Abstract
A preliminary needs assessment was conducted among faculty and students of three minority medical and health science institutions comprising the Puerto Rico Clinical and Translational Research Consortium (PRCTRC). The Web‐based survey was focused on evaluating the training interests in the clinical and translational research core areas and competencies developed by the National Institutes of Health‐Clinical and Translational Sciences Award. The survey was the result of a team effort of three PRCTRC key function's leaderships: Multidisciplinary Training and Career Development, Tracking and Evaluation and Community Research and Engagement. The questionnaire included 45 items distributed across five content areas including demographics, research training needs, training activities coordination and knowledge about the services offered by the PRCTRC. Analysis of research needs includes a sample distribution according to professor, assistant/associate professor and graduate students. The thematic area with highest response rate among the three groups was: “Identify major clinical/public health problems and relevant translational research questions,” with the competency “Identify basic and preclinical studies that are potential testable clinical research hypothesis.” These preliminary results will guide the training and professional development of the new generation of clinical and translational researchers needed to eliminate health disparities.
Keywords: translational research, ethics, outcomes research
Introduction
Successful and productive clinical and translational research teams require a set of values and skills that are composed of traditional core clinical research competencies and a set of relatively new core translational competencies.1, 2 The translational research team can be defined by the multiplicity of disciplines or settings (i.e., geographic or thematic) working together to address a challenge from diverse perspectives with the common goal of advancing the transfer of knowledge into action.3, 4 The build‐up of values and skills needed to work in a multidisciplinary research team is usually not an inherent talent, and for successful interactions to occur, requires the development of specific competencies.5, 6, 7 This process includes reinforcing what we already know about research, learning what is new and recognizing the role of technology in advancing research, communication and dissemination.8, 9 This transformation is an ongoing process and is required for anyone desiring to be an effective and efficient clinical and translational researcher, whether they are a graduate student, postdoctoral fellow or faculty member, beginning their career or if they are at later professional stages of their career: mid‐career, experienced, or reentering.
Learning is a continuous and transformative process;10, 11 however, a particular difference among learners is their perceived need to acquire additional competencies and the strategy used to acquire them. Examples include practice, informal training, self‐learning, mentored research, formal education, advanced degrees or any combination of these.12, 13 Since capacity building activities in any academic institution should be responsive to the needs of the students and faculty, training need analysis is the initial step in a cyclical process which contributes to the overall training and educational strategy of research teams.14, 15 This study was done as a first attempt to determine the perceived need of graduate students and faculty at different stages in their academic career for training in clinical and translational research. Participants were chosen from the three medical and health sciences institutions that constitute the Puerto Rico Clinical and Translational Research Consortium (PRCTRC, http://prctrc.rcm.upr.edu/).
Supported through the National Institute of Minority Health and Health Disparities (NIMHD) at the National Institutes of Health (NIH) (U54 RR 026139 and U54 MD 007587), the PRCTRC is a research infrastructure and capacity building partnership among the University of Puerto Rico‐Medical Sciences Campus (UPR‐MSC), a public academic health sciences center as the leader; the Ponce School of Medicine and Health Sciences (PSM&HS) and Universidad Central del Caribe (UCC). The mission of the PRCTRC is to create, develop, and support an integrated island‐wide infrastructure dedicated to clinical and translational research focused on health problems prevalent in Hispanic populations (e.g., mostly Puerto Rican). As such, the PRCTRC is committed to offer research‐related services and clinical facilities to researchers as well as students and faculty interested in becoming researchers. Additionally, research training and professional development, networking, and funding for pilot projects opportunities are available. One of the main goals of the PRCTRC is to enhance and support existing training and mentoring programs to increase the number of new minority investigators in clinical and translational research.
This paper focuses on the perceived need of graduate students and faculty at different stages in their academic career for training in clinical and translational research. The principal aim of this study was to determine if there was a difference in thematic areas (TAs) among the participants, according to their level of achievement (graduate students, assistant/associate and senior faculty; with or without funded research) in order to plan capacity building activities that would address specific areas of need.
