Abstract
Objective
This study examined whether individual differences in loneliness and/or daily exacerbations in loneliness relate to daily pain and frequency and perception of interpersonal events among individuals with fibromyalgia (FM).
Methods
118 participants with FM completed electronic diaries each evening for 21 days to assess the occurrence of positive and negative interpersonal events, event appraisals, and pain. Multilevel modeling was used to examine relations of chronic and transitory loneliness to daily life outcomes, controlling for daily depressive symptoms.
Results
Chronic and transitory loneliness were associated with more frequent reports of negative and less frequent reports of positive interpersonal daily events, higher daily stress ratings and lower daily enjoyment ratings, and higher daily pain levels. Neither chronic nor transitory loneliness moderated the relations between daily negative events and either stress appraisals or pain. However, both chronic and transitory loneliness moderated the relation between daily positive events and enjoyment appraisals. Specifically, on days of greater numbers of positive events than usual, lonely people had larger boosts in enjoyment than did nonlonely people. Similarly, days with greater than usual numbers of positive events were related to larger boosts in enjoyment if an individual was also experiencing higher than usual loneliness levels.
Conclusions
Chronic and transient episodes of loneliness are associated with more negative daily social relations and pain. However, boosts in positive events yield greater boosts in day-to-day enjoyment of social relations for lonely versus nonlonely individuals, and during loneliness episodes, a finding that can inform future interventions for individuals with chronic pain.
Keywords: loneliness, pain, stress, enjoyment
Individuals who are isolated from others are at risk for poorer health (Shankar, McMunn, Banks, & Steptoe, 2011). Objective markers of social isolation have included small social network size, reports of little social contact, and living alone. Independent of objective social isolation, individuals may also have a subjective experience of social isolation and disconnection, or loneliness. Loneliness is the feeling that one is isolated from the interpersonal intimacy and relationships one desires (Cacioppo et al., 2002; Peplau & Perlman, 2000; Shankar et al., 2011). Measures of objective social isolation and loneliness are only weakly related (Shankar et al., 2011). Indeed, loneliness ratings are only modestly related to indicators of social network size and frequency of interaction with network members (Hawkley, Masi, Berry, & Cacioppo, 2006), and only share approximately 50% of the variance with ratings of availability of support from the social network (e.g., Cacioppo, Hughes, Waite, Hawkley, & Thisted, 2006). Thus, the extant data indicate that loneliness represents the subjective, emotional experience of being socially isolated, distinct from objective markers of social isolation and lack of social support.
Similar to objective social isolation, loneliness has been linked with risk for poor health. The bulk of research in this area has examined whether longstanding feelings of loneliness are a risk factor for health problems. Chronic loneliness has been linked with negative consequences for psychological health, including increased risk for depression, and for physical health, including increased stress-related inflammation, sleep disturbance, poorer immune functioning, and elevated cardiovascular risk (Cacioppo, Hawkley, & Thisted, 2010; Jaremka et al., 2013; Hawkley & Cacioppo, 2007; Hawkley & Cacioppo, 2010). Further, chronic loneliness significantly predicts subsequent physical and emotional health, even when accounting for depression and social support (Cacioppo et al., 2010; Cacioppo et al., 2006).
Although loneliness has trait-like elements, it can also be a transitory experience with links to markers of daily functioning. For example, day-to-day and within-day fluctuations in loneliness have been related to deleterious changes in the stress response, especially under conditions of high interpersonal stress (Adam, Hawkley, Kudielka, & Cacioppo, 2006; Doane & Adam, 2010). In both young and older adults, higher feelings of loneliness on one day were associated with an increased cortisol awakening response on the following morning, a hormonal response pattern linked to elevated stress (Doane & Adam, 2010, Adam et al., 2006). Individuals with high versus low chronic interpersonal stress were especially vulnerable to the negative effects of episodes of loneliness, showing greater loneliness-induced increases in cortisol (Doane & Adam, 2010). Beyond its physiological effects, one day’s increase in loneliness has been associated with increases in the next day’s symptoms, including exhaustion and fatigue, over and above the influence of the prior day’s depressed affect and sleep duration (Hawkley, Preacher, & Cacioppo, 2010). Taken together, the available evidence indicates that both chronic loneliness and daily fluctuations in loneliness predict emotional and physical health.
The majority of investigations of loneliness and its repercussions have examined the impact of loneliness in physically healthy individuals. However, a small but growing body of evidence has linked loneliness to the experience of bodily pain, one of the most common and costly medical problems in the United States (Gaskin & Richard, 2012). Among breast cancer survivors, for example, chronic loneliness is associated with higher levels of pain, depression, and fatigue (Jaremka et al., 2012). Similarly, older adults with chronic pain report being significantly more lonely than do those without pain (Jacobs, Hammerman-Rozenberg, Cohen, & Stessman, 2006; Tse, Leung, & Ho, 2012). Moreover, loneliness predicts more than a four-fold increase in the prevalence of chronic pain among elderly individuals over time (Jacobs et al., 2006). Some intriguing evidence also points to a potential link between state loneliness and pain. In fact, episodes of physical pain and the perceived social exclusion that characterizes loneliness activate common brain circuits (Cacioppo, Norris, Decety, Monteleone, & Nusbaum, 2008), indicating that there may be a “pain signature” in the central nervous system that is activated by both physical and social stimuli (Eisenberger, Lieberman, & Williams, 2003; Wager et al., 2013). To the extent that loneliness shares common underlying neurophysiological circuitry with physical pain, acute increases in loneliness may increase vulnerability to physical pain (Eisenberger & Lieberman, 2004).
