Abstract
Background:
Increasing number of reports on medication errors and relevant subsequent damages, especially in medical centers has become a growing concern for patient safety in recent decades. Patient safety and in particular, medication safety is a major concern and challenge for health care professionals around the world. Our prospective study was designed to detect prescribing, transcribing, dispensing, and administering medication errors in two major university hospitals.
Materials and Methods:
After choosing 20 similar hospital wards in two large teaching hospitals in the city of Isfahan, Iran, the sequence was randomly selected. Diagrams for drug distribution were drawn by the help of pharmacy directors. Direct observation technique was chosen as the method for detecting the errors. A total of 50 doses were studied in each ward to detect prescribing, transcribing and administering errors in each ward. The dispensing error was studied on 1000 doses dispensed in each hospital pharmacy.
Results:
A total of 8162 number of doses of medications were studied during the four stages, of which 8000 were complete data to be analyzed. 73% of prescribing orders were incomplete and did not have all six parameters (name, dosage form, dose and measuring unit, administration route, and intervals of administration). We found 15% transcribing errors. One-third of administration of medications on average was erroneous in both hospitals. Dispensing errors ranged between 1.4% and 2.2%.
Conclusion:
Although prescribing and administrating compromise most of the medication errors, improvements are needed in all four stages with regard to medication errors. Clear guidelines must be written and executed in both hospitals to reduce the incidence of medication errors.
Keywords: Disguised direct observation, hospital, inpatient, medication error
INTRODUCTION
United States committee on quality of health published a report in 1999 by the title of “To Err Is Human” in which medical errors were mentioned as an epidemic problem leading to almost 44,000-98,000 deaths annually.[1] This report was remarkable for WHO eventually leading to an announcement prioritizing patient safety as an imperative for health care policy makers around the world.[2]
Increasing number of reports on medication errors and relevant subsequent damages, especially in medical centers has become a growing concern for patient safety in recent decades.[3,4,5,6,7] On the other hand, because of drug overuse and self-treatment within the society, especially among elderly, appropriate use of medications as well as their safety has become the superior concern of public health policy makers all around the world.[8]
A number of studies have been performed in the area of medication errors. An earlier study was performed by Harvard University on 3000 hospitalized patients showing 3.7% of patients affected by the health system errors leading to mortality or severe damage. Medication errors compromised 19% of such errors.[9] Similar studies in Canada, England, France, Australia, Spain, and some other states of the United States indicate that 5-10% of patients experience variable degrees of adverse effects of treatment - preventable errors - during the time they reside in the hospital.[10,11,12,13]
Only a fraction of medication errors are reported, but each report can raise awareness and voluntary reporting to prevent repetition of unwanted outcomes in similar situations.[11,12,13,14] Complex drug dispensing systems in hospitals highlights the importance of monitoring medication errors and incidence reporting by the staff to improve the quality of medication errors.[12]
Discovering error rates is not an easy process, but it should be taken into consideration that most of these errors which threat patients’ health and safety are repetitive and preventable.[15] Because of the large diversity of reported medication errors with different definitions and methodologies, defining the exact and consistent rate of such errors is a difficult task in general.[16,17,18,19,20,21]
A number of methods are used for medication error measurements each one of which has its pros and cons: Anonymous self-reports or questionnaires, incident voluntary reporting, critical incident technique, chart review, computer-assisted monitoring, disguised direct observation (DDO).[22,23,24,25,26,27,28] While plenty of biases have been identified for the majority of these methods, the DDO has been cited as most suitable for research.[22,29]
Several studies have been conducted in some parts of Iran regarding health system errors. Prescribing error of 10.5% and transcribing error of 29.9% have been reported as part of these published articles.[11,30,31,32,33,34]
To the best of our knowledge, none of the published studies conducted in Iran to date has exclusively and completely evaluated medication errors in four stages of prescribing, transcribing, dispensing and administering and most of them were affected by limitations and small sample size. Because of the importance of medication safety and lack of a comprehensive survey, we aimed to evaluate the incidence of medication errors in four stages (administration, transcribing, prescribing and dispensing) for the first time in Isfahan Province in two of its largest hospitals with two different medication distribution systems.