Methods
Questionnaire
Three key functions from within the PRCTRC collaborated on the design and implementation of the assessment: the Multidisciplinary Training and Career Development (MTCD) key function, the Tracking and Evaluation key Function (TEK) and the Community Research and Engagement (CRE) key function. A questionnaire was created to evaluate training interest in each of the 14 TAs and the 101 core competencies in clinical and translational research developed by the Education Core Competency Work Group of the National Institutes of Health‐Clinical and Translational Sciences (NIH‐CTS) Award.7 The set of competencies was designed to describe the skills, knowledge, and attitudes required to address clinical and translational research. Table 1 shows all TAs that were assessed. The questionnaire included 45 items distributed across five sections including an information sheet on the survey, demographics, research training needs, training activities coordination and knowledge about the services offered by the PRCTRC. It was designed to be completed in 5–15 minutes and was administered to faculty and students from the three PRCTRC member institutions using Survey Monkey, an online self‐administered questionnaire. The survey was available during a four week period during the Fall 2012.
Table 1.
Clinical and translational sciences thematic areas
| 1. Identifying Major Clinical/Public Health Problems and Relevant Translational Research Questions |
| 2. Critique the Literature Regarding the Status of a Health Problem |
| 3. Designing Study Protocol for Clinical and Translational Research |
| 4. Study Method/Design/Implementation |
| 5. Laboratory, Clinical, and Population Research Methods |
| 6. Statistical Methods and Analysis |
| 7. Biomedical and Health Informatics |
| 8. Conducting Ethically Responsible Research: |
| a. Clinical Research Ethics Competencies |
| b. Responsible Conduct of Research Competencies |
| 9. Scientific Communication Skills and Dissemination |
| 10. Population Diversity and Cultural Competency |
| 11. Translational Teamwork |
| 12. Leadership |
| 13. Cross Disciplinary Training and Mentoring |
| 14. Principles of Community Engagement |
Participant recruitment
MTCD coordinators from each PRCTRC institution requested a list of emails for all faculty and students from the Information System Office and Academic and Student Dean Offices at their respective institutions. A total of 4,406 emails were sent. Figure 1 shows the process of participants’ recruitment. Weekly follow‐up protocols were implemented by email in order to increase response rate. Only participants that completed all 14 TA (n = 321) were included in the analysis presented in this manuscript.
Figure 1.
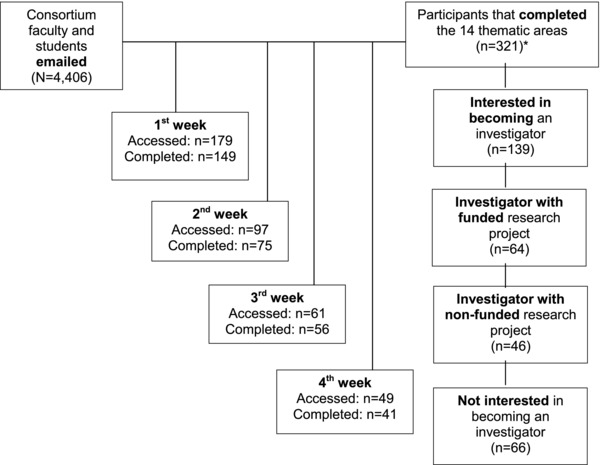
Participants recruitment.
Analysis
Descriptive statistics were used for the profile of participants who completed the survey. The interest of receiving clinical and translational research training was assessed by research investigator status (only investigators with funded or nonfunded projects and participants interested in becoming investigators were included in the study) and academic level or status (professor, assistant/associate professor, and graduate students). Chi‐square was used to determine differences between participants holding different academic level within each TA. Significant differences were identified as p‐values of <0.05. Analyses were performed using Statistical Package for the Social Sciences (SPSS) VS 19.
Results
Participants profile
A total of 321 faculty and students completed the 14 TAs of the online survey, resulting in a response rate of 7.3%. Overall, participation by institutional affiliation was: UPR‐MSC (78%, n = 252), UCC (13%, n = 40), PSM&HS (8.1%, n = 26), and other UPR centers (0.9%, n = 3). Most of the respondents were graduate students (49%, n = 156). Figure 2 shows the participant profile by academic levels. About 43% of all respondents indicated being interested in becoming an investigator; the majority were graduate students (68%, n = 95). Table 2 shows the percentage of participants within an academic level for every status of the research investigator.
Figure 2.