Given the links between chronic and state loneliness and pain, the experience of loneliness may have implications for adaptation among individuals managing a chronic pain condition. How might loneliness impact their adaptation? One possibility is through its impact on appraisals of social interactions. Lonely people have more negative perceptions of the quality of social interactions in their daily lives compared to their nonlonely counterparts, which seems to perpetuate a cycle of social disconnection (Hawkley, Preacher, & Cacioppo, 2007). Such social withdrawal may both increase their experience of interpersonal stress and limit their capacity to draw on positive social engagement, an important resource to sustain quality of life among people with chronic pain (Finan et al., 2010; Potter, Zautra, & Reich, 2000; Skinner, Zautra, & Reich, 2004). Thus, among individuals with chronic pain, loneliness may impair the capacity to effectively limit negative social contacts and draw on positive social resources to sustain healthy functioning. Because much of the work tying loneliness and health has focused on the impact of chronic elevations in loneliness, the impact of short-term, day-to-day fluctuations in loneliness on the physical and emotional health of those with chronic pain is largely unknown.
To address this gap in the literature, the current study drew on daily diary reports of individuals living with fibromyalgia (FM) to examine the links between loneliness, interpersonal experiences, and pain. FM is a prevalent condition that is characterized by widespread pain and fatigue of unknown origin (Wolfe et al., 1990). Co-morbid mood disturbance is common; anxiety and mood disorders have been reported by as many as 75% of individuals with FM (Thieme, Turk, & Flor, 2004). Moreover, persons with FM show deficits in positive affect (Finan, Zautra, & Davis, 2009) and report poor quality social ties (Schoofs, Bambini, Ronning, Bielak, & Woehl, 2004). Especially relevant for the current work, individuals with FM often feel alienated and isolated because the credibility of their illness as well as their personal integrity are often called into question by others (Åsbring & Närvänen, 2002). Those who experience that social isolation due to their FM report withdrawing from social situations as a strategy to avoid potential stressors (Åsbring & Närvänen, 2002).
The current study examined whether chronic levels of loneliness and/or daily fluctuations in loneliness among individuals with FM relate to 1) exposure to positive and negative interpersonal events, and 2) responses to day-to-day changes in interpersonal events in terms of event appraisals and pain. In line with the limited extant evidence, it was expected that elevated chronic and state loneliness would both be associated with higher pain levels, a more deleterious social milieu, and more maladaptive responses to interpersonal events, and that these effects would be evident even when accounting for daily depressive symptoms.
Methods
Participants
Individuals with chronic widespread pain were recruited from the Phoenix metropolitan area using newspaper advertisements, online postings, and flyers distributed in physician offices to participate in an ongoing randomized trial of behavioral treatments for FM. To maximize generalizability of study findings to individuals with FM, exclusionary criteria were minimized. To that end, individuals were eligible for participation if they: (1) were between the ages of 18 and 72 years; (2) lived in the Phoenix metro area for the duration of the study; (3) reported that they had pain for three months or more in at least three of four quadrants of the body, or in two quadrants of the body and experienced substantial sleep disturbance and fatigue; (4) reported pain in at least 11 of 18 tender points during a tender point exam (described below), consistent with diagnostic criteria for FM established by the American College of Rheumatology (Wolfe et al., 1990); (5) were free from autoimmune pain disorders; (6) were not currently enrolled in other research trials or receiving psychotherapy; (7) were not pursuing litigation related to their pain condition; and (8) were capable of participating in the questionnaire, laboratory, diary assessments, and group-based treatments related to the project.
One hundred and sixty individuals were screened by phone and through an in-person nurse visit to determine eligibility, and 6 were deemed ineligible because they did not meet criteria for widespread pain. Of the 154 who were enrolled, 36 dropped prior to the diary portion of the study, primarily due to their competing obligations and time constraints. The sample for the current study is comprised of the first 118 individuals who were enrolled in the study and completed the 21 daily diaries that preceded the intervention (described below).
Procedure
All procedures were approved by Institutional Review Board at Arizona State University. Interested individuals were initially screened by phone regarding their age, pain and fatigue levels, co-morbid autoimmune disorders, and involvement in other research protocols, psychotherapy, and litigation. Individuals who passed initial screening received a home visit from a registered nurse, who consented them and administered a tender point exam using a dolorimeter that delivered 4 kg of pressure to each of 18 tender points and 3 control points (Wolfe et al., 1990). To qualify for study enrollment, participants had to report experiencing pain in response to pressure on at least 11 of 18 tender points.
After eligible participants were enrolled in the study, they completed an initial questionnaire packet that included questions regarding demographics and personality attributes. As part of the pre-intervention evaluation, participants were subsequently interviewed by phone regarding depressive and anxiety symptoms and exposure to traumatic life events. They also completed assessments that included: (1) a laboratory assessment of physiological and affective responses to pain and emotion stimuli; (2) 21 days of electronic diary reports regarding interpersonal events, loneliness, pain, sleep quality, mood, and coping; and (3) questionnaires regarding current physical symptoms and physical and emotional functioning. Participants were then randomly assigned to one of three 7-week treatment conditions. Following completion of treatment, they underwent post-intervention assessments identical to those in pre-assessment, and completed six- and twelve-month follow-up questionnaires.
The current study is based on data from the pre-intervention evening diaries. To initiate the pre-intervention diary assessment, a member of the research team met with participants to provide them with a cell phone and detailed instructions and training on how to complete the phone diaries. Participants were prompted to complete diary reports four times per day for up to 21 days via an automated system that called the cell phone, delivered audio-recorded questions, and collected responses via phone keypad input from participants. The morning call time occurred 30 minutes after usual wake time, and the remaining calls occurred at 11:00 am, 3:30 pm, and 7:00 pm. If participants missed a call, they could call into the system within three hours of the automated call to complete the questions. Call completions were monitored by study staff members, who routinely checked in with each participant on his/her progress. If participants missed several calls, they were contacted immediately by study staff members to remedy any potential barriers to consistent completion. Participants were paid $2 for each day of completed diaries, with a bonus of $1/day when they completed at least 50% of the diaries.
