Abstract
The objective was to evaluate 2 primary molar sealant strategies for publicly insured children using an “expected value of perfect information” (EVPI) approach. We converted a 10,000-observation tooth-level cost-effectiveness simulation model comparing 2 primary molar sealant strategies – always seal (AS) and standard care (SC) – with a 1,250-observation child-level model. Costs per child per restoration or extraction averted were estimated. Opportunity losses under the AS strategy were determined for children for whom SC was the optimal choice. We determined the EVPI by multiplying mean opportunity losses by the projected incident population of publicly insured 3-year-olds in the US over 10 years with costs discounted at 2%. All analyses were conducted under assumptions of high and low intrachild correlations between at-risk teeth. The AS strategy cost $43.68 over SC (95% CI: −$5.50, $92.86) per child per restoration or extraction averted under the high intrachild correlation assumption and $15.54 (95% CI $7.86, $23.20) under the low intrachild correlation. Under high intrachild correlation, mean opportunity losses were $80.28 (95% CI: $76.39, $84.17) per child, and AS was the optimal strategy in 31% of children. Under low correlation, mean opportunity losses were $14.61 (95% CI: $12.20, $17.68) and AS was the optimal strategy in 87% of children. The EVPI was calculated at $530,813,740 and $96,578,389 (for high and low intrachild correlation, respectively), for a projected total incident population of 8,059,712 children. On average, always sealing primary molars is more effective than standard care, but widespread implementation of this preventive approach among publicly insured children would result in large opportunity losses. Additional research is needed to identify the subgroups of publicly insured children who would benefit the most from this effective and potentially cost-saving public health intervention.
Keywords: expected value of perfect information, sealants, Medicaid, cost-effectiveness, health economics, health policy
Introduction
Early childhood caries (ECC) rates in the US have increased significantly in the past 3 decades (Dye et al., 2007). Children from poor households are twice as likely to have untreated dental caries as children from higher income households (Dye et al., 2010). Furthermore, Medicaid-enrolled children are significantly more likely to have untreated caries than other children (Brickhouse et al., 2008). These factors have motivated efforts to address the ECC epidemic in socio-economically vulnerable children, in part, by ensuring access to preventive dental care.
The US Healthy People 2020 goals include increasing from 1.4% to 1.5% the proportion of children ages 3 to 5 years with a sealed primary molar (US DHHS, Healthy People 2020). Consistent with this goal, the American Academy of Pediatric Dentistry (AAPD) recommends pit-and-fissure sealants as part of a comprehensive caries prevention strategy for children age 3 years and older (AAPD, 2013). There is strong evidence that sealants prevent dental caries in permanent molars (Ahouvuo-Saloranta et al., 2013). However, consistent with caries prevalence rates, only half as many low-income children receive sealants as their higher income peers (Dye et al., 2007). Previous studies have identified the enablers and barriers to preventive dental care services for publicly insured children (Chi and Milgrom, 2009; Chi et al., 2010; Rozier et al., 2010; Askelson et al., 2014). Only 1-in-3 state Medicaid programs reimburses dentists for primary molar sealants (Chi and Singh, 2013), which is a potential barrier to the receipt of sealants for low-income children.
Most health economic studies to date on pit-and-fissure sealants for low-income children focus on permanent teeth (Weintraub et al., 2001; Bhuridej et al., 2005, 2007). The only published study on primary molar sealants presented a tooth-level model simulating outcomes associated with different sealant strategies (standard care, never sealing, and always sealing primary molars) in a pediatric Medicaid population (Chi et al., 2014). The always seal strategy was, on average, more costly than standard care, but resulted in fewer subsequent restorations and extractions. However, contrary to a risk-based clinical approach endorsed by the AAPD, always sealing does not account for heterogeneity in caries risk within the pediatric Medicaid population. In other words, some children in Medicaid whose primary molars are sealed would not receive additional health benefits from sealants because they are at lower risk for caries. There are gaps in the dental health services literature regarding optimization of preventive strategies.
