Abstract
Background
Little is known about factors influencing professionals’ use of wikis.
Objective
We developed and validated two questionnaires to assess health care professionals’ intention to use wiki-based reminders for the management of trauma patients.
Methods
We developed questionnaires for emergency physicians (EPs) and allied health professions (AHPs) based on the Theory of Planned Behavior and adapted them to the salient beliefs of each, identified in an earlier study. Items measured demographics and direct and indirect theoretical constructs. We piloted the questionnaires with 2 focus groups (5 EPs and 5 AHPs) to identify problems of wording and length. Based on feedback, we adjusted the wording and combined certain items. A new convenience sample of 25 EPs and 26 AHPs then performed a test-retest of the questionnaires at a 2-week interval. We assessed internal consistency using Cronbach alpha coefficients and temporal stability of items with an agreement intraclass correlation coefficient (ICC).
Results
Five EPs and 5 AHPs (3 nurses, 1 respiratory therapist, and 1 pharmacist) formed 2 focus groups; 25 EPs and 26 AHPs (12 nurses, 7 respiratory therapists, and 7 pharmacists) completed the test and retest. The EP questionnaire test-retest scores for consistency (Cronbach alpha) and stability (ICC) were intention (test: Cronbach alpha=.94; retest: Cronbach alpha=.98; ICC=.89), attitude (.74, .72, .70), subjective norm (.79, .78, .75), perceived behavioral control (.67, .65, .66), attitudinal beliefs (.94, .86, .60), normative beliefs (.83, .87, .79), and control beliefs barriers (.58, .67, .78) and facilitators (.97, .85, .30). The AHP questionnaire scores for consistency and stability were: intention (test Cronbach alpha=.69, retest Cronbach alpha=.81, ICC=.48), attitude (.85, .87, .83), subjective norm (.47, .82, .62), perceived behavioral control (.55, .62, .60), attitudinal beliefs (.92, .91, .82), normative beliefs (.85, .90, .74), and control beliefs barriers (.58, .55, .66) and facilitators (.72, .94, –.05). To improve the psychometric properties of both questionnaires, we reformulated poorly consistent or unstable items.
Conclusions
Our new theory-based questionnaires to measure health care professionals’ intention to use wiki-based reminders have adequate validity and reliability for use in large surveys. In the long run, they can be used to develop a theory-based implementation intervention for a wiki promoting best practices in trauma care.
Keywords: knowledge translation, wiki, collaborative writing applications, decision support tools, health informatics, Theory of Planned Behavior, trauma care, traumatic brain injury, interprofessional collaboration
Introduction
Clinical practice does not always reflect best evidence. High proportions of inappropriate care have been reported in different health care systems and settings [1]. This has a huge impact on both patient outcomes and health care costs. As passive dissemination of evidence has not proven adequate for encouraging implementation of research-based recommendations for changes in practice, new strategies are being advocated [2].
Information and communication technologies (ICTs) such as computerized decision support systems have been suggested as a possible solution for improving research uptake and increasing evidence-based practice [3]. Aiming to improve care and reduce costs, governments have invested billions of dollars to implement ICTs, including decision support systems, but these systems have yet to deliver the expected benefits [4]. Moreover, some health care professionals have rejected ICTs on the grounds that they are slow, incompatible with work processes, difficult to access, costly to implement, and cannot be adapted to local practices [4-10]. Furthermore, local initiatives to adapt various ICT solutions seem to be restricted to a small number of hospitals and tools are mostly designed for local use only [11-13]. Transfer of these local initiatives to the larger health care community is often slow and complex. In emergency departments (EDs), where shift work is prevalent, getting health care professionals to collaborate in creating, using, and updating decision support tools (eg, care protocols, care pathways, and decision aids) is particularly difficult [14]. These decision support tools can be translated into paper-based or computer-based reminders that support clinicians’ or patients’ decision making at the bedside. The most important factors influencing the creation, use, and updating of any form of reminders to promote best practices may be time and collaboration within and across care teams [15,16]. Wikis are an open-source and low-cost means of accelerating innovation and permitting a broad spectrum of stakeholders to collaborate efficiently for this purpose.
Wikis are knowledge management platforms that empower stakeholders to implement evidence-based decision support tools in different areas of health care [17]. A wiki is a website that uses a novel technology to allow people to view and edit website content, with viewing and editing privileges determined by various levels of access. Wikipedia—the best-known wiki—has 365 million visitors per month, is the sixth most popular website in the world, and its medical articles (available in 271 languages) are viewed approximately 150 million times per month [18]. Many health organizations have started using wikis to manage knowledge and coordinate care [19-23]. A recent scoping review found that wikis are effective educational interventions for health students and professionals and that they have many positive impacts on knowledge translation processes and outcomes: theoretical behavioral change domains (eg, beliefs about capabilities), learning (eg, skills and knowledge), communication, collaboration, knowledge management, health care efficiency, quality improvement, and disease prevention [17].
A wiki could permit stakeholders in 1 or many EDs to collaborate asynchronously in the updating and creation of reminders, decreasing duplication efforts and reducing the time needed. However, despite increasing evidence supporting the use of wikis in various settings, there is a lack of knowledge about the factors influencing professionals’ use of wikis and about how best to implement them in health care settings [24,25].
The objectives of this study were to develop and test the psychometric properties of 2 questionnaires based on the Theory of Planned Behavior (TPB) [26] exploring the intention of ED health care professionals and the determinants of this intention to use wiki-based reminders promoting best practices for the management of severe traumatic brain injury (TBI) victims.
Methods
Study Design
The protocol for this mixed methods study describes 4 phases [27]: (1) eliciting salient beliefs [25], (2) developing the questionnaires, (3) piloting the questionnaires, and (4) test-retest of the adjusted questionnaires. Phase 1 of this project identified ED professionals’ salient beliefs concerning the use of wiki-based reminders promoting best practices for the management of severe TBI [25]. The current study represents the later phases (2, 3, and 4) of the published research protocol [27]. Our participants, emergency physicians (EPs) and allied health professionals (AHPs), came from 3 hospitals of 3 different trauma levels (I, II, and III) in the province of Quebec, Canada. All our participants were French speaking. The ethics committees from the 3 hospitals approved this study and there were no financial incentives offered to participants.
