Abstract
Obesity is a significant problem affecting United States (US) firefighters. While body mass index (BMI) is widely used to diagnose obesity, its use for this occupational group has raised concerns about validity. We examined rates and types of misclassification of BMI-based obesity status compared to body fat percentage (BF%) and waist circumference (WC). Male career firefighters (N = 994) from 20 US departments completed all three body composition assessments. Mean BMI, BF%, and WC were 29 kg/m2, 23%, and 97 cm, respectively. Approximately 33% and 15% of BF%- and WC-defined obese participants were misclassified as non-obese (false negatives) using BMI, while 8% and 9% of non-obese participants defined by BF% and WC standards were identified as obese (false positives) using BMI. When stratified by race/ethnicity, Pacific Islanders showed high rates of false positive misclassification. Precision in obesity classification would be improved by using WC along with BMI to determine firefighters' weight status.
Keywords: body fat, BMI, firefighters, obesity, waist circumference
1. Introduction
Firefighters in the US experience high rates of obesity (ranging from 30%-40%) that are similar to that found among US adults [1,2]. In addition, studies demonstrate that firefighters experience insidious weight gains throughout their career of approximately 0.5 kg (1.1lb) to 1.6 kg (3.5lb) per year [3,4]. It also has been demonstrated that overweight and obesity results in greater risk for injury, injury-related absenteeism, disability, cardiovascular-related disability, and risk for sudden cardiac death [5–8].
For several decades, Body Mass Index (BMI; kg/m2) has been used to diagnose obesity and it is widely recommended as a method for matching individuals to weight loss interventions in clinical practices and is widely used in obesity research [9,10]. However, this method has raised questions regarding how well it reflects body composition, specifically with regard to distinguishing lean and fat mass in fitter or more athletic populations. Consequently, individuals in occupational groups who may have greater muscle mass such as athletes, police officers, or firefighters may be at greater risk for being misclassified as overweight or obese when using BMI [11,12].
Because the nature of the firefighting profession, firefighters need to maintain high levels of health and fitness given the rigorous physical and mental job requirements. However, several studies have documented high rates of substandard fitness among firefighters [2,14]. While there have been concerns expressed about the accuracy of BMI-based obesity classification for firefighters, we found that rates of false positives (i.e., labeling someone as obese based on BMI when they are not based on Body Fat Percentage (BF%; 2.9%) or Waist Circumference (WC; 9.8%) were very low. Unfortunately, while this sample was population-based, it was restricted to the Midwestern part of the US and lacked racial/ethnic diversity [2]. Thus, it is unknown how well BMI accurately characterizes obesity (BMI ≥30) when compared with BF%- and WC-determined weight status in a larger, more diverse, and national sample. The purpose of this study was to compare BMI-based obesity status with comparable BF% and WC standards [9,10,13] and examine rates and types of misclassification.
2. Materials and methods
Data for this study were collected between May 2010 and December 2011 from the baseline evaluation of a longitudinal cohort study examining the impact of wellness and fitness program on health and safety in career firefighters. Poston et al [14] provides details about selection and recruitment of participants. The study was approved by the National Development and Research Institutes (NDRI) and the University of Texas Houston Health Sciences Center (UTHHSC) Institutional Review Boards.
Twenty fire departments across the US and its territories were purposively sampled [15] to serve the primary aim of the parent study, which was to identify two groups of US fire departments, those with (n = 10) and without (n = 10) strong and comprehensive firefighter wellness programs. A total sample of 994 male firefighters with complete baseline anthropometric data was included in this analysis. Women were excluded because they represented less than 5% of the sample, which is consistent with the national fire service [16], thus precluding us from reliably examining gender differences.
Participants completed demographic and occupational history questionnaires. Anthropometric data including height, weight, BMI, BF%, and WC were assessed by trained investigators using current standards [9,10,13]. Height was assessed with a portable stadiometer. Participants were weighed while wearing light clothing and without shoes or socks. Body weight and BF% were determined using foot-to-foot bioelectrical impedance (Tanita 300, Tanita Corporation of America, Inc., IL), which has demonstrated concurrent validity DEXA [2,14]. WC was determined using a spring-loaded nonstretchable tape measure in accordance with recommendations current obesity guidelines [9,10,13]. BMI was computed as weight (kg) divided by height in meters squared (m2). Participants were categorized as non-obese or obese based on standard cutoffs, i.e., BMI ≥ 30 kg/m2, BF% > 25%, and WC > 102 cm [9,10].