MATERIALS AND METHODS
The design utilized is a descriptive cross-sectional study conducted on a total of 565 hospitalized patients in all 40 wards of medical, surgical and intensive care units of the two largest hospitals of Isfahan during September 2012 to February 2013. The two teaching hospitals, one affiliated to Isfahan University of Medical Sciences (Al-Zahra Hospital [AZH]) and another affiliated to the Social Security Organization (Dr. Shariati Hospital [DSH]), the former using unit-dose (distributing 24 h needs of each medication per patient) and the latter using floor stock system (distributing medication needs based on nursing request to distribute medications. The hospitals were selected because they are the two largest in the city and can provide a good representation of governmental hospitals in the province.
Sampling of wards
Twenty resembling wards in AZH and DSH (including all the medical, surgical and Intensive Care Units) were selected and their names were drawn randomly to determine, which ward to be visited first by the researcher.[37] A random number generator was used for the randomization process. Upon arrival on each ward, the first nurse seen by the researcher would be approached and asked whether she or he would agree to be accompanied by the researcher to be observed for drug distribution purposes. The head nurse was approached occasionally to facilitate this process.
According to the definition of The National Coordinating Council for Medication Error and Prevention, medication error is any preventable incidence, which leads to misuse of the drug or damage to patient whilst taking drugs is under health team or patient's control.[25] DDO, a previously validated method, was used as our method to detect and describe medication errors.[22,29] The number of doses (medication items) observed by the researcher which in fact represents the opportunities for error occurrence was used as the basis for sample size calculation.[37,38] Since, no data was available on the rate of medication errors in Isfahan hospitals; the total sample size of 1000 doses was calculated to be studied for each hospital.
Medication error detection tool
We evaluated types and incidence of medication errors utilizing DDO method in four stages including prescribing, transcribing, dispensing and administering.[35,36] To avoid or reduce bias due to the presence of researcher on performance of target individuals, hospital nurses, nurse aids, ward secretaries, pharmacists, and pharmacy technicians were told that the observer was assessing the process of drug distribution instead without giving further details. Diagrams for each drug distribution system in each hospital were drawn by the help of pharmacy directors in each hospital to clarify the steps involved in medication handling in each of the two institutions The outcome of the study was to measure the incidence rate of medication errors in the four stages. Sequence of stages of study is described as follows.
Administering stage
The observer entered the selected ward and approached the first nurse she saw. She introduced herself and the project as mentioned in the above section. Once oral consent of the nurse was obtained, the researcher would follow and observe the nurse. The researcher recorded the doses dispensed and continued observing until the 50 doses in that ward finished. The researcher occasionally had to observe more than one nurse or had to be present in a ward in AM, PM or Graveyard shifts to complete the 50 administered dose since in some wards medication administration was not as prevalent as in some other wards. After recording the details of administration, the observer checked patients’ documents to compare his/her records with what the physician had prescribed and what the hospital pharmacy had delivered in addition to the nursing reports for further verification. Detected inconsistencies were discussed in a team including the researcher, clinical pharmacist and head of the Pharmaceutical care Department of the hospital.[39] The definition of administration error used by the team is “any inconsistency, whether in dosage form, dose, administration route, dosing interval, between what has been ordered by a physician and what the patient receives by nurse.” Probable errors of administration that our observer focused on in this stage were unauthorized dose, extra dose, under-dose, omission dose, wrong dose, wrong route and wrong time and frequency. For example, wrong route error means when an intravenous drug was administered subcutaneously. Wrong time error occurred when a drug was administered >1 h before or after the scheduled time. The above-mentioned process went on until the records of 1000 doses were collected in each of the two hospitals.[23,25,40]
Transcribing stage
In both hospitals, physician orders are not delivered or presented to the hospital pharmacy directly contrary to what is typically seen in a community pharmacy. Once the order is written, the head nurse records the medications ordered onto a medication list (medication sheet) (T1). In AZH, one of the nurses transcribes the medication orders from the medication sheet onto a request list, which is sent to the Pharmacy Department whereas in DSH, the secretary sends the request through the computer system to the Pharmacy Department (T2). In AZH, a third step is involved and that is the information from the paper medication request list sent by the ward is entered by computer operators situated in the Pharmacy Department into the computer system (T3).