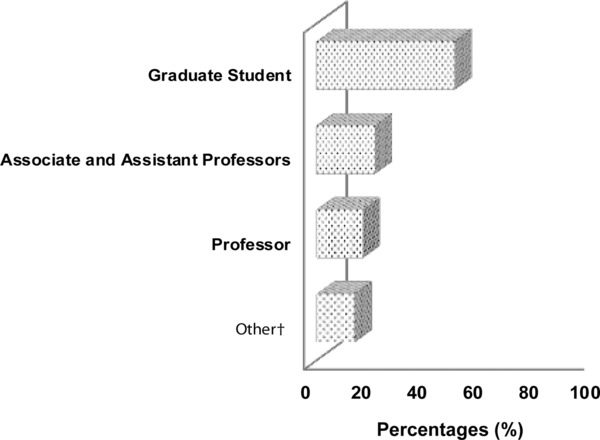
Participants profile by academic level.
Table 2.
Academic level by research investigator status (n = 315)
| Academic level, n (%) | ||||
|---|---|---|---|---|
| Research investigator status | Professors (n = 52) | Associate and assistant professors (n = 66) | Graduate students (n = 155) | Other (n = 42) |
| Not interested in becoming an investigator | 7 (13) | 6 (9.1) | 36 (23) | 17 (40) |
| Interested in becoming an investigator | 10 (19) | 16 (24) | 95 (61) | 18 (43) |
| Investigator with a funded research project | 23 (44) | 23 (35) | 14 (9.1) | 4 (9.5) |
| Investigator with a nonfunded research project | 12 (24) | 21 (32) | 10 (6.4) | 3 (7.1) |
Research training needs
TA‐1 (Identifying Major Clinical/Public Health Problems and Relevant Translational Research Questions) was the highest priority training area selected by faculty and graduate students followed by TA‐6 (Statistical Methods and Analysis) for faculty and TA‐4 (Study Method/Design/Implementation) for graduate students. However, graduate students were significantly more likely to select TA‐1 as a training need than professors and associate/assistant professors (89% vs. 71% vs. 78%; P = 0.018). Likewise, graduate students showed more interest towards TA‐4 (Study Method/Design/Implementation) and TA‐5 (Laboratory, Clinical, and Population Research Methods) than the faculty academic levels (p = 0.031 and 0.002, respectively). On the contrary, associate/assistant professors were more likely to choose TA‐11 (Translational Teamwork) as a training need as compared to students and professors (p < 0.001). Table 3 shows the comparisons of the results between academic levels for each TA.
Table 3.
Thematic areas of interest by academic level
| Thematic area, n (%) | Professor (n = 45) | Assistant and associate professors (n = 60) | Graduate students (n = 119) | p‐value* |
|---|---|---|---|---|
| 1. Identifying Major Clinical/Public Health Problems and Relevant Translational Research Questions | 32 (71) | 47 (78) | 104 (89) | 0.018 |
| 2. Critique the Literature Regarding the Status of a Health Problem | 26 (58) | 38 (63) | 84 (72) | 0.192 |
| 3. Designing Study Protocol for Clinical and Translational Research | 29 (64) | 41 (68) | 92 (79) | 0.119 |
| 4. Study Method/Design/Implementation | 27 (60) | 41 (68) | 94 (80) | 0.031 |
| 5. Laboratory, Clinical, and Population Research Methods | 23 (51) | 38 (63) | 90 (77) | 0.002 |
| 6. Statistical Methods and Analysis | 32 (71) | 46 (77) | 82 (70) | 0.686 |
| 7. Biomedical and Health Informatics | 29 (64) | 38 (63) | 63 (54) | 0.342 |
| 8. Conducting Ethically Responsible Research: | ||||
| a. Clinical Research Ethics Competencies | 19 (42) | 26 (43) | 57 (49) | 0.626 |
| b. Responsible Conduct of Research Competencies | 17 (38) | 27 (45) | 47 (40) | 0.695 |
| 9. Scientific Communication Skills and Dissemination | 27 (60) | 38 (63) | 80 (68) | 0.637 |
| 10. Population Diversity and Cultural Competency | 23 (51) | 32 (53) | 60 (51) | 0.987 |
| 11. Translational Teamwork | 28 (62) | 44 (73) | 48 (41) | <0.001 |
| 12. Leadership | 25 (56) | 31 (52) | 66 (56) | 0.780 |
| 13. Cross Disciplinary Training and Mentoring | 19 (42) | 29 (48) | 47 (40) | 0.660 |
| 14. Principles of Community Engagement | 20 (44) | 27 (45) | 47 (40) | 0.823 |
*Chi‐square test was used to compare academic appointment. Significant differences were identified as p‐values less than 0.05.
