Abstract
A patient with a large periapical lesion in relation to the maxillary right central and lateral incisors is presented here. During the conservative root canal treatment, aspiration of the fluid was done through the root canal, followed by placement of triple antibiotic paste for two weeks. Complete periapical healing was observed at the 24-month recall. This report confirms that for treatment of a large periapical lesion it is not always necessary to do surgical treatment and even cyst-like periapical lesions heal following conservative endodontic therapy.
Keywords: Healing, nonsurgical, periapical lesion
INTRODUCTION
Traumatic injuries generally disrupt the pulpal blood supply causing pulp necrosis and leading to anaerobic conditions favorable for the growth of opportunistic microorganisms, which may subsequently result in the development of periapical lesions.[1] Periapical lesions generally represent an inflammatory response to invasion of the root canal system by microorganisms and their by-products. Such lesions grow via a variety of mechanisms, including osmotic fluid accumulation in the lumen, epithelial proliferation, and molecular mechanisms (Nair, 1998).[2] Thus, if the lesion is effectively evacuated of the inflammatory exudates, so as to reduce the hydrostatic pressure, and if the microbiological etiology is removed by nonsurgical root canal treatment, these lesions may regress by the mechanisms of apoptosis.[3] Various techniques have been proposed for reducing hydrostatic pressure, such as, the decompression technique (Loushine et al., 1991, Martin et al., 2007),[4,5] aspiration-irrigation technique (Hoen et al., 1990),[6] and aspiration through the root canal system,[7] which may result in a shrinkage of the lesion.
Elimination of the microorganisms, in case of large periapical lesions, has been a challenge for the clinician. The polymicrobial infection makes sterilization of the root canal system difficult. As a consequence, the endodontic treatment may fail if the root canal treatment has not adequately eliminated or reduced the intraradicular burden, leading to persistent infections.[8] Mechanical instrumentation alone is unable to completely eradicate the root canal system from bacteria. Therefore, some form of chemical irrigation and disinfection is necessary to optimally disinfect the root canal system. Various medicaments have been widely advocated to help eliminate bacteria, reduce periapical inflammation and pain, and induce healing. Calcium hydroxide has been commonly used as an intracanal medicament, however, it has been reported that it is not effective in disinfecting the root canal system associated with persistent endodontic infections.[9]
Various combinations of antibiotics have also been used and among them a mixture of ciprofloxacin, metronidazole, and minocycline has been shown to be very effective in eliminating endodontic pathogens in vitro and in situ.[10,11] This combination is commonly referred to as triple antibiotic paste. Ozan and Er have found that a combination of antibiotic drugs (metronidazole, ciprofloxacin, and minocycline), when used as antibacterial dressing, is successful in healing large cyst-like periradicular lesions.[12]
This case report describes the nonsurgical management of a large persistent periapical lesion by decompression and aspiration of fluid through the root canal space, with subsequent application of triple antibiotic paste.
CASE REPORT
A 21-year-old male patient, with no relevant medical history, presented with a painful recurrent swelling, since six months, on the front right side of the upper jaw. The patient gave a history of trauma to the maxillary anterior teeth 10 years prior. He had undergone root canal treatment twice, at an interval of two years, for the same.
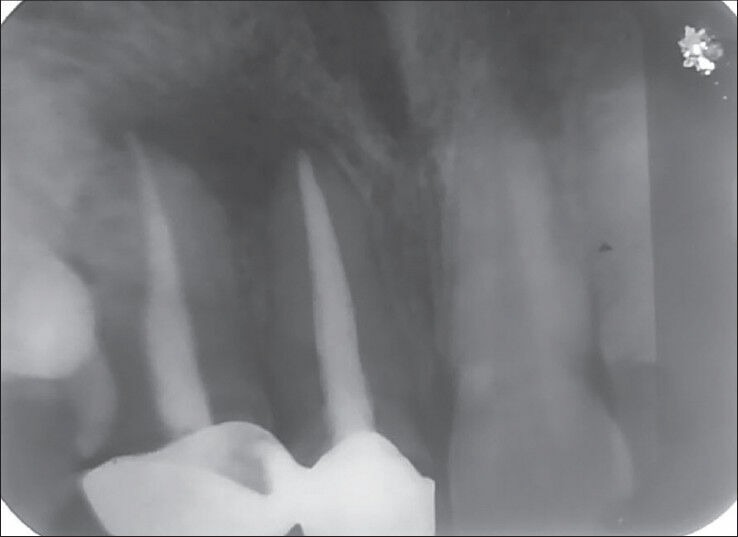
Intraoral examination revealed a painful swelling of the palatal mucosa, adjacent to teeth 11 and 12. There was moderate pain on palpation in relation to the labial side of tooth 11. A radiographic evaluation demonstrated poorly obturated root canals in relation to 11 and 12. There was a large radiolucent lesion with a uniform radiolucency and well-defined margins involving the apices of these teeth [Figure 1].
