Abstract
Objective:
The aim of the study was to assess the prevalence and patterns of dyslipidemia in Saudi patients with angiographically documented coronary artery disease (CAD).
Materials and Methods:
This is a cross-sectional, hospital-based study, which was conducted on all Saudi patients who underwent coronary angiography under the author's personal care and were found to have > 50% coronary stenosis. Fasting lipid profile was measured in all patients during the admission for the coronary angiography.
Results:
Two hundred and ninety-five patients were included in the study. The mean age (±Standard deviation) was 55.1 ± 11, ranging from 17 to 86 years. The majority of patients were males: 229 (77.6%). Mean total cholesterol was 175.6 ± 47.6 mg/dl, mean low-density lipoprotein cholesterol (LDL-C) was 111.3 ± 40.3 mg/dl, mean high density lipoprotein cholesterol (HDL-C) was 38.27 ± 9.5 mg/dl and mean triglyceride level was 141.8 ± 74.8 mg/dl. 21 (7.1%) patients had normal coronary arteries, 107 (36.3%) had one vessel disease, 78 (26.4%) had two vessel disease and 89 (30.2%) had three vessel disease. There was a significant correlation between the extent of CAD and age (P = 0.003), sex (P = 0.0002), total cholesterol (P = 0.02) and low HDL-C (P < 0.001. 21 (7.1%) patients were asymptomatic, 110 (37.3%) had stable angina, 127 (43.1%) had none ST elevation acute coronary syndrome, 20 (6.8%) had ST elevation myocardial infarction and 17 (5.7%) had heart failure. There was also a significant correlation between age (P = 0.03), sex (P < 0.001), LDL-C (P = 0.005) and low HDL-C (P < 0.001) and the severity of CAD.
Conclusion:
Dyslipidemia is a very prevalent risk factor in Saudi patients with CAD. Low HDL-C was the most frequent lipid abnormality, which significantly impacts on the extent of the CAD.
Keywords: Acute coronary syndrome, coronary artery disease, dyslipidemia, non ST elevation myocardial infarction, ST elevation myocardial infarction
INTRODUCTION
Cardiovascular disease (CVD) remains a leading cause of morbidity and mortality worldwide. Fortunately, the major risk factors contributing to the development of atherosclerotic CVD have been described in many epidemiological studies. Meanwhile, several randomized clinical trials have demonstrated the great benefits of effective modification of many of those major risk factors.[1] Evidence from long-term follow-up studies demonstrates that a favorable risk factor profile during the working years is associated with a longer, healthier life, and reduced medical care expenses after age of 65 years.[2] Treatment of each of the major cardiovascular risk factors such as high-level of low-density lipoprotein cholesterol (LDL-C), hypertension, diabetes, and smoking showed a significant reduction of the major adverse cardiovascular events.[3] There have been some studies on dyslipidemia and other major risk factors in the Kingdom of Saudi Arabia, but data is scarce on the prevalence of dyslipidemia in patients with documented coronary artery disease (CAD). Information about the pattern of specific lipid abnormalities in this kind of population, and its impact on the extent and severity of the clinical presentation of CAD[4] is particularly in short supply. The main objective of this study was to evaluate the prevalence and pattern of dyslipidemia in Saudi patients with CAD confirmed by coronary angiography.