In order to evaluate transcribing errors, the researcher categorized these errors into three types based on which stage of transcribing they occurred (T1, T2 or T3). Any inconsistency detected between the physician order, and the medication sheet was considered as type 1 transcribing error (T1). The researcher then checked the written (AZH) or computerized (DSH) list of requested drugs sent to the pharmacy against the medication sheet for probable inconsistencies in name, dose, dosage form, quantity, etc., (T2). Type 3 error was measured only in AZH on any inconsistencies between the paper request list of the ward and the computer list generated by the operators located in the Pharmacy Department (T3).
Prescribing stage
After observing the nurse and evaluating the administration stage, the researcher recorded the exact written order of the administered drug extracted from the chart. The researcher defined prescribing error if one of the following criteria were met:
The dose of the drug was not written based on the current available doses in the Iranian market. That is, MD wrote ranitidine tablet 100 mg instead of 150 mg or 300 mg.
The medication order lacked one of the following and therefore considered as not complete: Name, dosage form, dose and measuring unit such as mg or that is, administration route, intervals of administration.
Dispensing stage
The observer was present at the checking point in the pharmacy and the receiving point at the ward. She finished recording as soon as she reached the 1000 mark as the goal for dispensed medications and followed the medication courier to the ward. Given the fact that the checker at the checking point did not check all the medications specifically oral medications, the second stage (D2) seemed inevitable.
In order to detect the dispensing errors (D1 and D2), the observer checked the inaccuracies of what was dispensed against the computer generated list either by the computer operator in AZH or by the ward secretary in DSH at the checking point in the Pharmacy Department (D1). To detect the D2 errors, the researcher accompanied the medication courier and checked the medications sent to ward against the requested list. This showed the final checker error as part of dispensing error (D2). Recorded errors and inconsistencies of the above four stages were discussed and confirmed by the 3 member team.[39] Data were input into and analyzed by Statistical Package for Social Sciences (SPSS) version 20 (IBM Corporation, NY, USA). Chi-square test was used to compare different medication errors between the two hospitals.
RESULTS
A total number of recorded data were 8162, from which 8000 were complete and used for analysis. This data belonged to 565 patients and was collected in 4 stages. The number of records in each stage was 1000 in each hospital or 2000 records for each of the four stages. All three shifts were included in the evaluation process: morning (1094), afternoon (851) and graveyard (55) shifts comprised of 54.7%, 42.6% and 2.8% of the 2000 records, respectively in both hospitals in administering, transcribing, and prescribing stages. More than half (50.8%) of patients were males and the rest (49.2%) were females. Ages ranged from newborn to 89 years old (8.8% up to 2 years, 3.6% from 2 to 17 years, 66.1% from 18 to 65 years, and 22.2% above 65 years). Results of data analysis of each stage are described below:
Prescribing stage
As explained before, 2000 MD orders were assessed for 6 parameters including P1) drug route, P2) dosage form, P3) dose unit (mg, g, ml, etc.), P4) frequency interval, P5) drug name, P6) drug dose. As seen in the Table 1, only 27% were considered as complete orders consisting of all six parameters. Around one-third (34%) of orders had five parameters, whereas 39% of orders had four or less parameters. From all the six parameters of prescribing P5 (drug name) was not missed in any of orders and P6, P4, P3, P2, and P1 were the parameter with most frequent- omissions, respectively. Another error we detected while reviewing orders, which was not part of our early objectives was ordering doses of medications, which were not available in Iranian market (0.75%). More details and P values are shown in Table 2.
Table 1.
Overall prescribing error frequencies
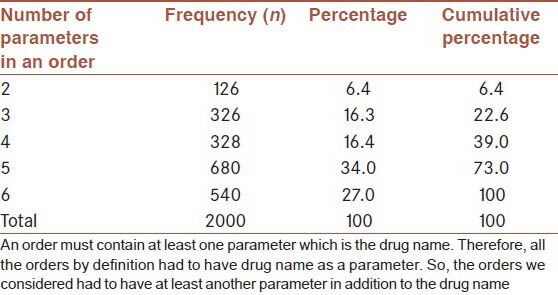
Table 2.
