Abstract
Background:
Complex indeterminate Bosniak category III renal cystic masses are traditionally considered to be malignant in 50%. Our aim was to retrospectively evaluate the attenuation characteristics in multiphase computed tomography (CT) and to determinate the incidence of malignancy based on histological findings on all Bosniak category III renal cystic masses investigated in our department between April 3, 2007 and November 21, 2013.
Materials and Methods:
Quadriphasic multidetector CT images of nineteen patients (mean age: 56.5 ± 16.5 years) with radiologically detected Bosniak category III lesions were reviewed retrospectively. All lesions were surgically removed, and the incidence of malignancy, based on pathological results was determined.
Results:
Calcification was present in four lesions (21%). The mean largest diameter was 48.7 ± 28.8 mm. All lesions were multilobulated and septated. Of the 19 removed lesions, 16 (84%) were malignant, and 3 (16%) were benign (one inflammatory cyst including a nephrolith, one cystic nephroma and one atypical angiomyolipoma). CT and histological findings of 19 Bosniak III cysts were correlated.
Conclusion:
Our study demonstrated much higher prevalence of malignancy (84%) in radiologically detected Bosniak category III cysts than it has been described before. It may due to the era of modern multidetector CT technology and multiphase protocol.
Keywords: Bosniak classification, computed tomography, contrast media, differential diagnosis, neoplasm, nephrology, prevalence, renal cell cancer
INTRODUCTION
Bosniak category III cystic masses are of indeterminate origin and present suggestive signs of malignancy.[1] The typical appearance includes uniform wall thickening, thickened and irregular calcifications, and thickened and irregular or multiple septa (>1 mm) without an intracystic nodular lesion.[1] Enhancement must be present in these cysts (in the thickened wall or in the septa). In case of no enhancement, Bosniak IIF category cysts are defined.
These moderately complicated Bosniak III cysts demonstrate a precontrast density of 0-20 Hounsfield Units.[2] Due to the 50% risk of malignancy, the recommended treatment for Bosniak category III lesions is surgical resection including tumor enucleation, partial or total nephrectomy.[1,3] Laparoscopic surgery for these complex cysts has been found to be a safe, feasible, and effective approach with minimal morbidity.[4]
Although the malignant potential of Bosniak category III cystic lesions is known to be approximately 50%,[5] several studies demonstrated different malignancy rates ranging from 31%[6] to 60%.[7,8] The confusion can be partly referred to the higher incidence of the detection of renal masses smaller than 3 cm most probably due to the increasing number of abdominal image studies.[9] In addition, some of these studies were performed in the 1990's based on spiral computed tomography (CT) scan use, which is totally different in results compared with multidetector CT. A good degree of interobserver agreement exists in the assessment of complex renal cysts (≥Bosniak category IIF) between radiologists.[10] In addition, malignancy rate is associated with the size of the cyst (>2 cm), male gender, and younger patient age (<50 years).[11]
Due to the availability of multiphase CT imaging technology of complex renal cystic masses, unenhanced, corticomedullary, nephrographic, and excretory phases can be performed to recognize the enhancement characteristics.[12] Enhancement is the strongest predictor of accurate diagnosis, identifying a 25-45% likelihood of malignancy.[13] To this end, our aim was to retrospectively analyze the Bosniak III category cystic tumor attenuation characteristics in multiphase CT and to determinate the incidence of malignancy based on histological findings.
MATERIALS AND METHODS
We performed a retrospective review of Bosniak III lesions to evaluate the pathologic diagnoses and clinical features associated with malignancy. Nineteen patients with radiological diagnosis of Bosniak category III cysts underwent surgical resection and histopathological evaluation. These cases were originally read as Bosniak III cystic renal lesion by the same radiologist over the 6-year period of time. We performed nephron sparing surgery from open lumbar surgical approach in thirteen cases, two laparoscopic and four open nephrectomies. CT images were analyzed retrospectively by one expert uro-radiologist to characterize the renal lesions (size, calcification, side) via a picture archiving and communication system (PACS Medical Workstation, Philips Medical Systems, Shelton, CT, USA) from April 3, 2007 to November 21, 2013 in reports from CT imaging studies performed in patients of 18 years or older. Institutional review board approval was not required, and informed consent was waived due to the retrospective feature of this study.