“Expected value of perfect information” (EVPI) methods from health economics provide an analytic framework for assessing whether clinical approaches, such as always sealing primary molars, should be widely adopted or if more research is needed before a decision to adopt is made by policymakers and clinicians (Claxton, 1999a). We conducted an EVPI study to achieve 2 goals: (1) to develop a population-level model that examines the opportunity losses associated with always sealing primary molars; and (2) to estimate the EVPI that would result from perfect selection of publicly insured children to receive primary molar sealants. This study is the first step in assessing the need for additional empirical research on primary molar sealants.
Materials & Methods
Study Design
We developed model-based, child-level economic simulation models from the public payer perspective using claims data from the Iowa Medicaid program and the published literature. The University of Iowa Institutional Review Board approved this study.
Characteristics of Study Population
Iowa Medicaid dental is a traditional fee-for-service program. In 2012, the program enrolled 286,400 children under age 18 years (unpublished observations). Income eligibility criterion is 375% Federal Poverty Level (FPL) for children under age 12 months and 167% FPL for children ages 12 months to 17 years (Centers for Medicare and Medicaid, 2014). Dental benefits include preventive care (e.g., examinations, prophylaxis, topical fluoride, pit-and-fissure sealants) and restorative care (e.g., restorations, crowns, extractions). In 2006, 56.3% of children in the Iowa Medicaid program utilized dental care (Chi et al., 2011). Iowa Medicaid began reimbursing dentists in February 2008 for primary molar sealants for enrollees through age 18 years (Iowa Department of Human Services, 2008). The Medicaid reimbursement rate in Iowa is in the bottom quartile among the 16 Medicaid programs that reimburse for primary molar sealants (Chi and Singh, 2013).
Child-level Cost-effectiveness Model
The first step in determining the EVPI for primary molar sealants is to convert a tooth-level model into a child-level cost-effectiveness model (Fig.) (Claxton, 1999b). A previous study presented a tooth-level cost-effectiveness model based on a Monte Carlo simulation with 10,000 primary molars and compared 3 strategies: standard care (SC), always seal (AS), and never seal (NS) (Chi et al., 2014). The model parameters and assumptions are provided in the Appendix. Standard care (SC) was based on the Iowa Medicaid claims data, which indicated that 11% of children received at least 1 primary molar sealant. Always seal was the preferred strategy that maximizes effectiveness (i.e., prevents restorations or extractions) while incurring some cost. For the current child-level model, we compared AS and SC. We adopted non-parametric methods, which account for multiple sources of data each with different underlying distributions (Briggs et al., 2008). Primary molar costs and outcomes for AS and SC were summed for each child-level observation. Mean incremental costs and mean number of restorations or extractions averted were determined at the child-level for the lifetime of each simulated primary molar. The incremental cost-effectiveness ratio (ICER) was calculated as the difference in costs (AS minus SC) divided by the difference in restorations and extractions (SC minus AS).
Figure.
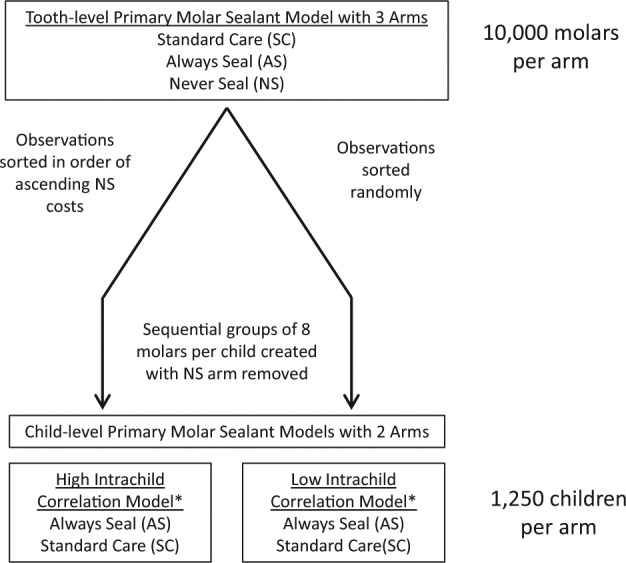
Conversion of tooth-level primary molar sealant cost-effectiveness model to child-level model primary molar sealant cost-effectiveness model. *The high intrachild correlation model was built from tooth-level observations sorted by ascending costs of the “never sealed” (NS) arm. The low intrachild correlation model was built by random sorting of tooth-level observations. Non-overlapping sequential groups of 8 molars corresponded to a total of 1,250 children in both the high and low intrachild correlation models.
