Abstract
Background
Although depressive symptoms are common postpartum, few studies have followed women beyond 12 months postpartum to investigate changes in the number and severity of these symptoms over time, especially in overweight and obese women. Using two complementary analytical methods, this study aims to identify trajectories of depressive symptoms over two years postpartum among overweight or obese mothers, and assess the demographic, socio-economic , and health covariates for these trajectories.
Methods
Using longitudinal data from two behavioral intervention studies (KAN-DO and AMP; N = 844), we used latent growth modeling to identify the overall trajectory of depressive symptoms and how it was related to key covariates. Next, we used latent class growth analysis to assess the heterogeneity in the depressive symptom trajectories over time, and thereby, identify subgroups of women with distinct trajectories.
Findings
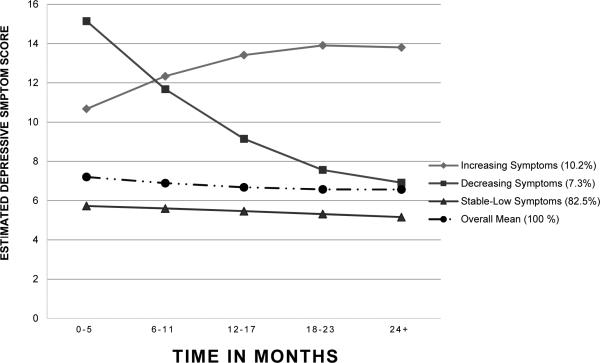
The overall trajectory of depressive symptoms over two years postpartum was relatively stable in our sample. However, the presence of three distinct latent class trajectories [stable-low (82.5%), decreasing symptoms (7.3%) and increasing symptoms (10.2%)], identified based on trajectory shape and mean depressive symptom score, supported heterogeneity in depressive symptom trajectories over time. Lower maternal education was related to a higher symptom score, and poorer subjective health status at baseline predicted inclusion in the increasing symptoms trajectory.
Conclusions
In some overweight or obese mothers postpartum depressive symptoms do not resolve quickly. Practitioners should be aware of this phenomenon and continue to screen for depression for longer periods of time postpartum.
Keywords: Postpartum depression, Obesity, Overweight, Trajectory analysis, USA
Introduction
Affective disorders are common postpartum, with the prevalence of any affective disorder, including the “baby blues”, reported to be as high as 40-60% (Reck, Stehle, Reinig, & Mundt, 2009). Postpartum depression (PPD), one type of affective disorder, occurs in 10-15% of new mothers (Gavin et al., 2005). The recent version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) (American Psychiatric Association, 2013) does not recognize PPD as a separate diagnosis, but rather as major depressive disorder with postpartum onset. Postpartum onset is defined here as within four weeks of childbirth. Symptoms of PPD include dysphoric feelings, changes in sleep or appetite, fatigue, and excessive guilt (O'hara & Swain, 1996). Symptoms generally last between a few weeks and six months following childbirth, but may persist longer for some women (Campbell, Cohn, Flanagan, Popper, & Meyers, 1992). Acknowledging PPD when it occurs is important for maintaining maternal well-being as well as family relationships and functioning (Burke, 2003; Luoma et al., 2001).
