Introduction
An estimated 42 million people are living with HIV/AIDS worldwide.1 Young people account for 50% of new infections reported annually in the United States, and the number of HIV-positive teens doubles every 14 months. HIV prevention has become a public health priority. Two primary groups of children and adolescents are affected by HIV: those born with the infection and those who acquire it through risky sexual behavior. The number of new cases of vertically transmitted HIV (transmitted in utero) has decreased dramatically in the United States, but those who were infected as infants and who received a transfusion are surviving into adolescence and becoming sexually active. These youths present a host of unique challenges for HIV prevention.
HIV infection among adolescents occurs mainly through unprotected sexual intercourse and other high-risk sexual behavior, such as sex with multiple partners and early sexual debut.3 Early sexual debut is associated with greater risk of HIV/STD infection because of added opportunities for sexual encounters, multiple partners, and high-risk partners. HIV is a prototypical disease for mental health professionals in understanding the interplay among biologic, genetic, and environmental factors. This article offers a social-personal framework to explain HIV-risk behaviors and reviews neurocognitive and psychiatric problems associated with HIV infection among youths.
Definition of HIV/AIDS
The definition of AIDS has undergone several revisions since the mid-1980s when HIV was identified as the causative agent of AIDS and specific diagnostic tests were developed to identify the infection. The 1993 CDC classification system is based on CD4+ T lymphocyte cell counts and clinical conditions associated with HIV infection including opportunistic infections.4 HIV-infected individuals with a CD4+ T cell count of < 200 have AIDS by definition whether or not symptoms or other diseases are present. Infants can show significant immune suppression at CD4 counts of > 200. A revision of the definition in 1999 included laboratory criteria and incorporated reporting criteria for HIV and AIDS into a single case definition.5 These definitions of AIDS were established for public health surveillance and not for practical patient care. Of note, CDC reporting was focused on the number of patients with AIDS and did not initially include all patients infected with HIV. In addition, the age categories of CDC surveillance are 0 to 12 years, 13 to 19, 20 to 24, and above 24. Thus, data about adolescents is often overlapping, extrapolated, or incomplete.
Epidemiology of HIV/AIDS
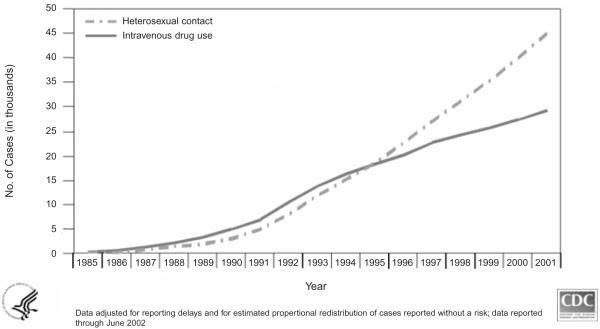
Rates of HIV infection acquired during adolescence are rising. Teenagers’ sexual and drug behavior initiated during this developmental period places them at elevated risk for infection, but some groups are at higher risk than others. Youths in psychiatric care are at elevated risk, because they engage in the same risky behaviors as their peers but at higher rates.6–8 Compared with youths in public schools, psychiatrically hospitalized teens report having been twice as likely to be sexually active, not use condoms, and use IV drugs.9 Adolescents with psychiatric disorders also are more likely to have a history of sexually transmitted diseases than their nontroubled peers,10 and teens in outpatient psychiatric care report high rates of sexual intercourse, sexual activity, having been pregnant, using drugs and alcohol during sex, having sex with a high-risk partner, and having sex without using a condom.7 Data on demographics such as ethnicity and gender, mode of transmission, and location by cities and states for pediatric and adolescent AIDS are updated regularly.11 The demographic face of HIV and AIDS is shifting as youth, women, and people of color are increasingly affected. Indeed, women now comprise approximately 50% of adults living with the disease worldwide (Figure 1).
Figure 1.
Over the past two decades, the incidence of HIV infection among female adults and adolescents has steadily grown. Women now comprise approximately 50% of adults living with the disease worldwide. (Source: www.cdc.gov/hiv/graphics/trends.htm.)