MATERIALS AND METHODS
This was a cross-sectional study on consecutive series of patients undergoing coronary angiography at a University Hospital in Saudi Arabia between January 2011 and February 2012. The coronary angiography was done using the standard technique. The severity of the lesion was visually assessed if it was >70% or <40%, but for lesions between 40% and 70% computer-assisted quantitative angiography was used. The lesion was considered significant if the luminal stenosis exceeded 50% in any epicardial vessel. The extent of CAD was reported as one, two or three-vessel disease, and if there was left main coronary artery involvement. The grading of CAD presentation was also reported as: Stable angina, none ST elevation acute coronary syndrome (NSTE-ACS), ST elevation myocardial infarction (STEMI) or congestive heart failure (HF). Lipid profile was measured for all patients after 12 h overnight fasting. For those with acute myocardial infarction, lipid measurement was done after 1 month of the acute event. All patients underwent evaluation of other risk factors for atherosclerosis such as diabetes, smoking, hypertension and obesity guided by body mass index. Demographic data of all patients were also recorded. Hypertension was defined as systolic blood pressure of 140 mmHg or greater, diastolic blood pressure of 90 mmHg or greater or physician diagnosis with the use of antihypertensive medications. The average blood pressure was composed of up to four readings on two separate occasions. Dyslipidemia was defined as total cholesterol level ≥200 mg/dl, triglyceride level ≥150 mg/dl, high-density lipoprotein cholesterol (HDL-C) level <40 mg/dl for males or <50 mg/dl for females, LDL-C level >100 mg/dl (in our CAD patients), a combination of these abnormalities, or a physician's diagnosis with medication use. Diabetes was defined as self-reported, a physician's diagnosis with use of antihyperglycemic agents, fasting glucose of ≥126 mg/dl in two separate occasions, random blood glucose ≥200 mg/dl in the presence of classical symptoms of hyperglycemia.
Statistical analysis
Numerical variables were reported as mean ± Standard deviation (SD) or as a percentage for risk factors. The Chi-square test was used for categorical variables and t-test for continuous variables. Significance was set at P < 0.05 and 0.05-0.1 was considered as statistical trend for all comparisons. Statistical analyses were performed using SPSS 15 software (Chicago, USA).
RESULTS
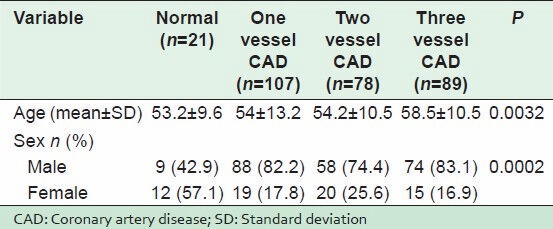
The study included 295 patients. The mean age (± SD) was 55.12 ± 11, range 17-86 years. The majority of patients were males; 229 (77.6%). The mean total cholesterol level was 175.6 ± 47.6 mg/dl, mean LDL-C was 111.3 ± 40.3 mg/dl, mean HDL-C was 38.3 ± 9.5 mg/dl and the mean triglyceride level was 141.8 ± 74.8 mg/dl [Table 1]. Normal coronary arteries were present in 21 (7.1%) cases, 107 (36%) cases had one vessel disease, 78 (26.4%) had two vessel disease, and 89 (30.2%) had three vessel disease. There was a highly significant correlation between the extent of CAD and low HDL-C (P < 0.001), [Table 2], old age (P = 0.003) and male sex (P = 0.02) [Table 3].
Table 1.
Baseline patient characteristics
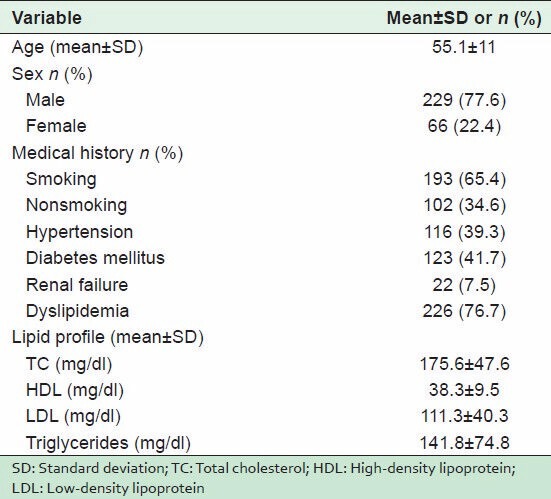
Table 2.
