Abstract
Rationale: Pneumonia is a frequent cause of hospitalization, yet drivers of post-pneumonia morbidity remain poorly characterized. Causes of hospital readmissions may elucidate important sources of morbidity and are of particular interest given the U.S. Hospital Readmission Reductions Program.
Objectives: To review the primary diagnoses of early (≤30 d) and late (≥31 d) readmissions after pneumonia hospitalization.
Methods: Systematic review of MEDLINE, Embase, and CINAHL databases. We identified original research studies of adults aged 18 years or older, hospitalized for pneumonia, and for whom cause-specific readmission rates were reported. Two authors abstracted study results and assessed study quality.
Measurements and Main Results: Of the 1,243 citations identified, 12 met eligibility criteria. Included studies were conducted in the United States, Spain, Canada, Croatia, and Sweden. All-cause 30-day readmission rates ranged from 16.8 to 20.1% across administrative studies; the weighted average for the studies using chart review was 11.6% (15.6% in United States–based studies). Pneumonia, heart failure/cardiovascular causes, and chronic obstructive pulmonary disease/pulmonary causes are the most common reasons for early readmission after pneumonia hospitalization. Although it was the single most common cause for readmission, pneumonia accounted for only 17.9 to 29.4% of all 30-day readmissions in administrative studies and a weighted average of 23.0% in chart review studies. After accounting for study population, there was no clear difference in findings between claims-based versus chart-review studies. Few studies assessed readmissions beyond 30 days, although the limited available data suggest similar primary diagnoses for early and late readmissions. No studies assessed whether reasons for readmission were similar to patients’ reasons for healthcare use before hospitalization.
Conclusions: Pneumonia, heart failure/cardiovascular disease, and chronic obstructive pulmonary disease/pulmonary disease are the most common readmission diagnoses after pneumonia hospitalization. Although pneumonia was the most common readmission diagnosis, it accounted for only a minority of all readmissions. Late readmission diagnoses are less thoroughly described, and further research is needed to understand how hospitalization for pneumonia fits within the broader context of patients’ health trajectory.
Keywords: patient readmission, health policy, outcomes assessment (health care), International Classification of Diseases
After childbirth, pneumonia is the most common cause of hospitalization in the United States (1). Each year, 1.1 million patients are hospitalized with pneumonia, and the vast majority of patients survive to hospital discharge (2). Once believed to be an acute illness with minimal repercussions, pneumonia is increasingly recognized to be a fundamental turning point in patients’ lives (3), resulting in new functional limitations (4), cognitive decline (4, 5), and increased long-term mortality (3, 6–8). The causes of this persistent mortality burden remain unclear, and reasons for rehospitalization may identify important sources of morbidity in this population.
After the launch of the Hospital Readmission Reduction Program in 2013 (9), U.S. hospitals with greater-than-expected 30-day readmission rates after acute myocardial infarction, pneumonia, and congestive heart failure hospitalizations have been subject to penalties from the Center for Medicare and Medicaid Services (9). Penalties average ∼$125,000 per hospital (10) and can reach $1 million for large academic centers paying the highest penalty rate (11).
As a result of the new legislation, hospitals across the United States have scrambled to develop interventions to reduce readmissions. To inform these efforts, Jencks and colleagues (12) and Dharmarajan and colleagues (13) analyzed Medicare claims in fee-for-service beneficiaries to determine the primary diagnoses associated with early hospital readmission. However, administrative data—particularly diagnosis-related groups (DRGs)—may not reliably identify hospitalizations for pneumonia (14). More recent work has also demonstrated that pneumonia is increasingly coded as sepsis (15). Beyond these concerns about the validity of diagnoses in administrative data, Jencks and Dharmarajan (12, 13) do not consider readmission diagnoses in non-Medicare patients or reasons for readmission beyond 30 days.
Given the long-lasting—and incompletely defined—impact of pneumonia, the current regulatory incentives to reduce readmissions, concern about the validity of administrative data, and the rising incidence of pneumonia (16, 17), we sought to systematically review studies measuring the causes of readmission after pneumonia hospitalization. We aim to answer several questions in this review: (1) What methodological approaches have been used to measure the reasons for readmission after pneumonia hospitalization, and do findings differ by study methodology? (2) What are the primary diagnoses associated with early (≤30-d) readmission after pneumonia hospitalization, relevant to the financial penalties? (3) What are the primary diagnoses associated with late (≥31-d) readmissions that may help explain the morbidity and excess mortality experienced by pneumonia survivors? (4) To what extent are the reasons for hospital readmission after pneumonia similar to patients’ reasons for healthcare use before pneumonia?
Methods
Information Sources and Search Strategy
To identify studies that assessed the reason for readmission after a pneumonia hospitalization, we searched MEDLINE via PubMed (1966–2014), Embase (1974–2014), and CINAHL (1981–2014) as of May 14, 2014. We used Boolean operators, Boolean logic, and—in MEDLINE and EMBASE searches—controlled vocabulary for each keyword. Specifically, we performed the following searches: In PubMed, “pneumonia” [MeSH] OR “pneumonia” [title/abstract] AND “patient readmission” [MeSH] OR “patient readmission” [title/abstract]; in Embase, ‘pneumonia’/exp OR ‘pneumonia’ AND ‘hospital’/exp OR ‘hospital’ [Emtree] AND (‘readmission’/exp OR readmission); in CINAHL, SU “pneumonia” AND TX “readmission.” We set no limits on language, patient age, or type of study in the initial searches but did exclude trade magazine and dissertation publications in our CINAHL search. We also hand-searched the reference lists of included citations.
Because pneumonia hospitalizations are increasingly coded as sepsis (15), we conducted preliminary searches for studies examining readmissions after sepsis hospitalizations. We used an identical search strategy to the one described above, substituting “sepsis” for “pneumonia.” However, we identified just one conference abstract that evaluated reasons for readmissions after sepsis hospitalization; given the paucity of published information, we maintained our focus on pneumonia for ease of presentation. To increase the sensitivity of our search, we also performed [title/abstract] searches of the word “rehospitalization.” This yielded an additional 71 citations not identified in our controlled vocabulary search, all of which we excluded after title review.