All multidetector CT scans (Philips Brilliance 16, Philips Healthcare, Amsterdam, the Netherlands) were performed according to a standard protocol covering the abdomen from the diaphragm to the iliac crest, while the patient was placed in the supine position. Non-ionic contrast agent (Ultravist 370, Bayer AG, Leverkusen, Germany; Optiray 350, Tyco Health/Mallinckrodt, St. Louis, MO, USA; or Visipaque 320, GE Healthcare, Waukesha, WI, USA) was administered (1.5 mL/kg), adapted to each weight kg, and was automatically injected at a flow-rate of 3 mL/s (power injector was utilized). A collimation setting of 16 mm × 1.5 mm was used, and the reconstructed slice thickness was 2 mm. Unenhanced, corticomedullary (30 s), nephrographic (70 s), and excretory phases (180 s) were imaged. The lesions were categorized based on 2009 TNM classification (pT1a <4 cm, pT1b <7 cm, - pT2a between 7 cm and 10 cm, pT2b >10 cm, but localisation to the organ).
RESULTS
Nineteen patients with Bosniak III lesions were included in the study. The mean age of the patients was 56.5 ± 16.5 years (11 males and 8 females). Three patients had hematuria before the imaging study (16%) and the other patients complained flank pain or were asymptomatic. There were 9 (47%) lesions on the right, 10 (53%) lesions on the left side. Calcification was present in the wall of four lesions (21%). The mean largest diameter was 48.7 ± 28.8 mm. All lesions were multilobulated and septated. No intracystic nodule was present in the lesions [Figure 1]. The same enhancement criteria were considered in all positive cases (absolute value, 15 HU) in order to call the lesions a Bosniak III category lesion. The enhancement was evaluated by drawing regions of interest of 5 mm2. The mean enhancement indicated 31.8 ± 12.5 HU in the unenhanced, 59.9 ± 26.0 in the arterial, 76.5 ± 32.2 HU in the venous and 69.1 ± 31 HU in the late phase. No subtraction imaging was utilized.
Figure 1.
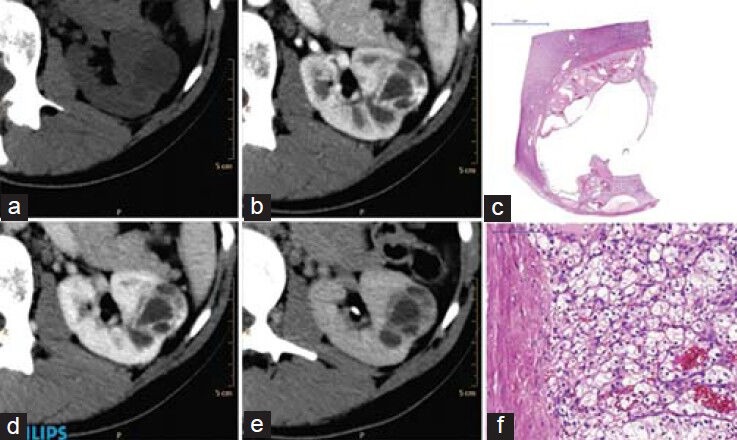
Computed tomography (CT) appearance of a typical Bosniak III category cystic lesion. Thickened irregular wall and septas with contrast enhancement can be observed in the lesion located in the middle third of the left kidney. Unenhanced (a), corticomedullary (b), nephrographic (c) and excretory phases (d) axial CT images. Histological H and E stained sections displaying an intracystic clear cell renal cell cancer at magnification ×1 (e) and ×20 (f)
Histological analysis confirmed that 16 of 19 lesions were conventional clear cell renal cell carcinomas (ccRCC) (84%). According to the TNM stage, eight of them proved to be pT1a (<4 cm in diameter and organ confined), six of them was pT1b (4-7 cm in diameter and organ confined), and two of them was pT2b (>10 cm in diameter and organ confined). The three remaining lesions were histologically proven to be an inflamed cyst including a nephrolith [Figure 2], a cystic nephroma [Figure 3] and an atypical “fat-poor” angiomyolipoma [Figure 4].
Figure 2.