The faculty ranked the TA‐6 (Statistical Methods and Analysis) as their second training priority but they prioritized different competencies. Professors identified “Describe the Uses of Meta‐Analytic Methods” as the priority competency area for training, while assistant and associate professors preferred training on “Compute Sample Size, Power, and Precision for Comparisons of Two Independent Samples with Respect to Continuous and Binary Outcomes” (see Table 4). Furthermore, the second highest area identified by graduate students was TA‐4 (Study Method/Design/Implementation), focused on the competency “Assess Threats to Internal Validity in any Planned or Completed Clinical or Translational Study, Including Selection Bias, Misclassification, and Confounding.” Faculty and graduate students showed similar interest on most TAs; however, TA‐9: Scientific Communication Skills and Dissemination had a consensus among all three academic levels, selecting the same competency (Communicate clinical and translational research findings to different groups of individuals, including colleagues, students, the lay public, and the media). Table 4 shows the preferred competencies within TAs for each academic level.
Table 4.
Highest core competency by thematic areas: preferences by academic level
| TA* | Professors | Assistant and associate professors | Graduate students | |||
|---|---|---|---|---|---|---|
| Highest core competency | n (%) | Highest core competency | n (%) | Highest Core Competency | n (%) | |
| 1 | Derive translational questions from clinical research data. | 24 (75) | Derive translational questions from clinical research data. | 30 (64) | Identify basic and preclinical studies that are potential testable clinical research hypotheses. | 74 (71) |
| 2 | Interpret published literature in a causal framework. | 18 (69) | Conduct a comprehensive and systematic search of the literature using informatics techniques. | 29 (76) | Summarize evidence from the literature on a clinical problem. | 58 (69) |
| 3 | Formulate well‐defined clinical or translational research question. | 21 (72) | Formulate well‐defined clinical or translational research question. | 34 (83) | Propose study designs for addressing a clinical or translational research question. | 76 (83) |
| Design a research study protocol. | Design a research data analysis plan. | |||||
| 4 | Integrate elements of translational research into given study designs that could provide the bases for future research, such as the collection of biological specimens nested studies and the development of community‐based interventions. | 22 (82) | Compare the feasibility, efficiency, and ability to derive unbiased inferences from different clinical and translational research study designs. | 35 (85) | Assess threats to internal validity in any planned or completed clinical or translational study, including selection bias, misclassification, and confounding. | 70 (75) |
| 5 | Assess data sources and data quality to answer specific clinical or translational research questions. | 17 (74) | Describe the concepts and implications of reliability and validity of study measurements. | 26 (68) | Assess threats to study validity(bias) including problems with sampling, recruitment, randomization, and comparability of study groups. | 66 (73) |
| 6 | Describe the uses of meta‐analytic methods. | 21 (66) | Compute sample size, power, and precision for comparisons of two independent samples with respect to continuous and binary outcomes. | 38 (83) | Compute sample size, power, and precision for comparisons of two independent samples with respect to continuous and binary outcomes. | 62 (76) |
| 7 | Collaborate with bioinformatics specialists in the design, development, and implementation of research projects. | 20 (69) | Collaborate with bioinformatics specialists in the design, development, and implementation of research projects. | 27 (71) | Describe the effects of technology on medical research, education, and patient care. | 46 (73) |
| Develop protocols utilizing management of information using computer technology. | ||||||
| Describe the effects of technology on medical research, education, and patient care. | ||||||
| 8a | Discuss the cultural and social variation in standards of research integrity. | 12 (63) | Discuss the cultural and social variation in standards of research integrity. | 21 (81) | Explain the special issues that arise in research with vulnerable participants and the need for additional safeguards. | 43 (75) |
| 8b | Apply the main rules, guidelines, codes, and professional standards for the conduct of clinical and translational research. | 11 (64) | Describe cultural and social variation in standards of research integrity. | 18 (67) | Apply the main rules, guidelines, codes, and professional standards for the conduct of clinical and translational research. | 40 (83) |
| Describe cultural and social variation in standards of research integrity. | ||||||
| 9 | Communicate clinical and translational research findings to different groups of individuals, including colleagues, students, the lay public, and the media. | 20 (74) | Communicate clinical and translational research findings to different groups of individuals, including colleagues, students, the lay public, and the media. | 29 (76) | Communicate clinical and translational research findings to different groups of individuals, including colleagues, students, the lay public, and the media. | 71 (89) |