Definition of the Behavior for the Present Survey
We chose to study the intention (and determinants of intention) of ED health care professionals to use a wiki-based reminder promoting best practices for the management of severe TBI victims in the ED in the Province of Quebec, Canada. Definition of the behavior was:
Action: to use
Target: a wiki-based reminder promoting best practice
Context: management of severe TBI victims in EDs in the province of Quebec, Canada
Phase 1: Elicitation of Salient Beliefs
A complete report of Phase 1 of our study has been published [25]. In summary, we conducted semistructured interviews to elicit EPs’ and AHPs’ beliefs about using a wiki-based reminder. In order to clearly depict the behavior being studied, 4 videos were created presenting 4 different health care professionals (emergency physician, nurse, respiratory therapist, and pharmacist) performing the behavior (see Multimedia Appendix 1 to access the YouTube videos in French). After watching the video specific to their profession, each participant was interviewed about their behavioral, control, and normative beliefs (ie, what they saw as advantages, disadvantages, barriers, and facilitators to their use of a wiki-based reminder) and how they felt important referents would perceive their use of a wiki-based reminder. After ranking each belief from the most reported to the least reported, we considered the top 75% most-reported beliefs as salient. We also retained certain beliefs as salient although they were not among the top 75% most reported. This decision was based on our knowledge of the literature, our experience in implementing care protocols for trauma, or our fear of excluding important negative beliefs. This study generated 2 different sets of salient beliefs for EPs and AHPs that were used to construct 2 different questionnaires.
Phase 2: Questionnaire Development
Direct Construct Items
In both questionnaires, we included items to measure the constructs identified in our theoretical model: intention (n=3), perceived behavioral control (n=3), attitude (n=4), and subjective norm (n=3). The items were formulated so that participants could then evaluate their level of agreement with each statement on a 7-point Likert scale.
Indirect Construct Items
We selected the salient behavioral, normative, and control beliefs identified in our published Phase I and converted these into a set of statements for each questionnaire. The items were formulated so that participants could evaluate their level of agreement on a 7-point Likert scale about each advantage, disadvantage, positive referent, negative referent, barrier, and facilitator presented.
Characteristics of Health Care Professionals
We assessed the following demographic characteristics: age, gender, type of health care professional, and diploma (AHP questionnaire), training level of EPs (EP questionnaire), type of health care center (level I, II, III), number of years in practice, presence of computers with unrestricted access to the Internet within their ED, availability of Wi-Fi for professionals, availability of Wi-Fi for patients, previous consultation of or contribution to a wiki, and membership in local trauma committees.
Ordering of Questions in the Questionnaires
The drafts of our initial questionnaires were created without randomly mixing the items and in the following order: intention, perceived behavioral control, subjective norm, attitude, control beliefs (facilitators), control beliefs (barriers), normative beliefs, and attitudinal beliefs (advantages and disadvantages).
Phase 3: Pilot Testing of the Questionnaires
We pilot tested our questionnaires by asking a convenience sample of 10 participants (5 physicians and 5 AHPs) from our population to answer the questionnaire intended for their own professional group before the focus group. Participants for this phase were recruited purposefully to represent a wide range of professionals and to represent different age groups. Participants could choose either a paper-based survey or a Web-based survey (SurveyMonkey). This choice was meant to ensure that participants less comfortable with computers could access a paper-based version of our questionnaire. We formed 2 focus groups (EPs in 1 and AHPs in the other) to tell us whether they had any difficulty answering the questions. The Web-based survey contained an HTML link to a YouTube video presenting the behavior being studied and paper-based participants were sent the link in the invitation email. For participants who had not completed the survey before the focus group, we presented the video during the focus groups and then they answered a paper-based questionnaire.
We then interviewed participants about both the Web-based and paper-based questionnaires to check comprehension and clarity. Interviews were based on a cognitive interview methodology using a preplanned questionnaire (see Multimedia Appendix 2) [28]. Focus group participants were asked to (1) read the instructions and tell us what they understood, (2) specify what our questions meant to them, (3) specify what the studied behavior meant to them and what a wiki-based reminder represented to them, (4) identify any ambiguous or complex terms, (5) evaluate their ease or difficulty in answering our questions and examine the difficulties, (6) identify the questions that were the most difficult to understand, (7) specify if each answer option was clearly different from the others and, if not, identify those that were too similar, and (8) suggest changing answer options that were ambiguous or that did not translate their thought processes adequately. We also asked questions about the questionnaire length and consequent participant fatigue. Focus groups were recorded, transcribed verbatim, and then analyzed to identify the adjustments that were needed to the wording of some items and to the visual presentation of the questionnaires.
Phase 4: Test and Retest
Once adjustments based on the focus groups’ comments were made, a test-retest study of the revised questionnaires was done with a different convenience sample of 25 EPs and 26 AHPs. These participants had not participated in the elicitation phase (Phase 1) or in the focus groups (Phase 2), but worked in the same 3 trauma centers (levels I, II, and III). The EP participants were recruited from these 3 EDs after presenting this project at a monthly departmental meeting in each center. The AHP participants were recruited after contacting the head of each service and asking them to identify potential participants. Consent to participate in this test-retest study was obtained from all participants after explaining the length of the questionnaire and they were informed that all personal information would remain confidential. However, participants were assigned a unique identifier code to write on their questionnaires to link their test and retest responses. This unique identifier was stored separately from the results. The same questionnaire was performed 2 weeks later with the same participants (retest). For this phase, we again allowed participants to choose between the paper-based and the Web-based questionnaire, but they had to use the same modality for both the test and retest. SurveyMonkey automatically collected the data for the Web version, but responses were manually entered in a spreadsheet for the paper-based questionnaires. The Web-based questionnaire did not contain an official completeness check to identify unanswered items; however, participants were allowed to review all their responses by returning to previous items and participants were asked at the last page to complete all items. We monitored duplicate participation with the unique identifier provided.
Data Analysis
Simple descriptive statistics were used to compare demographic information for EP and AHP participants in our test-retest sample. We also used simple descriptive statistics to compare the demographics of the participants who used the paper-based vs the Web-based questionnaire. We conducted t tests for normally distributed continuous variables and Wilcoxon-Mann-Whitney tests for continuous variables that were not normally distributed. For all categorical variables, we used the Fisher exact test. The internal consistency of the constructs (the tendency of answers within a group of constructs) was measured using Cronbach alpha coefficient. To measure stability over time in the constructs, an agreement intraclass correlation coefficient (ICC) was measured. We used criteria published by Landis and Koch to determine the level of consistency and reproducibility of our items [29]. For any missing data for single questionnaire items, we imputed the average of the other items measuring the same construct. Statistical analysis was performed by a biostatistician using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
Participants
The number of participants per phase of the study is presented in a flow diagram (Figure 1).