Biology of HIV/AIDS
There are two types of cytopathic human immunodeficiency viruses: HIV-1 and HIV-2. HIV-1 disease is more common, especially in the United States. It is further divided into groups M, O, and N. Viral subtypes of different strains can be identified and often indicate geographic origin.
HIV is transmitted through heterosexual and homosexual contact, by blood and blood products, and by infected mothers during pregnancy or delivery or through breast milk. Maternal transmission of HIV to the fetus occurs most commonly in the perinatal period. In industrialized countries, transmission has been significantly reduced from 25% to 3% through prophylactic antiretroviral therapy around delivery via cesarean section.12,13
There is speculation that girls may be especially vulnerable to infection because of immaturity of the cervical mucosa and hormonal changes. The replication cycle and genome of HIV have been identified, and these data have guided the development of numerous treatment strategies. However, treatments are evolving constantly with each new biologic discovery. The availability of many new antiretroviral agents has made the treatment regimen complex for people with HIV/AIDS. Toxicity, adherence, and viral resistance are some of the factors that influence the ability of youths to remain on anti-retroviral regimens. Information on testing, when to initiate therapy, and considerations for therapy among children and adolescents is published regularly.14
Neurocognitive Development Of HIV/AIDS
HIV virus is found mostly in microglia and macrophages and not in neurons directly. The virus has neurotoxic components, induces a variety of inflammatory factors that are neurotoxic, and causes cell death of neurons. Clinically, encephalopathy is characterized by microcephaly or brain atrophy, motor abnormalities, and cognitive delays. Classification of the types of encephalopathy, static or progressive, has been the subject of much debate. Clinical presentations of encephalopathy vary with age of infection and mode of transmission. Encephalopathy often presents in vertically HIV-infected children as an AIDS-defining illness before the child is severely immunocompromised.
Encephalopathy occurs in up to 21% of these children and contributes to significant morbidity and mortality.15 This is ecreasing with the advent of highly active anti-retroviral therapy. The Women and Infant Transmission Study Group found that scores on the Bayley Scales of Infant Development independently predicted mortality even after adjusting for age, viral load, CD4 count, and treatment.16 Early progressive encephalopathy usually is seen in young untreated infants with high viral loads and rapid clinical deterioration. Advanced maternal HIV disease, maternal encephalopathy, and possibly co-infection with cytomegalovirus (CMV) also are risk factors for children’s developing early progressive encephalopathy.
Encephalopathy generally presents later in children or adolescents who were infected through transfusion and follows a more-indolent course. For patients with hemophilia, encephalopathy is uncommonly an AIDS-defining illness. Practitioners are seeing more patients with gradual progression into dementia with bradykinesias, spasticity, and hallucinations in infected adolescents with late-stage AIDS regardless of the mode of transmission. Opportunistic CNS infections such as toxoplasmosis, progressive multifocal leukoencephalopathy (PML), and CNS lymphoma are rare in pediatric AIDS and may present with seizures or focal neurologic signs.17
The differential diagnosis for encephalopathy in infants and children should include:
Possible intrauterine drug exposure to cocaine, alcohol, or other substances;
Opiate withdrawal;
Congenital infections with toxoplasmosis, syphilis, or CMV; acquired
Cryptococcal meningitis; and
HIV virus
.
In older youths, cerebral malformations, cortical dysplasias, hypoxic-ischemic encephalopathies, and PML should be considered when cognitive development fails to progress appropriately. Expressive language is affected more than receptive language in children with vertically transmitted HIV. Adolescent patients who are long-term survivors frequently have cognitive problems, particularly in memory and attention. The Continuous Performance Test may be useful to detect subtle changes in attention.18 As HIV-infected children live longer and are healthier, cognitive issues have come to the fore, and these children’s educational needs are significant.