A few studies have evaluated PPD symptoms longitudinally (i.e. how they may change over time; Brugha, Morrell, Slade, & Walters, 2011; Bugdayci, Sasmaz, Tezcan, Kurt, & Oner, 2004; Edwards et al., 2012; Horowitz & Goodman, 2004; Mayberry, Horowitz, & Declercq, 2007; Ramos-Marcuse et al., 2010; Small, Brown, Lumley, & Astbury, 1994; Wu, Selig, Roberts, & Steele, 2011) and the degree of heterogeneity in symptom patterns among women beyond the first year postpartum (Mora et al., 2009; Ramos-Marcuse et al., 2010). Wu, Selig, Roberts, and Steele (2011) showed that the average trajectory of maternal depressive symptoms appears to be U-shaped with a nadir at 20 months and a gradual increase thereafter. A Turkish study (Bugdayci et al., 2004) assessed the prevalence and risk of developing PPD during and beyond the first year after childbirth. That study observed an increased prevalence of PPD over time, with a 42.7% increase at ≥13 months compared to the 0-2 month period and an increase in the risk for PPD over time (1.82 times greater at ≥13 months compared to the 0-2 month period. Another study followed women for two years postpartum and observed the continued presence of mild and moderate-to-severe depressive symptoms throughout that same period (Mayberry et al., 2007). With a few exceptions (e.g., Mora et al., 2009; Ramos-Marcuse et al., 2010; Sutter-Dallay, Cosnefroy, Glatigny-Dallay, Verdoux, & Rascle, 2012), there has been limited study of heterogeneity in depressive symptoms over time. Ramos-Marcuse and his colleagues (2010) evaluated the stability of maternal depression symptoms among African American adolescent mothers (n=181), and identified three distinct trajectory groups; a “low”, “medium”, and “high” group based on their level of depressive symptoms over the 12 month postpartum period. The high group reported elevated symptoms throughout the 12 months. Among a sample of 1,735 women followed from pregnancy through the 24 months postpartum, Mora et al. (2009) identified 5 depressive symptom trajectories: 1) “chronic, persistently high level of depressive symptoms (7% of sample)”; 2) “antepartum depressive symptomatology present only at the first prenatal visit”; 3) “postpartum depressive symptoms present within 6 weeks of delivery that subside over time”; 4) “late with low levels of depressive symptoms ante- and peripartum that increase in the second year postpartum”; and 5) “never elevated, with continuous low levels of depressive symptoms”. The “late” group above, those with rapidly increasing depression scores between 12 to 24 months, supports the notion that depressive symptoms postpartum may persist or increase for some women long after the delivery of their child. Finally, among a sample of 579 women, Sutter-Dallay (2012) identified four distinct trajectories from pregnancy to two years postpartum in a low risk cohort: depressive symptoms only during the postnatal period; depressive symptoms throughout the follow-up period, with a higher intensity during pregnancy; and stable highly intense symptoms throughout the follow-up period. Together, these studies highlight the heterogeneity in terms of patterns of postpartum or perinatal depressive symptoms from delivery up until 24 months. Additional research is needed to further describe the patterns of depressive symptoms over a longer period beyond just the 3-6 months following delivery. It would also be important to evaluate these trajectory patterns among women who may be at greater risk for depressive symptoms.
Women who are overweight or obese have been shown to be at greater risk for depressive symptoms in the postpartum period, possibly due to their higher likelihood of complications during pregnancy and delivery (Carter, Baker, & Brownell, 2000; LaCoursiere, Baksh, Bloebaum, & Varner, 2006; LaCoursiere, Barrett-Connor, O'Hara, Hutton, & Varner, 2010). However, this relationship has not been consistently found (Boury, Larkin, & Krummel, 2004; Milgrom, Skouteris, Worotniuk, Henwood, & Bruce, 2012; Vernon, Young-Hyman, & Looney, 2010). In addition to different study designs (e.g., cross-sectional vs. longitudinal; duration of observation; normal weight vs. overweight/obese, and different inclusion criteria), this inconsistency in findings may also be due to differences in trajectories of depressive symptoms. In this study, we extend the existing literature on PPD by observing the heterogeneity in depressive symptoms score trajectories (common patterns of change) over the first two years postpartum in a population of new mothers who were overweight or obese (body mass index (BMI) ≥ 25 kg/m2) before pregnancy.
A number of demographic and social characteristics have been examined in the context of postpartum depressive symptoms. For instance, younger maternal age, single/divorced marital status, and lack of social support have been reported to be correlated to both a longer duration and greater severity of depressive symptoms during the postpartum period (Bugdayci et al., 2004; Campbell et al., 1992; Mayberry et al., 2007; O'hara & Swain, 1996; Robertson, Grace, Wallington, & Stewart, 2004). Low socio-economic status (SES) is also related to a higher likelihood of depression (Lorant, Deliège, Eaton, Robert, Philipot, and Ansseau, 2003). In the present study, these demographic and social characteristics were included as potential predictors of postpartum depressive symptoms among a primarily overweight or obese group of women.