Figure 1.
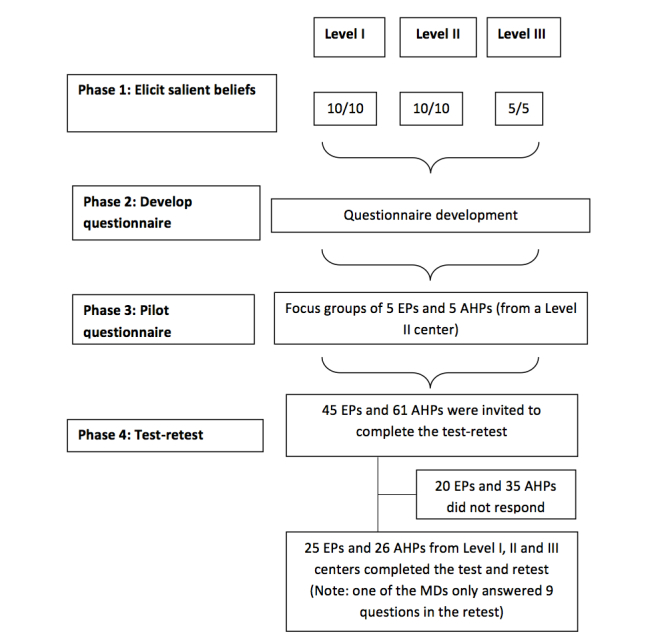
Number of participants per phase of the study. EPs: physicians; AHPs: allied health professionals.
Demographic characteristics of the focus groups and test-retest participants are presented in Table 1.
Table 1.
Demographic characteristics of the focus groups and test-retest participants.
| Variables | Focus groups | Test-retest participants | ||||
|
|
EPs (n=5) |
AHPs (n=5) |
EPs (n=25) |
AHPs (n=26) |
P valuea | |
| Age (years) |
|
|
|
|
|
|
|
|
Mean (SD) | 49 (10) | 36 (3) | 41.5 (8.9) | 35.5 (11.6) | .03 |
|
|
Median (IQR) | 48 (41-56) | 36 (35-38) | 42 (34-48) | 33 (26-43) |
|
| Gender, n (%) |
|
|
|
|
|
|
|
|
Male | 4 (80) | 2 (40) | 19 (76) | 3 (12) | <.001 |
|
|
Female | 1 (20) | 3 (60) | 6 (24) | 23 (88) |
|
| Trauma center level, n (%) |
|
|
|
|
.23 | |
|
|
I | 0 | 0 | 6 (24) | 7 (27) |
|
|
|
II | 5 (100) | 5 (100) | 18 (72) | 14 (54) |
|
|
|
III | 0 | 0 | 1 (4) | 5 (19) |
|
| Profession, n (%) |
|
|
|
|
|
|
|
|
Physician | 5 (100) |
|
25 (100) |
|
|
|
|
Nurse |
|
3 (60) |
|
12 (46) |
|
|
|
Respiratory therapist |
|
1 (20) |
|
7 (27) |
|
|
|
Pharmacist |
|
1 (20) |
|
7 (27) |
|
| Emergency medicine certification, n (%) |
|
N/A |
|
N/A |
|
|
|
|
College of Family Physicians | 2 (40) |
|
21 (84) |
|
|
|
|
Royal College of Physicians of Canada | 3 (60) |
|
3 (12) |
|
|
|
|
Other | 0 |
|
1 (4) |
|
|
| Clinical experience (years) |
|
|
|
|
|
|
|
|
Mean (SD) | 15 (9) | 12 (4) | 12.5 (9.4) | 13.2 (11.1) | .79 |
|
|
Median (IQR) | 13 (8-18) | 12 (11-14) | 11 (5.5-17) | 10.8 (5-19.8) |
|
| Internet access in the ED, n (%) | 5 (100) | 3 (60) | 25 (100%) | 20 (77) | .02 | |
| Professional use of a wiki, n (%) | 2 (40) | 2 (40) | 5 (20) | 2 (8) | .25 | |
| Personal use of a wiki, n (%) | 4 (80) | 2 (40) | 18 (72) | 8 (31) | .005 | |
| Previous editing of a wiki, n (%) | 1 (20) | 1 (20) | 0 (0) | 0 (0) | >.99 | |
a P values were only calculated for the test-retest group.
Five EPs and 5 AHPs (3 nurses, 1 respiratory therapist, and 1 pharmacist) formed the focus groups. Among all the test-retest participants, 25% (13/51) came from the level I trauma center, 63% (32/51) from the level II and 12% (6/51) from the level III. Among the 26 test-retest AHPs, there were 12 nurses, 7 respiratory therapists, and 7 pharmacists. Most participating EPs were certified in Emergency Medicine by the College of Family Physicians of Canada (84%, 21/25), 12% (3/25) were certified by the Royal College of Physicians of Canada, and 1 was a family physician certified by the College of Family Physicians of Canada without any Emergency Medicine certification. Compared to the AHPs, the EPs participating in the test-retest were more likely to be older (P=.03), male (P<.001), to have better access to the Internet (P=.02) and to report a higher prevalence of wiki use for personal purposes (72% vs 31%, P=.005). Although more EPs tended to use wikis for professional purposes (20%) than AHPs (8%), this difference was not significant. None of our test-retest participants had ever edited a wiki before. However, in our focus groups 1 EP and 1 AHP had edited a wiki.
Phase 2: Number and Content of Items in the First Version of the Questionnaires
In the EP questionnaire, there were a total of 13 pages with 63 items: 13 direct construct items, 35 indirect construct items, and 15 demographic characteristic items. For the AHP questionnaire, we created 11 pages with 58 items: 13 direct construct items, 31 indirect construct items, and 14 demographic characteristic items. The original versions of the questionnaires developed during Phase 2 are available in French (see Multimedia Appendices 3 and 4).
Phase 3: Focus Group Comments and Changes Made to the Questionnaires
In the focus groups, all EPs chose to answer the Web-based survey rather than the paper-based version. The reason evoked was that it was easier to access the survey after receiving the email invitation. One AHP chose the paper version because this participant had not filled out the questionnaire before the focus group and all the other AHPs used the Web-based questionnaire before attending the focus group. Multimedia Appendix 5 lists all the comments made by our focus group participants and the changes we made to the questionnaire in consequence. In summary, we changed the wording of certain items, reduced the length of the questionnaire (without reducing any of the TPB items), removed 1 item from our demographic questions (a question about Wi-Fi availability), and clarified certain items to make the questionnaire easier to complete.