3. Results
Overall, participants were in their late 30s (39.2 ± 8.8), married (76.9%), had at least some college education (90.5%), and had annual household income of more than $50,000 (92.0%). The majority of participants was Caucasian (67.3%), was firefighters, firefighter/paramedics, or firefighter/drivers/operators (73.9%), worked in 24-hr shift (84.7%), and had average of 14 (±8.6) years of fire service. Stratified by race/ethnicity, our cohort was comprised of Caucasian (67.3%), African-Americans (4.4%), Pacific Islander (7.8%), Hispanic (13.0%), and other race/ethnicity (7.5%). On average, the mean BMI, BF%, and WC of this cohort were 28.6 kg/m2, 23.2%, and 97.3 cm, respectively. Obesity classification by BMI (≥30 kg/m2), BF% (>25%), and WC (>102 cm) standards indicated that obesity rates estimated by BMI and WC were much lower than those derived from BF% (29.9% and 27.7% compared to 38.1%, respectively). Correlations between BMI and BF%, and WC were high and statistically significant (rBMI-WC = 0.742; rBMI-BF% = 0.626; rBF%-WC = 0.619; all p < 0.001).
Rates of false positives and false negatives for comparing BF% and WC standards to the BMI-based obesity are shown in Table 1.
Table 1.
Rates of false positives and negatives using BMI-based obesity classification and comparable body fat (BF%) and waist circumference (WC) categories
| Obesity status | BF% standard∗ |
Types and rates of misclassification | |
|---|---|---|---|
| Obese | Nonobese | ||
| Obese (BMI ≥ 30.0) | 247 | 45 | False positive (15.4%) |
| Nonobese (BMI < 30.0) | 124 | 557 | False negative (18.2%) |
| Obesity status | WC standard∗ |
Types and rates of misclassification | |
|---|---|---|---|
| Obese | Nonobese | ||
| Obese (BMI ≥ 30.0) | 234 | 66 | False positive (22.0%) |
| Nonobese (BMI < 30.0) | 40 | 649 | False negative (5.8%) |
For each analysis, either BF% or WC categories serve as the standards and BMIbased categories as the “screening test”; cutpoints for BF% and WC from current standards [9,10].
Approximately 33% and 15% of BF%- and WC-defined obese participants were misclassified as non-obese using BMI (i.e., false negatives). On the other hand, 8% and 9% of non-obese participants defined by BF% and WC standards were identified as obese using BMI (i.e., false positives). We next examined the distributions of BF% and WC of these groups and found that the majority of those misclassified as false positives had BF% and WC values at the upper end of non-obese range for both indices (i.e., BF% between 18% - 24%, and WC between 94 cm - 102 cm) [9,10]; see Table 2), demonstrating that most false positives based on BMI were close to the obesity threshold for BF% or WC. BMI was slightly more accurate for correctly identifying participants' weight status when WC-based obesity was the standard (89%) than when using BF% as the standard (83%).
Table 2.
Number and percent of participants misclassified as false positives using BMI stratified by BF% and WC categories
| False positives, n (%) | Nonobese, based on the BF% definition (n = 45) |
|||
|---|---|---|---|---|
| Essential fat (2–5%) | Athlete (6–13%) | Fitness (14–17%) | Average (18–24%) | |
| 0 (0.0) | 1 (2.2) | 6 (13.3) | 38 (84.4) | |
| False positives, n (%) | Nonobese, based on the WC definition (n = 66) |
|
|---|---|---|
| Normal (< 94 cm) | High Risk (94–102 cm) | |
| 9 (13.6) | 57 (86.4) | |
Figs. 1 and 2 present the percentage of false negatives and false positive for BMI-based obesity classification when compared with BF% and WC as standards stratified by race/ethnicity. Caucasian, African-American, and Hispanic male firefighters showed higher rates of false negatives than false positives for BMI-defined obesity when compared with BF%-defined obesity, indicating that they were likely to be misidentified as not obese based on BMI when they were obese based on BF%. In contrast, Pacific Islanders participants were more likely to be misclassified as being obese when using BMI when they were not based on BF%. False negative and false positive rates when comparing BMI to WC classification demonstrated that all minority groups had a similar pattern of higher false positive rates. However, Caucasians were more likely to be misidentified as not obese based on BMI when they actually were obese based on WC. In addition, Pacific Islanders had statistically significant higher false positive rates than the other minority groups.
Fig. 1.
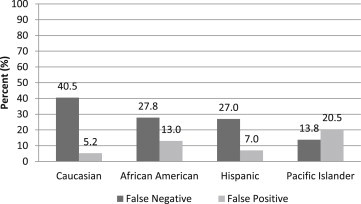
BMI-based false positive and negative rates by race and ethnicity using BF% as the Standard.
Fig. 2.