The current study drew on data from the 7:00 pm calls, because they included an extensive assessment of participants’ interpersonal events and appraisals. The mean number of evening diaries completed by participants was 16.89 of 21 possible days (Range = 1 to 23, SD = 5.20). [Six participants completed one to two diaries beyond the 21 days outlined in the study protocol because of errors within the automated dialing system. Because these errors occurred by chance and accounted for few extra days in the data set (i.e., 6 days in the sample of 1782 diary days for the total sample), the extra days of diary reports were retained for analyses.]
Measures
Pre-intervention depressive symptoms and functional health
The 9-item short form version of the Hamilton Depression Inventory (HDI; Reynolds & Kobak, 1995) was used as a one-time assessment of depressive symptoms. The HDI assesses standard depression symptoms over the last two weeks with higher scores reflecting higher depression levels. The HDI has demonstrated high levels of reliability and validity across depression studies (Reynolds & Kobak, 1995). Cronbach’s alpha of the HDI in the current sample was .89.
The 10-item Fibromyalgia Impact Questionnaire (FIQ; Bennett, 2005) assessed impairment in physical functioning, psychological functioning, sleep, and well-being due to FM. Higher scores reflect greater impairment. The FIQ has been shown to be a highly valid and reliable measure of FM impairment (Bennett, 2005). FIQ scores in the current sample showed high internal consistency, with a Cronbach’s alpha of .91.
Pain
Daily pain was measured on a 101-point numerical rating scale (Jensen, Karoly, & Braver, 1986) Participants were asked, “What was your overall level of pain today? Enter a number between 0 and 100 that best describes your pain level. A zero would mean ‘no pain’ and a one hundred (100) would mean ‘pain as bad as it can be.’” Fifty-nine percent of the variance in pain scores was between-person and 41% of the variance was within-person in the current sample.
Loneliness
Daily loneliness was assessed via a face-valid item asking the extent to which an individual felt lonely that day with the question, “Were you lonely?” (Watson & Clark, 1994). Scores were rated on a 5-point scale from 1 (not at all) to 5 (completely). End of day loneliness was significantly correlated with the 11 am and 4 pm loneliness ratings taken the same day (rs>.65, ps<.001), indicating consistency of scores across the day. Fifty-four percent of the variance in lonely scores was between-person and 46% of the variance was within-person in the current sample. Daily loneliness scores were disaggregated to create indicators of chronic loneliness and episodes of loneliness (described in the Data Analysis section below).
Occurrence of interpersonal events
Daily interpersonal events were measured using items from the Inventory of Small Life Events (ISLE) for older adults (Zautra, Schultz, & Reich, 2000). The ISLE items assessed positive and negative daily events occurring within three relationship domains: spouse, family, and friends/acquaintances. In the current study, four items involving interpersonal rejection by the spouse were included together with the original items. Thus, for the spouse domain, participants were asked if 6 desirable and 8 undesirable events occurred with their spouse across the day. Examples of positive events include “You celebrated with your spouse or partner,” and examples of negative events include “Your spouse or partner was critical or angry with you.” Family events included 10 desirable and 5 undesirable events, and friend events included 6 desirable and 5 undesirable events. Counts of total undesirable and desirable events across interpersonal domains were generated for each participant. Although referred to as a reflection of the frequency of daily events, the ISLE scores represent the number of diverse positive and negative events that occurred each day.
Non-partnered participants were not administered partner-related event items; thus, partnered individuals could accrue 22 total positive and 18 negative events whereas unpartnered participants could accrue 16 total positive events and 10 negative events. Because all event counts were centered within person for the primary analyses (described below), each individual’s event scores represented deviations above and below his/her own average number of interpersonal events.
Appraisal of interpersonal events
After each set of questions about desirable events with a spouse, family, or friends and acquaintances, participants were asked how enjoyable their relations were that day within each domain on a scale ranging from 1 (not at all) to 5 (completely). Similarly, after each set of questions about undesirable events with a spouse, family, or friends and acquaintances, participants were asked how stressful their relations were that day within each group using the same response scale. Because spouse, family, and friend appraisals were significantly correlated (rs .26-.47, ps<.05), appraisals across domains within a day were averaged to create separate daily stress and enjoyment scores. Spouse, family, and friend appraisals showed modest internal reliability (Cronbach’s alphas = .59 and .68 for stress and enjoyment, respectively). In the current sample, 64% of the variance was within-person for stress, whereas 50% of the variance was within-person for enjoyment.
Depressive symptoms
Daily depressive symptoms levels were measured with five items drawn from the Patient Health Questionnaire (Kroenke & Spitzer, 2002), modified to refer to that day. Items were rated on a 3-point scale from 1 (no) to 3 (yes, very much). Items included: “Did you feel… a lack of interest in your activities; down on yourself; restless or slowed down; an increase or decrease in appetite; difficulty concentrating or making decisions?” A mean of these items was computed to create a depressive symptom score for each day. Fifty-five of the variance in depression scores was within-person.
Data Analysis
The current study had two levels of data consisting of days (Level 1 or within-person) nested within individuals (Level 2 or between-person). To disaggregate the between- from the within-person variation included in the end-of-day reports, daily study variables were centered within-person. Specifically, each participant’s mean score over all days of assessment was subtracted from his/her daily score (i.e., person-centered). Thus, each centered score signifies each day’s deviations from an individual’s mean across all days of assessment (i.e., Level 1 variable), whereas the mean score reflects a between-person measure (i.e., Level 2 variable). The intercept was also centered within the sample by subtracting the sample’s average on the same variable from each participant’s average score on that variable (i.e., grand mean-centered). With regard to loneliness, centered loneliness reflects the Level 1 day-to-day deviations from an individual’s average loneliness score (i.e., “when” someone feels lonely), whereas mean loneliness across the 21 days represents the Level 2 variable of chronic loneliness (i.e., someone “who” feels lonely). Level 1 person-centered scores are uncorrelated with Level 2 scores on the same variable, facilitating interpretation of effects (Enders & Tofighi, 2007).