Relationship between patient's lipid profile and extent of CAD (n=295, mean±SD)
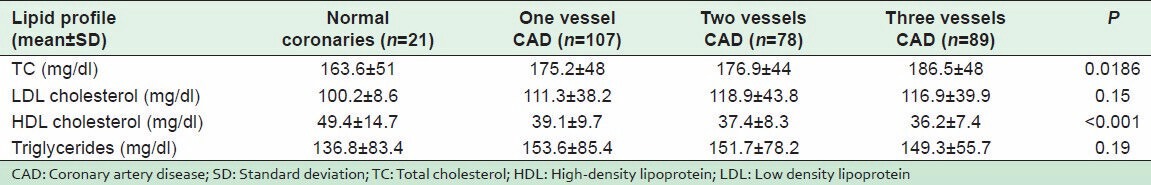
Table 3.
Age and sex impact on the extent of CAD
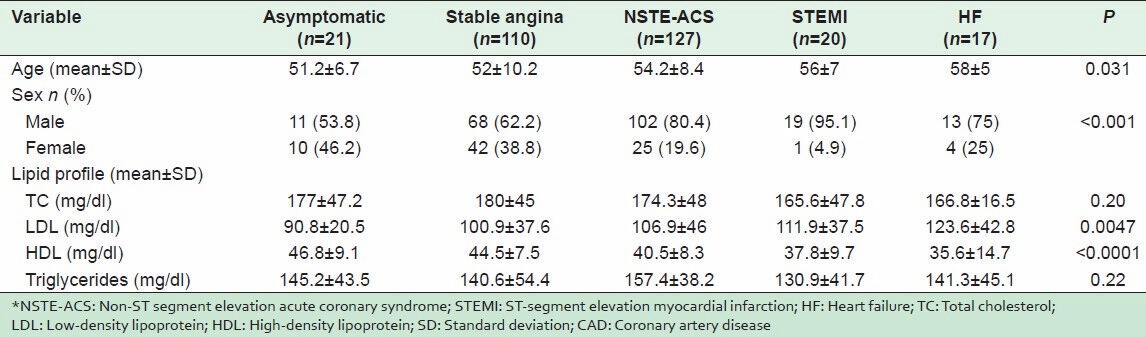
21 (7.1%) patients were asymptomatic, 110 (37.3%) had stable angina, 127 (43.1%) had NSTE-ACS, 20 (6.8%) STEMI and 17 (5.7%) had HF. There was also a significant correlation between age (P = 0.03), sex (P < 0.001), LDL-C (P = 0.005) and low HDL-C (P < 0.001) and severity of CAD [Table 4].
Table 4.
Relationship between lipid profile and severity of CAD symptoms*
DISCUSSION
Many international studies have shown significantly increased risk for CAD in the presence of dyslipidemia.[5,6,7] However, available information about the prevalence and the pattern of lipid abnormalities in Saudi patients with established coronary atherosclerosis is scarce. In our study, we evaluated lipid disorders and their patterns in Saudi patients who were diagnosed with coronary atherosclerosis based on coronary angiography. Major CAD risk factors including age, male sex, diabetes mellitus, hypertension and smoking were noted to be very prevalent in our studied population, which is similar to previous published data evaluating the prevalence of these risk factors in Saudis.[8,9] In the agreement with Al-Nozha et al., 75% of our patients with coronary atherosclerosis had dyslipidemia, which illustrates the importance of this risk factor among other factors in increasing prevalence of CAD in the Saudi population. Of those, 44% had Low HDL-C level as the main lipid abnormality, which was significantly correlated with two and three-vessel CAD. Furthermore, such low HDL-C level was also correlated with frequent STEMI and congestive HF. We attribute this high-prevalence of Low HDL-C in Saudi patients to the lack of exercise as most of our Saudis had a sedentary life and were physically inactive,[10] with a high-prevalence of cigarette smoking.[11]
The strong impact of low HDL-C on the extent of CAD in our patients is in accord with previous epidemiological studies that have consistently demonstrated an inverse association between HDL-C levels and the risk of coronary heart disease.[12]
The LDL-C levels in our patients were significantly correlated with the severity of the presentation of CAD and an adverse clinical outcome, and tend to be correlated with the extent of CAD (number of affected vessels). This positive correlation between the LDL-C levels with the adverse clinical outcome and the extent of CAD is in agreement with previous published data that addressed this positive correlation.[13,14]
CONCLUSION