Study Eligibility and Selection Criteria
Criteria for study eligibility were (1) adult subjects, aged 18 years or older; (2) identification of index hospitalization for pneumonia; (3) measurement of cause-specific readmission rates; and (4) original research publication. Exclusion criteria included (1) case reports, (2) case series with fewer than 10 subjects, and (3) nonoriginal research articles. For studies using identical datasets, we included the study reporting outcomes on the most patients.
One author (H.C.P.) reviewed all titles for possible inclusion. Two authors (H.C.P. and M.W.S.) independently reviewed all abstracts identified potentially eligible after title review. Two authors (H.C.P. and M.W.S). then independently reviewed the full text of each article selected for inclusion by one or more authors. Disagreement regarding eligibility of a full text was adjudicated by discussion between H.C.P. and M.W.S. We calculated interrater agreement between the authors with kappa coefficients for (1) selection of abstracts for full text review, and (2) selection of full texts for inclusion (18).
To encompass all available information, we also present readmission statistics from the Nationwide Inpatient Sample (NIS)—a stratified 20% sample of U.S. community hospitals—available online for 2009 to 2011 at the Healthcare Cost and Utilization Project website (19). We queried readmission rates after hospitalizations with a primary diagnosis of pneumonia, defined by clinical classification software category for pneumonia. We determined the rate of all-cause readmission, readmission with a primary diagnosis of pneumonia, and readmission with a secondary diagnosis of pneumonia in 2009 to 2011 for patients 18 years of age or older and for the subset of patients 65 years of age or older.
Data Abstraction
For each eligible study, two authors (H.C.P., M.W.S.) independently abstracted data on study methodology, definitions of exposure and outcome variables, and the overall and cause-specific rates of readmission using a standardized abstraction tool (see Appendix E1 in the online supplement). Discrepancies in abstracted data were adjudicated by discussion between H.C.P. and M.W.S.
Calculation of Readmission Rates
Some studies reported readmission rates stratified by a particular characteristic (e.g., by year of index admission). To simplify the presentation of results, we combined the strata and calculated a single readmission rate.
Studies also used different equations to calculate readmission rates:
| (1) |
| (2) |
| (3) |
To allow for meaningful comparisons across studies, we recalculated readmission rates when necessary to present all readmission rates using Equation 2. When necessary, we contacted study authors to obtain additional data to complete these calculations. Due to marked heterogeneity in the sample size, demographics, and methodology across studies, we did not perform a metaanalysis. However, we present pooled estimates of readmission rates (weighted by study size) for studies using chart review to assign readmission diagnosis.
Study Quality
For each eligible study, H.C.P. and M.W.S. independently assessed study quality using criteria adapted from the STrengthening the Reporting of OBservational studies in Epidemiology guidelines for reporting observational research: (1) representativeness of the study population, (2) mechanism to identify the index hospitalization for pneumonia, and (3) mechanism to identify and assess the cause of hospital readmission (20).
Unfortunately, there is no generally accepted optimal method to identify index hospitalizations or readmissions for pneumonia. Studies assessing claims-based algorithms reach differing conclusions regarding the validity of administrative data (14, 21). Furthermore, the signs and symptoms of pneumonia are nonspecific, and no collection of signs, symptoms, or even radiologic findings confirm a diagnosis of pneumonia. Thus, reviewing patients’ charts may also result in misclassification of the primary hospital diagnosis. With no consensus on the best method to identify pneumonia, we did not rate studies on quality and did not exclude any studies based on quality assessment.
Results
Search Results
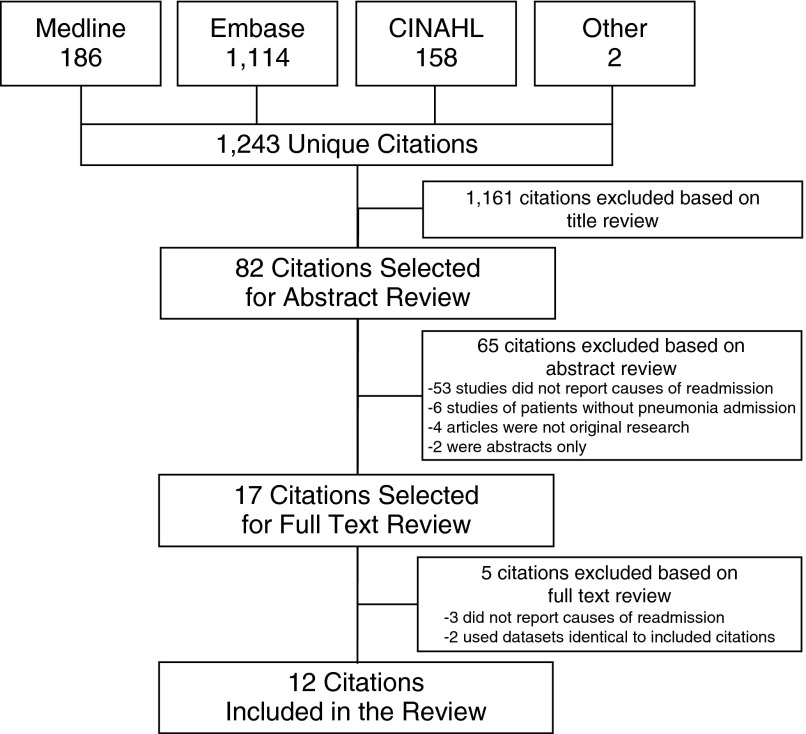
We identified 1,460 citations, of which 12 studies met eligibility criteria (Figure 1). Reviewer agreement on selection of abstracts for full-text evaluation was 88.9% (κ = 0.62) and for inclusion of articles in the review was 100% (κ = 1.0).
Figure 1.
Flow diagram for study search.
Characteristics of the Included Studies
Study characteristics are provided in Table 1, and study-specific main findings are detailed in Table 2. Studies varied widely in their size, methodology, length of follow-up, and demographics. Study populations ranged from single hospital units to nationwide administrative datasets. The number of readmissions evaluated ranged from fewer than 100 in most of the chart review studies to more than 100,000 in the larger studies of administrative claims. Mean age of the patients ranged from 59 to 81 years, and some studies were limited to elderly populations. Follow-up ranged from 30 days to several years. Studies were conducted in the United States (n = 8), Spain (n = 2), Canada (n = 1), Croatia (n = 1), and Sweden (n = 1).