Multi-level random effects modeling was employed to examine relations among variables, a method that can control for the correlation between observations from consecutive days (i.e., autocorrelation) and account for missing data. Level 1 predictors were included as random effects when doing so improved the fit of the models. All analyses were completed using the SAS 9.2 PROC MIXED statistical package (Littell, Milliken, Stroup, & Wolfinger, 1996). Models evaluated whether chronic loneliness and/or episodes of loneliness 1) related to daily pain, interpersonal events, and event appraisals, and 2) moderated the relations between negative interpersonal events and pain and stress appraisals, and between positive interpersonal events and enjoyment appraisals. Moderating effects of loneliness are reflected in significant interactions between loneliness terms (i.e., chronic loneliness and transitory loneliness) and daily fluctuations in negative or positive events (i.e., centered negative events and centered positive events). Raw daily depressive symptom scores (containing both Level 1 and Level 2 variation) were included as a control variable in all analyses. Demographic variables, including age and marital status, were tested as covariates in all models but were unrelated to outcomes and did not change the main findings and so were not included in final, moderated models.
Results
Sample Characteristics and Descriptive Analyses
The mean age of participants was 52 years (SD = 11.30). Most participants were female (84.7%), married (54%), Caucasian (75.6%), and employed (55.3%), and approximately one-third had attended 1–3 years of college (32.5%). The modal annual family household income of participants was between $30,000 and $49,999. At pre-intervention, the mean HDI depression score of the sample was 11.3 (SD= 5.7; range 1–27), which falls in a range indicating mild depression. The mean FIQ functional health score of the sample was 52.44 (SD = 16.24; range 8–80), reflecting substantial functional impairment in the sample due to FM. Depression and FIQ scores in the current sample were similar to those reported in other samples of individuals with FM (Arnold et al., 2004; Bennett, 2005; Davis & Zautra, 2013). Participants also frequently reported living with other medical conditions, the most common of which were headaches (64%), chronic fatigue syndrome (33%), stomach ulcers or disease (33%), irritable bowl syndrome (31%), endocrine/thyroid dysfunction (32%), and high blood pressure or heart disease (19%).
Means, standard deviations, ranges, and intercorrelations among study variables are presented in Table 1 for between-person variables and in Table 2 for within-person variables. Skewness and kurtosis of study variables indicated that they were normally distributed (i.e., skewness less than 2 and kurtosis less than 4). In general, chronic loneliness was characterized by reports of fewer positive interpersonal events and more negative interpersonal events; less interpersonal enjoyment and more perceived interpersonal stress; higher pain and depressive symptoms; younger age; and being unmarried/unpartnered. Chronic loneliness was unrelated to the overall mean number of interpersonal events across 21 days. Similarly, days of elevated loneliness were characterized by fewer positive interpersonal events and more negative interpersonal events; lower levels of interpersonal enjoyment and higher levels of perceived interpersonal stress; and higher pain and depressive symptoms levels than usual for an individual. Thus, both chronic and transitory loneliness were related to less frequent and rewarding positive interpersonal engagement and more frequent and aversive negative interpersonal engagement, as well as higher pain and depressive symptom levels.
Table 1.
Descriptive Statistics and Intercorrelations of Between-person Variables Across All Days (N= 118)
| Measures | M (SD) | Observed Range | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Chronic Loneliness | 1.77 (.89) | 1–5 | - | ||||||||||
| 2. Daily Pain | 52.13 (19.87) | 6–90 | .35*** | - | |||||||||
| 3. Daily Negative Events | 1.25 (1.19) | 0–6 | .26** | .09 | - | ||||||||
| 4. Daily Positive Events | 3.35 (1.80) | 0–9 | −.22* | −.13 | .04 | - | |||||||
| 5. Total Events | 4.60 (2.21) | 0–10 | −.04 | −.06 | .58*** | .84*** | - | ||||||
| 6. Interpersonal Stress | 1.80 (.61) | 1–3 | .49*** | .32*** | .72*** | −.27** | .17 | - | |||||
| 7. Interpersonal Enjoyment | 3.63 (.79) | 2–5 | −.35*** | −.31** | −.43*** | .43*** | .12 | −.67*** | - | ||||
| 8. Age | 52.03 (11.34) | 19–72 | −.27** | −.10 | −.17 | .09 | −.02 | −.11 | .23* | - | |||
| 9. Employed | .53 (.50) | 0–1 | .09 | −.20* | .05 | −.00 | .02 | .01 | .04 | .01 | - | ||
| 10. Married/Partnered | .61 (.49) | 0–1 | −.22* | −.02 | .19* | .50*** | .51*** | −.13 | .21* | .00 | −.11 | - | |
| 11. Depressive symptoms | 1.82 (.37) | 1–3 | .60*** | .38*** | .27** | .03 | .17 | .39*** | −.28** | −.32** | −.14 | .10 | - |
p < .05;
p < .01;
p < .001
Table 2.
Intercorrelations of Daily Variables Centered Within-person
| Measures | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. ΔLoneliness | - | ||||||
| 2. ΔDaily Pain | .10*** | - | |||||
| 3. ΔDaily Negative Events | .11*** | .06* | - | ||||
| 4. ΔDaily Positive Events | −.11*** | .00 | .02 | - | |||
| 5. ΔInterpersonal Stress | .12*** | .09*** | .49*** | −.06* | - | ||
| 6. ΔInterpersonal Enjoyment | −.20*** | −.10*** | −.26*** | .33*** | −.31*** | - | |
| 7. ΔDepressive symptoms | .26*** | .24*** | .10*** | −.18*** | .13*** | −.20*** | - |
Note: Δ reflects person-centered score.
p < .05;
p < .01;
p < .001.
The sample size for correlations ranges from 1782 to 6014.