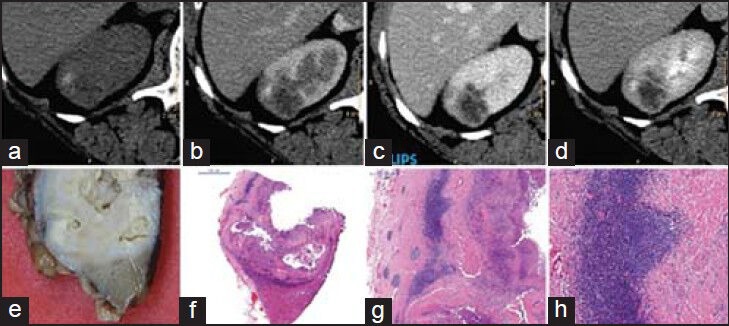
Computed tomography (CT) appearance of the inflammated cyst including a nephrolith mimicking a Bosniak III lesion. A 45-year-old female with a history of pyuria, hematuria and bacteruria. Thickened irregular wall and septa with contrast enhancement can be observed in the upper third of the right kidney. Unenhanced (a), corticomedullary (b), nephrographic (c) and excretory (d) phases axial CT images. Macroscopic documentation (e), with H and E stained histological sections at magnification ×1 (f), ×5 (g) and ×10 (h)
Figure 3.
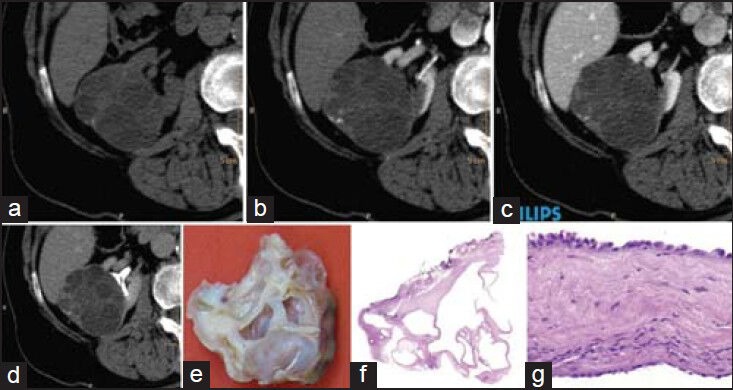
Computed tomography (CT) appearance of the cystic nephroma mimicking a Bosniak III lesion. 78-year-old female with a history of limb and lower back pain, and expansive subcostal pain in the past months. Thickened irregular wall and septa with contrast enhancement can be observed in the upper third of the right kidney. Unenhanced (a), corticomedullary (b), nephrographic (c) and excretory phases (c) axial CT images. Macroscopic documentation (e) with H and E stained histological sections at magnification ×1 (f) and ×20 (g)
Figure 4.
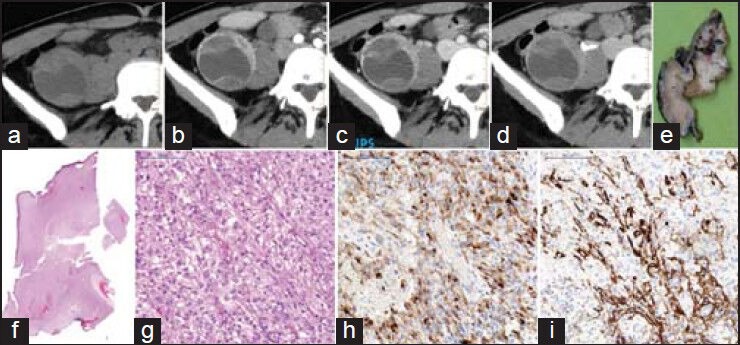
Computed tomography (CT) appearance of the atypical angiomyolipoma mimicking a Bosniak category III lesion. 37-year-old asymptomatic lady. Thickened, irregular wall and septa with contrast enhancement can be appreciated in the lower third of the right kidney. Unenhanced (a), corticomedullary (b), nephrographic (c) and excretory phases (d) axial CT images. Macroscopic documentation (e) with H and E stained histological sections at magnification ×1 (f) and ×20 (g). Immunohistochemical images of HMB-45 (h) and SMA (i) of the identical region of the tumor at magnification ×20
DISCUSSION
Our study demonstrated a higher prevalence of malignancy (84%) in radiologically detected Bosniak category III cysts than it had been described before,[5,6,7,8,11] and draws attention to the differential diagnostic obstacles.