Research Questions and Hypotheses
The purpose of this study was to evaluate changes in depressive symptoms over two years postpartum among overweight or obese mothers, and assess the relationships of SES, demographic characteristics, and health covariates (BMI, self-reported overall health, and parity) with the trajectory of depressive symptoms, controlling for participation in a weight-loss intervention. We used two different but complementary analytical approaches. We first conducted latent growth modeling to identify the shape of the overall trajectory of depressive symptoms and how it is related to maternal socio-demographic and health characteristics. However, this analytical approach assumes homogeneity of the population with regard to the pattern of change in depressive symptoms over time. Thus, we then applied a complementary technique, latent class growth analysis, to identity potential classes (subgroups) of women that follow distinct trajectories of depressive symptoms.
Building on previous studies, three general hypotheses guided the present study. First, depressive symptoms would generally resolve for a majority of overweight or obese women. Second, there would be heterogeneity in the pattern of depressive symptoms over time among overweight or obese women. Third, younger maternal age, lower educational level, and lower income would be related to more depressive symptoms throughout the postpartum period.
Methods
Overall Design
We conducted secondary analysis of data from Active Mothers Postpartum (AMP; n = 400) and Kids and Adults Now!-Defeat Obesity (KAN-DO; n = 450), two randomized control behavioral intervention trials conducted in the Triangle and Triad areas of North Carolina. The design and rationale for both studies have been published previously (Østbye et al., 2008; Østbye et al., 2011). Study participants in both studies were women between 4 weeks to 7 months postpartum at the time of their baseline assessment, who were followed until approximately 24 months postpartum (see Table 2). On average, each AMP participant provided 2.50 (ranged from 1 to 3) data points whereas KAN-DO participants provided 1.86 data points (ranged from 0 to 2). Because six cases were missing depression scores across all time points, the final analytical sample of the current study was 844.
Table 2.
Sample size by time points and study
| Time point (postpartum period range in months) | T1 (0-5 months) | T2 (6-11 months) | T3 (12-17 months) | T4 (18-23 months) | T5 (24+ months) |
|---|---|---|---|---|---|
| KAN-DO | 273 | 145 | 280 | 27 | 275 |
| AMP | 426 | 14 | 4 | 332 | 50 |
| Overall | 699 | 159 | 284 | 359 | 325 |
Note. On average, each participant from AMP provided 2.50 (ranged from 1 to 3) data points whereas KAN-DO participants provided 1.86 data points (ranged from 0 to 2)
Active Mothers Postpartum (AMP)
AMP was a randomized behavioral intervention trial to evaluate the effect of an intervention to promote physical activity and healthy diet for weight loss among overweight and obese (BMI ≥25 kg/m2 based on self-reported pre-pregnancy BMI) postpartum women. Women were randomized to either minimal care or the AMP intervention, which included telephone counseling and group classes to educate and motivate mothers regarding healthy diet and increased physical activity. Women in the study completed a baseline survey (i.e., with 2 months of delivery of a baby) and follow-up surveys at 12 and 24 months post-baseline.
Kids and Adults Now – Defeat Obesity (KAN-DO)
KAN-DO was also a randomized behavioral intervention trial. It was designed to promote healthy eating, increased physical activity, and healthy weight attainment in preschoolers (age 2-5) and their overweight and obese postpartum mothers who were recruited within six months of delivering a new baby. These mothers were followed-up at 10 months post-baseline and again one year later. Women had to have a self-reported pre-pregnancy BMI ≥25 kg/m2, and a verified BMI ≥25 kg/m2 postpartum, as measured by study staff on calibrated scales during the baseline visit, to be included in the study. Women randomized to the control group received a general reading intervention not related to weight, food, or physical activity.