Table 1.
Characteristics of studies reporting reason for readmission after hospitalization for pneumonia
| Author (Reference) | Country | Study Population | Enrollment Years | Index Discharges (Alive) | Age, (Mean or Median, yr) | Follow-up Duration | All-Cause 30-d Readmission Rate (%) | 30-d Readmission Rate for Pneumonia (%) |
|---|---|---|---|---|---|---|---|---|
| Studies using claims assessment to determine of cause for readmission | ||||||||
| Hedlund (22) | Sweden | 1 Hospital, specific unit | 1987 | 241 | 62 | Up to 3 yr | — | — |
| 1991–1993 | 95 | 69.6 | 6 mo | — | — | |||
| Metersky (29) | United States | Connecticut Medicare Beneficiaries | 1992–1997 | 34,500 | 80 | 30 d | — | 3.4 |
| Bohannon (30) | United States | 1 Hospital | 1999–2000 | 892 | 81.3 | 1 yr | 16.8 | — |
| Polić-Vizintin (31) | Croatia | 7 Hospitals | 1998–2000 | 180 | 66 | Up to 3 yr | — | — |
| Johnstone (24) | Canada | 6 Hospitals | 2000–2002 | 2,950 | 68.9 | Median 3.8 yr | 2.2 | |
| Jencks (12) | United States | All fee-for-service Medicare beneficiaries | 2003–2004 | — | — | 1 yr | 20.1 | 5.9 |
| Dharmarajan (13) | United States | All fee-for-service Medicare beneficiaries | 2007–2009 | 1,168,624 | 80 | 30 d | 18.3 | 4.1 |
| HCUP (NIS, patients 18+ yr) (19) | United States | 20% Stratified sample of U.S. community hospitals | 2009–2011 | 2,544,265 | — | 30 d | 16.8 | 3.0 |
| Studies using chart review to determine cause for readmission | ||||||||
| Jasti (23) | United States | 7 Hospitals | 1998–1999 | 577 | 71 | 30 d | 12 | 2.4 |
| Capelastegui (25) | Spain | 1 Hospital | 2003–2007 | 1,117 | 69 | 30 d | 7.3 | 2.6 |
| Adamuz (26) | Spain | 1 Hospital | 2007–2009 | 828 | 71 | 30 d | 8.7 | 3.4 |
| Aliberti (27) | United States | 1 Hospital | 2001–2006 | 464 | 72 | 30 d | 13.6 | 3.9 |
| Shorr (28) | United States | 1 Hospital | 2010 | 771 | 59 | 30 d | 19.3 | 1.4 |
HCUP = Healthcare Cost and Utilization Project; NIS = Nationwide Inpatient Sample.
Table 2.
Major findings of studies reporting reason readmission after hospitalization for pneumonia
| Author (Reference) | Year | Country | Major Findings |
|---|---|---|---|
| Studies with claims assessment to determine of cause for readmission | |||
| Hedlund (22) | 1995 | Sweden | 20.7% of patients were readmitted with pneumonia within average of 31 mo follow-up period; 8.1 episodes pneumonia per 100 person-years in pneumonia survivors vs. 1.2 in survivors of nonpneumonia hospitalizations. |
| Hedlund (22) | 1995 | Sweden | At 6 mo, 22% of patients were readmitted. Readmissions for respiratory tract infections occurred in 5.3%. The next most common reasons for readmission were vascular diseases (5.3%) and malignancy (3.2%). |
| Metersky (29) | 2000 | United States | At 30 d, 3.4% of patients readmitted with pneumonia. |
| Bohannon (30) | 2003 | United States | All-cause readmissions were 16.8% at 30 d, 35.6% at 6 mo, and 46% at 1 yr. At 1 yr, 8.1% of patients were readmitted for pneumonia-related causes. The next most common causes were CHF (3.8%), COPD (1.8%), and sepsis (1.7%) |
| Polić-Vizintin (21) | 2005 | Croatia | At 1 yr, 12.2% of patients were rehospitalized with pneumonia. (Readmissions within 30 d were excluded, as these were believed to be nonresolution of the index pneumonia.) |
| Johnstone (24) | 2008 | Canada | Pneumonia-related readmissions occurred in 2.2% at 30 d, 9.2% at 1 yr, and 16% during the median 3.8 yr of follow-up. At study end, 72% of patients had been readmitted, and 69% had a pneumonia-unrelated readmission. Of the pneumonia-unrelated readmissions at 3.8 yr, the most common reasons were other respiratory diagnoses, circulatory disorders, digestive disorders, fall-related injuries, and cancer. |
| Jencks (12) | 2009 | United States | At 30 d, 20.1% of patients were readmitted. Pneumonia-related admissions occurred in 5.9%. The next most common reasons for readmissions were heart failure (1.5%), COPD (1.2%), and septicemia (0.7%). |
| Dharmarajan (13) | 2013 | United States | At 30 d, 18.3% of patients were readmitted. Pneumonia accounted for 4.1% of admissions. The next most common reasons for readmission were heart failure (1.6%), COPD/asthma (1.4%), sepsis (1.1%), renal disorders (1.0%), cardiorespiratory failure (0.8%), arrhythmias (0.5%), Clostridium difficile infection (0.5%), urinary tract infection (0.4%), gastrointestinal hemorrhage (0.4%), and stroke/TIA (0.4%). |
| HCUP (NIS, patients 18+ yr) (19) | 2009–2011 | United States | At 30 d, 18.1% of patients ≥ 65 yr and 16.8% of all adult patients ≥ 18 yr were readmitted for any cause. The rate of 30-d readmission for primary diagnosis of pneumonia was 3.2 and 3.0% in ≥ 65 yr and ≥ 18 yr, respectively. The rate of 30-d readmission for primary or secondary diagnosis of pneumonia was 7.5 and 7.0% in ≥ 65 yr and ≥ 18 yr, respectively. |
| Studies with chart review to determine of cause for readmission | |||
| Jasti (23) | 2008 | United States | At 30 d, 12.1% of patients were readmitted. Pneumonia-related admissions occurred in 2.5% and nonpneumonia readmissions in 9.0%; the remaining 0.6% were attributed to both pneumonia and other causes. Of the comorbidity-related readmissions, the most common reasons were cardiovascular (3.3%), pulmonary (1.0%), neurologic (1.0%), gastrointestinal (0.9%), genitourinary (0.9%), orthopedic (0.7%), and neoplastic (0.5%). |