Most of the radiologists believe that the malignancy rate of Bosniak category III cystic lesions is nearly 50%.[5] However, several studies demonstrated different malignancy rates, some studies certified a higher prevalence, usually around 54%.[8,11] These to date published studies have used older CT technology.[6,7,13,14] Even if Goenka et al. and Smith et al. had a larger sample size in their retrospective studies than ours, no standardized protocol was applied, and different equipments were used during the long data collecting period.[8,15,16] Graumann et al. collected data between 2003 and 2009 and all patients were examined with the same CT scanner and CT protocol similarly to our study, however, only Bosniak IIF cysts were analyzed.[17] However, these previous studies had serious limitations:
Various CT technologies were applied,
Multiple readers interpreted the CT images and
Bosniak criteria were applied inconsistently.
In our study, higher rate of malignancy was unexpectedly found compared to most of these past studies; however, the same affiliated urogenital radiologist interpreted all images and the same scanner and standardized CT protocol was applied for all patients during the last 6 years. Graumann et al. also demonstrated on Bosniak IIF cysts that categorization of complex cystic changes in the kidney must be performed with high-quality CT in several phases.[17] In this paper authors also argued that in order to detect enhancement in small areas such as a septum or the wall of a cyst, a CT without contrast (non-contrast CT) and a minimum of two CT single-bolus phases with contrast-enhanced CT and cardiac CT in an arterial and venous phase is needed.[17]
The literature on interobserver agreement is controversial: Interobserver variation in Bosniak IIF and III category cysts is lower in academic centers, however, in the real clinical practice tends to be higher. For instance, a study of 113 complex renal cystic masses demonstrated that the interpersonal variability is significant among the Bosniak groups II, IIF and III, and the overall category was changed in 20-54% following histological results.[16] In contrast to this finding, we found a relatively objective scoring based on the above mentioned parameters.
Pathological studies have revealed that the most frequent malignant renal tumors in the series is usually conventional ccRCC, taking into account that only 4-15% of all renal cell carcinomas represent cystic growth pattern.[8,18] Other reports suggested higher rate (40%) of renal cell carcinomas having cystic component.[19] Since these subjects should undergo surgery, Bosniak III cystic lesions which cause a differential diagnostic problem (16% in our sample) may be problematic. The three remaining lesions included cystic lesions such as an inflammated cyst, a cystic nephroma and an atypical angiomyolipoma showed identical imaging features with Bosniak category III cystic lesions (contrast enhancement in the thickened wall or thickened and irregular septa, no sign of any intracystic contrast enhancing nodular lesion) [Figures 2–4]. However, the most surprising finding was the atypical angiomyolipoma with the absence of fatty component, which also appeared cystic radiologically. Angiomyolipomas with undetectable fat occur in nearly 15% of angiomyolipomas, and malignancy should be suspected if intratumoral calcifications, large, irregular tumor invading the perirenal envelope or sinus fat, large necrotic tumor with small foci of fat or nonfatty lymph nodes or venous invasion is present.[20] Accordingly, Bosniak III cystic renal lesions could cause difficulties in the differential diagnosis.