Tests to Diagnose and Monitor HIV Status
Testing to diagnose HIV infection has evolved to provide quicker, more-accurate, and cost-effective results. Current testing approaches detect the virus directly or demonstrate antibody to the virus or a component, which usually appears 2–12 weeks after acute infection. These methods include enzyme-linked immunosorbent assay, or EIA; Western Blot; p24 antigen capture assay; HIV-1 DNA polymerase chain reaction; and HIV-1 RNA assay. In addition to using these tests, clinicians frequently monitor CD4+ T cell counts, viral load (HIV RNA concentrations), and HIV-drug resistance testing to follow the clinical course. Counseling around HIV testing is critical, and guidelines are available.14
Neuroimaging can be used to manage youths with HIV/AIDS, although findings of microcalcifications on computed tomography (CT) may lag behind clinical encephalopathy. The most common CT findings associated with encephalopathy are basal ganglia calcifications, brain atrophy with enlarged ventricles, and enlarged cortical sulci.19 Magnetic resonance imaging (MRI) may detect mass lesions found in toxoplasmosis or CNS lymphoma. MRI also is useful in detecting cerebrovascular complications since HIV-infected children have a higher incidence of ischemic strokes and cerebral artery aneurysms that may expand or rupture. MRI screening has been recommended for high-risk children who are asymptomatic from HIV disease but are displaying neurocognitive dysfunction.20 Positron emission tomography (PET) may indicate diffuse hypometabolism in some children with severe encephalopathy, but PET and functional MRI remain largely theoretical tools for early detection of neurocognitive deficits.
Theoretical Framework for Understanding HIV Risk
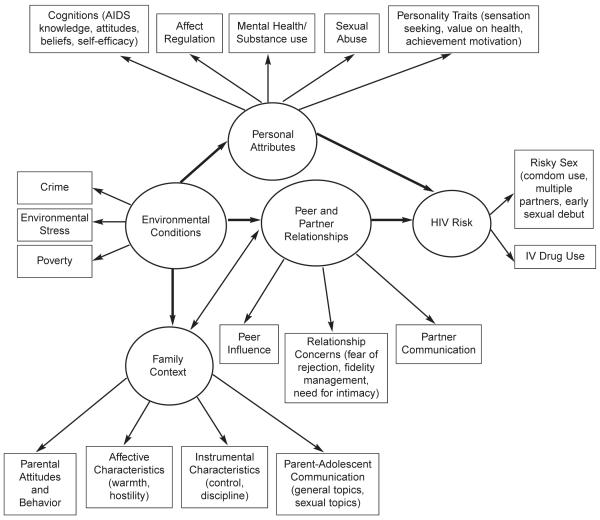
The processes associated with vertical transmission of HIV are well understood, but the mechanisms related to HIV transmission through risky sex are less clear. Specifically, no theoretical model encompasses the full range of psychosocial influences on risk behavior among teens in psychiatric care. Most theories fail to consider developmental and maturational constructs that are important during adolescence (i.e., developmental processes implicated in adolescent risk-taking) and require a level of intellectual maturity and stability yet to develop in many teens. Donenberg developed a social-personal framework to explain HIV-risk behavior that includes important psychosocial, and contextual risk factors specific to teens with psychiatric problems (Figure 2). The framework emphasizes the interplay between individual and social factors, incorporating the effects of:
Personal attributes (cognitions, affect dysregulation, mental health, substance use, sexual abuse, personality traits);
Family context (affective and instrumental behaviors, parent-adolescent communication, parental attitudes and behavior);
Peer and partner relationship concerns (need for intimacy, fear of rejection, peer influence, partner communication); and
Environmental circumstances (crime, poverty, stress).
Figure 2.
Donenberg’s social-personal framework to explain HIV-risk behavior.The model draws from diverse literature on HIV-risk, developmental psychopathology, family functioning, substance abuse, health behavior, and multisystemic theories of child behavior.6, 41, 42
Personal Attributes and HIV-Risk
Important personal attributes are implicated in adolescent HIV risk.