Loneliness as a Moderator of Responses to Daily Negative Interpersonal Events
The next set of models tested whether days of increased negative interpersonal events were more strongly related to increases in perceived stress and pain for more versus less lonely people and during lonely episodes. Models included chronic and transitory loneliness, centered negative events, interactions between each loneliness term and negative events, and daily depressive symptom scores as a covariate. Results for hypothesized models are depicted in Table 3.
Table 3.
Models Including Loneliness, Person-centered Interpersonal Events, and Their Interactions Predicting Daily Outcomes
| Dependent Variable | B(SE) | df | p-value |
|---|---|---|---|
| Pain | |||
|
| |||
| Level 1 | |||
| ΔLoneliness | .92 (.53) | 1659 | .08 |
| ΔDaily Negative Events | .21 (.37) | 1659 | .57 |
| ΔLoneliness X ΔNegative Events | .33 (.31) | 1659 | .28 |
| Chronic Loneliness X ΔNegative Events | −.28 (.45) | 1659 | .54 |
| Depressive Symptoms | 8.98 (.96) | 1659 | <.0001 |
| Level 2 | |||
| Chronic Loneliness | 5.53 (1.97) | 116 | <.01 |
|
| |||
| Interpersonal Stress | |||
|
| |||
| Level 1 | |||
| ΔLoneliness | .06 (.03) | 1659 | .06 |
| ΔDaily Negative Events | .26 (.02) | 1659 | <.0001 |
| ΔLoneliness X ΔNegative Events | .01 (.01) | 1659 | .40 |
| Chronic Loneliness X ΔNegative Events | .01 (.02) | 1659 | .68 |
| Depressive Symptoms | .15 (.04) | 1659 | <.001 |
| Level 2 | |||
| Chronic Loneliness | .31 (.06) | 116 | <.0001 |
|
| |||
| Interpersonal Enjoyment | |||
|
| |||
| Level 1 | |||
| ΔLoneliness | −.13 (.03) | 1659 | <.0001 |
| ΔDaily Positive Events | .12 (.01) | 1659 | <.0001 |
| ΔLoneliness X ΔPositive Events | .03 (.01) | 1659 | <.05 |
| Chronic Loneliness X ΔPositive Events | .04 (.01) | 1659 | <.01 |
| Depressive Symptoms | −.24 (.04) | 1659 | <.0001 |
| Level 2 | |||
| Chronic Loneliness | −.25 (.08) | 116 | <.01 |
|
| |||
Note. Δdenotes person-centered variable. Chronic loneliness scores are sample-centered.
As expected, episodes of negative events were related to elevations in perceived stress. Higher chronic loneliness was significantly related to elevations in pain and stress and episodic loneliness was marginally related to elevations. Contrary to hypotheses, neither chronic nor transitory loneliness moderated the associations between negative interpersonal events and either pain or stress.
Loneliness as a Moderator of Responses to Daily Positive Interpersonal Events
Next, data were examined to test whether days of increased positive interpersonal events were less strongly related to increases in perceived interpersonal enjoyment for more versus less lonely people and during lonely episodes. Models included chronic and transitory loneliness, centered positive interpersonal events, interactions between each loneliness term and positive events, and depressive symptoms scores as a covariate, and results are depicted in Table 3.
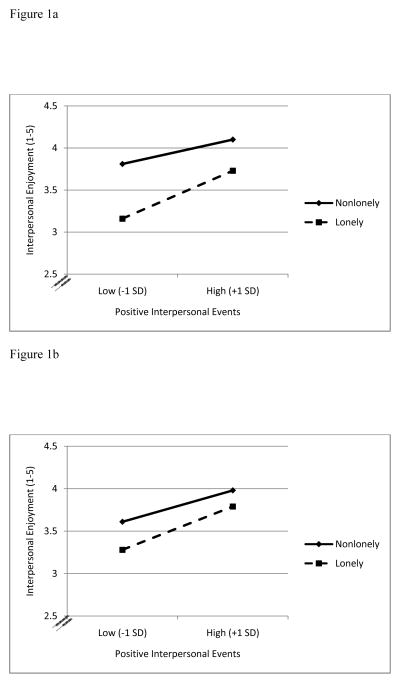
As expected, positive interpersonal events were associated with more perceived interpersonal enjoyment, and higher chronic loneliness levels, episodes of loneliness, and depressive symptoms were all associated with less enjoyment. Moreover, both chronic loneliness levels and episodes of loneliness significantly moderated the relation between episodes of positive interpersonal events and enjoyment. The relations between each loneliness term, positive events, and enjoyment are depicted in Figure 1a for chronic loneliness and Figure 1b for episodic loneliness. The figures show that the results were opposite of hypothesized models. That is, days with higher than average positive events brought a greater boost in enjoyment both for people who were more versus less lonely, and during episodes of higher versus lower loneliness.
Figure 1.
Figure 1a. Chronic Loneliness Predicting Daily Interpersonal Enjoyment at Different Values of Person-centered Positive Events
Figure 1b. Episodes of Loneliness Predicting Daily Interpersonal Enjoyment at Different Values of Person-centered Positive Events
Discussion
Loneliness has been identified as a meaningful indicator of psychological and physical outcomes in recent years (Cacioppo, Hawkley et al., 2006; Hawkley, Thisted, & Cacioppo, 2009; MacDonald & Leary, 2005). The current study focused on examining how both chronic and transitory loneliness dimensions related to the daily pain and interpersonal experiences of individuals with chronic widespread pain, to begin to elaborate the processes by which loneliness affects health longer term. Findings revealed that the relations of loneliness with daily pain and stress are distinct from its relation with interpersonal enjoyment. Specifically, both chronic and transitory loneliness were related to increases in bodily pain and stressful appraisals of interpersonal interactions, but did not affect reactivity to negative interpersonal events. A different picture emerged with regard to the experience of positive event responsivity. Both chronic and transitory loneliness were associated with less interpersonal enjoyment, as expected. Moreover, both chronically lonely individuals and individuals experiencing temporary increases in loneliness reported a boost in interpersonal enjoyment on days with more positive interpersonal events than usual, contrary to hypothesized models.