The costs per child per restoration and extraction averted were calculated under both high and low intrachild correlation assumptions (see Data Analyses section below).
Child-level Opportunity Losses
We defined the optimal strategy for each child as the strategy resulting in fewer restorations or extractions or, if these were equal, the lower cost strategy. An opportunity loss was incurred when AS was not the optimal strategy for a child in the child-level model. We calculated the mean opportunity losses, corresponding to the losses that could be averted if we had perfect information based on which children should receive sealants under SC. These losses are also known as the EVPI at the child-level (EVPIchild). We further calculated the mean cost difference stratified by the optimal strategy to demonstrate the effect of optimal strategy selection on cost.
Population-level EVPI
The EVPIpopulation is the child-level EVPI (EVPIchild) multiplied by the incident population (I) summed for the anticipated lifetime usefulness of the intervention, when the intervention will be assumed to be useful (T), modified by a discount rate (r), compounded over time (t).
The incident population (I) is the number of children enrolled in Medicaid or the State Children’s Health Insurance Plan (SCHIP) with newly erupted primary molars. Although the study by Chi and colleagues (2014) focused solely on children in Medicaid, in the current study we assumed that children enrolled in SCHIP would also benefit similarly from policies involving reimbursement for primary molar sealants. We assumed that if the results of the cost-effectiveness analysis previously described were applied universally, this would happen at age 3 years, the age at which sealants could reasonably be placed on primary molars by a dentist, and the effects would last until the primary molars exfoliated. Thus, the time horizon was 8.5 years post-eruption or until age 11.5 years. We used Medical Expenditure Panel Survey (MEPS) data (calendar years 2002 to 2011) from the Agency for Healthcare Research and Quality to determine the yearly proportion of Medicaid- or SCHIP-enrolled children with a dental visit at age 3 years. We used the mean annual growth rate to extrapolate to a population beginning in 2015 using a linear prediction model, with the last cohort ending in 2024, resulting in 10 cohorts of 3-year-old Medicaid/SCHIP enrollees (Cohen, 1997; Selden, 2009).
We assumed the lifetime usefulness of the technology (T) at 10 years. The evaluation of a decade of usefulness is reasonable from a policymaker standpoint (Claxton et al., 2002). We used a discount rate (r) of 2%, which reflects the mean rate of return on a relatively safe investment. Discounting is common in economic analyses and is based on 2 premises: (1) that the current value of a good or service is likely to deteriorate over time; and (2) that individuals prefer present over future consumption of goods, the latter of which has less value. All costs are reported in 2012 US dollars, corresponding to the most recent year for which model parameter data were available.
Data Analyses
In converting a tooth-level model to a child-level model (Fig.), we evaluated 2 types of intrachild correlation: (1) high (intraclass correlation coefficient = 0.99); and (2) low (intraclass correlation coefficient = 0.00). In the high correlation model, healthy, restored, and extracted molars are assumed to cluster within individual children, an assumption supported by previous research (Stephenson et al., 2010). Observations from the NS strategy in the tooth-level model were sorted on ascending restoration and extraction costs, representing a natural history of the tooth in the absence of sealants. The sorted observations were divided into groups of 8 molars to form child-level observations. In the low correlation model, we performed a random sort of tooth-level observations to approximate a random distribution of healthy, restored, and extracted molars across children. Each correlation model included a total of 1,250 children with 8 primary molars at time 0. All analyses were completed with STATA 11.0 (StataCorp, College Station, TX, USA).