| 10 | Discuss the role of health literacy principles of human subjects in their ability to learn, retrain, and practice health information. | 18 (78) | Describe studies that recognize the determinants of health disparities. | 25 (78) | Differentiate between cultural and population diversity principles. | 53 (88) |
| 11 | Manage a clinical and/or translational research study. | 21 (75) | Build an interdisciplinary/intradisciplinary/multidisciplinary team that matches the objectives of the research problem. | 32 (73) | Build an interdisciplinary/intradisciplinary/multidisciplinary team that matches the objectives of the research problem. | 41 (81) |
| 12 | Maintain skills as mentor and mentee. | 19 (76) | Work as a leader of a multidisciplinary research team. | 25 (81) | Maintain skills as mentor and mentee. | 58 (88) |
| 13 | Incorporate adult learning principles and mentoring strategies into interactions with beginning scientists and scholars in order to engage them in clinical and translational research. | 14 (74) | Provide clinical and translational science instruction to beginning scientists. | 21 (72) | Apply principles of adult learning and competency‐based instruction to educational activities. | 37 (79) |
| 14 | Summarize(analysis level) the principles and practices of the spectrum of community‐engaged research. | 17 (85) | Specify (synthesis level) how cultural and linguistic competence and health literacy have an impact on the conduct of community engaged research. | 22 (82) | Apprise (analysis & evaluation levels) the role of community engagement as a strategy for identifying community health issues, translating health research to communities and reducing health disparities. | 40 (85) |
*TA: see Table 1.
Discussion
This study determined the interest of a specific group of students and faculty at nonresearch‐intensive minority institutions for the NIH core and TAs and competencies in clinical and translational research. The results will guide our efforts in the planning of capacity building activities and design of future needs surveys for faculty and graduate students engaged in this field of research. The online survey presented is a first comprehensive initiative to explore training needs in these core TAs and competencies of faculty and graduate students interested in research from the three PRCTRC Consortium institutions.
More than 4,000 invitations to complete the online Survey Monkey questionnaire were distributed via e‐mail among the three PRCTRC institutions. A total of 321 faculty and graduate students completed the 14 TAs of the online survey in a period of four weeks. Perhaps lower response rate in online survey are due to population interest in the survey topic.16 One of the possible consequences of low response rate in this study is higher representation of participants who are interested in conducting basic, clinical and translational research; therefore, our final group of participants is not a representative sample of all faculty and graduate students in three PRCTRC institutions. However, the primary goal of our survey was to identify areas of interest among those who will benefit from PRCTRC trainings in research field in the future. Therefore, this initiative provides relevant preliminary data for the development of training activities in clinical and translational research emphasizing on faculty and graduate students’ specific needs.17
The majority of respondents were graduate students, and faculty members with assistant and associate professor academic ranks. Faculty members had research projects; either funded or nonfunded; and most graduate students were interested in becoming investigators. There were differences, often significant, in the degree of priority needs between faculty and graduate students. Among faculty there were differences in the TAs, based on academic appointment. Thus, there are training needs common to all participants, as well as specific needs depending on their academic level. Activities directed towards participants from diverse levels of research expertise, as a group, must take into consideration the specific needs of each group. It is interesting to note that although 66 participants indicated that they were not interested in becoming a researcher, they completed the whole questionnaire answering their interest for the 14 TAs. Since our main goal was to address the needs of those interested in becoming a researcher, their answers were not included in this evaluation. Nevertheless, their major area of interest coincided with TA‐1 (Identifying Major Clinical/Public Health Problems and Relevant Translational Research Questions), which was the training area most highly prioritized by faculty and graduate students. This one was followed by TA‐2: (Critique the Literature Regarding the Status of a Health Problem).
Regarding the formation of translational teams as a new model to increase the value of research to address health needs, we found that associate/assistant professors (in our institutions, usually with at least 10 years of academic experience) are significantly more interested in learning about TA‐11 Translational Teamwork, than senior faculty and graduate students. This finding is consonant with the range of candidates that are actively pursuing to become clinical and translational researchers. Another finding that denotes awareness of the importance of developing communication skills to improve health is that the only competency in a specific area that was selected by all three groups studied was found in TA‐9: Communicate clinical and translational research findings to different groups of individuals, including colleagues, students, the lay public, and the media.