Phase 4: Test-Retest Results and Changes Made to the Questionnaires
Table 2 compares the characteristics of participants who chose the Web-based questionnaire with those of participants who chose the paper-based questionnaire.
Table 2.
Demographic characteristics of participants using Web-based questionnaire vs paper-based questionnaire.
| Variables | Emergency physicians (n=25)a |
Allied health professionals (n=26) |
|||||
|
|
Paper (n=18) |
Web (n=7) |
P | Paper (n=2) |
Web (n=24) |
P | |
| Age (years) |
|
|
|
|
|
|
|
|
|
Mean (SD) | 41.6 (8.6) | 41.3 (10.5) | .95 | 43.5 (20.5) | 34.8 (11.4) | .44 |
|
|
Median (IQR) | 42 (36-47) | 41 (32-49) |
|
44 (32-49) | 33 (24-35) |
|
| Gender, n (%) |
|
|
.74 |
|
|
.60 | |
|
|
Male | 14 (78) | 5 (71) |
|
0 (0) | 3 (12.5) |
|
|
|
Female | 4 (22) | 2 (29) |
|
2 (100) | 21 (87.5) |
|
| Trauma center level, n (%) |
|
|
.007 |
|
|
.003 | |
|
|
I | 2 (11) | 4 (57) |
|
0 (0) | 7 (29) |
|
|
|
II | 16 (88) | 2 (29) |
|
0 (0) | 14 (58) |
|
|
|
III | 0 (0) | 1 (14) |
|
2 (100) | 3 (12.5) |
|
| Certification, n (%) |
|
|
.11 |
|
N/A |
|
|
|
|
College of Family Physicians | 16 (88) | 4 (57) |
|
|
|
|
|
|
Royal College of Physicians | 2 (11) | 2 (29) |
|
|
|
|
|
|
Other | 0 (0) | 1 (14) |
|
|
|
|
| Profession, n (%) |
|
|
|
|
|
.13 | |
|
|
Physician | 18 (100) | 7 (100) |
|
|
|
|
|
|
Nurse |
|
|
|
0 (0) | 12 (50) |
|
|
|
Respiratory therapist |
|
|
|
2 (100) | 5 (20) |
|
|
|
Pharmacist |
|
|
|
0 (0) | 7 (29) |
|
| Clinical experience (years) |
|
|
|
|
|
|
|
|
|
Mean (SD) | 12.2 (9.1) | 13.1 (11.1) | .88 | 21 (22.6) | 12.6 (10.2) | .55 |
|
|
Median (IQR) | 11 (5-18) | 11 (5-20) |
|
21 (13-29) | 11 (5-17) |
|
| Internet access in ED, n (%) | 18 (100) | 7 (100) | >.99 | 0 (0) | 20 (83%) | .046 | |
| Professional use of a wiki, n (%) | 4 (22) | 1 (14) | .66 | 1 (50) | 1 (4) | .15 | |
| Personal use of a wiki, n (%) | 12 (66) | 6 (86) | .63 | 2 (100) | 6 (25) | .09 | |
| Previous editing of a wiki, n (%) | 0 (0) | 0 (0) | >.99 | 0 (0) | 0 (0) | >.99 | |
a16 EPs were asked to use the paper-based survey and the 9 others could choose Web- or paper-based. All AHPs had the choice to use either Web- or paper-based.
Most EPs (72%, 18/25) used the paper-based version. In contrast, most AHPs (92%, 24/26) preferred the Web-based version for the test-retest and only 2 of 26 AHPs (8%) chose to use the paper-based version. There were no significant differences in characteristics between EPs who used the Web-based vs the paper-based questionnaire. However, 16 of 18 EPs who used the paper-based version did so because the survey was presented during a monthly department meeting when Internet access was not available. Among EPs who had the choice between paper and Web, 6 of 9 (67%) opted for the Web-based questionnaire. The 2 AHPs who chose the paper version worked at the level III trauma center and did not have Internet access in their hospital. All participants used the same administration mode (paper vs Web) for the test and retest. All participants completed the test and retest except 1 EP who only completed 9 items in the retest questionnaire and did not complete it. The data for these 9 items (all relating to direct TPB questionnaire items) were retained in our analysis, but no imputation was performed for the missing data for this participant. There were no duplicate participants.
Overall psychometric properties of our 2 questionnaires are presented in Table 3. Internal consistency and temporal stability for each individual item in both questionnaires are presented in Multimedia Appendix 6.
Table 3.
Overall internal consistency (Cronbach alpha) and temporal stability (intraclass correlation coefficient, ICC) of our questionnaire
| Questionnaire constructs | Emergency physicians | Allied health professionals | ||||
|
|
Internal consistency | Stability | Internal consistency | Stability | ||
|
|
Test | Retest | ICC | Test | Retest | ICC |
| Intention | .94 | .98 | .89 | .69 | .81 | .48a |
| Attitude | .74 | .72b | .70 | .85 | .87 | .83 |
| Subjective norm | .79 | .78 | .75 | .47a | .82 | .62 |
| Perceived behavioral control | .65 | .67a | .68 | .55a | .62 | .60 |
| Attitudinal beliefs | .94 | .86 | .60 | .92 | .91 | .82 |
| Normative beliefs | .83 | .87 | .80 | .85 | .90 | .74 |
| Control beliefs-barriers | .58 | .67c | .78 | .58d | .55 | .66 |
| Control beliefs-facilitators | .97 | .85 | .30e | .72 | .94 | –.05f |
a1 item was reformulated.
b1 item was removed (with 3 items: test Cronbach alpha=.89, retest Cronbach alpha=.91, ICC=.78).
c2 items were reformulated.
d2 items were removed.
e3 items were reformulated and 2 removed.
f1 item was removed.