Incidence of medication errors in two hospitals
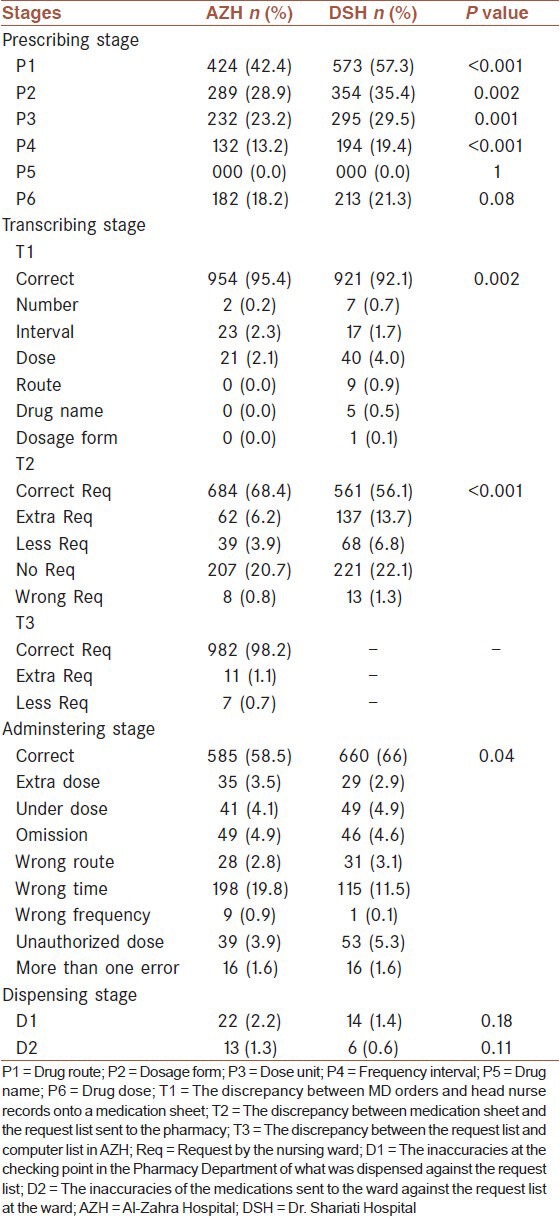
Transcribing stage
Three kinds of errors were defined for this stage, which was described earlier as T1, T2, and T3 in the methods section. Reported incidences of errors were 6.3%, 37.7%, and 1.8%, respectively. The detailed breakdown for each hospital is seen in Table 2. The errors related to the additional stage (T3) in AZH consisted of 1.8% of transcribing errors. Fortunately, omitting this additional stage (T3) occurred at the end of our study and a computerized list of required drugs is now directly sent to the pharmacy in AZH like DSH.
Dispensing stage
As described in the methods section evaluation of dispensing stage was performed at two distinct levels and times (D1 and D2). As shown in Table 2, there is not a significant difference between errors of D1 between the two hospitals.
Administering stage
Our findings showed that administration errors were frequent in both hospitals occurring at an average rate of 1 in every three doses. Administration error was 41.5% in AZH and 34% in DSH, which are significantly different (P = 0.04). On an average, the most frequent error was the wrong time (15.6%) and omission, unauthorized dose, under-dose, extra dose, wrong route, and wrong frequency occurred in 4.7, 4.6, 4.5, 3.2, 2.9, and 0.5% of cases, respectively. A great portion of errors were wrong time errors, none of the cases proved fatal. We found more than a single administration error for almost 1% of all 2000 doses. Unauthorized administration consisted mostly of analgesics such as diclofenac suppository [Table 2].
DISCUSSION
Evaluation of medication errors is a fairly new issue in Iran. One of the problems in these types of studies is differences in definitions, terminology, methods and indices used making comparisons of results difficult. A review article published in 2013 in Iran reported administration error as the most frequent medication error with a prevalence range of 14.3-70%. Furthermore, they showed that 83.3% of reviewed studies measured administration errors solely or in combination with other medication error types. Other types of errors reported according to this review were 29.8-47% for prescribing, 11.2-33.6% for dispensing, and 10-51.8% for transcribing errors.[19]
To the best of our knowledge, none of the available studies conducted in Iran has exclusively and completely evaluated medication errors in all levels to date and most of them were affected by limitations and small sample size as the largest one belonged to Fahimi, et al. study on 524 patient medical charts in 2008.[30] In the current study, 8000 data belonging to 565 patients were evaluated in two large teaching hospitals. Although the severity of errors was not part of this study, but our observations showed that there was no known life-threatening risk error in our study, but there were several near miss errors like mistaken selection of Heparin instead of tramadol or amikacin instead of Ranitidine because of their similarities in appearance that were fortunately caught by the nurse prior to administration.