Survey results have been disseminated to PRCTRC senior leadership and leadership of all key functions for use in planning training activities supported by the Consortium. Consequently, the MTCD will work with other PRCTRC Key functions leaders in planning and offering training activities from basic, to intermediary, to advanced levels in the following five TAs, which are considered essential components for any clinical research development program: TA‐1 (Identifying Major Clinical/Public Health Problems and Relevant Translational Research Questions); TA‐2 (Critique the Literature Regarding the Status of a Health Problem); TA‐3 (Designing Study Protocol for Clinical and Translational Research); TA‐4 (Study Methodology/Design/Implementation); and TA‐6 (Statistical Methods and Analysis).
The following five TAs of training needs are additional interests to the basic clinical research skills and reflect the translational transformation of research to facilitate implementation and innovation of approaches: 1) Biomedical and Health Informatics (TA‐7); 2) Scientific Communication Skills and Dissemination (TA‐9); 3) Population Diversity and Cultural Competency (TA‐10); 4) Translational Teamwork (TA‐11) and; 5) Leadership (TA‐12).
Collaborative strategies will be developed to offer training activities emphasizing the TAs described above. The MTCD will work with PRCTRC Governance, Evaluation and Collaborations & Partnerships Components, as well as local and national research resources to develop activities where researchers can update their skills through the use of technology and distance learning. One pathway that will be used is the UPR‐MSC Postdoctoral Master's Program in Clinical and Translational Research (MSc) online courses. These will serve as the platform to create conferences and workshops that can be shared with interested faculty and graduate students through the support of the PRCTRC. Specifically, the MSc currently offers the following online courses that respond to some of priority TAs identified in this study:
Scientific Communication in Clinical and Translational Research;
Introduction to Biomedical Informatics;
Health Disparities: A Translational Research Approach; and
Gender Considerations in Clinical Research.
On the other hand, it is important to mention that PRCTRC training initiatives will also provide capacity building in TAs not identified as a priority by survey participants. For example, there were four TAs that received a score of less than 50%:
Laboratory, Clinical and Population Research Methods (TA‐5);
Conducting Ethically Responsible Conduct (TA‐8);
Cross Disciplinary Training and Mentoring (TA‐13); and
Principles of Community Engagement (TA‐14).
Although these topics obtained low scores in the rankings of survey respondents, they constitute essential areas that need to continue to be developed. To plan activities in each TA, MTCD leadership will reflect on the workshop/training evaluations from previous training offerings, along with survey results, to develop appropriate training on specific competencies.
Conclusion
The NIH core and TAs and competencies in clinical and translational research are used to guide capacity building for faculty and graduate students engaged in this field of research. The results of the online Survey Monkey questionnaire provide relevant data for the development of training activities in clinical and translational research, emphasizing faculty and graduate students’ specific needs. There are training needs common to all participants, as well as specific needs depending on individual levels of expertise in research. Activities directed towards participants from diverse levels of research expertise as a group, must take into consideration the specific needs of each group. The preliminary results presented will be used in the development of capacity building activities to be offered by the PRCTRC.
The fact that the TAs went in the order of 1–14 in all questionnaires, could be considered a limiting factor in the survey being reported. This strategy could preclude the possibility of answering with enthusiasm only the first areas that appear in the questionnaire and slowly losing interest while completing the survey. As such, from 386 that accessed the questionnaire, 17% (n = 65) did not completed the questionnaire. In order to improve performance of survey, follow up activities in similar questionnaires will be managed to randomly order the TAs.
Acknowledgments
IRB Number: A9050111. This project is supported by the Puerto Rico Clinical and Translational Research Consortium (PRCTRC) U54MD007587 and the post‐Master of Science in Clinical and Translational Research (MSc) R25MD007607, both from the National Institute on Minority Health and Health Disparities (NIMHD), a component of the National Institutes of Health (NIH).
We acknowledge the statistical support of Ms. Lorena González and Dr. Sona Rivas‐Tumanyan in the revision of data analysis and presentation of results and the support of Dr. Mary Helen Mays in scientific writing. We also thank all respondents for their support in completing this study.