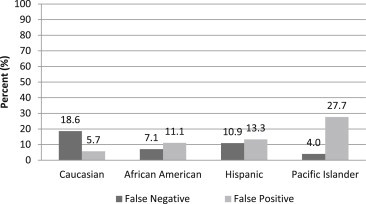
BMI-based false positive and negative rates by race and ethnicity using WC as the Standard.
4. Discussion
The purpose of this study was to examine the accuracy of BMI-determined obesity status when compared with BF% and WC standards in a large, racially and ethnically diverse, and national sample of fire service personnel. On average, firefighters' mean BMI was 28.6 kg/m2, which classified them in the overweight category. Similarly, BF% and WC values at 23.2%, and 97.3 cm placed them in the average BF% and high risk WC categories. However, when using standard obesity status cutoffs for BMI (≥30 kg/m2), BF% (>25), and WC (>102 cm), 28-38% of participants were classified as obese. The prevalence of obesity using BF% was higher than that estimated by BMI and WC methods.
Comparing BMI categories to analogous BF% categories resulted in low rates of false positives (7.5%) but relatively high rates of false negative (33.4%). However, using WC as the standard yielded a different patterns of results, which showed low rates of false positives (9.2%) and moderate rates of false negatives (14.6%), which was similar to our previous studies [2,12]. BMI has been widely used to define obesity status in numerous epidemiologic studies including those from the fire service and related occupational groups [5–7,11,12,17,18]. While concerns have been raised about the potential for high rates of false positive misclassification, our data suggest that most firefighters who are misclassified as obese using BMI are near the obesity thresholds for WC and BF%, which in line with our previous study [12].
When stratified by race/ethnicity, Pacific Islander participants showed high rates of false positive misclassification when BMI was compared to BF% and WC standards. Several studies have demonstrated that Pacific Islanders have different fat distribution (e.g., low fat-to-fat-free mass ratio) compared to Caucasians and African Americans [19,20]. The high likelihood of Pacific Islander participants being misclassified as obese when using BMI might result in overestimating their morbidity and disability risks, so it would be prudent to also measure WC or BF% in this group. False negative misclassification based on BMI also can jeopardize firefighters' health by underestimating weight-related health problems and fitness performances [2].
Strengths of this study include the use of multiple body composition measures administered by trained professionals in a national, large, and racially/ethnically diverse cohort. Several limitations also should be noted. First, only male firefighters' data were analyzed; therefore, the results cannot be extended to female firefighters. Second, we also did not have sufficient racial diversity to examine misclassification among Asians or Native Americans. Third, bioelectrical impedance was used to estimate BF% which is suitable for field assessments but it is not the gold standard for assessing BF%. However, our BF% method has demonstrated concurrent validity with DEXA (dual energy X-ray absorptiometry) [2].
In conclusion, BMI was most accurate when compared to WC as the standard (i.e., overall accuracy = 89%). However, to minimize misclassification, it would be prudent to use either WC or BF% along with BMI in order to classify obesity status among firefighters properly.
Conflicts of interest
No potential conflicts of interest related to this article were reported.
Acknowledgments
This study was supported by the Federal Emergency Management Agency in the Department of Homeland Security [EMW-2009-FP-01971]. The authors would like to thank all of the firefighters and their fire departments for participating in this study.
Footnotes
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Contributor Information
Nattinee Jitnarin, Email: jitnarin@ndri.org.
Walker S.C. Poston, Email: poston@ndri.org.
Christopher K. Haddock, Email: haddock@ndri.org.
Sara A. Jahnke, Email: Jahnke@ndri.org.
Rena S. Day, Email: Rena.S.Day@uth.tmc.edu.