Since the majority of works in the central pharmacy of the hospital are performed in the morning shift, the observer collected her data on dispensing errors in the hospital pharmacy solely in the morning.
When evaluating prescribing errors, we found that few MD orders (27%) met all the 6 parameters as explained before. Incomplete orders may lead to more medication errors because of assumptions (sometimes wrong), which have to be made by the nursing or pharmacy personnel. For example, if a physician does not clarify the quantity of the medication ordered, this could be interpreted as 1 or 2 or any other quantity, which inherently could lead to error. This shows that physicians may not be aware of or obey laws or regulations governing prescribing and re-educating them may be necessary. As considered before, total prescribing error in Iran was reported to a range from 29.8% to 47.8%, but this may depend on the definitions and methods used.[19] Prescribing errors have been defined differently by various investigators. For example, Vesal considered mostly clinical parameters in her 4-month evaluation of prescribing errors in 2010, which yielded a 39% prevalence: wrong frequency, wrong drug selection, overdose, failure to discontinue, failure to order, under-dose, wrong time, therapeutic monitoring, wrong route, and drug interactions. Also, Lewis et al., in his systematic review article addresses the wide variations in prescribing errors, 2-14%, mainly due to differences in settings, definitions, research methods making any comparison quite difficult.
We reported mean prevalence of 15.26% for transcribing errors, which is in the range reported by Mansouri et al. (10-51.8%). As seen in Table 2, most of the transcribing errors (37.7%) occur in the T2 stage, showing the problem in the request lists, either paper or electronic, sent to the pharmacy by the wards. Specifically, most of these errors in the T2 stage were due to no requests (21.4%), which might have been due to the presence of medications in the floor stocks of the wards, and requests of extra doses (9.9%) of medications by the wards. Also, most errors occurred in the medication dosage in the T1 stage in the two hospitals. The additional stage of transcribing (T3) in AZH was omitted beginning Farvardin 1392 because of computerization of transcribing process. In a study by Lisby et al., transcribing errors were 56% quite higher than our study and outside the range of Mansouri's article showing that settings of the study and definitions used could impact the numbers reported.
Dispensing error was reported to be 4% by Lisby, et al. and 11.2-33.6% by Mansouri, et al. studies, respectively. Again, differences reported among different numbers shows that different settings and definitions can impact on the prevalence of medication errors in the dispensing stage.
As shown in the results section of this article, the error rate (D1) in AZH is almost twice that of DSH. From these dispensing errors, the main differences between the two hospitals is shown in Table 3. Higher workload relative to the number of technicians dispensing or checking medications could perhaps be one of the explanations for higher rate of dispensing errors in one institution. Look-a-likes and sound-a-likes could easily be missed in higher workload situations especially in the morning shifts. In addition, in AZH the pharmacy is responsible to render intravenous solutions as well as solid dosage forms at the same time whilst DSH has a separate dispensing system for intravenous solutions reducing the workload for the final checker. Other causative factors such as work experience may play a role in the difference observed, which are out of scope for this research.
Table 3.
Comparison of two hospitals in dispensing stage
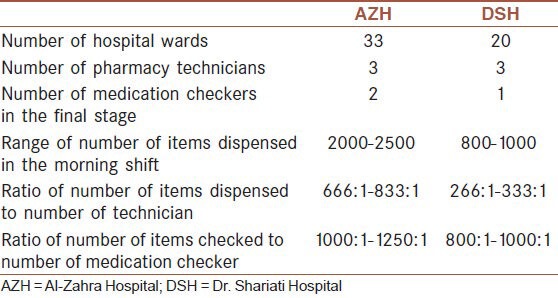
Higher demands from the pharmacy especially during 10:30 am to 12:30 pm could be alleviated by designating time slots to each ward for their medication requests. This may spread the traffic of requests over a 4-5 h period reducing potential for dispensing errors in turn.