Cognitions
Knowledge about the causes of HIV/AIDS and modes of transmission has not led to changes in sexual risk-taking among youths. By contrast, their attitudes and beliefs about HIV may influence their behavior. Perceptions of personal vulnerability, motivation to prevent infection, and positive attitudes toward prevention predict health-promoting behavior. Teens in psychiatric care, however, display significant knowledge deficits and other cognitive impairments that place them at elevated risk of infection. Distorted cognitions, dysfunctional thinking about relationships, and problems in accurate judgment result in decreased ability to assess risk, poor decision-making, diminished problem-solving, limited information processing, and poor reality testing.6 Perceptions of self-efficacy to practice prevention are linked to less risky sex, but youths with psychiatric problems lack critical interpersonal and social skills (assertiveness, effective communication) to negotiate safe sex.21 The sexual behavior of teens in psychiatric care is more likely to be impulsive and spontaneous and not the result of calm decision-making.
Affect Dysregulation
Affect regulation is the ability to respond to the environment with a range of emotions, and to react spontaneously or suppress immediate reactions when necessary. 22 The ability to regulate affect matures throughout life and is necessary for adapting to and coping with negative emotional arousal. The inability to regulate distress often leads to short-term self-soothing behaviors.23 Youths with mental health problems often experience negative emotional arousal without adequate affect regulation skills, and thus, they use self-soothing behaviors (e.g., risky sex, sharing cutting utensils) that increase HIV risk. Distress and anxiety in sexual situations may be particularly problematic because of relationship maintenance concerns or previous trauma.
Mental Health and Substance Use
Mental health problems have been implicated in HIV-risk behavior, and some of the same psychosocial factors linked to risk-taking also are associated with psychopathology, such as disinhibition, low self-esteem, feelings of powerlessness, and poor interpersonal relationships.6 Risk behavior, however, is associated with externalizing (impulsivity and aggression) more than internalizing (anxiety and depression) problems.7 As many as 30% of adolescents with psychiatric disorders have co-morbid substance abuse, and alcohol and drugs are associated with unprotected sex because they limit teens’ ability to manage affective arousal and make safe decisions.
Sexual Abuse
History of sexual abuse is a correlate of psychopathology and predicts elevated rates of HIV-risk behavior among teens in psychiatric care.24 Sexually abused teens report earlier sexual debut, more frequent sexual activity, and less-consistent condom use than nonabused high school students.25 Abused youths are more likely to have gotten someone pregnant or to have been pregnant and to have engaged in coercive sex. Teens with abuse histories also report lower self-efficacy for condom use, increased concern with conforming to peer sexual norms, anxiety about partner rejection, and more lifetime sexual partners. In role playing by psychiatric inpatient youths, abused teens communicated their views less consistently, clearly, and directly than non-abused teens, and they lacked appropriate assertiveness.
Personality Traits
At least three personality traits are linked to HIV-risk behavior: sensation seeking, attitudes toward health, and achievement orientation. Sensation seeking is associated with less-consistent condom use,26 and greater health concerns are related to decreased risk-taking behavior.27 Increased risk-taking is associated with school failure and low achievement motivation,28 whereas high achievement motivation is linked to delays in sexual activity and fewer cases of early pregnancy.29
Family Context and HIV-Risk
Parents and families play a central role in adolescents’ sexual values, attitudes, and behavior. Four areas of the family context have been associated with youths’ sexual risk-taking and attitudes:
Affective characteristics (warmth, support, hostility);
Instrumental characteristics (monitoring, supervision, control);
Parent-adolescent communication; and
Parental attitudes and behavior.
Affective Characteristics
Postivie affective characteristics of the family mitigate high-risk behavior among teens. Family availability, support, connectedness, and cohesion are related to reduced sexual experience, less risky sexual behavior, and delayed sexual debut.30,31
Instrumental characteristics
Parental monitoring, strictness/permissiveness, and supervision are related to teens’ sexual risk-taking. Parental monitoring reduces opportunities for sexual activity, predicts less risky sex, and is linked to reductions in other high-risk behaviors that often occur with risky sex, such as drug and alcohol use and delinquency. Research with youths in psychiatric care also links teens’sexual behavior to parental monitoring, supervision, and permissiveness, with stronger links for girls than boys.8
Parent-Teen Communication
Positive parent-teen communication about general and sexual topics is related to less sexual experience and reduced risky sex among adolescents. Research suggests a unique relationship between sexual risk-taking and sexual communication between parents and youths in psychiatric care; the most risky teens were those who engaged in equal discussions with their parents, while teens whose parents disagreed with them or were more dominating reported less sexual risk-taking.32 This pattern may reflect poorer boundaries between parents and adolescents in psychiatric care, so when parents act like peers rather than authority figures, these youths engage in more risky behavior.