In case of these indeterminate lesions, the presence of spontaneous bleeding with concomitant multiple angiomyolipomas, and tuberous sclerosis complex may help the diagnosis on CT imaging.[20] Localized cystic disease, a rare, nongenetic and nonprogressive cystic disease, is an additional mimic of cystic neoplasms or hereditary polycystic disease which should be kept in mind.[21] A recent study showed that diagnostic accuracy improves for differentiating renal cell carcinoma if Bosniak classification and enhancement differences measured on CT between the precontrast and maximal enhancement phases is combined.[22]
In order to reduce unnecessary surgeries for benign lesions, a protocol is needed because that is the current dilemma in this category. Our findings mainly highlight the opposite of the findings of previous studies: The hazard of leaving a malignant lesion in the patient is higher than operating a benignant lesion. In our opinion, additional diagnostic tests are not beneficial, including intraoperative ultrasound (e.g., operator-dependent, difficult to perform, radiologist is needed in the operating theater; if the surgery is already going you can already resect the cyst, the surgical risk remains the same). Biopsy has an increased risk of bleeding, tumor cell spread, cytology is less informative in case of cystic lesions in comparison with solid tumors, and pseudonegative results are relatively often. In general, magnetic resonance imaging (MRI) is similar to CT in the majority of cystic renal masses, but additional septa, thickening of the wall and/or septa, or enhancement are sometimes better depicted by MRI, which may cause a lesion to be upgraded.[23] In addition, quantitative diffusion-weighted MRI is a promising new sequence in the differentiation of benign from malignant renal tumors, even histologically subtyping renal cell cancer.[24] In the recent years, more emphasis has been put on the value of contrast-enhanced ultrasound in the imaging of complex renal masses since contrast-enhanced ultrasound was superior to CT for the diagnosis of malignancy in complex cystic renal masses.[25] Contrast-enhanced ultrasound is another important and widely used method in the detection and differentiation of cystic renal masses, which might better visualize septa number, septa and/or wall thickness, solid component and the enhancement of some renal cystic masses than CT, resulting in upgrade of Bosniak classification and affecting their treatment plan.[26]
Biopsy of these complicated cystic lesions is not as reliable and often false negative.[27] Latest guidelines recommend that biopsy in category III lesions is only useful in selected cases, such as in patients with poor general condition to avoid surgery, and if the chance of an infected cyst or abscess is high.[27] According to the Guidelines of the European Association of Urology all the renal lesions should be removed, when CT raises the suspicion for malignancy. Since the lack of effective systemic treatment (e.g., chemotherapy or irradiation) surgery remains the only effective tool in our hands. All the patients fit for surgery must be operated (laparoscopic or open surgery, nephrectomy or organ preserving surgery), and only high risk, elderly patients could be observed. All the included patients in our study were fit for surgical treatment.
Smith et al. recommend only observation in patients with Bosniak III lesions and multiple co-morbidities or short life expectancy due to low chance of local progression or metastatic disease.[8,28] Our data do not support this recommendation due to the unexpectedly high rate of malignancies. Especially in these cases, several authors suggest the use of radiofrequency ablation of these lesions; however, because radiofrequency ablation treatment destroys tissue without yielding a diagnostic specimen, preoperative renal biopsy may be necessary.[29]
This study possesses some limitations. The major limitation is the number of cases, although, they were comparable to those in previous investigations.[6,7,13,14] Second, the retrospective nature of the study do not predispose to selection bias, since the study population was not limited to symptomatic patients (e.g., due to hematuria) with preoperative multiphase CT examination. As previously mentioned, the use of multidetector CT with multiphase technique with strict protocol using small region of interests in contrast to spiral CT studies can strongly influence the results. In fact, there is a possibility that some Bosniak III cysts are categorized as Bosniak II cysts, therefore, no surgery, that is, histological result is available in these lesions, which could bias our results since our findings did not include the underestimated cases.
CONCLUSION
This study confirms a high prevalence of malignancy (in 84% of patients) with Bosniak category III lesions which can be attributed mainly due to the era of modern multidetector CT technology and multiphase protocol. The findings underpin the importance of surgical resection in Bosniak III lesions due to the high prevalence of malignancy. Our results suggest that certain atypical benign lesions, such as inflamed cyst, cystic nephroma or atypical angiomyolipoma may mimic Bosniak category III cystic tumors yielding to a differential diagnostic dilemma.
AUTHORS’ CONTRIBUTIONS
PB, ADT, DLT, AMS, GP, BF, JG, PN, VB, KK, AS carried out the design and coordinated the study, participated in most of the experiments and prepared the manuscript. PB, GP, BF, JG provided assistance for all experiments. All authors have read and approved the content of the manuscript.
Footnotes
Source of Support: A.M.S. was supported by the European Union and the State of Hungary, co-financed by the European Social Fund in the framework of TÁMOP 4.2.4.A/2-11-1-2012-0001 ‘National Excellence Program.
Conflict of Interest: None declared.
