Am Soc Echocardiogr. 2004;17:290–297. doi: 10.1016/j.echo.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 58.Kuecherer HF, Muhiudeen IA, Kusumoto FM, Lee E, Moulinier LE, Cahalan MK, Schiller NB. Estimation of mean left atrial pressure from transesophageal pulsed Doppler echocardiography of pulmonary venous flow. Circulation. 1990;82:1127–1139. doi: 10.1161/01.cir.82.4.1127. [DOI] [PubMed] [Google Scholar]
- 59.Bursi F, Weston SA, Redfield MM, Jacobsen SJ, Pakhomov S, Nkomo VT, Meverden RA, Roger VL. Systolic and diastolic heart failure in the community. JAMA. 2006;296:2209–2216. doi: 10.1001/jama.296.18.2209. [DOI] [PubMed] [Google Scholar]
- 60.Srichai MB, Lim RP, Wong S, Lee VS. Cardiovascular applications of phase-contrast MRI. AJR Am J Roentgenol. 2009;192:662–675. doi: 10.2214/AJR.07.3744. [DOI] [PubMed] [Google Scholar]
- 61.Paelinck BP, de Roos A, Bax JJ, Bosmans JM, van Der Geest RJ, Dhondt D, Parizel PM, Vrints CJ, Lamb HJ. Feasibility of tissue magnetic resonance imaging: a pilot study in comparison with tissue Doppler imaging and invasive measurement. J Am Coll Cardiol. 2005;45:1109–1116. doi: 10.1016/j.jacc.2004.12.051. [DOI] [PubMed] [Google Scholar]
- 62.Gotte MJ, Germans T, Russel IK, Zwanenburg JJ, Marcus JT, van Rossum AC, van Veldhuisen DJ. Myocardial strain and torsion quantified by cardiovascular magnetic resonance tissue tagging: studies in normal and impaired left ventricular function. J Am Coll Cardiol. 2006;48:2002–2011. doi: 10.1016/j.jacc.2006.07.048. [DOI] [PubMed] [Google Scholar]
- 63.Arques S, Roux E, Sbragia P, Pieri B, Gelisse R, Luccioni R, Ambrosi P. Usefulness of bedside tissue Doppler echocardiography and B-type natriuretic peptide (BNP) in differentiating congestive heart failure from noncardiac cause of acute dyspnea in elderly patients with a normal left ventricular ejection fraction and permanent, nonvalvular atrial fibrillation: insights from a prospective, monocenter study. Echocardiography. 2007;24:499–507. doi: 10.1111/j.1540-8175.2007.00418.x. [DOI] [PubMed] [Google Scholar]
- 64.Okura H, Takada Y, Kubo T, Iwata K, Mizoguchi S, Taguchi H, Toda I, Yoshikawa J, Yoshida K. Tissue Doppler-derived index of left ventricular filling pressure, E/E’, predicts survival of patients with non-valvular atrial fibrillation. Heart. 2006;92:1248–1252. doi: 10.1136/hrt.2005.082594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chirillo F, Brunazzi MC, Barbiero M, Giavarina D, Pasqualini M, Franceschini-Grisolia E, Cotogni A, Cavarzerani A, Rigatelli G, Stritoni P, Longhini C. Estimating mean pulmonary wedge pressure in patients with chronic atrial fibrillation from transthoracic Doppler indexes of mitral and pulmonary venous flow velocity. J Am Coll Cardiol. 1997;30:19–26. doi: 10.1016/s0735-1097(97)00130-7. [DOI] [PubMed] [Google Scholar]
- 66.Ha JW, Lulic F, Bailey KR, Pellikka PA, Seward JB, Tajik AJ, Oh JK. Effects of treadmill exercise on mitral inflow and annular velocities in healthy adults. Am J Cardiol. 2003;91:114–115. doi: 10.1016/s0002-9149(02)03016-3. [DOI] [PubMed] [Google Scholar]
- 67.Ha JW, Oh JK, Pellikka PA, Ommen SR, Stussy VL, Bailey KR, Seward JB, Tajik AJ. Diastolic stress echocardiography: a novel noninvasive diagnostic test for diastolic dysfunction using supine bicycle exercise Doppler echocardiography. J Am Soc Echocardiogr. 2005;18:63–68. doi: 10.1016/j.echo.2004.08.033. [DOI] [PubMed] [Google Scholar]
- 68.Burgess MI, Jenkins C, Sharman JE, Marwick TH. Diastolic Stress Echocardiography: Hemodynamic Validation and Clinical Significance of Estimation of Ventricular Filling Pressure With Exercise. J Am Coll Cardiol. 2006;47:1891–1900. doi: 10.1016/j.jacc.2006.02.042. [DOI] [PubMed] [Google Scholar]
- 69.Holland DJ, Prasad SB, Marwick TH. Prognostic implications of left ventricular filling pressure with exercise. Circ Cardiovasc Imaging. 2010;3:149–156. doi: 10.1161/CIRCIMAGING.109.908152. [DOI] [PubMed] [Google Scholar]