Results
Child-level Cost-effectiveness Model
Compared with standard care (SC), the mean difference in cost per child of always sealing (AS) primary molars was $13.52 (95% confidence interval [CI]: –$1.03, $28.08), and the mean number of restorations or extractions averted under the AS strategy was 1.81 per child (95% CI: 1.65, 1.96), corresponding to an ICER of $7.49 per restoration or extraction averted (95% CI: $2.85, 12.12) (Table 1). Under high intrachild correlation, the cost per child per restoration or extraction averted was $43.68 (95% CI: –$5.50, $92.86) compared with $15.54 (95% CI: $7.86, $23.20) per child per restoration or extraction averted under the low correlation assumption.
Table 1.
Child-level Cost-effectiveness Model Results with Mean Costs (US$, 2012), Mean Numbers of Restorations or Extractions Averted, and Incremental Cost-effectiveness Ratios under High and Low Intrachild Correlation Assumptions
| Mean Cost, 2012 US$ | Mean Numbers of Restorations and Extractions Averted | |
|---|---|---|
| Always Seal (AS) | $182.47 | 0.28 |
| Standard Care (SC) | $168.95 | 2.08 |
| Difference (AS-SC) | $13.52 (95% CI: –$1.03, $28.08) |
−1.81* (95% CI: −1.96, −1.65) |
| ICER [(CostsAS-CostsSC)/(Restorations + ExtractionsSC – Restorations + ExtractionsAS)] | $7.49 (95% CI: $2.85, $12.12) |
|
| Cost per Child for Restorations or Extractions Averted Associated with AS Strategy (High Intrachild Correlation Assumption) | $43.68 (95% CI: −$5.50, $92.86) |
|
| Cost per Child for Restorations or Extractions Averted Associated with AS Strategy (Low Intrachild Correlation Assumption) | $15.54 (95% CI: $7.86, $23.20) |
|
AS = Always Seal; SC = Standard Care; ICER = Incremental Cost-effectiveness Ratio; CI = Confidence Interval.
A negative difference in the mean number of restorations or extractions averted indicates that the Always Seal strategy avoids a greater number of restorations and extractions than Standard Care.
Child-level Opportunity Losses Associated with Imperfect Information
Under the assumption of high intrachild correlation, the mean opportunity loss was $80.28 per child (95% CI: $76.39, $84.17) (Table 2). AS was not the optimal strategy in 69% of children. The mean opportunity loss for the AS strategy for these children was $116.29 (95% CI: $112.67, $119.90). For children who had at least 1 restoration or extraction under SC, AS would save $215.63 per child (95% CI: –$252.90, –$178.36). Under the assumption of low intrachild correlation, the mean opportunity loss was $14.61 (95% CI: $12.20, $17.18). AS was not the optimal strategy in 13% of children. The mean opportunity loss for the AS strategy for these children was $112.71 (95% CI: $103.66, $121.76), while the strategy was cost-saving at the mean for children experiencing at least 1 restoration or extraction under standard care (mean opportunity loss: –$1.25; 95% CI: –$8.27, $5.78)
Table 2.
Child-level Opportunity Loss and under High and Low Intrachild Correlation Assumptions for 1,250 Child Simulations
| Mean Opportunity Loss per Child | 95% Confidence Interval | Percentage of Children for whom AS is Optimal Strategy* | 95% Confidence Interval | Mean Opportunity Loss per Child if SC Optimal* | 95% Confidence Interval | Mean Opportunity Loss per Child if AS Optimal* | 95% Confidence Interval | |
|---|---|---|---|---|---|---|---|---|
| High intrachild correlation | $80.28 | $76.39, $84.17 | 31% | 28%, 34% | $116.29 | $112.67, $119.90 | −$215.63 | −$252.90, −$178.36 |
| Low intrachild correlation | $14.61 | $12.20, $17.18 | 87% | 85%, 89% | $112.71 | $103.66, $121.76 | −$1.25 | −$8.27, $5.78 |
AS = Always Seal; SC = Standard Care.