Parental Attitudes and Behavior
Parents are uniquely positioned to influence their adolescents’ sexual health and development because they are the primary source of sexual socialization and education for their children. Mothers influence their teens’ sexual attitudes and behaviors through verbal messages and their own attitudes and behaviors.33 Compared with women who were older at first child-birth, teen mothers are more likely to have daughters who are sexually active as adolescents, and daughters of teen mothers often become teen moms themselves. The young age of the mother’s sexual debut is strongly associated with her daughter’s becoming sexually active by age 14.
Peer and Partner Relationships and HIV Risk
Peers and romantic partners become increasingly important during adolescence, and perceptions of peer norms exert a strong influence on youths’ sexual behavior. Few studies have examined the influence of romantic or sexual partnerships on adolescent sexual risk-taking because these relationships often are short-lived and sexual intercourse does not necessarily occur. Three areas of peer and partner relationships are especially salient for youths in psychiatric care:
Relationship concerns;
Peer influence; and
Partner communication.
Relationship Concerns
This refers to the desire to maintain relationships regardless of their quality, and valuing relationship stability over other goals (e.g., HIV prevention). Teens may engage in high-risk behavior to serve relationship needs like affiliation, closeness, and intimacy, and to avoid rejection.34 Practicing prevention may be a low priority if it risks partner rejection or disapproval by peers, while engaging in risky behavior may enhance peer approval and/or secure a partner’s love and commitment. Relationship concerns may be especially strong for troubled youths whose interpersonal relationships are unstable and who have difficulty regulating affect. Mental health problems and substance abuse are linked to fear of rejection and difficulty tolerating intimacy.6
Peer Influence
Teens’ sexual behavior often reflects their perceptions of peer norms, and peers are an important source of sexual information. For youths in psychiatric care, the need for peer acceptance is strong, but their peer norms often are inconsistent with safe sex practices.6 Peer norms among delinquent and aggressive youths are related to risky sex and failure to use condoms.7 Peer influence may be higher in the context of negative family relationships; poor family relationships may increase relationship concerns, and these concerns may interfere with risk reduction efforts.
Partner Communication
Increased communication between teenage partners is related to less sexual risk-taking, more HIV prevention self-efficacy, fewer partners, and more-consistent condom use.35 Girls who express a desire to use condoms are more likely to use them, and girls who talk to their partners about their sexual history have fewer partners. Low partner communication and self-efficacy (i.e., perceived inability to practice safe-sex) are related to less-responsible sexual behavior. Fear of rejection may explain teenagers’ poor sexual communication skills and less-open communication with sexual partners. Girls are expected to be passive in sexual relationships and ignorant about sex and condom use.36 Therefore, asking a partner to use a condom is believed to endanger the trust between partners.37
Environmental Circumstances and HIV Risk
Environmental factors affect youths’risk of HIV infection. Variation among communities in rates of alcohol and drug use, sexual behavior, and childbearing38 underscore the critical role of neighborhoods in promoting or discouraging risk behavior. Communities with high rates of AIDS increase risk because sexual partners are more likely to be infected. Neighborhood disadvantage, low socioeconomic status, and stressful life events are related to increased sexual activity, permissiveness, and other high-risk behavior. Financial need reduces access to condoms,39 and early sexual activity is linked to neighborhood disorganization and exposure to community violence. Of note, the presence of a supportive adult can mitigate the impact of stress on risk.40 Commitment to education and regular involvement in church activities also can protect against high-risk behavior.