Existing evidence gleaned from healthy adults has indicated that loneliness is associated with increased interpersonal stress levels (Hawkley, Burleson, Berntson, & Cacioppo, 2003; Hawkley & Cacioppo, 2007). The current study extends these findings by demonstrating that not only are chronically lonely individuals with chronic pain likely to report more interpersonal stress than their nonlonely counterparts, but they also experience worsened daily pain. These relations hold even when accounting for daily depressive symptoms, indicating that loneliness has implications for quality of life in chronic pain over and above the influence of depression. The findings are also consistent with the limited research to date linking social and physical pain in healthy individuals (Cacioppo et al., 2008; MacDonald & Leary, 2005). Beyond chronic loneliness, transitory loneliness was related to day-to-day experiences of persons with chronic pain. On days when individuals experienced a lonely episode, they also reported exacerbations in stress and marginally more pain, suggesting that even brief episodes of loneliness may affect daily quality of life among individuals with chronic pain.
Although they are associated with poorer health outcomes, neither chronic nor transitory loneliness appears to worsen pain or stress on days with more negative interpersonal events than usual. Previous work examining daily experiences in healthy individuals also found no association between loneliness and poorer responses to daily negative interpersonal events (Hawkley et al., 2007). Taken together, the existing research suggests that chronic and transitory loneliness are not associated with greater reactivity to daily negative interpersonal events in healthy individuals or those with FM. However, both forms of loneliness are linked to more frequent negative interpersonal events, more negative interpersonal appraisals, and more pain for individuals with FM pain.
In addition to highlighting the difficulties of lonely people with negative social interactions, prior work has found that lonely individuals may not find positive social interactions as rewarding as nonlonely individuals and thus do not experience the many benefits that come from being socially connected (Cacioppo et al., 2008; Hawkley et al., 2007). The current study found that both chronic and transitory loneliness were associated with reports of lower levels of enjoyment in social relations. Despite potential problems in their capacity to fully enjoy social relations, however, lonely individuals do appear to have the ability to benefit from positive interpersonal events. Contrary to hypotheses, chronically lonely people had greater boosts in enjoyment of their social relations on days with increased positive interpersonal events relative to people who were not lonely. In a similar pattern, on days with increased loneliness, experiencing an increase in positive interpersonal events was associated with a greater boost in enjoyment of social relations compared to days of decreased loneliness. Therefore, for people who feel chronically lonely, and when people feel an increase in loneliness, days with more positive events than usual are accompanied by a boost in the sense of enjoyment of social ties. These findings were maintained even when accounting for daily depressive symptoms. What can account for this unexpected “silver lining?” One possibility is that loneliness increases attention to socially relevant information, and may help individuals recognize opportunities to build more positive social bonds (Richman & Leary, 2009). The current study contextualizes previous laboratory-based findings that lonely individuals feel less rewarded by positive social cues by examining how daily increases in positive social interactions within their networks may actually foster adaptive changes in the way lonely individuals perceive social relations.
Previous research has suggested that lonely people report being more prone than nonlonely people to withdraw from social experiences (Cacioppo et al., 2000). However, the current work found that loneliness was unrelated to the total number of interpersonal events across 21 days, indicating that lonely people did not have fewer social events overall compared to those who were not lonely. Rather, lonely individuals came into contact with others, but their interpersonal exchanges were more often negative and less often positive compared to exchanges reported by their nonlonely counterparts. Of note, depression levels did not account for the relation between loneliness and more frequent negative events, but did account for the relation between loneliness and less frequent positive events (data not shown).
The current study has several limitations that are important to note. First, the study used a single question to assess loneliness rather than a multiple-item measure like the R-UCLA Loneliness Scale (Russell, Peplau, & Cutrona, 1980). On the other hand, deriving a chronic loneliness measure from 21 days of diary reports has the advantage of sampling feelings in daily life, which may provide a window into individuals’ typical ongoing experiences. Further, the pattern of associations between loneliness and interpersonal perceptions replicates those of earlier work on loneliness (e.g., Cacioppo et al., 2008; Hawkley et al., 2007), suggesting that the single-item measure employed over 21 days here provided an adequate assessment of the construct. Although the loneliness assessment appeared valid in the current study, research going forward should use more precise and comprehensive measures of loneliness that distinguish it from related measures such as depression and social support. A second limitation is the cross-sectional nature of the design. Because the current study evaluated concurrent relations based on end-of-day reports rather than testing lagged effects, temporal precedence cannot be established. Finally, the study also did not explore possible mechanisms linking loneliness with daily outcomes such as interpersonal cognitions or behaviors, which may help to elaborate how loneliness operates on a daily basis.
The findings highlight the potential value of daily increases in positive interpersonal events during episodes of loneliness and provide some clues to inform clinical work targeting lonely individuals who are managing a chronic pain condition. Incorporating strategies to help lonely people access positive interpersonal events may be paramount to improving their level of social connection. In addition to providing more opportunities for social interactions, however, treatments for loneliness may need to address maladaptive cognitions that could sabotage those interactions (Masi, Chen, Hawkley, & Cacioppo, 2011). Further, interventions for loneliness may need to be flexible in targeting both chronic and transient feelings of loneliness. For example, addressing broader maladaptive beliefs about social relationships and one’s ability to have positive interactions may be useful for alleviating chronic loneliness, whereas helping individuals quickly bounce back from more transient feelings of loneliness by reaching out to other people may address fluctuating feelings of loneliness. Some evidence suggests that targeting specific aspects of the experience of loneliness and associated social cognitions may have the additional benefit of alleviating future symptoms of depression (VanderWheele, Hawkley, Thisted, & Cacioppo, 2011).