Figure 1.
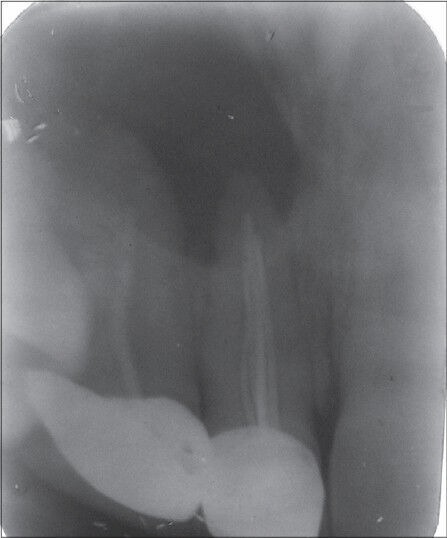
Preoperative radiograph
Taking into account the medical and dental history of the patient, a presumptive diagnosis of periapical cyst was established. Nonsurgical endodontic retreatment was planned, to treat the involved teeth.
Following access cavity preparation and gutta-percha removal, there was drainage of straw-colored fluid from tooth 11. When the drainage ceased, the apical foramen for both teeth was gauged using hand K-files and the apical width was found to be equivalent to size 45 for tooth 11 and size 30 for tooth 12 [Figure 2]. The root canals were prepared using K-files, until the final preparation sizes of 60 and 40, respectively, for 11 and 12, were achieved. Apical patency was maintained throughout the procedure. During the preparation, the canals were thoroughly irrigated with 3% sodium hypochlorite (NaOCl) and normal saline. The final irrigation was performed with 2% Chlorhexidine (CHX) and the access cavity was temporarily sealed with Cavit G. The patient was prescribed analgesics for three days and was advised warm saline rinses.
Figure 2.
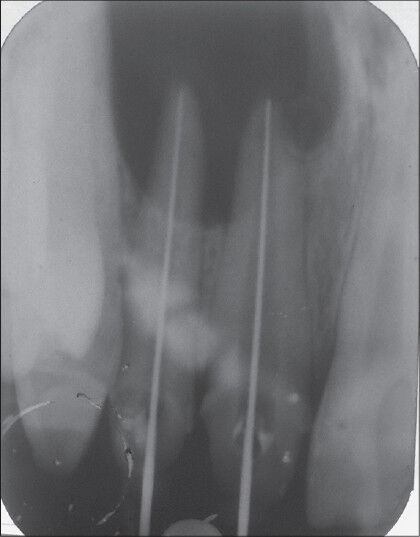
Working length radiograph
The next day, when the patient came, the swelling had decreased. The canals were again copiously irrigated and filled with a paste of calcium hydroxide Ca(OH)2 mixed with 2% CHX. The intracanal dressing was to be reviewed after one week, but the patient reported back in two days with a recurrence of swelling. The pain on palpation in the labial vestibule was still present. After irrigating the canals, the intracanal Ca (OH)2 dressing was again repeated for one week. There was no decrease in the swelling or pain even after the second change of dressing.
The root canal was again debrided and irrigated. A 25-guage needle attached to a 5 ml syringe was inserted through the root canal, past the apical foramen, into the bony cavity. Approximately 5 ml of the fluid was aspirated while simultaneous digital pressure was applied on the labial and palatal cortical plates. After irrigating and drying the cavity, Ca (OH)2 paste was again placed in the canal.
At the next appointment after one week, there was considerable decrease in the swelling, but the pain in the labial vestibule still remained on palpation. The canals were again debrided, irrigated, aspirated, and it was decided to fill triple antibiotic paste in the canal. After two days, the patient reported with absence of pain and swelling, but a slight discomfort on palpation on the labial side. The patient was asymptomatic when re-examined after one week.