The current study demonstrated a very high-prevalence of dyslipidemia in Saudi patients with CAD, and also showed the significant impact of Low HDL-C cholesterol on the extent of CAD. It illustrates also the strong impact of low HDL-C and high LDL-C on the clinical outcome of patients suffering from CAD. Such findings must alert the treating physicians at the primary and secondary prevention levels to be more aggressive in their control of these lipid abnormalities by promoting lifestyle modifications, encouraging regular exercise, and the use of appropriate medical therapy as required.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Lloyd-Jones DM, Leip EP, Larson MG, D'Agostino RB, Beiser A, Wilson PW, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–8. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 3.Goraya TY, Leibson CL, Palumbo PJ, Weston SA, Killian JM, Pfeifer EA, et al. Coronary atherosclerosis in diabetes mellitus: A population-based autopsy study. J Am Coll Cardiol. 2002;40:946–53. doi: 10.1016/s0735-1097(02)02065-x. [DOI] [PubMed] [Google Scholar]
- 4.Al-Nozha MM, Arafah MR, Al-Maatouq MA, Khalil MZ, Khan NB, Al-Marzouki K, et al. Hyperlipidemia in Saudi Arabia. Saudi Med J. 2008;29:282–7. [PubMed] [Google Scholar]
- 5.Austin MA, King MC, Vranizan KM, Krauss RM. Atherogenic lipoprotein phenotype. A proposed genetic marker for coronary heart disease risk. Circulation. 1990;82:495–506. doi: 10.1161/01.cir.82.2.495. [DOI] [PubMed] [Google Scholar]
- 6.Tornvall P, Karpe F, Carlson LA, Hamsten A. Relationships of low density lipoprotein subfractions to angiographically defined coronary artery disease in young survivors of myocardial infarction. Atherosclerosis. 1991;90:67–80. doi: 10.1016/0021-9150(91)90245-x. [DOI] [PubMed] [Google Scholar]
- 7.Després JP, Moorjani S, Lupien PJ, Tremblay A, Nadeau A, Bouchard C. Regional distribution of body fat, plasma lipoproteins, and cardiovascular disease. Arteriosclerosis. 1990;10:497–511. doi: 10.1161/01.atv.10.4.497. [DOI] [PubMed] [Google Scholar]
- 8.Al-Nozha MM, Arafah MR, Al-Mazrou YY, Al-Maatouq MA, Khan NB, Khalil MZ, et al. Coronary artery disease in Saudi Arabia. Saudi Med J. 2004;25:1165–71. [PubMed] [Google Scholar]
- 9.Al-Nozha M, Al-Khadra A, Arafah MR, Al-Maatouq MA, Khalil MZ, Khan NB, et al. Metabolic syndrome in Saudi Arabia. Saudi Med J. 2005;26:1918–25. [PubMed] [Google Scholar]
- 10.Al-Hazzaa HM. Prevalence of physical inactivity in Saudi Arabia: Abrief review. East Mediterr Health J. 2004;10:663–70. [PubMed] [Google Scholar]
- 11.Rao Ch S, Subash Y E. The effect of chronic tobacco smoking and chewing on the lipid profile. J Clin Diagn Res. 2013;7:31–4. doi: 10.7860/JCDR/2012/5086.2663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Natarajan P, Ray KK, Cannon CP. High-density lipoprotein and coronary heart disease: Current and future therapies. J Am Coll Cardiol. 2010;55:1283–99. doi: 10.1016/j.jacc.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 13.Wilson PW. The Anglo-Scandinavian cardiac outcomes Trial lipid-lowering arm: Significant lipid and coronary heart disease effects. Curr Cardiol Rep. 2003;5:462–7. [Google Scholar]
- 14.Mohan V, Deepa R, Rani SS, Premalatha G. Chennai Urban Population Study (CUPS No. 5). Prevalence of coronary artery disease and its relationship to lipids in a selected population in South India: The Chennai Urban Population Study (CUPS No 5) J Am Coll Cardiol. 2001;38:682–7. doi: 10.1016/s0735-1097(01)01415-2. [DOI] [PubMed] [Google Scholar]