Conclusion
Vertical transmission of HIV is decreasing steadily while infection among teens is increasing. Youths in psychiatric care are at elevated risk of infection because of their sexual behavior and substance use. Once someone is infected, HIV spreads through the body, including the brain, and causes further progression of neurologic, developmental, and psychiatric conditions. With the advent of aggressive antiretroviral treatment, we have increased survival into the reproductive years and adulthood, but we have not been able to eradicate the virus. The absence of a cure underscores the importance of prevention. We have described a theoretical framework that highlights key areas where mental health clinicians can intervene, such as counseling parents, diagnosing mental health and substance problems, enhancing parent-teen and teen-partner communication, increasing adolescent achievement motivation, and/or closely monitoring the progression of HIV infection. Important risk and protective factors have been identified to guide clinicians’ efforts to stem the epidemic and improve the lives of youths at-risk or infected with HIV.
Learning Objectives.
After reading this issue, the participant should be able to:
Describe the epidemiology of HIV infection among youths.
State the biological concomitants of HIV in youths.
List individual and social factors associated with increased risk of HIV infection in youths.
Footnotes
The opinions expressed in this article by Dr. Pao do not necessarily reflect the opinions of the U.S. Government.
The authors have disclosed that they have no significant relationships with or financial interests in any commercial organizations pertaining to this educational activity.
Contributor Information
Geri R. Donenberg, University of Illinois at Chicago, Institute for Juvenile Research, 840 South Wood (M/C 747), Chicago, IL 60612; gdonenberg@psych.uic.edu.
Maryland Pao, Deputy Clinical Director in the National Institute of Mental Health, NIH, DHHS, Bethesda, MD.
REFERENCES
- 1.Joint United Nations Programme on HIV/AIDS www.unaids.org/worldaidsday/2002/press/Epiupdate.html. [PubMed]
- 2.Pequegnat W, Szapocznik J. The role of families in preventing and adapting to HIV/AIDS: Issues and answers. In: Pequegnat W, Szapocznik J, editors. Working With Families in the Era of HIV/AIDS. Sage Publications; Thousand Oaks, CA: 2000. [Google Scholar]
- 3.Centers for Disease Control and Prevention Young people at risk: HIV/AIDS among America’s youth. 2000 www.cdc.gov/hiv/pubs/facts/youth.pdf.
- 4.Centers for Disease Control and Prevention 1993 revised classification system for HIV infection and expanded AIDS surveillance case definition for adolescents and adults. MMWR Morb Mortal Wkly Rep. 1993;42(RR-17) [Google Scholar]
- 5.Centers for Disease Control and Prevention CDC guidelines for national human immunodeficiency virus case surveillance, including monitoring for human immunodeficiency virus infection and acquired immunodeficiency syndrome. MMWR Morb Mortal Wkly Rep. 1999;48(RR-13):1–36. [PubMed] [Google Scholar]
- 6.Brown LK, Danovsky MB, Lourie KJ, et al. Adolescents with psychiatric disorders and the risk of HIV. J Am Acad Child Adolesc Psychiatry. 1997;36:1609–1617. doi: 10.1016/S0890-8567(09)66573-4. [DOI] [PubMed] [Google Scholar]
- 7.Donenberg GR, Emerson E, Bryant FB, et al. Understanding AIDS-risk behavior among adolescents in psychiatric care: Links to psychopathology and peer relationships. J Am Acad of Child Adolesc Psychiatry. 2001;40:642–653. doi: 10.1097/00004583-200106000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donenberg G, Wilson H, Emerson E, et al. Holding the line with a watchful eye: The impact of perceived parental permissiveness and parental monitoring on risky sexual behavior among adolescents in psychiatric care. AIDS Educ Prev. 2002;14:138–157. doi: 10.1521/aeap.14.2.138.23899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DiClemente RJ, Ponton LE. HIV-related risk behaviors among psychiatrically hospitalized adolescents and school-based adolescents. Am J Psychiatry. 1993;150:324–325. doi: 10.1176/ajp.150.2.324. [DOI] [PubMed] [Google Scholar]
- 10.Baker D, Mossman D. Potential HIV exposure in psychiatrically hospitalized adolescent girls. Am J Psychiatry. 1991;148:528–530. doi: 10.1176/ajp.148.4.528. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. National Center for HIV, STD, and TB Prevention. Divisions of HIV/AIDS Prevention AIDS Surveillance-Trends. www.cdc.gov/hiv/graphics/trends.htm.