Optimal strategy defined as the strategy for each observation that averts the highest number of restorations or extractions (i.e., is most effective) or, with equal effectiveness, costs the least.
Population-level EVPI
Based on MEPS data, the proportion of Medicaid-/SCHIP-enrolled children with a dental visit by age 3 years increased by 6.6% per year from 2002 to 2011. This corresponds to an incident population of 674,925 and 937,017 3-year-olds in 2015 and 2025, respectively, or a total of 8,059,712 3-year-olds during the 10-year-period who would be projected to utilize dental care and receive primary molar sealants (Table 3). Under the assumption of high intra-child correlation, the population-level EVPI for our population of interest is $530,813,740 (95% CI: $505,100,100, $556,527,400) (data not shown). Under the low intrachild correlation assumption, the population-level EVPI is $96,578,389 ($80,682,410, $112,474,400).
Table 3.
Annual Predicted Incident Population of Publicly Insured 3-year-old Children in the USA for Estimation of Population-level Expected Value of Perfect Information
| Year | Number of Publicly Insured 3-year-old Children with an Annual Dental Visit* | Predicted Incident Population (I) |
|---|---|---|
| 2002 | 307,159 | 296,348 |
| 2003 | 312,349 | 325,469 |
| 2004 | 383,386 | 354,591 |
| 2005 | 447,786 | 383,712 |
| 2006 | 399,793 | 412,833 |
| 2007 | 342,753 | 441,955 |
| 2008 | 411,122 | 471,076 |
| 2009 | 556,098 | 500,197 |
| 2010 | 481,031 | 529,319 |
| 2011 | 632,461 | 558,440 |
| 2012 | – | 587,561 |
| 2013 | – | 616,683 |
| 2014 | – | 645,804 |
| 2015 | – | 674,925 |
| 2016 | – | 704,047 |
| 2017 | – | 733,168 |
| 2018 | – | 762,289 |
| 2019 | – | 791,411 |
| 2020 | – | 820,532 |
| 2021 | – | 849,653 |
| 2022 | – | 878,775 |
| 2023 | – | 907,896 |
| 2024 | – | 937,017 |
| Sum, Predicted Incident Population, 2015-2024 (IT) | 8,059,712 | |
Based on data from the Medical Expenditure Panel Survey (MEPS) Consolidated Files (2002-2011) for 3-year-old children with at least 1 annual dental visit paid for by Medicaid or SCHIP. Person-level weights were used to derive nationally representative point estimates. Predictions are for univariate linear regression of year on annual totals for 2002-2011, followed by predictions for years 2012-2024.
Discussion
Expected value of perfect information studies enable researchers and policymakers to determine if additional research is required to evaluate the cost-effectiveness of a given health intervention. This is the first known publication that adopted EVPI methods to evaluate 2 primary molar sealant strategies (always sealing vs. standard care). We had 2 goals: (1) to estimate the opportunity losses associated with always sealing primary molars of publicly insured children; and (2) to assess the EVPI associated with perfect selection of children to receive primary molars sealants. Our main findings are summarized below.
First, opportunity losses are incurred under the strategy of always sealing primary molars. In a previous study, it was shown that always sealing primary molars had the greatest likelihood of preventing restorations and extractions (Chi et al., 2014). Although the always seal strategy was not cost-saving over the lifetime of the primary molar, the mean differences in restorations and extractions averted compared with standard care were substantial and significant. Collectively, these findings suggest that opportunity losses could be reduced, thereby optimizing the cost-effectiveness of a primary molar sealant strategy by ensuring that only high-risk children receive sealants. This approach is consistent with a risk-based disease prevention strategy (Gao et al., 2013) and results of previous cost-effectiveness studies on permanent molar sealants (Weintraub, 2001; Bhuridej et al., 2007). While various caries risk assessment tools are available (Ramos-Gomez and Ng, 2011; Campus et al., 2012; AAPD, 2013), none has been used in the context of cost-effectiveness evaluations of preventive care for children. Future studies should continue to identify the risk factors for caries in young publicly insured children and assess the specificity and sensitivity of risk factors so that primary molar sealant strategies can be optimized.