Measures
Depressive symptoms
Women were assessed for PPD at every visit in both AMP and KAN-DO using the Edinburgh Postnatal Depression Scale (EPDS) (Cox, Holden, & Sagovsky, 1987). The EPDS is a 10-item scale assessing psychological, cognitive, and emotional disturbance over the past week. Each item is scored from 0-3, with a possible total score of 0-30. EDPS has been validated for detection of major depression episodes in postpartum women (Cox, Chapman, Murray, & Jones, 1996). Generally, a score of 13 or above suggests PPD (Murray & Carothers, 1990). Women could contribute one to three EPDS measurements to the trajectories depending on how many assessments they completed.
Maternal demographic characteristics, SES, and health covariates
Covariates, measured at baseline, included maternal demographic characteristics, SES, race (white vs. non-white), age, marital status (married vs. not), education (high school diploma or less, vocational or some college, college degree, at least some post-grad education), annual family income (up to $15,000, $15,001 to $30,000, $30,001 to $45,000, $45,001 to $60,000, and $60,001 or more), work status (working full or part time versus not working for pay), and subjective overall health status (a single question scored from 1 [poor] to 5 [excellent]).
Control variables
Variables that were controlled for in the analyses included maternal BMI and parity (range: 1-7), study (KAN-DO vs. AMP), and arm (control vs. intervention group).
Statistical Analysis
Latent growth modeling (LGM) using Mplus, version 7.11, was utilized to model the overall trajectory of depressive symptoms over time, from baseline through 24 months postpartum among the participants. Individual participants contributed up to three repeated observations of depressive symptoms at different months during the postpartum follow-up. These data were then grouped into five time points based on month postpartum at the time of assessment (0-5, 6-11, 12-17, 18-23, and 24+ month). Women with at least one depressive symptom score available were included as Mplus employs full information maximum likelihood (FIML) to handle missing data. FMIL allows all parameters to be estimated directly without imputing missing data (Muthén & Muthén, 1998-2006). The rationale for favoring FIML, over other methods such as listwise deletion or pairwise deletion, is that it provides more robust and efficient estimations as outlined by Enders and Bandalos (2001), and reduces the possibility of errors, as the handling of missing data is done within the model and takes all variables in the model into consideration. LGM is a statistical technique that estimates the parameters of the intercept (i.e., average level of starting point), slope (i.e., rate of increase/decrease over time), and curvature (i.e., the rate of change in the increase/decrease) for the growth curve or overall trajectory of a variable (in this case, postpartum depressive symptoms) (Bollen & Curran, 2006; Duncan & Duncan, 2004). It also allows for determining the influence of a particular covariate on the intercept, slope and curvature of the growth curve, as was done for the covariates (i.e., demographic characteristics, SES, and health condition) in this analysis. LGM is a variant of structural equation modeling (Bollen & Curran, 2006; Christ & Schlueter, 2007), that overcomes the shortcomings of traditional statistical approaches (e.g. autoregressive models, repeated t-tests/ANOVA/MANOVA) when dealing with longitudinal data by assessing the changes over time and delineating the change of trajectory between and within individuals (Preacher, Wichman, MacCallum, & Briggs, 2008).
However, LGM assumes homogeneity of the population, which may not accurately reflect an empirical conceptualization of depressive symptom variation in the population. Therefore, to allow for heterogeneity, or the potential for subgroups of women with distinct trajectories of postpartum depressive symptoms, latent class growth analysis (LCGA) was subsequently applied to identify such subgroups based on trajectories of depressive symptoms. Model fit was evaluated by Bayesian Information Criterion (BIC) (Schwarz, 1978), entropy (i.e., indicator of the precision of classification), the percentage in the smallest subgroup, parsimony and substantive interpretability (models with lower BIC values, higher entropy, and same size in the smallest class/subgroup are preferred) (Connell, Dishion, & Deater-Deckard, 2006; Muthén & Muthén, 2000). After the best-fitting model was established, the association between the covariates of interest and identified subgroups, each with a distinct depressive symptoms trajectory, was examined via multinomial logistic regression. This was done within Mplus 7.11 using 20 pseudo draws based on posterior probabilities of group membership for each individual. The results reported here examine the association of a covariate with individual depressive symptoms groups as compared with one of the other groups (Clark & Muthén, 2009).