- 12.The European Mode of Delivery Collaboration Elective cesarean-section versus vaginal delivery in prevention of vertical HIV-1 transmission: A randomized clinical trial. Lancet. 1999;353:1035–1039. doi: 10.1016/s0140-6736(98)08084-2. [DOI] [PubMed] [Google Scholar]
- 13.The International Perinatal HIV Group The mode of delivery and vertical transmission of human immunodeficiency virus type 1—a meta-analysis of 15 prospective cohort studies. N Engl J Med. 1999;340:977–987. doi: 10.1056/NEJM199904013401301. [DOI] [PubMed] [Google Scholar]
- 14.U.S. Department of Health and Human Service AIDSinfo. www.aidsinfo.nih.gov/guidelines/
- 15.Cooper ER, Hanson C, Diaz C, Women and Infants Transmission Study Group Encephalopathy and progression of human immunodeficiency virus disease in a cohort of children with perinatally acquired human immunodeficiency virus infection. J Pediatr. 1998;132:808–812. doi: 10.1016/s0022-3476(98)70308-7. [DOI] [PubMed] [Google Scholar]
- 16.Llorente A, Brouwers P, Charurat M, et al. Women and Infants Transmission Study Group Early neurodevelopmental markers predictive of mortality in infants infected with HIV-1. Dev Med Child Neurol. 2003;45:76–84. [PubMed] [Google Scholar]
- 17.Mitchell W. Neurological and developmental effects of HIV and AIDS in children and adolescents. Ment Retard Dev Disabil Res Rev. 2001;7:211–216. doi: 10.1002/mrdd.1029. [DOI] [PubMed] [Google Scholar]
- 18.Watkins JM, Cool VA, Usner D, et al. Attention in HIV-infected children: Results from the Hemophilia Growth and Development Study. J Int Neuropsychol Soc. 2000;6:443–454. doi: 10.1017/s1355617700644028. [DOI] [PubMed] [Google Scholar]
- 19.Brouwers P, DeCarli C, Tudor-Williams G, et al. Interrelations among patterns of change in neurocognitive, CT brain imaging, and CD4 measures associated with anti-retroviral therapy in children with symptomatic HIV infection. Adv Neuroimmunol. 1994;4:223–231. doi: 10.1016/s0960-5428(06)80260-3. [DOI] [PubMed] [Google Scholar]
- 20.Patsalides AD, Wood LV, Atac GK, et al. Cerebrovascular disease in HIV-infected pediatric patients: Neuroimaging findings. AJR Am J Roentgenol. 2002;179:999–1003. doi: 10.2214/ajr.179.4.1790999. [DOI] [PubMed] [Google Scholar]
- 21.Brown LK, Reynolds LA, Lourie KJ. A pilot HIV prevention program for adolescents in a psychiatric hospital. Psychiatr Serv. 1997;48:531–533. doi: 10.1176/ps.48.4.531. [DOI] [PubMed] [Google Scholar]
- 22.Cicchetti D, Ackerman BP, Izard CE. Emotions and emotion regulation in developmental psychopathology. Dev Psychopathol. 1995;7:1–10. [Google Scholar]
- 23.Tice DM, Bratslavsky E, Baumeister RF. Emotional distress regulation takes precedence over impulse control: If you feel bad, do it! J Pers Soc Psychol. 2001;80:53–67. [PubMed] [Google Scholar]
- 24.Brown LK, Kessel SM, Lourie KJ, et al. Influence of sexual abuse on HIV-related attitudes and behaviors in adolescent psychiatric inpatients. J Am Acad Child Adolesc Psychiatry. 1997;36:316–322. doi: 10.1097/00004583-199703000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Lodico M, DiClemente R. The association between childhood sexual abuse and prevalence of HIV-related risk behaviors. Clin Pediatr (Phila) 1994;33:498–502. doi: 10.1177/000992289403300810. [DOI] [PubMed] [Google Scholar]
- 26.Brown LK, DiClemente RJ, Park T. Predictors of condom use in sexually active adolescents. J Adolesc Health. 1992;13:651–657. doi: 10.1016/1054-139x(92)90058-j. [DOI] [PubMed] [Google Scholar]