| Capelastegui (25) | 2009 | Spain | At 30 d, 7.3% of patients were readmitted. 2.5% had pneumonia-related readmissions, 4.7% had pneumonia-unrelated readmissions. Of the pneumonia-unrelated readmissions, the most common reasons for readmission were cardiovascular (1.6%), pulmonary (1.1%), gastrointestinal (0.6%), orthopedic (0.2%), and neurologic (0.2%). |
| Adamuz (26) | 2011 | Spain | At 30 d, 8.7% of patients were readmitted. Pneumonia-related readmissions occurred in 3.4%, and pneumonia-unrelated readmissions in 3.7%. The remainder were attributed to both pneumonia and other causes. Of the nonpneumonia readmissions, the most common reasons were cardiovascular (1.5%), pulmonary (1.0%), neoplastic (0.6%), and infection (0.2%). |
| Aliberti (27) | 2011 | United States | At 30 d, 13.6% of patients were readmitted. Pneumonia-related readmissions occurred in 3.9% and pneumonia-unrelated readmissions in 9.7%. |
| Shorr (28) | 2013 | United States | At 30 d, 19.3% of patients were readmitted. Pneumonia readmission occurred in 1.4%. The most common reasons for readmission were COPD (4.8%) and CHF (4.4%). Infection (including pneumonia) occurred in 3.4%. |
Definition of abbreviations: CHF = congestive heart failure; COPD = chronic obstructive pulmonary disease; HCUP = Healthcare Cost and Utilization Project; NIS = Nationwide Inpatient Sample; TIA = transient ischemic attack.
For each percentage reported in this table, the denominator is patients discharged alive from the hospital.
Methodology of Included Studies
How were index hospitalizations for pneumonia identified?
Studies varied in their approach to identifying index hospitalizations (Table E2). Five used prospective clinical assessment (22–26), two used retrospective clinical assessment (27, 28), and five relied on administrative claims data (29–33). Studies using clinical assessment often required (1) a clinical presentation consistent with pneumonia, and (2) radiologic evidence of an infiltrate. Some studies specified the clinical symptoms necessary for diagnosis of pneumonia (24, 27).
Claims-based definitions drew on various administrative data, including International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) (13, 29), ICD-10 (31), and DRG codes (12, 30). All studies required a primary diagnosis code or DRG for pneumonia, with the exception of one study that also included hospitalizations with principal diagnoses of sepsis (038.0–038.9) or respiratory failure (518.21), with a secondary diagnosis of pneumonia (29).
How were the reasons for hospital readmission assessed?
Studies varied in their approach to defining the cause of readmission. Five studies used retrospective clinical assessment (23, 25–27), and seven studies used administrative data (12, 13, 29–31) (Table E3).
To define pneumonia as the cause of readmission, clinical assessment strategies required both (1) clinical symptoms of pneumonia, and (2) radiographic evidence of an infiltrate on admission. In the event of insufficient documentation to determine presence of an infiltrate, two studies accepted alternate criteria of hypoxia (26) or hypoxia and leukocytosis (23).
Studies using administrative claims relied on various data sources, including DRGs (12, 30), ICD-9-CM codes (24, 29), ICD-10 codes (24, 31), and Centers for Medicare & Medicaid Services condition categories (13). Most claims-based definitions required a principal diagnosis of pneumonia, but some studies accepted additional principal diagnoses, such as the DRG for “respiratory diagnosis with ventilator support” (475) (30) or the ICD-9-CM for sepsis (038.0–038.9) or respiratory failure (518.21) with a secondary diagnosis of pneumonia (29).
Studies used varying degrees of specificity to assign causes for readmission for diagnoses other than pneumonia, but followed two general approaches: (1) assigning a specific diagnosis (e.g., chronic obstructive pulmonary disease [COPD]) (12, 28, 30), or (2) assigning the general organ system (e.g., pulmonary) or broad clinical category (e.g., neoplastic) (23–26) (Table E4). Two studies fell toward the middle of this continuum and combined specific diagnoses into discrete categories with more specificity than the general organ system or clinical category approach (e.g., a category of asthma or COPD) (13, 22). No studies assessed whether readmissions were due to new comorbidities versus exacerbations of preexisting conditions.
Early Readmissions after a Hospitalization for Pneumonia
How often are patients readmitted within 30 days?
Eight studies assessed all-cause 30-day readmissions after pneumonia hospitalization, with rates ranging from 7.3 to 20.1% (12, 13, 23, 25–28, 30) across individual studies. In the NIS 2009 to 2011, 16.8% of adults 18 years or older and 18.1% of adults 65 years or older were readmitted for any cause within 30 days of hospital discharge. The pooled all-cause 30-day readmission was 11.6% in studies using chart review and 15.6% in the subset of U.S.-based studies.
Rates of all-cause 30-day readmission were generally higher in U.S.-based versus non–U.S.-based studies and in elderly populations (≥65 yr) versus general adult populations (≥18 yr). Studies using claims assessment tended to report higher rates of early readmission, although this is confounded by the fact all claims-based studies reporting all-cause 30-day readmission rates were U.S.-based studies of elderly populations. Comparing the 30-day readmission rate in the NIS 2009 to 2011 (16.8%) to the pooled estimate in U.S.-based chart review studies (15.6%) yields similar readmission rates.