The internal consistency of the items in the EP questionnaire was high (Cronbach alpha >.8) for 4 constructs (intention, attitudinal beliefs, normative beliefs, and control belief facilitators), substantial (Cronbach alpha=.6-.8) for 3 constructs (attitude, perceived behavioral control, and subjective norm), and moderate (Cronbach alpha=.4-.6) for control belief barriers (test Cronbach alpha=58; retest Cronbach alpha=.67). One item measuring the attitude construct was removed due to lack of consistency (test: Cronbach alpha=.06; retest: Cronbach alpha=.02) (see Multimedia Appendix 6). This reduced the length of the questionnaire without affecting the internal consistency of this construct (3 items to measure attitude: test: .89; retest: .91). One item measuring perceived behavioral control was formulated differently because it had low consistency (test: Cronbach alpha=.20; retest: Cronbach alpha=.26) (see Multimedia Appendix 6). For the control beliefs, 2 items were reformulated to increase their internal consistency. All items were considered moderately stable over time (ICC >.4) except for the items measuring facilitators (ICC=.30). Consequently, we reformulated the 3 items concerning facilitators and removed items that represented beliefs that were less salient (based on their ranking in our Phase 1 study) to decrease the questionnaire length.
For the AHP questionnaire, internal consistency was high (Cronbach alpha >.8) for 3 constructs (attitude, attitudinal beliefs, and normative beliefs), substantial (Cronbach alpha=.6-.8) for 2 constructs (intention and control beliefs facilitators), and moderate for 3 constructs (subjective norm, perceived behavioral control, and control beliefs barriers). Therefore, we reformulated items with poor internal consistency: 1 item measuring intention, 1 item for perceived behavioral control, and 1 item for subjective norm. The stability of the items in our AHP questionnaire was good for most constructs except control beliefs facilitators (ICC= –.05). Because the consistency and stability of the items measuring control beliefs (barriers and facilitators) were low, we removed 2 items measuring control beliefs (1 barrier and 1 facilitator) that were not consistent or stable.
The changes made to all the items in our questionnaires are listed in Multimedia Appendices 7 (EPs) and 8 (AHPs) and the final versions (in French) are found in Multimedia Appendices 9 (EPs) and 10 (AHPs). English versions of the questionnaires are also available (Multimedia Appendices 11 and 12). The final EP questionnaire has 11 pages with 55 items and the AHP questionnaire has 9 pages containing 53 items.
Discussion
Principal Results
The objectives of this study were to develop and test the psychometric properties of 2 questionnaires exploring the intention of ED health care professionals and the determinants of this intention to use wiki-based reminders promoting best practices for the management of severe TBI victims. Building on a previous study that had identified the salient beliefs of health care professionals about using wiki-based reminders, our 2 questionnaires will also measure the importance of each of these beliefs. The 4 videos developed in support of these 2 questionnaires helped the participants understand the behavior being investigated. The EP questionnaire now contains 55 items and the AHP questionnaire contains 53 items including the demographic items, as opposed to their original 68 and 58 items, respectively. Both questionnaires take approximately 10 minutes to complete after viewing a 6-minute video. Although some items needed reformulating, our questionnaires now have adequate validity and reliability for large surveys. These results lead us to the following observations.
First, to our knowledge, these questionnaires are among the first to be developed to understand how to implement a wiki that will promote best clinical practices in any area of health care. Other authors have used the Technology Assessment Model to explore how health care professionals use and contribute to social media in general to share medical knowledge with other physicians in the medical community [24]. In contrast, we developed and validated our questionnaires by rigorously following the TPB methodology [30] and included all its constructs, both direct and indirect. As a result, our questionnaires will allow researchers to identify which behavioral determinants are most influential and, therefore, which determinants should be targeted when developing a theory-based intervention.
Second, these 2 questionnaires were developed and validated for 4 types of professionals (EPs, registered nurses, respiratory therapists, and pharmacists) and, thus, are ready for use across this range of health care professionals. The questionnaires are similar in terms of number of items, length of administration, and direct construct items, and many of the items investigating indirect construct items are similar (eg, validity of the information, hospital administration support, ease of access to the wiki-based reminder). However, other items exploring indirect constructs differ from 1 questionnaire to the other depending on the different salient beliefs held by each group of professionals (information captured in Phase 1). For example, the EP questionnaire contains an item investigating the influence of surgeons on their intention to use a wiki-based reminder to care for TBI victims, whereas the AHP questionnaire contains instead an item exploring the influence of quality control managers on their intention. Our results confirm our decision to begin our study by exploring salient beliefs and adapt each questionnaire accordingly. For example, our finding of higher current wiki use and Internet access among EPs than among AHPs supports the need for interventions adapted to each profession. Future investigations using our questionnaires will help us verify the importance of these factors among the different ED health care professionals and then construct profession-specific interventions to guide the implementation of a wiki promoting best practices in TBI trauma care.
Third, some of the constructs in our questionnaires lacked high levels of consistency (eg, perceived behavioral control and control beliefs), more so in the AHP questionnaire than in the EP questionnaire. One explanation for this lack of internal consistency is that the AHP participants were a more heterogeneous group than the EP participants. The AHPs were nurses, respiratory therapists, and pharmacists who all have different clinical tasks and who potentially perceive different levels of control over their clinical practice and behaviors. Moreover, although we tried to make the studied behavior as clear as possible by using profession-specific videos and repeating the description of the behavior in each question, it is still possible that participants did not all have the same behavior in mind. Future investigations with larger samples will help us verify these discrepancies between groups of professionals, and will be important to consider in a future implementation strategy.
Fourth, if given the choice, EPs and AHPs preferred to use the Web-based version rather than the paper version. Although our small sample size prevented us from comparing the internal consistency and stability of the Web-based version compared to the paper-based version, we must continue to have a paper version available because some professionals do not have Internet access (eg, AHPs and those working in smaller trauma centers). Offering a paper version will also allow us to capture the opinions of professionals who are not computer- or Web-savvy and yet are important stakeholders to consider in a future theory-based intervention. Most importantly, lack of Internet access among participants in this survey is an important barrier that must be addressed in any future wiki intervention. For our survey, we addressed this barrier by installing the survey videos on local hospital computers.
Fifth, the videos we created proved to be a useful tool for helping assess the intention of health care professionals to use wiki-based reminders. Using a video was advantageous in that the behavior being studied is new and complex (ie, to use a wiki-based reminder promoting best practice for the management of severe TBI victims in the ED in the Province of Quebec, Canada) and depends on many smaller microbehaviors (eg, logging on to the Internet, using a keyboard to type in the search terms to find the wiki-based reminder, checking off the appropriate prescriptions suggested by the wiki-based reminder). These videos allowed respondents to understand all the small implicit lead-in behaviors necessary to performing the behavior that we were studying.