Administration errors varied among different working shifts in both hospitals: In the mornings, the rate was 472/1094 (43.1%), evenings 334/851 (39.2%), and graveyard shifts 9/55 (16.3%). This is in line with Capuzzo's findings. He reported that most of the unintended events including different medical errors such as medication errors occurred in the morning shifts as opposed to the afternoon and night shifts. These findings may be explained by nurses’ heavier workload in the morning shifts as well as the presence of medical, nursing and pharmacy students in morning shifts who due to lack of experience may ask unnecessary questions from the nurse or commit errors in administering by the nursing students.
Barker and Kenneth also used direct observation method and reported administration errors to be 19%, most of which (43.1%) was related to the wrong time of administration while omission, wrong dose and unauthorized drug errors were reported to be 30%, 17%, and 4%, respectively.[23] His findings closely follow ours. We also have shown that wrong time administration errors are the most, whereas, wrong dose (combination of under and over dose) of 7.7% was next, followed by omission and unauthorized errors as next most frequent ones. Tisset et al., have reported lower rates for administration errors (14.9%) of which wrong dose and wrong time were 41%, and 26%, respectively accounting for most frequent administration errors. Fahimi et al., have reported rate of administration error to be 9.4% quite lower than ours. The main reason for wrong time error as the most frequent administration error in DSH may be the fact that nurses usually do not pay much attention to the exact time of orders and they tend to administer all medications in that shift at the same time to improve efficiency. But in AZH, the most important cause for the wrong time error was perhaps due to the delay, which occurred in receiving the drugs from the Pharmacy Department due to lack of an extensive floor stock. Administration error were high in DSH. The researcher poses the theory that perhaps due to the nature of DSH as being a Social Security Organization facility in which patients receives free care, might be a reason for less motivation among the nurses and therefore committing more errors.
In none of above studies including ours, administration of expired medications were not studied as part of administration errors. One of the reasons for this was that the expiration date on some of the medications was not clear or easily readable. Although there are similarities among our results with other research, the differences might be as the result of different methods and settings that these studies have been performed in.
The advantage of this study was that all four stages of administering, transcribing, prescribing, and dispensing were observed in two different large hospitals. This contributes to the generalizability of the study in a large city such as Isfahan. The limitations were that we did not investigate the clinical aspects of prescribing errors and simply limited to only the parameters comprising a physician order.
CONCLUSION
Although prescribing and administrating compromise most of the medication errors, improvements are needed in all four stages with regard to medication errors. Clear guidelines must be written and executed in both hospitals to reduce incidence of medication errors.
AUTHOR'S CONTRIBUTIONS
AHZ and FS contributed to the conception and design of the work, analysis, and interpretation of data; prepared the manuscript; did final approval of the version to be published; and agreed to be accountable for all aspects of the work.
ACKNOWLEDGMENTS
The authors would like to gratefully thank vice chancellery for research of Isfahan University of Medical Science for financial support of this research (Research Project Number 393345) and also the Social Security Organization of Isfahan for allowing this study to take place. We also whole heartedly thank directors of Pharmacy Departments of AZH and DSH, Drs. Reza Heidari and Ali Tork Ladani for their special assistance and the pharmacy staff and nursing personnel of the two institutions for their help.
Footnotes
Source of Support: The authors would like to gratefully thank vice chancellery for research of Isfahan University of Medical Science for financial support of this research (Research Project Number…) and also the Social Security Organization of Isfahan for allowing this study to take place.
Conflict of Interest: None declared.
REFERENCES
- 1.Kohn LT, Corrigan JM, Donaldson MS. Washington, DC: National Academy Press; 2000. Institute of Medicine (U.S) Committee on Quality of Health Care in America To Err Is Human: Building a Safer Health System. [PubMed] [Google Scholar]
- 2.World Health Assembly Resolution WHA55.18 and related documents. [Last accessed on 2013 Oct 10]. Available from: http://www.who.int/patientsafety/about/wha resolution/en/index.html .