Furthermore, we estimated that the mean opportunity losses for children who would fare no better under always sealing than standard care are similar in both high- and low-correlation assumptions ($116 and $112, respectively). A possible explanation is that, under the assumption of high intrachild correlation of at-risk teeth, restorations and extractions occurring under standard care are concentrated in fewer children, while the majority of children would have the same outcome regardless of a primary molar sealant intervention. For children who benefit from sealants, the magnitude of benefit is greater, resulting in larger cost savings (i.e., more teeth per child are spared the costs associated with restorations or extractions). In contrast, the assumption of low intrachild correlation results in a greater likelihood that an individual child benefits from the sealant intervention, thereby reducing opportunity losses, but minimizing the magnitude of benefit of the always seal strategy over standard care at the child-level. Collectively, the importance of these findings is that the opportunity losses are greater when high intrachild correlation is assumed, but are substantial regardless of the type of correlation assumed. The higher the intrachild correlation of restorations and extractions under standard care, the greater the opportunity losses that occur from blanket implementation of an always seal strategy, but the cost savings for those children who benefit from always seal is also greater. Improved selection of children whose primary molars should be sealed based on risk factors would minimize opportunity losses and maximize cost savings.
Second, the EVPI associated with primary molar sealants for publicly insured 3-year-olds in the US ranges from $100 to $500 million, depending on the level of correlation assumed. Our estimated EVPIs correspond to 1.1% to 10% of the total US child Medicaid/SCHIP dental expenditures (Wall and Brown, 2008; Wall, 2012) and are similar in magnitude to the EVPI estimated for oral cancer screening programs in the United Kingdom (Speight et al., 2006). These findings highlight the importance of additional research on primary molar sealants to identify children who would benefit most from sealants (e.g., children with special health care needs), which would allow for the development of empirical clinical guidelines on primary molar sealant indications.
Our study has important implications for clinical practice and future research. Generating perfect information to help dentists and other dental health professionals select appropriate, high-risk children to receive primary molar sealants would maximize the benefits of sealants by reducing dental disease and need for invasive treatment. Additional research to improve selection of high-risk children would also lead to substantial cost savings. For instance, a $1 million study yielding information that improved the optimal sealant strategy selection by 10% (i.e., increasing the proportion of children for whom always sealing is optimal from 31% to 34% under high intrachild correlation) would reduce opportunity losses by $23 million. If a random distribution of molars without intrachild correlation is assumed, a 5% improvement in optimal strategy selection (from 87% to 91%) would save over $29 million in opportunity losses. These estimates suggest substantial clinical and economic value associated with additional research on ways to improve primary molar sealant strategies. These methods are likely to be applicable to assessments of patient-tailored delivery of other forms of preventive dental care, including dental examinations and recall periodicity, cleanings, and topical fluoride treatment.