References
- 1.Flegal K.M., Carroll M.D., Ogden C.L., Curtin L.R. Prevalence and trends in obesity among US adults, 999-2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Poston W.S.C., Haddock C.K., Jahnke S.A., Jitnarin N., Tuley B.C., Kales S.N. The prevalence of overweight, obesity, and substandard fitness in a population-based firefighter cohort. J Occup Environ Med. 2011;53:266–273. doi: 10.1097/JOM.0b013e31820af362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elliot D.L., Goldberg L., Kuehl K.S., Moe E.L., Breger R.K., Pickering M.A. The PHLAME (Promoting Helathy Lifestyles: Alternative models’ Effects) firefighter study: outcomes of two models of behavior change. J Occup Environ Med. 2007;49:204–213. doi: 10.1097/JOM.0b013e3180329a8d. [DOI] [PubMed] [Google Scholar]
- 4.Soteriades E.S., Hauser R., Kawachi I., Liarokapis D., Christiani D.C., Kales S.N. Obesity and cardiovascular disease risk factors in firefighters: a prospective cohort study. Obes Res. 2005;13:1756–1763. doi: 10.1038/oby.2005.214. [DOI] [PubMed] [Google Scholar]
- 5.Jahnke S.A., Poston W.S.C., Haddock C.K., Jitnarin N. Obesity and incident injury among career firefighters in the Central United States. Obesity. 2013;21:1505–1508. doi: 10.1002/oby.20436. [DOI] [PubMed] [Google Scholar]
- 6.Poston W.S.C., Jitnarin N., Haddock C.K., Jahnke S.A., Tuley B.C. Obesity and injury-related absenteeism in a population-based firefighter cohort. Obesity. 2011;19:2076–2081. doi: 10.1038/oby.2011.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Soteriades E.S., Hauser R., Kawachi I., Christiani D.C., Kales S.N. Obesity and risk of job disability in male firefighters. Occup Med (Lond) 2008;58:245–250. doi: 10.1093/occmed/kqm153. [DOI] [PubMed] [Google Scholar]
- 8.Yang J., Teehan D., Farioli A., Baur D.M., Smith D., Kales S.N. Sudden cardiac death among firefighters ≤45 years of age in the United States. Am J Cardiol. 2013;15:1962–1967. doi: 10.1016/j.amjcard.2013.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults (US) National Heart, Lung, and Blood Institute; Bethesda (MD): 1998. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults; p. 228. [Google Scholar]
- 10.World Health Organization . World Health Organization; Geneva (Switzerland): 2000. Obesity: preventing and managing the global epidemic; p. 265. Report No. 894. [PubMed] [Google Scholar]
- 11.Alasagheirin M.H., Clark M.K., Ramey S.L., Grueskin E.F. Body mass index misclassification of obesity among community police officers. AAOHN J. 2011;59:469–475. doi: 10.3928/08910162-20111017-01. [DOI] [PubMed] [Google Scholar]
- 12.Jitnarin N., Poston W.S.C., Haddock C.K., Jahnke S., Tuley B.C. Accuracy of body mass index-defined overweight in fire fighters. Occup Med (Lond) 2013;63:227–230. doi: 10.1093/occmed/kqs213. [DOI] [PubMed] [Google Scholar]
- 13.American Council on Exercise . The American Council on Exercise; San Diego (CA): 2009 December 2. What are the guidelines for percentage of body fat loss? [Internet]http://www.acefitness.org/blog/112/what-are-the-guidelines-for-percentage-of-body-fat [cited 2014 Apr 20]. Available from: [Google Scholar]
- 14.Poston W.S.C., Haddock C.K., Jahnke S.A., Jitanrin N., Day R.S. An examination of the benefits of health promotion programs for the national fire service. BMC Public Health. 2013;13:805. doi: 10.1186/1471-2458-13-805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shadish W.R., Cook T.D., Campbell D.T. Houghton-Mifflin; Boston (MA): 2002. Experimental and quasi-experimental designs for generalized causal inference; p. 623. [Google Scholar]
- 16.Hulett D.M., Bendick M., Thomas S.Y., Moccio F.A. International Association of Women in Fire & Emergency Services; Madison (WI): 2008. National report card on women in firefighting; p. 20. [Google Scholar]
- 17.Spratlin K. 2011 Jan 1. Firefighter obesity: a public safety risk. Fire Engineering [Internet]http://www.fireengineering.com/articles/print/volume-164/issue-1/departments/fire-service_ems/firefighter-obesity-a-public-safety-risk.html [cited 2014 Apr 20];164. Available from: [Google Scholar]
- 18.Heinrich K.M., Jitnarin N., Suminski R.R., Berkel L., Hunter C.M., Alvarez L., Brundige A.R., Peterson A.L., Foreyt J.P., Haddock C.K., Poston W.S.C. Obesity classification in military personnel: a comparison of body fat, waist circumference, and body mass index measurements. Mil Med. 2008;173:67–73. doi: 10.7205/milmed.173.1.67. [DOI] [PubMed] [Google Scholar]
- 19.Rush E.C., Freitas I., Plank L.D. Body size, body composition and fat distribution: comparative analysis of European, Maori, Pacific Island and Asian Indian adults. Br J Nutr. 2009;102:632–641. doi: 10.1017/S0007114508207221. [DOI] [PubMed] [Google Scholar]
- 20.Swinburn B.A., Craig P.L., Daniel R., Dent D.P., Strauss B.J. Body composition differences between Polynesians and Caucasians assessed by bioelectrical impedance. Int J Obes Relat Metab Disord. 1996;20:889–894. [PubMed] [Google Scholar]