References
- 1. Larson EL, Begg MD. Building interdisciplinary research models: a didactic course to prepare interdisciplinary scholars and faculty. Clin Transl Sci. 2011; 4(1):38–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Estape E, Segarra B, Baez A, Huertas A, Diaz C, Frontera W. Shaping a new generation of hispanic clinical and translational researchers addressing minority health and health disparities. PR Health Sciences J. 2011; 30(4): 167–175. [PMC free article] [PubMed] [Google Scholar]
- 3. Woolf SH. The meaning of translational research and why it matters. JAMA. 2008; 299(2): 211–213. [DOI] [PubMed] [Google Scholar]
- 4. Rubio DM, Schoenbaum EE, Lee LS, Schteingart DE, Marantz PR, Anderson KE, Dewey‐Platt L, Báez A, Esposito K. Defining translational research: implications for training. Acad Med. 2010; 85 (3): 470–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Estapé ES, Rodríguez‐Orengo JF, Scott VJ. Development of multidisciplinary academic programs for clinical research education. J Allied Health. 2005; 34 (2): 55–70. [Google Scholar]
- 6. Straus SE, Brouwers M, Johnson D, Lavis JN, Légaré F, Majumdar SR, McKibbon KA, Sales AE, Stacey D, Klein G, Grimshaw J; KT Canada Strategic Training Initiative in Health Research (STIHR). Core competencies in the science and practice of knowledge translation: a description of a Canadian strategic training initiative. Implement Sci. 2011; 6: 127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Clinical and Translational Sciences Award‐ Education Core Competency Work Group . (2011, November 15). Core Competencies for Clinical and Translational Research. CTSA Home Page. Accessed November 20, 2012, from https://www.ctsacentral.org/education_and_career_development/core‐competencies‐clinical‐and‐translational‐research
- 8. Estape E, Soto de Laurido LE, Shaheen M, Quarshie A, Frontera W, Mays MH, Harrigan R, White R. A multi institutional, multidisciplinary model for developing and teaching translational research in health disparities. Clin Transl Sci. 2011; 4 (6): 434–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Awosogba T, Betancourt JR, Conyers FG, Estapé ES, Francois F, Gard SJ, Kaufman A, Lunn MR, Nivet MA, Oppenheim JD, et al. Prioritizing health disparities in medical education to improve care. Ann NY Acad. Sci. 2013; 1287(1):17–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Van de Wiel MWJ, Van den Bossche P, Jansen S, Josserger H. Exploring deliberate practice in medicine: how do physicians learn in the workplace? Adv Health Sci Educ. 2011; 16: 81–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abid K. Faculty development: a need in time for educators in healthcare. J Pak Med Assoc. 2013; 63(4):428–431. [PubMed] [Google Scholar]
- 12. Forsetlund L, Bjorndal A, Rashidian A, Jamtvedt G, O'Brien MA, Wolf F, Davis D, Odgaard‐Jensen J, Oxman AD. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2009; 2: CD003030. doi: 10.1002/14651858.CD003030.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Urquhart R, Cornelissen E, Lal S, Colquhoun H, Klein G, Richmond S, Witteman HO. A community of practice for knowledge translation trainees: an innovative approach for learning and collaboration. J Contin Educ Health Prof. 2013; 33(4):274–281. [DOI] [PubMed] [Google Scholar]
- 14. Goulda D, Kellyb D, Whitea I, Chidgeyc J. Training needs analysis: A literature review and reappraisal. Int J Nurs Stud. 2004; 41: 471–486. [DOI] [PubMed] [Google Scholar]
- 15. Bartholomew LK, Parcel GS, Kok G, Gottlieb NH, Fernández ME. 2011. Planning Health Promotion Programs: An Intervention Mapping Approach. 3rd edn. San Francisco, CA: Jossey‐Bass. [Google Scholar]
- 16. Archer TM. Characteristics Associated with Increasing the Response Rates of Web‐Based Surveys. Practical Assessment Research & Evaluation, 2007; 12(12). Available online: http://pareonline.net/getvn.asp?v=12&n=12. Accessed December 12, 2013. [Google Scholar]
- 17. Cook C, Heath F, Thompson R. A meta‐analysis of response rates in web or Internet‐based surveys. Educ Psychol Measur., 2000; 60, 821–836. [Google Scholar]