Our study had 4 main limitations. First, it was based on a prior model of cost-effectiveness of 3 sealant strategies. Although that model was based on the best available evidence, any misspecification of parameters would affect the results of the EVPI model presented. Second, our population estimates were conservative and may have underestimated the population at risk. State Medicaid expansion under the Affordable Care Act will result in increased enrollment of children, which is likely to result in increased used of dental care by Medicaid-insured children. However, our model accounted for growth in the number of 3-year-olds in Medicaid/SCHIP with an annual dental visit using a linear prediction model from nationally representative data. A major policy decision by states to reimburse dentists for primary molar sealants may create greater demand for the procedure, increasing the number of children receiving primary sealants. The net effect of a larger incident population would be a larger EVPI, which further supports research to refine patient selection strategies. Third, the conversion of a tooth-level model to a child-level model assumes either that teeth requiring restorations or extractions in the absence of sealants segregate together or that at-risk molars cluster randomly. These 2 approaches represent extremes of perfect or near-perfect intrachild correlation. Although our estimated population-level EVPIs differ substantially between these 2 correlation extremes, either approach suggests that better selection of sealant candidates would be cost-saving. Fourth, we assumed continuous enrollment of children in Medicaid/CHIP. Future models should consider accounting for the complexity of enrollment lapses, which may have implications for assessing costs and outcomes from the public payer perspective.
Supplementary Material
Footnotes
A supplemental appendix to this article is published electronically only at http://jdr.sagepub.com/supplemental.
This study was funded by the National Institute of Dental and Craniofacial Research (NIDCR), Grant No. K08DE020856, and by the William T. Grant Foundation Scholar Program.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- AAPD Council on Clinical Affairs (2013). Guideline on caries-risk assessment and management for infants, children, and adolescents. Pediatr Dent 35:E157-E164. [PubMed] [Google Scholar]
- Ahovuo-Saloranta A, Forss H, Walsh T, Hiiri A, Nordblad A, Mäkelä M, et al. (2013). Sealants for preventing dental decay in the permanent teeth. Cochrane Database Syst Rev 3:CD001830. [DOI] [PubMed] [Google Scholar]
- Askelson NM, Chi DL, Momany E, Kuthy R, Ortiz C, Hanson JD, et al. (2014). Encouraging early preventive dental visits for preschool-aged children enrolled in Medicaid: using the Extended Parallel Process Model to conduct formative research. J Public Health Dent 74:64-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhuridej P, Damiano PC, Kuthy RA, Flach SD, Kanellis MJ, Heller KE, et al. (2005). Natural history of treatment outcomes of permanent first molars: a study of sealant effectiveness. J Am Dent Assoc 136:1265-1272. [DOI] [PubMed] [Google Scholar]
- Bhuridej P, Kuthy RA, Flach SD, Heller KE, Dawson DV, Kanellis MJ, et al. (2007). Four-year cost-utility analyses of sealed and nonsealed first permanent molars in Iowa Medicaid-enrolled children. J Public Health Dent 67:191-198. [DOI] [PubMed] [Google Scholar]
- Brickhouse TH, Rozier RG, Slade GD. (2008). Effects of enrollment in Medicaid versus the state children’s health insurance program on kindergarten children’s untreated dental caries. Am J Public Health 98:876-881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs A, Claxton K, Sculpher M. (2008). Decision modelling for health care evaluation. New York, NY: Oxford University Press. [Google Scholar]
- Campus G, Cagetti MG, Sale S, Carta G, Lingström P. (2012). Cariogram validity in schoolchildren: a two-year follow-up study. Caries Res 46:16-22. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid (2014). Medicaid/CHIP MAGI Eligibility Levels by FPL. URL accessed on 6/30/2014 at: http://www.medicaid.gov/AffordableCareAct/Medicaid-Moving-Forward-2014/Downloads/Medicaid-and-CHIP-Eligibility-Levels-Table.pdf.