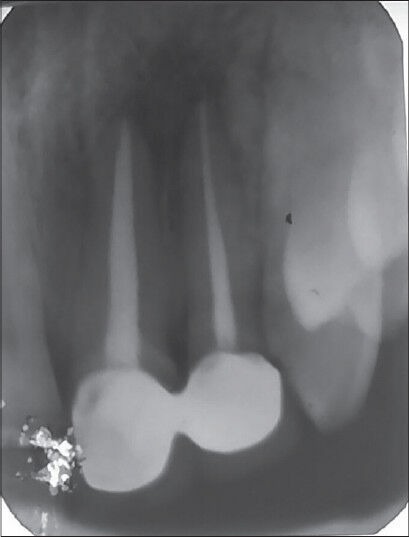
The dressing was left undisturbed for another one week, after which the canals were obturated with gutta-percha and zinc oxide eugenol cement sealer [Figure 3].
Figure 3.
Immediate postoperative radiograph
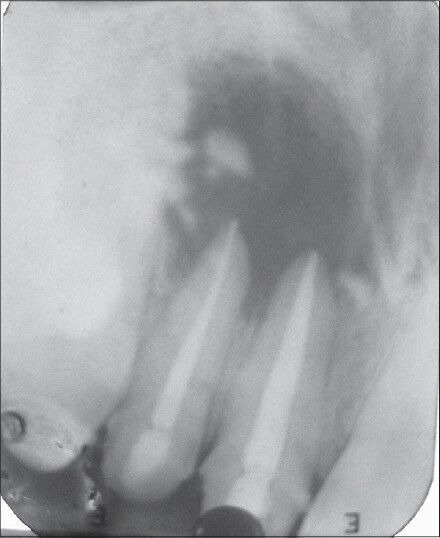
The patient was recalled after a three-month interval. However, the patient turned up only after one year. The clinical and radiographic examination demonstrated that the patient was asymptomatic and exhibited proper integrity of the periodontal tissues after one year [Figures 4 and 5].
Figure 4.
Postoperative one year
Figure 5.
Postoperative one year three months
DISCUSSION
There is clinical evidence that as the periapical lesions increase in size, the proportion of the radicular cysts increases.[13] The incidence of a cyst within the periapical lesions varies between 6 and 55%. However, some large lesions may be granulomas or may have a direct communication with the root canal system (apical pocket cyst or bay cyst) and respond favorably to nonsurgical treatment.[14] On the other hand, true cysts are completely enclosed by the lining epithelium and may be attached to the root apex by a cord of epithelium.[15] In the past, it was considered that true cysts would not respond to root canal treatment alone and that surgery was always required. However, in recent years, there is greater awareness of the root canal morphology, and the development of newer instruments, techniques, and materials has greatly enhanced the clinician's abilities.[16] Of late, it has been proved that if the lesion is effectively evacuated of the inflammatory exudates and the microbial load is reduced with an effective intracanal medicament, it is possible to stimulate the immunological system to induce repair, even in cystic lesions.[17] Considering all this, nonsurgical root canal treatment should always be the first choice in cases of non-vital teeth with infected root canals. Elimination of bacteria from the root canal is the most important factor for the successful treatment of periapical lesions, and the lack of regression of such lesions is generally assigned to the persistence of bacteria inside the root canal.[8] In the present case, failure of the root canal treatment twice before the patient presented to our clinic could be attributed to the improper debridement and disinfection. Moreover, poor obturation of the root canals allowed leakage and more bacterial contamination. A presumptive diagnosis of a periapical cyst was made on the basis of the radiographic features and the presence of straw-colored fluid.
Aspiration through the root canal system is a simple technique that reduces the hydrostatic pressure without causing additional discomfort to the patient.[7] The aspiration technique was used in this case by inserting a 25 gauge needle just beyond the root apex in tooth 11, so as to reduce the hydrostatic pressure. During aspiration, digital pressure was applied on the labial and palatal cortical plates that aided in reducing the size of the swelling. It is important to apply digital pressure throughout the procedure so as to avoid entrapment of air in the bony cavity, which can result in increased intra-bony pressure.