In conclusion, the current findings together with those of earlier investigations indicate that both chronic loneliness and episodes of loneliness can have negative consequences. Among individuals dealing with FM pain, chronic and episodic loneliness relate to both pain and interpersonal stress. Nevertheless, the results are also encouraging. They suggest that although positive events may not happen as often for lonely people, such events can make a significant and positive difference in their level of interpersonal enjoyment when they do occur. Indeed, a positive social milieu among persons with chronic pain, including those with FM, helps to preserve functional health and well-being (Taylor, Davis, & Zautra, 2013). Capitalizing on the positive aspects of social relations while combating negative cognitive beliefs about interactions may be the key to helping lonely people in chronic pain successfully cope with many of the interpersonal challenges associated with their condition.
Acknowledgments
Research reported in this manuscript was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number R01 AR053245.
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience—cortisol associations in a population-based sample of older adults. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:17058–17063. doi: 10.1073/pnas.0605053103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold LM, Rosen A, Pritchett YL, D’Souza DN, Goldstein DJ, Iyengar S, Wernicke JF. A randomized, double-blind, placebo-controlled trial of duloxetine in the treatment of women with fibromyalgia with or without depressive disorder. Pain. 2005;119:5–15. doi: 10.1016/j.pain.2005.06.031. [DOI] [PubMed] [Google Scholar]
- Åsbring P, Närvänen A. Women’s experiences of stigma in relation to chronic fatigue syndrome and fibromyalgia. Qualitative Health Research. 2002;12:148–160. doi: 10.1177/104973230201200202. [DOI] [PubMed] [Google Scholar]
- Bennett R. The Fibromyalgia Impact Questionnaire (FIQ): A review of its development, current version, operating characteristics and uses. Clinical and Experimental Rheumatology. 2005;23:S154–S162. [PubMed] [Google Scholar]
- Cacioppo JT, Ernst JM, Burleson MH, McClintock MK, Malarkey WB, Hawkley LC, et al. Lonely traits and concomitant physiological processes: The MacArthur Social Neuroscience Studies. International Journal of Psychophysiology. 2000;35:143–154. doi: 10.1016/s0167-8760(99)00049-5. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Crawford LE, Ernst JM, Burleson MH, Kowalewski RB, Malarkey WB, Van Cauter E, Berntson GG. Loneliness and health: Potential mechanisms. Psychosomatic Medicine. 2002;64:407–417. doi: 10.1097/00006842-200205000-00005. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Ernst JM, Burleson M, Berntson GG, Nouriani B, Spiegel D. Loneliness within a nomological net: An evolutionary perspective. Journal of Research in Personality. 2006;40:1054–1085. [Google Scholar]
- Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging. 2010;25:453–463. doi: 10.1037/a0017216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychology and Aging. 2006;21:140–151. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Norris CJ, Decety J, Monteleone G, Nusbaum H. In the eye of the beholder: Individual differences in perceived social isolation predict regional brain activation to social stimuli. Journal of Cognitive Neuroscience. 2008;21:83–92. doi: 10.1162/jocn.2009.21007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis MC, Zautra AJ. An online mindfulness intervention targeting socioemotional regulation in fibromyalgia: Results of a randomized controlled trial. Annals of Behavioral Medicine. 2013 doi: 10.1007/s12160-013-9513-7. [DOI] [PubMed] [Google Scholar]
- Doane LD, Adam EK. Loneliness and cortisol: Momentary, day-to-day, and trait associations. Psychoneuroendocrinology. 2010;35:430–441. doi: 10.1016/j.psyneuen.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger NI, Lieberman MD. Why rejection hurts: a common neural alarm system for physical and social pain. Trends in Cognitive Sciences. 2004;8:294–300. doi: 10.1016/j.tics.2004.05.010. [DOI] [PubMed] [Google Scholar]
- Eisenberger NI, Lieberman MD, Williams KD. Does Rejection Hurt? An fMRI Study of Social Exclusion. Science. 2003;302:290–292. doi: 10.1126/science.1089134. [DOI] [PubMed] [Google Scholar]
- Enders CK, Tofighi D. Centering predictor variables in cross-sectional multilevel models: A new look at an old issue. Psychological Methods. 2007;12:121–138. doi: 10.1037/1082-989X.12.2.121. [DOI] [PubMed] [Google Scholar]
- Finan PH, Okun MA, Kruszewski D, Davis MC, Zautra AJ, Tennen H. Interplay of concurrent positive and negative interpersonal events in the prediction of daily negative affect and fatigue for rheumatoid arthritis patients. Health Psychology. 2010;29:429–437. doi: 10.1037/a0020230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finan PH, Zautra AJ, Davis MC. Daily affect relations in fibromyalgia patients reveal positive affective disturbance. Psychosomatic Medicine. 2009;71:474–482. doi: 10.1097/PSY.0b013e31819e0a8b. [DOI] [PubMed] [Google Scholar]
- Gaskin DJ, Richard P. The economic costs of pain in the United States. The Journal of Pain. 2012;13:715–724. doi: 10.1016/j.jpain.2012.03.009. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Burleson MH, Berntson GG, Cacioppo JT. Loneliness in everyday life: Cardiovascular activity, psychosocial context, and health behaviors. Journal of Personality & Social Psychology. 2003;85:105–120. doi: 10.1037/0022-3514.85.1.105. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Cacioppo JT. Aging and loneliness: Downhill quickly? Current Directions in Psychological Science. 2007;16:187–191. [Google Scholar]
- Hawkley LC, Cacioppo JT. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine. 2010;40:218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Masi CM, Berry JD, Cacioppo JT. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychology and Aging. 2006;21:152–164. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Preacher KJ, Cacioppo JT. Multilevel modeling of social interactions and mood in lonely and socially connected individuals: The MacArthur Social Neuroscience Studies. In: Ong AD, van Dulmen MHM, editors. Oxford Handbook of Methods in Positive Psychology. New York: Oxford University Press; 2007. pp. 559–575. [Google Scholar]