- Chi D, Milgrom P. (2009). Preventive dental service utilization for Medicaid-enrolled children in New Hampshire: a comparison of care provided by pediatric dentists and general dentists. J Health Care Poor Underserved 20:458-472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi DL, Singh J. (2013). Reimbursement rates and policies for primary molar pit-and-fissure sealants across state Medicaid programs. J Am Dent Assoc 144:1272-1278. [DOI] [PubMed] [Google Scholar]
- Chi DL, Momany ET, Kuthy RA, Chalmers JM, Damiano PC. (2010). Preventive dental utilization for Medicaid-enrolled children in Iowa identified with intellectual and/or developmental disability. J Public Health Dent 70:35-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi DL, Momany ET, Neff J, Jones MP, Warren JJ, Slayton RL, et al. (2011). Impact of chronic condition status and severity on dental utilization for Iowa Medicaid-enrolled children. Med Care 49:180-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi DL, van der Goes D, Ney JP. (2014). Cost-effectiveness of pit-and-fissure sealants on primary molars in Medicaid-enrolled children. Am J Public Health 104:555-561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claxton K. (1999a). Bayesian approaches to the value of information: implications for the regulation of new pharmaceuticals. Health Econ 8:269-274. [DOI] [PubMed] [Google Scholar]
- Claxton K. (1999b). The irrelevance of inference: a decision-making approach to the stochastic evaluation of health care technologies. J Health Econ 18:341-364. [DOI] [PubMed] [Google Scholar]
- Claxton K, Sculpher M, Drummond M. (2002). A rational framework for decision making by the National Institute for Clinical Excellence (NICE). Lancet 360:711-715. [DOI] [PubMed] [Google Scholar]
- Cohen S. (1997). Sample design of the 1996 Medical Expenditure Panel Survey Household Component. Vol. 2 Rockville, MD: Agency for Healthcare Research and Quality. [Google Scholar]
- Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, et al. (2007). Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat 11 248: 1-92. [PubMed] [Google Scholar]
- Dye BA, Arevalo O, Vargas CM. (2010). Trends in paediatric dental caries by poverty status in the United States, 1988-1994 and 1999-2004. Int J Paediatr Dent 20:132-143. [DOI] [PubMed] [Google Scholar]
- Gao X, Di Wu I, Lo EC, Chu CH, Hsu CY, Wong MC. (2013). Validity of caries risk assessment programmes in preschool children. J Dent 41:787-795. [DOI] [PubMed] [Google Scholar]
- Iowa Department of Human Services (2008). Iowa Medicaid enterprise documents. Informational letter no. 675: sealants, root canal retreatments and implants. URL accessed on 6/30/2014 at: http://www.ime.state.ia.us/docs/675_RulesChange.pdf.
- Ramos-Gomez F, Ng MW. (2011). Into the future: keeping healthy teeth caries free: pediatric CAMBRA protocols. J Calif Dent Assoc 39:723-733. [PMC free article] [PubMed] [Google Scholar]
- Rozier RG, Stearns SC, Pahel BT, Quinonez RB, Park J. (2010). How a North Carolina program boosted preventive oral health services for low-income children. Health Aff (Millwood) 29:2278-2285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selden T. (2009). Using adjusted MEPS data to study incidence of health care finance. Paper presented at: AHRQ Annual Conference, Bethesda, MD URL accessed on 6/30/2014 at: http://www.ahrq.gov/news/events/conference/2009/selden/index.html. [Google Scholar]
- Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, et al. (2006). The cost-effectiveness of screening for oral cancer in primary care. Health Technol Assess 10:1-144, iii-iv. [DOI] [PubMed] [Google Scholar]
- Stephenson J, Chadwick BL, Playle RA, Treasure ET. (2010). Modelling childhood caries using parametric competing risks survival analysis methods for clustered data. Caries Res 44:69-80. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services. Healthy People 2020. Oral Health Objectives. URL accessed on 6/30/2014 at: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=32.
- Wall TP. (2012). Dental Medicaid – 2012. Dental Health Policy Analysis Series. Chicago, IL: American Dental Association, Health Policy Resources Center. [Google Scholar]
- Wall TP, Brown LJ. (2008). Public dental expenditures and dental visits among children in the U.S., 1996-2004. Public Health Rep 123:636-645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weintraub JA. (2001). Pit and fissure sealants in high-caries-risk individuals. J Dent Educ 65:1084-1090. [PubMed] [Google Scholar]
- Weintraub JA, Stearns SC, Rozier RG, Huang CC. (2001). Treatment outcomes and costs of dental sealants among children enrolled in Medicaid. Am J Public Health 91:1877-1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