The role of intracanal medicament cannot be underestimated in the eradication of the bacteria, as chemomechanical preparation alone is not enough to predictably eliminate all the bacteria, and a small portion of the flora survives. To date, calcium hydroxide has been considered the gold standard for optimally disinfecting root canals. It has been proved to be a reliable and effective means of canal disinfection in cases of primary apical periodontitis.[18] However, its role in the elimination of the bacteria associated with persistent apical infections is controversial. Bacteria associated with persistent apical infections have the ability to invade the dentinal tubules and buffer the high pH produced by calcium hydroxide. In addition, dentin has also been found to have a buffering effect,[19] further compromising the antimicrobial effect of calcium hydroxide.[20] All these may be the possible reasons for persistent swelling and pus discharge from the root canals after calcium hydroxide dressing.
Use of antimicrobial agents has been suggested by various authors for the eradication of bacteria associated with persistent endodontic infections. Due to the potential risk of adverse effects following systemic application, and the ineffectiveness of systemic antibiotics in necrotic pulpless teeth and periradicular tissues, the local application of antibiotics may be a more effective mode for delivery in endodontics.[21] Application of a single antibiotic may be ineffective in the sterilization of the canal due to the vast microflora harboring the root canal system, consisting of both aerobic and anerobic bacteria.[11] To overcome these obstacles, the concept of ‘Lesion Sterilization and Tissue Repair (LSTR)’ by the Cariology Research Unit of the Niigata University School of Dentistry, was developed. This uses a triple antibiotic paste of ciprofloxacin, metronidazole, and minocycline, for disinfection.[22] It has been shown that this combination of drugs can kill any bacteria in the carious lesions, necrotic pulp, infected root dentin, and periapical lesions.[10,11] Even in the present case, there was a remarkable reduction in the symptoms after the use of triple antibiotic paste. The swelling did not recur in the 14-day course of the dressing and when the dressing was removed, no pus discharge was observed.
Even though a very low dose of the drug combination is required for topical application, one should consider that unnecessary, inadequate, and lengthy application of antibacterial drugs may induce drug-resistant bacteria. Other case reports have also demonstrated healing with this combination of antibiotic paste, but they have used the drug for one to three months.[20] Contradictory to this, in our case, the patient was comfortable within one week of placement of the triple antibiotic paste, although we allowed it to remain for two weeks. Early resolution of symptoms after placement of the triple antibiotic paste, in our case, could be attributed to additional use of the aspiration technique.
However, if the topical application of the drug is preceded by the noninvasive technique of decompression and aspiration through the root canal system in order to reduce the hydrostatic pressure of the confined fluid, it may help to decrease the application time of the drug mixture.
CONCLUSION
In this case report, it is seen that a large periapical cyst-like lesion has healed by nonsurgical root canal treatment, using intracanal aspiration and triple antibiotic paste. This confirms that even large periapical lesions can respond favorably to nonsurgical treatment, and therefore, it must always be the first treatment of choice.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Soares J, Santos S, Silveira F, Nunes E. Nonsurgical treatment of extensive cyst-like periapical lesion of endodontic origin. Int Endod J. 2006;39:566–75. doi: 10.1111/j.1365-2591.2006.01109.x. [DOI] [PubMed] [Google Scholar]
- 2.Nair PN. New perspectives on radicular cysts: Do they heal? Int Endod J. 1998;31:155–60. doi: 10.1046/j.1365-2591.1998.00146.x. [DOI] [PubMed] [Google Scholar]
- 3.Lin LM, Ricucci D, Lin J, Rosenberg PA. Nonsurgical root canal therapy of large cyst-like inflammatory periapical lesions and inflammatory apical cysts. J Endod. 2009;35:607–15. doi: 10.1016/j.joen.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 4.Loushine RJ, Weller RN, Bellizzi R, Kulild JC. A 2-day decompression: A case report of a maxillary first molar. J Endod. 1991;17:85–7. doi: 10.1016/S0099-2399(06)81614-6. [DOI] [PubMed] [Google Scholar]