Finally, EPs and AHPs in our sample reported lower wiki use for professional purposes (20% and 8%) than reported in a recent review of wiki use in health care. This review identified studies reporting a range of usage rates ranging from 18% for nurse practitioners and physician assistants to 35% for pharmacists, 55% for consultants, and 80% for junior physicians [17,31-34]. Although these differences are possibly due to our small convenience sample, future surveys with larger samples will produce better estimates of current wiki use for professional purposes.
Limitations
Our study has some limitations. First, we had originally planned to use the 2-arm expectancy-value model to measure the influence of indirect constructs (salient beliefs, ie, behavioral beliefs, outcome evaluation, normative beliefs, motivation to comply, control beliefs, and perceived power to influence). However, considering the large number of salient beliefs we retained in our qualitative survey and the fact that the 2-arm expectancy-value model has not shown any advantage over simply using 1 arm of the belief-based measures (only measuring behavioral beliefs, normative beliefs, and control beliefs), we decided to only include items measuring these 3 belief-based measures in our questionnaire [35]. This reduced the number of items in our final questionnaire and likely lowered its administration time, thus reducing participant fatigue and the boredom of answering questions that seem redundant in the 2-arm expectancy model. Shorter questionnaires have been shown to produce more valid information [36].
Second, certain indirect items in our questionnaire lacked temporal stability (eg, control beliefs). This lack of temporal stability might be due to participants changing their assessment of the importance of the different facilitators after 2 weeks, especially if they decided not to watch the video before the retest to save time. Although the retest instructed participants to watch the video again, we did not ask participants if they actually followed this instruction.
Third, our use of the TPB limits our capability to directly assess the importance of environmental factors such as organizational readiness for change. The use of the Theoretical Domains Framework to inform our theory-based intervention could correct this [37,38].
Finally, our questionnaire does not measure the determinants of contributing to the wiki, in addition to consulting it. By definition, a wiki is a product of its users and remains relevant only if its users continue to update it and create new content. Getting experts and other members of a wide community to contribute to a collaborative writing project is a difficult task and a theory-based approach will be needed to stimulate and promote this behavior [14,39,40]. Unfortunately, time constraints are a major barrier when studying clinician behavior in the ED [41,42]. Thus, questionnaire length limited the number of behaviors we could assess in this study. Several further behaviors will need to be studied in the future, but we chose the one we felt to be the most important (using the wiki). If clinicians do not intend to consult a wiki during their clinical duties, we need to understand the determinants of this behavior before asking them to update and create content.
Future Studies
The next step will be to use these questionnaires in a larger population of ED health care professionals in the Province of Quebec. However, to use this questionnaire in an even broader population across Canada and internationally, our survey instruments (videos and questionnaires) will need to be translated from French to English and other languages and validated using cross-cultural adaptation of the self-report measures [43]. Although we have produced an English version of our questionnaires (Multimedia Appendices 11 and 12), they still need to be validated with a population of English-speaking health care professionals before they can be used in large surveys. Using these questionnaires in multiple settings and countries will help identify the behavioral determinants that a future theory-based intervention should target in order to stimulate the use of wikis promoting best practices in trauma care around the world. Although our questionnaires already contain certain items that are not exclusively relevant to trauma care and EDs and which could serve as a basis for new questionnaires investigating the intention to use wiki-based reminders in other fields of health care, in order to use them to investigate the use of wiki-based reminders in other settings they need to be adapted and validated.
Conclusion
Our newly developed theory-based questionnaire to measure health care professionals’ intention to use wiki-based reminders has adequate validity and reliability for use in a large survey. In the long run, this will help develop theory-based interventions for wikis promoting best practices in trauma care.
Acknowledgments
France Légaré is Canada Research Chair in the Implementation of Shared Decision Making in Primary Care. Marie-Pierre Gagnon is Canada Research Chair in the Implementation of Information Technology in Health Care. Patrick Archambault and Richard Fleet hold a Junior 1 Career Scientist award from FRQS. Funding for this study was provided by a CADRE program (reference number: PDA 1850) supported by a partnership between the Canadian Health Services Research Foundation (now the Canadian Foundation for Healthcare Improvement) and the Canadian Institutes of Health Research. It was also supported by a CSSS Alphonse-Desjardins research grant. The funding bodies did not play any role in the design, collection, analysis, or interpretation of data; in the writing of the manuscript; or in the decision to submit the manuscript for publication. We would like to thank Gaston Godin, Ariane Bélanger-Gravel, Claudine Blanchet, Simon Rioux, Cynthia Fournier, Claudie-Anne Giasson, Catherine Nadeau, Michèle Dugas, Andrea Bilodeau, and Jean-François Rancourt for their support in various phases of this project. We would also like to thank Louisa Blair for editing our manuscript and translating our questionnaires. Finally, we would like to thank all the participants who generously took the time to participate in the focus group and who participated in the test-retest.
Abbreviations
- AHP
allied health professional
- ED
emergency department
- EP
emergency physician
- ICC
intraclass correlation coefficient
- TBI
traumatic brain injury
- TPB
Theory of Planned Behavior
Multimedia Appendix 1
Links to YouTube videos presenting the behaviour studied.
Multimedia Appendix 2
Cognitive interview questionnaire (in French).
Multimedia Appendix 3
AHP questionnaire developed during Phase 2.
Multimedia Appendix 4
MD questionnaire developed during Phase 2.
Multimedia Appendix 5
Comments made by focus group participants and changes made to questionnaire.
Multimedia Appendix 6
Analysis of internal consistency and temporal stability for each item in the MD and AHP questionnaires.
Multimedia Appendix 7
Changes made to the EP questionnaire after the two-week test-retest.
Multimedia Appendix 8
Changes made to the AHP questionnaire after the two-week test-retest.
Multimedia Appendix 9
Final AHP questionnaire (French).
Multimedia Appendix 10
Final MD questionnaire (French).
Multimedia Appendix 11
Final AHP questionnaire (English).
Multimedia Appendix 12
Final MD questionnaire (English).
Footnotes
Conflicts of Interest: None declared.