- 27.Costa FM, Jessor R, Fortenberry JD, et al. Psychosocial conventionality, health orientation, and contraceptive use in adolescence. J Adolesc Health. 1996;18:404–416. doi: 10.1016/1054-139X(95)00192-U. [DOI] [PubMed] [Google Scholar]
- 28.DiClemente RJ, Lodico M, Grinstead OA, et al. African-American adolescents residing in high-risk urban environments do use condoms: Correlates and predictors of condom use among adolescents in public housing developments. Pediatrics. 1996;98:269–278. [PubMed] [Google Scholar]
- 29.Brooks-Gunn J, Guo G, Furstenburg FF. Who drops out of and who continues beyond high school? A 20-year follow-up of black urban youth. J Res Adolesc. 1993;3:271–294. [Google Scholar]
- 30.Donenberg G, Bryant F, Emerson E, et al. Tracing the roots of early sexual debut among adolescents in psychiatric care. J Am Acad of Child Adolesc Psychiatry. 2003;42:594–608. doi: 10.1097/01.CHI.0000046833.09750.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fisher L, Feldman SS. Familial antecedents of young adult health risk behavior: A longitudinal study. J Fam Psychol. 1998;12:66–80. [Google Scholar]
- 32.Wilson HW, Donenberg G. Quality of parent communication about sex and its relationship to mentally ill adolescents’ risky sexual behavior. J Child Psychol Psychiatry. doi: 10.1111/j.1469-7610.2004.00229.x. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wickrama K, Conger RD, Wallace LE, et al. The intergenerational transmission of health-risk behaviors: Adolescent lifestyles and gender moderating effects. J Health Soc Behav. 1999;40:258–272. [PubMed] [Google Scholar]
- 34.Cochran S, Mays V. Women and AIDS-related concerns. Roles for psychologists in helping the worried well. Am Psychol. 1989;44:529–535. doi: 10.1037//0003-066x.44.3.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Whitaker DJ, Miller KS, May DC, et al. Teenage partners’ communication about sexual risk and condom use: The importance of parent-teenager discussions. Fam Plann Perspect. 1999;31:117–121. [PubMed] [Google Scholar]
- 36.Brooks-Gunn J, Paikoff RL. Sex is a gamble, kissing is a game: Adolescent sexuality and health promotion. In: Millstein SG, Petersen AC, Nightingale EO, editors. Promoting the Health of Adolescents: New Directions for the Twenty-First Century. Oxford University Press; New York: 1993. pp. 180–208. [Google Scholar]
- 37.Eyre SL, Auerswald C, Hoffman V, et al. Fidelity management: African-American adolescents’ attempts to control the sexual behavior of their partners. J Health Psychol. 1998;3:393–406. doi: 10.1177/135910539800300308. [DOI] [PubMed] [Google Scholar]
- 38.National Research Council . Losing Generations: Adolescents in High-Risk Settings. National Academy Press; Washington, DC: 1993. [Google Scholar]
- 39.Stiffman AR, Dore P, Cunningham RM. Inner-city youths and condom use: Health beliefs, clinic care, welfare, and the HIV epidemic. Adolescence. 1994;29:805–820. [PubMed] [Google Scholar]
- 40.Wills TA, Vaccaro D, McNamara G. The role of life event, family support, and competence in adolescent substance use: A test of vulnerability and protective factors. Am J Community Psychol. 1992;20:349–374. doi: 10.1007/BF00937914. [DOI] [PubMed] [Google Scholar]
- 41.Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Dev Psychol. 1986;22:723–742. [Google Scholar]
- 42.Henggeler S, Borduin C. Family therapy and beyond: A multisystemic approach to treating the behavior problems of children and adolescents. Brooks/Cole; California: 1990. [Google Scholar]