- 3.Conen D. Measures to enhance patient safety. Importance of efficiency evaluation. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2011;54:171–5. doi: 10.1007/s00103-010-1201-1. [DOI] [PubMed] [Google Scholar]
- 4.Patel I, Balkrishnan R. Medication error management around the globe: An overview. Indian J Pharm Sci. 2010;72:539–45. doi: 10.4103/0250-474X.78518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med. 2003;348:2526–34. doi: 10.1056/NEJMsa020847. [DOI] [PubMed] [Google Scholar]
- 6.Joolaee S, Hajibabaee F, Peyrovi H, Haghani H, Bahrani N. The relationship between incidence and report of medication errors and working conditions. Int Nurs Rev. 2011;58:37–44. doi: 10.1111/j.1466-7657.2010.00872.x. [DOI] [PubMed] [Google Scholar]
- 7.Leape LL. A systems analysis approach to medical error. J Eval Clin Pract. 1997;3:213–22. doi: 10.1046/j.1365-2753.1997.00006.x. [DOI] [PubMed] [Google Scholar]
- 8.Devine EB, Hansen RN, Wilson-Norton JL, Lawless NM, Fisk AW, Blough DK, et al. The impact of computerized provider order entry on medication errors in a multispecialty group practice. J Am Med Inform Assoc. 2010;17:78–84. doi: 10.1197/jamia.M3285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, et al. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324:377–84. doi: 10.1056/NEJM199102073240605. [DOI] [PubMed] [Google Scholar]
- 10.Thomas EJ, Studdert DM, Burstin HR, Orav EJ, Zeena T, Williams EJ, et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care. 2000;38:261–71. doi: 10.1097/00005650-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138:161–7. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 12.Weingart SN, McL Wilson R, Gibberd RW, Harrison B. Epidemiology of medical error. West J Med. 2000;172:390–3. doi: 10.1136/ewjm.172.6.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reason J. Human error: Models and management. BMJ. 2000;320:768–70. doi: 10.1136/bmj.320.7237.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boyle TA, Mahaffey T, Mackinnon NJ, Deal H, Hallstrom LK, Morgan H. Determinants of medication incident reporting, recovery, and learning in community pharmacies: A conceptual model. Res Social Adm Pharm. 2011;7:93–107. doi: 10.1016/j.sapharm.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 15.Schachter M. The epidemiology of medication errors: How many, how serious? Br J Clin Pharmacol. 2009;67:621–3. doi: 10.1111/j.1365-2125.2009.03418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harding L, Petrick T. Nursing student medication errors: A retrospective review. J Nurs Educ. 2008;47:43–7. doi: 10.3928/01484834-20080101-05. [DOI] [PubMed] [Google Scholar]
- 17.Dean Franklin B, Vincent C, Schachter M, Barber N. The incidence of prescribing errors in hospital inpatients: An overview of the research methods. Drug Saf. 2005;28:891–900. doi: 10.2165/00002018-200528100-00005. [DOI] [PubMed] [Google Scholar]
- 18.Lisby M, Nielsen LP, Brock B, Mainz J. How are medication errors defined? A systematic literature review of definitions and characteristics. Int J Qual Health Care. 2010;22:507–18. doi: 10.1093/intqhc/mzq059. [DOI] [PubMed] [Google Scholar]
- 19.Mansouri A, Ahmadvand A, Hadjibabaie M, Kargar M, Javadi M, Gholami K. Types and severity of medication errors in Iran; a review of the current literature. Daru. 2013;21:49. doi: 10.1186/2008-2231-21-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alsulami Z, Conroy S, Choonara I. Medication errors in the Middle East countries: A systematic review of the literature. Eur J Clin Pharmacol. 2013;69:995–1008. doi: 10.1007/s00228-012-1435-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joolaee S, Hajibabaee F, Peyrovi H, Haghani H, Bahrani N. The relationship between incidence and report of medication errors and working conditions. Int Nurs Rev. 2011;58:37–44. doi: 10.1111/j.1466-7657.2010.00872.x. [DOI] [PubMed] [Google Scholar]
- 22.Cohen MR. Washington DC: American Pharmacists Association; 2007. Medication Errors; pp. 24–7. [DOI] [PubMed] [Google Scholar]
- 23.Barker KN, Flynn EA, Pepper GA, Bates DW, Mikeal RL. Medication errors observed in 36 health care facilities. Arch Intern Med. 2002;162:1897–903. doi: 10.1001/archinte.162.16.1897. [DOI] [PubMed] [Google Scholar]
- 24.Morimoto T, Gandhi TK, Seger AC, Hsieh TC, Bates DW. Adverse drug events and medication errors: Detection and classification methods. Qual Saf Health Care. 2004;13:306–14. doi: 10.1136/qshc.2004.010611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Flynn EA. A brief history of medication errors. 2004. [Last accessed on 2013 Dec 25]. pp. 1–6. Available from: http://www.medaccuracy.com/Papers%20and%20Publications/A%20Brief%20History%20of%20Medication%20Errors.pdf .