References
- 1.Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients' care. Lancet. 2003 Oct 11;362(9391):1225–30. doi: 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]
- 2.Straus SE, Tetroe J, Graham ID. In: Knowledge Translation in Health Care: Moving from Evidence to Practice. Straus SE, Tetroe J, Graham I, editors. Hoboken, NJ: Wiley-Blackwell; 2009. [Google Scholar]
- 3.Sahota N, Lloyd R, Ramakrishna A, Mackay JA, Prorok JC, Weise-Kelly L, Navarro T, Wilczynski NL, Haynes RB, CCDSS Systematic Review Team Computerized clinical decision support systems for acute care management: a decision-maker-researcher partnership systematic review of effects on process of care and patient outcomes. Implement Sci. 2011;6:91. doi: 10.1186/1748-5908-6-91. http://www.implementationscience.com/content/6//91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Black AD, Car J, Pagliari C, Anandan C, Cresswell K, Bokun T, McKinstry B, Procter R, Majeed A, Sheikh A. The impact of eHealth on the quality and safety of health care: a systematic overview. PLoS Med. 2011;8(1):e1000387. doi: 10.1371/journal.pmed.1000387. http://dx.plos.org/10.1371/journal.pmed.1000387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lang ES, Wyer PC, Haynes RB. Knowledge translation: closing the evidence-to-practice gap. Ann Emerg Med. 2007 Mar;49(3):355–63. doi: 10.1016/j.annemergmed.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 6.Holroyd BR, Bullard MJ, Graham TA, Rowe BH. Decision support technology in knowledge translation. Acad Emerg Med. 2007 Nov;14(11):942–8. doi: 10.1197/j.aem.2007.06.023. [DOI] [PubMed] [Google Scholar]
- 7.Weingart SN, Toth M, Sands DZ, Aronson MD, Davis RB, Phillips RS. Physicians' decisions to override computerized drug alerts in primary care. Arch Intern Med. 2003 Nov 24;163(21):2625–31. doi: 10.1001/archinte.163.21.2625. [DOI] [PubMed] [Google Scholar]
- 8.Stiell IG, Bennett C. Implementation of clinical decision rules in the emergency department. Acad Emerg Med. 2007 Nov;14(11):955–9. doi: 10.1197/j.aem.2007.06.039. [DOI] [PubMed] [Google Scholar]
- 9.Chan J, Shojania KG, Easty AC, Etchells EE. Does user-centred design affect the efficiency, usability and safety of CPOE order sets? J Am Med Inform Assoc. 2011 May 1;18(3):276–81. doi: 10.1136/amiajnl-2010-000026. http://jamia.bmj.com/cgi/pmidlookup?view=long&pmid=21486886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wright A, Sittig DF, Carpenter JD, Krall MA, Pang JE, Middleton B. Order sets in computerized physician order entry systems: an analysis of seven sites. AMIA Annu Symp Proc. 2010;2010:892–6. http://europepmc.org/abstract/MED/21347107. [PMC free article] [PubMed] [Google Scholar]
- 11.Wright A, Bates DW, Middleton B, Hongsermeier T, Kashyap V, Thomas SM, Sittig DF. Creating and sharing clinical decision support content with Web 2.0: Issues and examples. J Biomed Inform. 2009 Apr;42(2):334–46. doi: 10.1016/j.jbi.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 12.Shojania KG, Jennings A, Mayhew A, Ramsay C, Eccles M, Grimshaw J. Effect of point-of-care computer reminders on physician behaviour: a systematic review. CMAJ. 2010 Mar 23;182(5):E216–25. doi: 10.1503/cmaj.090578. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=20212028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Theal J, Protti D. CPOE with evidence-based clinical decision support improves patient outcomes: the journey to date for a Canadian hospital. Healthc Q. 2014;17(1):24–9. doi: 10.12927/hcq.2014.23780. [DOI] [PubMed] [Google Scholar]
- 14.Riley J, McGowan M, Rozmovits L. Exploring the value of technology to stimulate interprofessional discussion and education: a needs assessment of emergency medicine professionals. J Med Internet Res. 2014;16(6):e162. doi: 10.2196/jmir.3482. http://www.jmir.org/2014/6/e162/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jibuike OO, Paul-Taylor G, Maulvi S, Richmond P, Fairclough J. Management of soft tissue knee injuries in an accident and emergency department: the effect of the introduction of a physiotherapy practitioner. Emerg Med J. 2003 Jan;20(1):37–9. doi: 10.1136/emj.20.1.37. http://emj.bmj.com/cgi/pmidlookup?view=long&pmid=12533365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Trzeciak S, Dellinger Rp, Abate Nl, Cowan Rm, Stauss M, Kilgannon Jh, Zanotti S, Parrillo Je. Translating research to clinical practice: a 1-year experience with implementing early goal-directed therapy for septic shock in the emergency department. Chest. 2006 Feb;129(2):225–32. doi: 10.1378/chest.129.2.225. [DOI] [PubMed] [Google Scholar]
- 17.Archambault PM, van de Belt TH, Grajales FJ, Faber MJ, Kuziemsky CE, Gagnon S, Bilodeau A, Rioux S, Nelen WL, Gagnon MP, Turgeon AF, Aubin K, Gold I, Poitras J, Eysenbach G, Kremer JA, Légaré F. Wikis and collaborative writing applications in health care: a scoping review. J Med Internet Res. 2013;15(10):e210. doi: 10.2196/jmir.2787. http://www.jmir.org/2013/10/e210/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heilman JM, Kemmann E, Bonert M, Chatterjee A, Ragar B, Beards GM, Iberri DJ, Harvey M, Thomas B, Stomp W, Martone MF, Lodge DJ, Vondracek A, de Wolff JF, Liber C, Grover SC, Vickers TJ, Meskó B, Laurent MR. Wikipedia: a key tool for global public health promotion. J Med Internet Res. 2011;13(1):e14. doi: 10.2196/jmir.1589. http://www.jmir.org/2011/1/e14/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heilman J, Bastian H, Tharyan P. Cochrane Collaboration. 2014. Aug, [2014-08-05]. Wikipedia meets Cochrane: working to get better evidence into mass use; The 21st Cochrane Colloquium http://2013.colloquium.cochrane.org/abstracts/wikipedia-meets-cochrane-working-get-better-evidence-mass-use.