- 5.Martin SA. Conventional endodontic therapy of upper central incisor combined with cyst decompression: A case report. J Endod. 2007;33:753–7. doi: 10.1016/j.joen.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 6.Hoen MM, LaBounty GL, Strittmatter EJ. Conservative treatment of persistent periradicular lesions using aspiration and irrigation. J Endod. 1990;16:182–6. doi: 10.1016/S0099-2399(06)81968-0. [DOI] [PubMed] [Google Scholar]
- 7.Fernandes M, De Ataide I. Non-surgical management of a large periapical lesion using a simple aspiration technique: A case report. Int Endod J. 2010;43:536–42. doi: 10.1111/j.1365-2591.2010.01719.x. [DOI] [PubMed] [Google Scholar]
- 8.Leonardo MR, Leal JM. Endodontics: Root canal treatment. 3rd ed. São Paulo: Médica Panamericana; 1998. [Google Scholar]
- 9.Leonardo MR, Hemandez ME, Silva LA, Tanomaru-Filho M. Effect of a calcium hydroxide-based root canal dressing on periapical repair in dogs: A histological study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:680–5. doi: 10.1016/j.tripleo.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 10.Sato I, Ando-Kurihara N, Kota K, Iwaku M, Hoshino E. Sterilization of infected root- canal dentine by topical application of a mixture of ciprofloxacin, metronidazole and minocycline in situ. Int Endod J. 1996;29:118–24. doi: 10.1111/j.1365-2591.1996.tb01172.x. [DOI] [PubMed] [Google Scholar]
- 11.Hoshino E, Kurihara-Ando N, Sato I, Uematsu H, Sato M, Kota K, et al. In vitro antibacterial susceptibility of bacteria from infected root dentin to a mixture of ciprofloxacin, metronidazole and minocycline. Int Endod J. 1996;29:125–30. doi: 10.1111/j.1365-2591.1996.tb01173.x. [DOI] [PubMed] [Google Scholar]
- 12.Özan Ü, Er K. Endodontic treatment of a large cyst-like periradicular lesion using a combination of antibiotic drugs: A case report. J Endod. 2005;31:898–900. doi: 10.1097/01.don.0000164129.74235.8e. [DOI] [PubMed] [Google Scholar]
- 13.Fernandes M, De Ataide I. Nonsurgical management of Periapical lesions. J Conserv Dent. 2010;13:240–5. doi: 10.4103/0972-0707.73384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramachandran Nair PN, Pajarola G, Schroeder HE. Types and incidence of human periapical lesions obtained with extracted teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81:93–102. doi: 10.1016/s1079-2104(96)80156-9. [DOI] [PubMed] [Google Scholar]
- 15.Lin LM, Huang GT, Rosenberg PA. Proliferation of epithelial cell rests, formation of apical cysts, and regression of apical cysts after periapical wound healing. J Endod. 2007;33:908–16. doi: 10.1016/j.joen.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 16.Saatchi M. Healing of large periapical lesion: A non-surgical endodontic treatment approach. Aust Endod J. 2007;33:136–40. doi: 10.1111/j.1747-4477.2007.00061.x. [DOI] [PubMed] [Google Scholar]
- 17.Broon NJ, Bortoluzzi EA, Bramante CM. Repair of large periapical radiolucent lesions of endodontic origin without surgical treatment. Aust Endod J. 2007;33:36–41. doi: 10.1111/j.1747-4477.2007.00046.x. [DOI] [PubMed] [Google Scholar]
- 18.Portenier I, Haapasalo H, Rye A, Waltimo T, Orstavik D, Haapasalo M. Inactivation of root canal medicaments by dentine, hydroxylapatite and bovine serum albumin. Int Endod J. 2001;34:184–8. doi: 10.1046/j.1365-2591.2001.00366.x. [DOI] [PubMed] [Google Scholar]
- 19.Haapasalo HK, Siren EK, Waltimo TM, Orstavik D, Haapasalo MP. Inactivation of local root canal medicaments by dentine: An in vitro study. Int Endod J. 2000;33:126–31. doi: 10.1046/j.1365-2591.2000.00291.x. [DOI] [PubMed] [Google Scholar]
- 20.Taneja S, Kumari M. Use of triple antibiotic paste in the treatment of large periradicular lesions. J Investig Clin Dent. 2011;3:72–6. doi: 10.1111/j.2041-1626.2011.00082.x. [DOI] [PubMed] [Google Scholar]
- 21.Mohammadi Z, Abbott PV. On the local applications of antibiotics and antibiotic-based agents in endodontics and dental traumatology. Int Endod J. 2009;42:555–67. doi: 10.1111/j.1365-2591.2009.01564.x. [DOI] [PubMed] [Google Scholar]
- 22.Hoshino E, Takushige T. LSTR 3Mix-MP method- better and efficient clinical procedures of lesion sterilization and tissue repair (LSTR) therapy. Dent Rev. 1998;666:57–106. [Google Scholar]