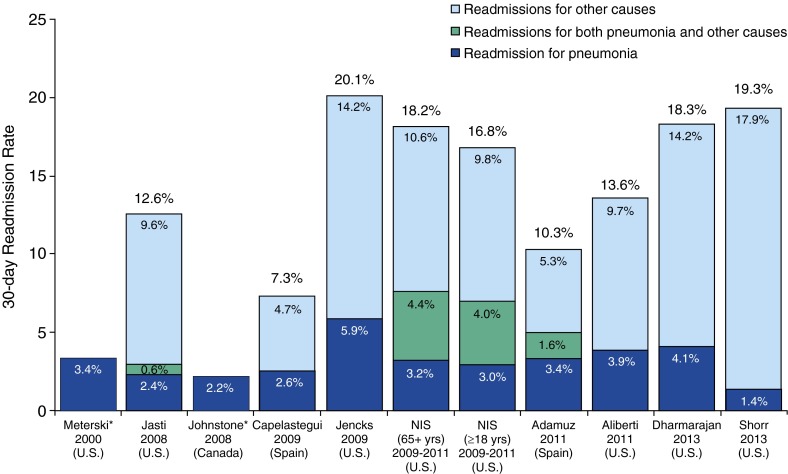
How often are early readmissions for pneumonia?
Nine studies assessed early readmissions for pneumonia, with rates ranging from 1.4 to 5.9% (12, 13, 23–29) across studies, or 7.3 to 39.1% of all 30-day readmissions (12, 13, 23, 25–28) (Figure 2). Within the NIS 2009 to 2011, rates of readmission for a primary diagnosis of pneumonia were 3.0% in adults 18 years or older and 3.2% in those 65 years or older, or 17.9 and 17.7% of total readmissions, respectively. The pooled estimate of 30-day readmissions for pneumonia across chart review studies was 2.7%, or 23.0% of the total readmissions.
Figure 2.
Percentage of patients readmitted within 30 days of discharge from pneumonia hospitalization. Studies with an asterisk did not report all-cause 30-day readmission rates. Readmissions attributed to pneumonia, to both pneumonia and other causes, and to other causes alone are represented in dark blue, green, and light blue bars, respectively. Study country is listed in parenthesis, below study author and publication year. NIS = Nationwide Inpatient Sample.
What are the leading causes of early readmission after pneumonia?
Six studies—two claims based and four chart review—assessed the rate of early readmissions for causes other than pneumonia (Table 3) (12, 13, 23, 25, 26, 28). The leading diagnoses of early readmission were pneumonia, heart failure/cardiovascular disease, and COPD/pulmonary disease. In both claims-based studies, the single most common reason for early readmission was pneumonia, followed by heart failure, then COPD with or without asthma (12, 13). In each of these studies, readmission for pneumonia (22.4–29.1% of total readmissions) was significantly more common than readmission for heart failure (7.4–8.7% of total readmissions) (12, 13).
Table 3.
The most common causes of hospital readmission by study
| Duration of Follow-up | 30 d | 6 mo | 12 mo | Median 3.8 yr | |||||
|---|---|---|---|---|---|---|---|---|---|
| Study Author (Reference) | Jasti (23) | Capelastegui (25) | Adamuz (26) | Shorr (28) | Jencks (12) | Dharmarajan (13) | Hedlund (22) | Bohannon (30) | Johnstone (24) |
| Readmission assessment | Chart review | Chart review | Chart review | Chart review | Claims assessment | Claims assessment | Claims assessment | Claims assessment | Claims assessment |
| Reasons for readmission | |||||||||
| Most frequent | Cardiovascular | Pneumonia | Pneumonia | COPD | Pneumonia | Pneumonia | Respiratory infection | Pneumonia | Respiratory |
| 2nd Most frequent | Pneumonia | Cardiovascular | Cardiovascular | Heart failure | Heart failure | Heart failure | Vascular | Heart failure | Pneumonia |
| 3rd Most frequent | Pulmonary | Pulmonary | Pulmonary | Infection | COPD | COPD/asthma | Malignancy | COPD | Circulatory |
| 4th Most frequent | Neurologic | Gastrointestinal | Neoplastic | Pneumonia | Sepsis | Sepsis | — | Sepsis | Digestive system |
Definition of abbreviation: COPD = chronic obstructive pulmonary disease.
The four studies using chart review each assessed a much small number of readmissions (range, 70–149; totaling 372 readmission across the four studies) and had discrepant findings regarding the most common reason for readmission; pneumonia was most common in two studies (25, 26), cardiovascular disease in one (23), and COPD in the fourth study (28). Pooling the results from these four studies, there were an equal number of readmissions for pneumonia (22.0% of total readmission) and for heart failure/cardiovascular disease (22.3% of total readmissions), followed by readmissions for COPD/pulmonary disease (16.9% of readmission).
The two claims-based studies found that readmissions for sepsis or septicemia (diagnosed by DRG [12, 30] or Centers for Medicare & Medicaid Services condition category [13] for septicemia) occur in 0.7 to 1.1% of survivors within 30 days (12, 13), representing the fourth most common cause of readmission in each of these studies. The studies using chart review did not assess specifically for readmissions due to sepsis.
Late Readmissions after a Hospitalization for Pneumonia
How common is readmission 31 days or more after pneumonia hospitalization?
No studies specifically assessed all-cause late readmissions separately from early readmissions. However, four studies assessed cumulative readmission rates at time periods beyond 30 days and found rates of 22 to 35.6% at 6 months (22, 30), 46% at 12 months (30), and 72% after a median 3.8 years of follow-up (24).
How common are late readmissions for pneumonia?
Three studies assessed readmissions for pneumonia at 1 year and determined that 9.2 to 17.2% of pneumonia survivors are readmitted for pneumonia in the year after discharge (24, 30, 31). One of these studies excluded early readmissions and found a 12.2% pneumonia-related readmission rate in the 31 to 365 days after hospital discharge, compared with 1.2% for the survivors of other hospitalizations (P < 0.001) (31). A fourth study, with a mean of 31 months’ follow-up, found that pneumonia survivors experienced pneumonia-related readmission at a rate of 8.1 per 100 person-years, compared with 1.2 per 100 person-years in patients surviving hospitalizations for alternate causes (22).
What are the leading diagnoses of late readmissions?