- Hawkley LC, Preacher KJ, Cacioppo JT. Loneliness impairs daytime functioning but not sleep duration. Health Psychology. 2010;29:124–129. doi: 10.1037/a0018646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Thisted RA, Cacioppo JT. Loneliness predicts reduced physical activity: Cross-sectional &longitudinal analyses. Health Psychology. 2009;28:354–363. doi: 10.1037/a0014400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs MJ, Hammerman-Rozenberg R, Cohen A, Stessman J. Chronic back pain among the elderly: Prevalence, associations, and predictors. Spine. 2006;31:E203–E207. doi: 10.1097/01.brs.0000206367.57918.3c. [DOI] [PubMed] [Google Scholar]
- Jaremka LM, Fagundes CP, Glaser R, Bennett JM, Malarkey WB, Kiecolt-Glaser JK. Loneliness predicts pain, depression, and fatigue: Understanding the role of immune dysregulation. Psychoneuroendocrinology. 2012 doi: 10.1016/j.psyneuen.2012.11.016. S0306-4530(12), 00403-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaremka LM, Fagundes CP, Peng J, Bennett JM, Glaser R, Malarkey WB, Kiecolt-Glaser JK. Loneliness promotes inflammation during acute stress. Psychological Science. 2013 doi: 10.1177/0956797612464059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: A comparison of six methods. Pain. 1986;27:117–126. doi: 10.1016/0304-3959(86)90228-9. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9: A new depression and diagnostic severity measure. Psychiatric Annals. 2002;32:509–521. [Google Scholar]
- Littell RC, Milliken GA, Stroup WW, Wolfinger RD, Schabenberger O. SAS for Mixed Models. 2. SAS Institute Inc; Cary NC: 2006. [Google Scholar]
- MacDonald G, Leary MR. Why does social exclusion hurt? The relationship between social and physical pain. Psychological Bulletin. 2005;131:202–223. doi: 10.1037/0033-2909.131.2.202. [DOI] [PubMed] [Google Scholar]
- Masi CM, Chen H, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. Personality and Social Psychology Review. 2011;15:219–266. doi: 10.1177/1088868310377394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peplau LA, Loneliness Perlman D. A sourcebook of current theory, research, and therapy. New York: Wiley Interscience; 2000. [Google Scholar]
- Potter PT, Zautra AJ, Reich JW. Stressful events and information processing dispositions moderate the relationship between positive and negative affect: Implications for pain patients. Ann Behav Med. 2000;22:191–198. doi: 10.1007/BF02895113. [DOI] [PubMed] [Google Scholar]
- Reynolds WM, Kobak KA. Hamilton Depression Inventory: A self-report version of the Hamilton Depression Rating Scale (HDRS) Odessa: Psychological Assessment Resources, Inc; 1995. [Google Scholar]
- Richman LS, Leary MR. Reactions to discrimination, stigmatization, ostracism, and other forms of interpersonal rejection: A multimotive model. Psychological Review. 2009;116:365–383. doi: 10.1037/a0015250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell D, Peplau LA, Cutrona C. The revised UCLA Loneliness Scale: Concurrent and discriminant validity. Journal of Personality and Social Psychology. 1980;39:472–480. doi: 10.1037//0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- Schoofs N, Bambini D, Ronning P, Bielak E, Woehl J. Death of a lifestyle: The effects of social support and healthcare support on the quality of life of persons with fibromyalgia and/or chronic fatigue syndrome. Orthopaedic Nursing. 2004;23:364–374. doi: 10.1097/00006416-200411000-00005. [DOI] [PubMed] [Google Scholar]
- Shankar A, McCmunn A, Banks J, Steptoe A. Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychology. 2011;30:377–385. doi: 10.1037/a0022826. [DOI] [PubMed] [Google Scholar]
- Skinner MA, Zautra AJ, Reich JW. Financial stress predictors and the emotional and physical health of chronic pain patients. Cognitive Therapy and Research. 2004;28:695–713. [Google Scholar]
- Taylor SS, Davis MC, Zautra AJ. Relationship status and quality moderate daily pain-related changes in physical disability, affect, and cognitions in women with chronic pain. Pain. 2013;154:147–153. doi: 10.1016/j.pain.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tse M, Leung R, Ho S. Pain and psychological well-being of older persons living in nursing homes: An exploratory study in planning patient-centered intervention. Journal of Advanced Nursing. 2012;68:312–321. doi: 10.1111/j.1365-2648.2011.05738.x. [DOI] [PubMed] [Google Scholar]
- Thieme K, Turk DC, Flor H. Comorbid depression and anxiety in fibromyalgia syndrome: Relationship to somatic and psychosocial variables. Psychosomatic Medicine. 2004;66:837–844. doi: 10.1097/01.psy.0000146329.63158.40. [DOI] [PubMed] [Google Scholar]
- VanderWheele TJ, Hawkley LC, Thisted RA, Cacioppo JT. A marginal structural model analysis for loneliness: Implications for intervention trials and clinical practice. Journal of Consulting and Clinical Psychology. 2011;79:225–235. doi: 10.1037/a0022610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wager TD, Atlas LY, Lindquist MA, Roy M, Woo C, Kross E. An fMRI-based neurological signature of physical pain. The New England Journal of Medicine. 2013;368:1388–1397. doi: 10.1056/NEJMoa1204471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA. Manual for the positive and negative affect schedule - expanded form. University of Iowa; 1994. [Google Scholar]
- Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, Sheon RP. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis and Rheumatism. 1990;33(2):160–172. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Schultz AS, Reich JW. The role of everyday events in depressive symptoms for older adults. In: Williamson GM, Shaffer DR, Parmelee PA, editors. Physical Illness and Depression in Older Adults: A Handbook of Theory, Research, and Practice. New York, NY: Kluwer Academic Publishers; 2000. pp. 65–91. [Google Scholar]