REFERENCES
- 1.Prando A. Incidence of malignancy in complex cystic renal masses (Bosniak category III): Should imaging-guided biopsy precede surgery? Int Braz J Urol. 2003;29:175–6. [PubMed] [Google Scholar]
- 2.Bosniak MA. Problems in the radiologic diagnosis of renal parenchymal tumors. Urol Clin North Am. 1993;20:217–30. [PubMed] [Google Scholar]
- 3.Whelan TF. Guidelines on the management of renal cyst disease. Can Urol Assoc J. 2010;4:98–9. doi: 10.5489/cuaj.10023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pinheiro T, Sepulveda F, Natalin RH, Metrebian E, Medina R, Goldman SM, et al. Is it safe and effective to treat complex renal cysts by the laparoscopic approach? J Endourol. 2011;25:471–6. doi: 10.1089/end.2010.0254. [DOI] [PubMed] [Google Scholar]
- 5.Bosniak MA. The current radiological approach to renal cysts. Radiology. 1986;158:1–10. doi: 10.1148/radiology.158.1.3510019. [DOI] [PubMed] [Google Scholar]
- 6.Cloix P, Martin X, Pangaud C, Maréchal JM, Bouvier R, Barat D, et al. Surgical management of complex renal cysts: A series of 32 cases. J Urol. 1996;156:28–30. [PubMed] [Google Scholar]
- 7.Wilson TE, Doelle EA, Cohan RH, Wojno K, Korobkin M. Cystic renal masses: A reevaluation of the usefulness of the Bosniak classification system. Acad Radiol. 1996;3:564–70. doi: 10.1016/s1076-6332(96)80221-2. [DOI] [PubMed] [Google Scholar]
- 8.Smith AD, Remer EM, Cox KL, Lieber ML, Allen BC, Shah SN, et al. Bosniak category IIF and III cystic renal lesions: Outcomes and associations. Radiology. 2012;262:152–60. doi: 10.1148/radiol.11110888. [DOI] [PubMed] [Google Scholar]
- 9.Wunderlich H, Reichelt O, Schumann S, Schlichter A, Kosmehl H, Werner W, et al. Nephron sparing surgery for renal cell carcinoma 4 cm. or less in diameter: Indicated or under treated? J Urol. 1998;159:1465–9. doi: 10.1097/00005392-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 10.El-Mokadem I, Budak M, Pillai S, Lang S, Doull R, Goodman C, et al. Progression, interobserver agreement, and malignancy rate in complex renal cysts (= Bosniak category IIF) Urol Oncol. 2014;32:24e1–7. doi: 10.1016/j.urolonc.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 11.Han HH, Choi KH, Oh YT, Yang SC, Han WK. Differential diagnosis of complex renal cysts based on lesion size along with the Bosniak renal cyst classification. Yonsei Med J. 2012;53:729–33. doi: 10.3349/ymj.2012.53.4.729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohan RH, Sherman LS, Korobkin M, Bass JC, Francis IR. Renal masses: Assessment of corticomedullary-phase and nephrographic-phase CT scans. Radiology. 1995;196:445–51. doi: 10.1148/radiology.196.2.7617859. [DOI] [PubMed] [Google Scholar]
- 13.Siegel CL, McFarland EG, Brink JA, Fisher AJ, Humphrey P, Heiken JP. CT of cystic renal masses: Analysis of diagnostic performance and interobserver variation. AJR Am J Roentgenol. 1997;169:813–8. doi: 10.2214/ajr.169.3.9275902. [DOI] [PubMed] [Google Scholar]
- 14.Aronson S, Frazier HA, Baluch JD, Hartman DS, Christenson PJ. Cystic renal masses: Usefulness of the Bosniak classification. Urol Radiol. 1991;13:83–90. doi: 10.1007/BF02924596. [DOI] [PubMed] [Google Scholar]
- 15.Goenka AH, Remer EM, Smith AD, Obuchowski NA, Klink J, Campbell SC. Development of a clinical prediction model for assessment of malignancy risk in Bosniak III renal lesions. Urology. 2013;82:630–5. doi: 10.1016/j.urology.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 16.Weibl P, Klatte T, Kollarik B, Waldert M, Schüller G, Geryk B, et al. Interpersonal variability and present diagnostic dilemmas in Bosniak classification system. Scand J Urol Nephrol. 2011;45:239–44. doi: 10.3109/00365599.2011.562233. [DOI] [PubMed] [Google Scholar]