Three studies assessed readmission diagnoses beyond 30 days for diagnoses other than pneumonia (22, 24, 30). One study of nearly 900 patients found that readmission diagnoses at 1 year were very similar to those identified in the studies of early readmissions: pneumonia, heart failure, COPD, and sepsis were the most frequent primary diagnoses of readmission (30). A second, smaller study identified respiratory infection, vascular disease, and malignancy as the leading readmission diagnoses at 6 months (22). A third study found respiratory diseases, pneumonia, circulatory disorders, and digestive disorders to be the most common reasons for hospitalization during a median 3.8-year follow-up period.
How do the primary diagnoses of late readmissions compare with patients’ prior reasons for healthcare use?
No studies compared reasons for hospital readmission after pneumonia to patients’ baseline reasons for healthcare use.
Quality of the Included Studies
Characteristics of study design and quality are detailed in Table 4. All studies adequately reported inclusion and exclusion criteria. One study had an institution-specific sampling frame and no method to capture readmissions to other hospitals, suggesting the possibility for loss to follow-up. The rates and reasons for readmission reported in this study were not substantively different than the findings of other studies.
Table 4.
Quality assessment of included studies
| Author | Patients Included | No. of Readmissions Assessed | Sampling Frame | Identification and Classification of Index Hospitalization | Identification and Classification of Readmission | Includes All Readmissions |
|---|---|---|---|---|---|---|
| Hedlund (22) | 95 | 21 | Single hospital unit | Prospective clinical | Claims | Yes |
| Metersky (29) | 34,500 | >1,000 | Connecticut Medicare beneficiaries | Claims | Claims | Yes |
| Bohannon (30) | 892 | 150 | Single hospital | Claims | Claims | No |
| Polić-Vizintin (31) | 180 | <100 | 7 Hospitals | Claims | Claims | Yes |
| Jasti (23) | 577 | 70 | 7 Hospitals | Prospective clinical | Retrospective clinical | Yes |
| Johnstone (24) | 2,950 | 410 | 6 Hospitals | Prospective clinical | Claims | Yes |
| Capelastegui (25) | 1,117 | 81 | Single hospital | Prospective clinical | Retrospective clinical | Yes |
| Jencks (12) | — | >1,000 | All FFS Medicare beneficiaries | Claims | Claims | Yes |
| Adamuz (26) | 828 | 72 | Single hospital | Prospective clinical | Retrospective clinical | Yes |
| Aliberti (27) | 464 | 63 | Single hospital | Retrospective clinical | Retrospective clinical | Yes |
| Dharmarajan (13) | 1,168,624 | 214,239 | Elderly FFS Medicare beneficiaries | Claims | Claims | Yes |
| Shorr (28) | 771 | 149 | Single hospital | Retrospective clinical | Retrospective clinical | Yes |
| HCUP (NIS, patients 18+ yr in 2009–2011) (19) | 2,544,265 | 427,0041 | 20% Stratified sample of U.S. community hospitals | Claims | Claims | Yes |
Definition of abbreviations: FFS = fee for service; HCUP = Healthcare Cost and Utilization Project; NIS = Nationwide Inpatient Sample.
Discussion
Our study systematically reviews the literature on the primary diagnoses of hospital readmission after pneumonia. We compare findings across studies of disparate methodologies—large analyses of administrative claims and smaller studies in which the investigators reviewed charts to determine readmission diagnosis. We found that hospital readmission after pneumonia is common, particularly in the United States, where 12.1 to 20.1% of patients were readmitted within 30 days. The most frequent readmission diagnoses are pneumonia, heart failure/cardiovascular disease, and COPD/pulmonary disease. These top three diagnoses were consistent across claims-based and chart-review studies, general adult populations, and studies conducted in different countries. The consistency of findings between studies using chart review and administrative data suggests that administrative data provide useful information, despite concerns about decreased diagnostic sensitivity relative to chart review. Furthermore, administrative data may be the only feasible method to identify less common causes for readmission that are nonetheless important on a population scale.
The relative proportion of readmissions attributed to pneumonia versus heart failure or cardiovascular causes differed slightly between claims-based and chart review studies. However, this difference likely results from the fact that chart review studies tended to classify readmissions as being due to “cardiovascular” problems, whereas claims-based studies broke down cardiovascular readmissions into discrete categories of heart failure, arrhythmias, myocardial infarction, etc.
A few studies assessed readmissions for sepsis using ICD-9-CM codes for sepsis or septicemia and found it to be the fourth most common cause for readmission. However, explicit sepsis codes have poor sensitivity relative to other claims-based measurements of sepsis (32) and are likely to underestimate the true incidence of readmissions for this reason. Future studies should assess the proportion of readmissions due to infection and sepsis.
Few studies assessed readmission diagnoses beyond 30 days. Those that did indicate that pneumonia, cardiovascular disease, and pulmonary disease remain the most common diagnoses. No studies assessed whether leading causes of readmission were similar to patients’ reasons for healthcare use before index pneumonia admission.
As the Hospital Readmissions Reduction Program has drawn attention to the topic of hospital readmissions, many people have noted that 30-day readmissions often occur for diagnoses other than the index admission (12, 13, 23, 33). Our study affirms this finding: studies with differing patient populations, country of origin, and methodologies have consistently found that a majority of readmissions after pneumonia are not for pneumonia. However, this does not mean that they are completely unrelated.
No studies included in the review evaluated the extent to which the causes for hospital readmission reflect patients’ baseline comorbidities versus new problems. It is possible that pneumonia hospitalization contributes to a patient’s cardiovascular (or pulmonary) comorbidity burden—either by hastening the development of new cardiovascular disease or by worsening the severity or control of preexisting cardiovascular disease. Acute respiratory infections have been associated with increased rates of acute myocardial infarction (34–37), stroke (35), congestive heart failure (37), and cardiac arrhythmias (37) in the days to weeks after pneumonia diagnosis. The mechanisms underlying this relationship are unproven, and there are at least three plausible mechanisms. First, pneumonia may be associated with increased surveillance for and labeling of disease but not necessarily hasten the development or long-term progression of that comorbidity. Second, pneumonia might reduce patients’ physiologic reserve, leading to increased vulnerability and more rapid manifestations of existing comorbidities. Third, pneumonia may lead to increased inflammation, dysbiosis, hypercoagulability, immune dysregulation and other biologic impairments that accelerate the development and long-term progression of comorbidities.