- 26.Taylor-Powell E, Steele S. Wiscounsin: University of Wisconsin-Extension; 1996. Collecting evaluation data: Direct observation. Program Development and Evaluation; pp. 1–7. [Google Scholar]
- 27.Montesi G, Lechi A. Prevention of medication errors: Detection and audit. Br J Clin Pharmacol. 2009;67:651–5. doi: 10.1111/j.1365-2125.2009.03422.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Allan EL, Barker KN. Fundamentals of medication error research. Am J Hosp Pharm. 1990;47:555–71. [PubMed] [Google Scholar]
- 29.Dean B, Barber N. Validity and reliability of observational methods for studying medication administration errors. Am J Health Syst Pharm. 2001;58:54–9. doi: 10.1093/ajhp/58.1.54. [DOI] [PubMed] [Google Scholar]
- 30.Fahimi F, Ariapanah P, Faizi M, Shafaghi B, Namdar R, Ardakani MT. Errors in preparation and administration of intravenous medications in the intensive care unit of a teaching hospital: An observational study. Aust Crit Care. 2008;21:110–6. doi: 10.1016/j.aucc.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 31.Khalili H, Dashti-Khavidaki S, Talasaz AH, Mahmoudi L, Eslami K, Tabeefar H. Is deep vein thrombosis prophylaxis appropriate in the medical wards? A clinical pharmacists’ intervention study. Pharm World Sci. 2010;32:594–600. doi: 10.1007/s11096-010-9412-y. [DOI] [PubMed] [Google Scholar]
- 32.Kazemi A, Ellenius J, Pourasghar F, Tofighi S, Salehi A, Amanati A, et al. The effect of computerized physician order entry and decision support system on medication errors in the neonatal ward: Experiences from an Iranian teaching hospital. J Med Syst. 2011;35:25–37. doi: 10.1007/s10916-009-9338-x. [DOI] [PubMed] [Google Scholar]
- 33.Vessal G. Detection of prescription errors by a unit-based clinical pharmacist in a nephrology ward. Pharm World Sci. 2010;32:59–65. doi: 10.1007/s11096-009-9341-9. [DOI] [PubMed] [Google Scholar]
- 34.Fahimi F, Abbasi Nazari M, Abrishami R, Sistanizad M, Mazidi T, Faghihi T, et al. Transcription errors observed in a teaching hospital. Arch Iran Med. 2009;12:173–5. [PubMed] [Google Scholar]
- 35.Qureshi NA, Neyaz Y, Khoja T, Magzoub MA, Haycox A, Walley T. Physicians’ medication prescribing in primary care. In Riyadh City, Saudi Arabia. Literature review, part : Prescribing errors. East Mediterr Health J. 2011;17:140–8. [PubMed] [Google Scholar]
- 36.Franklin BD, Reynolds M, Shebl NA, Burnett S, Jacklin A. Prescribing errors in hospital inpatients: A three-centre study of their prevalence, types and causes. Postgrad Med J. 2011;87:739–45. doi: 10.1136/pgmj.2011.117879. [DOI] [PubMed] [Google Scholar]
- 37.Colton T. Boston: Little, Brown and Company; 1974. Statistics in Medicine; pp. 257–62. [Google Scholar]
- 38.Aspden P, Wolcott J, Bootman L, Cronewett LR. Boston: IOM; 2007. Preventing Medication Errors: Quality Series; pp. 108–15. [Google Scholar]
- 39.Segura-Cardona A, Berbesí-Fernández D, Cardona-Arango D, Ordóñez-Molina J. Preliminary construction of a questionnaire about knowledge of HIV/AIDS in Colombian veterans. Rev Peru Med Exp Salud Publica. 2011;28:503–7. doi: 10.1590/s1726-46342011000300015. [DOI] [PubMed] [Google Scholar]
- 40.Lu CY, Roughead E. Determinants of patient-reported medication errors: A comparison among seven countries. Int J Clin Pract. 2011;65:733–40. doi: 10.1111/j.1742-1241.2011.02671.x. [DOI] [PubMed] [Google Scholar]