- 17.Graumann O, Osther SS, Karstoft J, Hørlyck A, Osther PJ. Evaluation of Bosniak category IIF complex renal cysts. Insights Imaging. 2013;4:471–80. doi: 10.1007/s13244-013-0251-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hartman DS, Davis CJ, Jr, Johns T, Goldman SM. Cystic renal cell carcinoma. Urology. 1986;28:145–53. doi: 10.1016/0090-4295(86)90109-3. [DOI] [PubMed] [Google Scholar]
- 19.Charboneau JW, Hattery RR, Ernst EC, 3rd, James EM, Williamson B, Jr, Hartman GW. Spectrum of sonographic findings in 125 renal masses other than benign simple cyst. AJR Am J Roentgenol. 1983;140:87–94. doi: 10.2214/ajr.140.1.87. [DOI] [PubMed] [Google Scholar]
- 20.Hélénon O, Merran S, Paraf F, Melki P, Correas JM, Chrétien Y, et al. Unusual fat-containing tumors of the kidney: A diagnostic dilemma. Radiographics. 1997;17:129–44. doi: 10.1148/radiographics.17.1.9017804. [DOI] [PubMed] [Google Scholar]
- 21.Ding Y, Chen L, Deng FM, Melamed J, Fan R, Bonsib S, et al. Localized cystic disease of the kidney: Distinction from cystic neoplasms and hereditary polycystic diseases. Am J Surg Pathol. 2013;37:506–13. doi: 10.1097/PAS.0b013e318271eff9. [DOI] [PubMed] [Google Scholar]
- 22.Song C, Min GE, Song K, Kim JK, Hong B, Kim CS, et al. Differential diagnosis of complex cystic renal mass using multiphase computerized tomography. J Urol. 2009;181:2446–50. doi: 10.1016/j.juro.2009.01.111. [DOI] [PubMed] [Google Scholar]
- 23.Israel GM, Hindman N, Bosniak MA. Evaluation of cystic renal masses: Comparison of CT and MR imaging by using the Bosniak classification system. Radiology. 2004;231:365–71. doi: 10.1148/radiol.2312031025. [DOI] [PubMed] [Google Scholar]
- 24.Inci E, Hocaoglu E, Aydin S, Cimilli T. Diffusion-weighted magnetic resonance imaging in evaluation of primary solid and cystic renal masses using the Bosniak classification. Eur J Radiol. 2012;81:815–20. doi: 10.1016/j.ejrad.2011.02.024. [DOI] [PubMed] [Google Scholar]
- 25.Quaia E, Bertolotto M, Cioffi V, Rossi A, Baratella E, Pizzolato R, et al. Comparison of contrast-enhanced sonography with unenhanced sonography and contrast-enhanced CT in the diagnosis of malignancy in complex cystic renal masses. AJR Am J Roentgenol. 2008;191:1239–49. doi: 10.2214/AJR.07.3546. [DOI] [PubMed] [Google Scholar]
- 26.Park BK, Kim B, Kim SH, Ko K, Lee HM, Choi HY. Assessment of cystic renal masses based on Bosniak classification: Comparison of CT and contrast-enhanced US. Eur J Radiol. 2007;61:310–4. doi: 10.1016/j.ejrad.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 27.Bosniak MA. The Bosniak renal cyst classification: 25 years later. Radiology. 2012;262:781–5. doi: 10.1148/radiol.11111595. [DOI] [PubMed] [Google Scholar]
- 28.Berland LL, Silverman SG, Gore RM, Mayo-Smith WW, Megibow AJ, Yee J, et al. Managing incidental findings on abdominal CT: White paper of the ACR incidental findings committee. J Am Coll Radiol. 2010;7:754–73. doi: 10.1016/j.jacr.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 29.Harisinghani MG, Maher MM, Gervais DA, McGovern F, Hahn P, Jhaveri K, et al. Incidence of malignancy in complex cystic renal masses (Bosniak category III): Should imaging-guided biopsy precede surgery? AJR Am J Roentgenol. 2003;180:755–8. doi: 10.2214/ajr.180.3.1800755. [DOI] [PubMed] [Google Scholar]