Going forward, it will be important to understand the extent to which pneumonia or its treatment contributes causally to the most common causes of readmission—those for pneumonia, heart failure, COPD, and other infections.
There are several limitations to our study. The studies included in this this review would traditionally be considered of low to moderate quality because they are observational studies, often without a comparison group. However, as exposure to pneumonia cannot be randomly allocated, we depend on observational research to understand readmissions after pneumonia. One study sampled patients from a single hospital and had no mechanism to capture readmissions to other hospitals, but we did not identify systematic differences in the findings from this study. As with any systematic review, there is potential for bias in the included studies. To limit this possibility, we placed few limits in our initial search and instead excluded case reports, case series, nonoriginal research studies, and studies of pediatric populations during our selection process.
Conclusions
Although pneumonia is the leading early readmission diagnosis across studies, it explains only a minority of total readmissions. Congestive heart failure and COPD were the next most common early readmission diagnoses. And, in those studies that assessed for it, sepsis was the fourth most common readmission diagnosis. These findings were consistent across studies with differing populations and methodologies. The limited available data on readmissions beyond 30 days suggest that causes are similar to those of early readmission. Whether the reasons for readmission simply reflect patients’ preexisting comorbidities or are somehow altered by pneumonia remains unclear.
Acknowledgments
Acknowledgment
The authors thank Vineet Chopra, M.D., M.Sc., of University of Michigan for his thoughtful feedback on this manuscript.
Footnotes
Supported by grants T32 HL007749 (T.J.I.) from the National Institutes of Health and IIR 11–109 (H.C.P.) from the Department of Veterans Affairs Health Services Research and Development Service.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the U.S. government.
Author Contributions: H.C.P. designed the study, performed data analysis, and drafted the manuscript. M.W.S. performed data analysis and revised the manuscript critically for intellectual content. T.J.I. helped design the study and revised the manuscript critically for intellectual content.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Pfuntner A, Wier LM, Stocks C.Most Frequent Conditions in US Hospitals2010. HCUP Statistical Brief #148. January 2013. Agency for Healthcare Research and Quality, Rockville, MD [2014 Feb 1]. Available from: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb148.pdf
- 2.Center for Disease ControlPneumonia Fast Facts [updated 2013 June 6; accessed 2014 Feb 5]. Available from: http://www.cdc.gov/nchs/fastats/pneumonia.htm
- 3.Kaplan V, Clermont G, Griffin MF, Kasal J, Watson RS, Linde-Zwirble WT, Angus DC. Pneumonia: still the old man’s friend? Arch Intern Med. 2003;163:317–323. doi: 10.1001/archinte.163.3.317. [DOI] [PubMed] [Google Scholar]
- 4.Davydow DS, Hough CL, Levine DA, Langa KM, Iwashyna TJ. Functional disability, cognitive impairment, and depression after hospitalization for pneumonia. Am J Med. 2013;126:615–624.e5. doi: 10.1016/j.amjmed.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah FA, Pike F, Alvarez K, Angus D, Newman AB, Lopez O, Tate J, Kapur V, Wilsdon A, Krishnan JA, et al. Bidirectional relationship between cognitive function and pneumonia. Am J Respir Crit Care Med. 2013;188:586–592. doi: 10.1164/rccm.201212-2154OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Meara ES, White M, Siscovick DS, Lyles MF, Kuller LH. Hospitalization for pneumonia in the Cardiovascular Health Study: incidence, mortality, and influence on longer-term survival. J Am Geriatr Soc. 2005;53:1108–1116. doi: 10.1111/j.1532-5415.2005.53352.x. [DOI] [PubMed] [Google Scholar]
- 7.Waterer GW, Kessler LA, Wunderink RG. Medium-term survival after hospitalization with community-acquired pneumonia. Am J Respir Crit Care Med. 2004;169:910–914. doi: 10.1164/rccm.200310-1448OC. [DOI] [PubMed] [Google Scholar]
- 8.Prescott HC, Langa KM, Liu V, Escobar GJ, Iwashyna TJ. Increased 1-year healthcare use in survivors of severe sepsis. Am J Respir Crit Care Med. 2014;190:62–69. doi: 10.1164/rccm.201403-0471OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Readmissions Reduction Program[accessed 2014 Jan 9]. Available from: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html
- 10.The effect of medicare readmissions penalties on hospitals' efforts to reduce readmissions: perspectives from the field. 2013. Feb 26. The Commonwealth Fund Blog [accessed 2014 Feb 1]. Available from: http://www.commonwealthfund.org/Blog/2013/Feb/The-Effect-of-Medicare-Readmissions-Penalties-on-Hospitals.aspx
- 11.Medicare To Penalize 2,217 Hospitals For Excess Readmissions. Kaiser Health News. 2012. Aug 13 [accessed 2014 Feb 1]. Available from: http://www.kaiserhealthnews.org/stories/2012/august/13/medicare-hospitals-readmissions-penalties.aspx
- 12.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 13.Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, Barreto-Filho JA, Kim N, Bernheim SM, Suter LG, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aronsky D, Haug PJ, Lagor C, Dean NC. Accuracy of administrative data for identifying patients with pneumonia. Am J Med Qual. 2005;20:319–328. doi: 10.1177/1062860605280358. [DOI] [PubMed] [Google Scholar]