- 20.National Institutes of Health. [2013-06-18]. Guidelines for Participating in Wikipedia from NIH - Office of Communications & Public Liaison http://www.nih.gov/icd/od/ocpl/resources/wikipedia/
- 21.McIntosh B , Cameron C, Singh S, Yu C, Ahuja T, Welton N, Dahl M. 2011. [2013-05-05]. Second-line therapy in patients with type 2 diabetes inadequately controlled with metformin monotherapy: A systematic review and mixed treatment comparisons meta-analysis http://livewiki.openmedicine.ca/Second-line_therapy_in_patients_with_type_2_diabetes_inadequately_controlled_with_metformin_monotherapy:_A_systematic_review_and_mixed_treatment_comparisons_meta-analysis. [PMC free article] [PubMed]
- 22.Meenan C, King A, Toland C, Daly M, Nagy P. Use of a wiki as a radiology departmental knowledge management system. J Digit Imaging. 2010 Apr;23(2):142–51. doi: 10.1007/s10278-009-9180-1. http://europepmc.org/abstract/MED/19184221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yu R, Crotty B. Wikis to better manage shared information in a hospitalist group. Society of Hospital Medicine. Research, Innovations, Clinical Vignettes Competition; May 10-13, 2011; Gaylord Texan Resort and Convention Center, Grapevine, TX. 2011. pp. 140–141. [Google Scholar]
- 24.McGowan BS, Wasko M, Vartabedian BS, Miller RS, Freiherr DD, Abdolrasulnia M. Understanding the factors that influence the adoption and meaningful use of social media by physicians to share medical information. J Med Internet Res. 2012;14(5):e117. doi: 10.2196/jmir.2138. http://www.jmir.org/2012/5/e117/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Archambault PM, Bilodeau A, Gagnon MP, Aubin K, Lavoie A, Lapointe J, Poitras J, Croteau S, Pham-Dinh M, Légaré F. Health care professionals' beliefs about using wiki-based reminders to promote best practices in trauma care. J Med Internet Res. 2012;14(2):e49. doi: 10.2196/jmir.1983. http://www.jmir.org/2012/2/e49/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Conner M. Predicting Health Behaviour: Research and Practice with Social Cognition Models. Buckingham: Open University Press; 1996. [Google Scholar]
- 27.Archambault PM, Légaré F, Lavoie A, Gagnon MP, Lapointe J, St-Jacques S, Poitras J, Aubin K, Croteau S, Pham-Dinh M. Healthcare professionals' intentions to use wiki-based reminders to promote best practices in trauma care: a survey protocol. Implement Sci. 2010;5:45. doi: 10.1186/1748-5908-5-45. http://www.implementationscience.com/content/5//45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Willis GB. Cognitive Interviewing: A Tool for Improving Questionnaire Design. Thousand Oaks, CA: Sage Publications; 2005. [Google Scholar]
- 29.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977 Mar;33(1):159–74. [PubMed] [Google Scholar]
- 30.Francis JJ, Eccles MP, Johnston M, Walker A, Grimshaw J, Foy R, Kaner EFS, Smith L, Bonetti D. Constructing Questionnaires Based on the Theory Constructing Questionnaires Based on the Theory of Planned Behaviour: A Manual for Health Services Researchers. Newcastle upon Tyne, UK: University of Newcastle upon Tyne; 2004. [2014-09-09]. http://openaccess.city.ac.uk/id/eprint/1735. [Google Scholar]
- 31.Sandars J, Schroter S. Web 2.0 technologies for undergraduate and postgraduate medical education: an online survey. Postgrad Med J. 2007 Dec;83(986):759–62. doi: 10.1136/pgmj.2007.063123. http://europepmc.org/abstract/MED/18057175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hughes B, Joshi I, Lemonde H, Wareham J. Junior physician's use of Web 2.0 for information seeking and medical education: a qualitative study. Int J Med Inform. 2009 Oct;78(10):645–55. doi: 10.1016/j.ijmedinf.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 33.Brokowski L, Sheehan AH. Evaluation of pharmacist use and perception of Wikipedia as a drug information resource. Ann Pharmacother. 2009 Nov;43(11):1912–3. doi: 10.1345/aph.1M340. [DOI] [PubMed] [Google Scholar]
- 34.Iyer AK. Uspace Institutional Repository. University of Utah; 2011. [2014-09-09]. Drug information-seeking behavior among healthcare professionals within the University of Utah Community Clinics [master's thesis] http://content.lib.utah.edu/cdm/ref/collection/etd3/id/2754. [Google Scholar]
- 35.Gagne C, Godin G. The Theory of Planned Behavior: Some Measurement Issues Concerning Belief-Based Variables. J Appl Social Pyschol. 2000 Oct;30(10):2173–2193. doi: 10.1111/j.1559-1816.2000.tb02431.x. [DOI] [Google Scholar]
- 36.Krosnick JA. Response strategies for coping with the cognitive demands of attitude measures in surveys. Applied Cognitive Psychology. 1991 May;5(3):213–236. doi: 10.1002/acp.2350050305. [DOI] [Google Scholar]
- 37.Huijg JM, Gebhardt WA, Crone MR, Dusseldorp E, Presseau J. Discriminant content validity of a theoretical domains framework questionnaire for use in implementation research. Implement Sci. 2014;9:11. doi: 10.1186/1748-5908-9-11. http://www.implementationscience.com/content/9//11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care. 2005 Feb;14(1):26–33. doi: 10.1136/qshc.2004.011155. http://qhc.bmj.com/cgi/pmidlookup?view=long&pmid=15692000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Archambault P, Thanh J, Blouin D, Gagnon S, Poitras J, Fountain RM, Fleet F, Rioux R, van de Belt TH, Legare F. Emergency medicine residents’ beliefs about contributing to an online collaborative slideshow. Can J Emerg Med. 2014 doi: 10.1017/cem.2014.49. (forthcoming) [DOI] [PubMed] [Google Scholar]
- 40.Archambault PM, Blouin D, Poitras J, Fountain RM, Fleet R, Bilodeau A, Légaré F. Emergency medicine residents' beliefs about contributing to a Google Docs presentation: a survey protocol. Inform Prim Care. 2011;19(4):207–16. doi: 10.14236/jhi.v19i4.815. [DOI] [PubMed] [Google Scholar]
- 41.Gaddis GM, Greenwald P, Huckson S. Toward improved implementation of evidence-based clinical algorithms: clinical practice guidelines, clinical decision rules, and clinical pathways. Acad Emerg Med. 2007 Nov;14(11):1015–22. doi: 10.1197/j.aem.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 42.Scott SD, Osmond MH, O'Leary KA, Graham ID, Grimshaw J, Klassen T, Pediatric Emergency Research Canada (PERC) MDI/spacer Study Group Barriers and supports to implementation of MDI/spacer use in nine Canadian pediatric emergency departments: a qualitative study. Implement Sci. 2009;4:65. doi: 10.1186/1748-5908-4-65. http://www.implementationscience.com/content/4//65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976) 2000 Dec 15;25(24):3186–91. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]