- 15.Lindenauer PK, Lagu T, Shieh MS, Pekow PS, Rothberg MB. Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003-2009. JAMA. 2012;307:1405–1413. doi: 10.1001/jama.2012.384. [DOI] [PubMed] [Google Scholar]
- 16.Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988-2002. JAMA. 2005;294:2712–2719. doi: 10.1001/jama.294.21.2712. [DOI] [PubMed] [Google Scholar]
- 17.Hebert PL, McBean AM, Kane RL. Explaining trends in hospitalizations for pneumonia and influenza in the elderly. Med Care Res Rev. 2005;62:560–582. doi: 10.1177/1077558705279310. [DOI] [PubMed] [Google Scholar]
- 18.Cyr L, Francis K. Measures of clinical agreement for nominal and categorical data: the kappa coefficient. Comput Biol Med. 1992;22:239–246. doi: 10.1016/0010-4825(92)90063-s. [DOI] [PubMed] [Google Scholar]
- 19.HCUPnet. Aquency for Healthcare Research and Quality. [accessed 2014 May 28]. Available from: http://hcupnet.ahrq.gov/HCUPnet.jsp?Id=D845DDB952F43F6B&Form=MAINSEL&JS=Y&Action=%3E%3ENext%3E%3E&_MAINSEL=Readmission Summary Tables
- 20.Statement STROBE2009[accessed 2013 Dec 19]. Available from: http://www.strobe-statement.org/index.php?id=strobe-home
- 21.Skull SA, Andrews RM, Byrnes GB, Campbell DA, Nolan TM, Brown GV, Kelly HA. ICD-10 codes are a valid tool for identification of pneumonia in hospitalized patients aged > or = 65 years. Epidemiol Infect. 2008;136:232–240. doi: 10.1017/S0950268807008564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hedlund J. Community-acquired pneumonia requiring hospitalisation. Factors of importance for the short-and long term prognosis. Scand J Infect Dis Suppl. 1995;97:1–60. [PubMed] [Google Scholar]
- 23.Jasti H, Mortensen EM, Obrosky DS, Kapoor WN, Fine MJ. Causes and risk factors for rehospitalization of patients hospitalized with community-acquired pneumonia. Clin Infect Dis. 2008;46:550–556. doi: 10.1086/526526. [DOI] [PubMed] [Google Scholar]
- 24.Johnstone J, Eurich DT, Majumdar SR, Jin Y, Marrie TJ. Long-term morbidity and mortality after hospitalization with community-acquired pneumonia: a population-based cohort study. Medicine (Baltimore) 2008;87:329–334. doi: 10.1097/MD.0b013e318190f444. [DOI] [PubMed] [Google Scholar]
- 25.Capelastegui A, España Yandiola PP, Quintana JM, Bilbao A, Diez R, Pascual S, Pulido E, Egurrola M. Predictors of short-term rehospitalization following discharge of patients hospitalized with community-acquired pneumonia. Chest. 2009;136:1079–1085. doi: 10.1378/chest.08-2950. [DOI] [PubMed] [Google Scholar]
- 26.Adamuz J, Viasus D, Campreciós-Rodríguez P, Cañavate-Jurado O, Jiménez-Martínez E, Isla P, García-Vidal C, Carratalà J. A prospective cohort study of healthcare visits and rehospitalizations after discharge of patients with community-acquired pneumonia. Respirology. 2011;16:1119–1126. doi: 10.1111/j.1440-1843.2011.02017.x. [DOI] [PubMed] [Google Scholar]
- 27.Aliberti S, Peyrani P, Filardo G, Mirsaeidi M, Amir A, Blasi F, Ramirez JA. Association between time to clinical stability and outcomes after discharge in hospitalized patients with community-acquired pneumonia. Chest. 2011;140:482–488. doi: 10.1378/chest.10-2895. [DOI] [PubMed] [Google Scholar]
- 28.Shorr AF, Zilberberg MD, Reichley R, Kan J, Hoban A, Hoffman J, Micek ST, Kollef MH. Readmission following hospitalization for pneumonia: the impact of pneumonia type and its implication for hospitals. Clin Infect Dis. 2013;57:362–367. doi: 10.1093/cid/cit254. [DOI] [PubMed] [Google Scholar]
- 29.Metersky ML, Tate JP, Fine MJ, Petrillo MK, Meehan TP. Temporal trends in outcomes of older patients with pneumonia. Arch Intern Med. 2000;160:3385–3391. doi: 10.1001/archinte.160.22.3385. [DOI] [PubMed] [Google Scholar]
- 30.Bohannon RW, Maljanian RD. Hospital readmissions of elderly patients hospitalized with pneumonia. Conn Med. 2003;67:599–603. [PubMed] [Google Scholar]
- 31.Polić-Vizintin M, Leppée M, Stimac D, Vodopija I, Cindrić J. Risk of pneumonia recurrence in patients previously hospitalized for pneumonia—a retrospective study (1998-2000) Coll Antropol. 2005;29:213–219. [PubMed] [Google Scholar]
- 32.Iwashyna TJ, Odden A, Rohde J, Bonham C, Kuhn L, Malani P, Chen L, Flanders S. Identifying patients with severe sepsis using administrative claims: patient-level validation of the Angus Implementation of the International Consensus Conference definition of severe sepsis. Med Care. 2014;52:e39–e43. doi: 10.1097/MLR.0b013e318268ac86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Krumholz HM. Post-hospital syndrome—an acquired, transient condition of generalized risk. N Engl J Med. 2013;368:100–102. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meier CR, Jick SS, Derby LE, Vasilakis C, Jick H. Acute respiratory-tract infections and risk of first-time acute myocardial infarction. Lancet. 1998;351:1467–1471. doi: 10.1016/s0140-6736(97)11084-4. [DOI] [PubMed] [Google Scholar]
- 35.Smeeth L, Thomas SL, Hall AJ, Hubbard R, Farrington P, Vallance P. Risk of myocardial infarction and stroke after acute infection or vaccination. N Engl J Med. 2004;351:2611–2618. doi: 10.1056/NEJMoa041747. [DOI] [PubMed] [Google Scholar]
- 36.Clayton TC, Thompson M, Meade TW. Recent respiratory infection and risk of cardiovascular disease: case-control study through a general practice database. Eur Heart J. 2008;29:96–103. doi: 10.1093/eurheartj/ehm516. [DOI] [PubMed] [Google Scholar]
- 37.Perry TW, Pugh MJ, Waterer GW, Nakashima B, Orihuela CJ, Copeland LA, Restrepo MI, Anzueto A, Mortensen EM. Incidence of cardiovascular events after hospital admission for pneumonia. Am J Med. 2011;124:244–251. doi: 10.1016/j.amjmed.2010.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]