Results
Descriptive Statistics
Table 1 presents the baseline characteristics of the full sample. The largest groups of women in the two studies were married (76.9%), white (62.8%), had annual income above $60,000 (48.2%), had earned a college degree (36.9%), and rated their physical health as good (40.3%). The mean age of participants was 31.9 (SD = 5.4) years.
Table 1.
Demographic, socioeconomic status and health characteristics of the study sample at baseline (and, for PPD score, at follow up) (N = 844)
| Variable | M (SD) or n (%) |
|---|---|
| Age, years | 31.70 (5.33) |
| Married | 670 (79.4%) |
| Race | |
| White | 534 (63.3%) |
| Black | 288 (34.1%) |
| Other | 22 (2.6%) |
| Family Income | |
| Up to $15,000 | 67 (8.0%) |
| $15,000–$30,000 | 128 (15.3%) |
| $30,001–$45,000 | 99 (11.8%) |
| $45,001–$60,000 | 124 (14.8%) |
| $60,001 or more | 420 (49.8%) |
| Education | |
| High school diploma or less | 136 (16.1%) |
| Vocational or some college | 189 (22.4%) |
| College degree | 302 (35.8%) |
| Some post-grad education | 217 (25.7%) |
| Work Status | |
| Not working for pay | 552 (65.4%) |
| Full/Part-time | 292 (34.6%) |
| Self-Rated Physical Health | |
| Poor | 9 (1.1%) |
| Fair | 76 (9.0%) |
| Good | 330 (39.1%) |
| Very good | 317 (37.6%) |
| Excellent | 112 (13.3%) |
| BMI | 32.89 (6.04) |
| Parity | 2.18 (0.97) |
| EPDS Depression Score | |
| 0-5 months | 7.08 (4.66) |
| 6-11 months | 7.75 (4.64) |
| 12-17 months | 7.30 (4.64) |
| 18-23 months | 6.06 (4.22) |
| 24+ months | 6.82 (4.70) |
| Study | |
| KAN-DO | 400 (47.4%) |
| AMP | 444 (52.6%) |
| Study arm | |
| Control | 421 (49.9%) |
| Intervention | 423 (50.1%) |
Note: KAN-DO = Kids and Adults Now - Defeat Obesity; AMP = Active Mothers Postpartum; EPDS= Edinburgh Postnatal Depression Scale.
Latent Growth Modeling of Change in Postpartum Depressive Symptoms
The overall postpartum depressive symptoms trajectory had a logit-unit estimated intercept (i.e., initial level of depressive scores) of 2.48 (SE = 0.58, p < .001), slope (i.e., how much decrease/increase from initial level of depressive scores) of −.84 (SE= 2.62, p =.749) and curvature (i.e., the upturn/downturn of the linear change of depressive scores, representing the non-linear changes over time) of .253 (SE = 2.40, p =.916). Neither slope nor curvature terms reached statistical significance, indicating that there were no changes (linear or non-linear) over time, in other words: the average symptom endorsement over time was quite stable. The estimated mean EPDS score reported by the participants at baseline was 7.20, implying that on average women did not reach the level of a likely clinical diagnosis of depression (see Figure 1).
Fig. 1.
Trajectories of depressive symptoms across observations (n = 844).
Table 3 shows that mothers with higher income (b = −.15, p = 0.020) or better self-rated physical health reported less depressive symptoms (b = −.28, p < 0.001) at baseline. Higher educational level was associated with decreasing in depressive symptoms (slope b = −.97, p < .001; quadratic b = .93, p < .001).
Table 3.
The relationship between covariates and intercept, slope and curvature of the overall trajectory of postpartum depressive symptoms: Results from Latent Growth Modeling
| Intercept | Slope | Curvature | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Est. | SE | p | Est. | SE | p | Est. | SE | p | |
| Intercept | 2.48 | 0.58 | < .001 | −0.84 | 2.62 | 0.749 | 0.25 | 2.40 | 0.916 |
| Age | −0.03 | 0.06 | 0.674 | 0.20 | 0.28 | 0.469 | −0.14 | 0.26 | 0.572 |
| Married | −0.09 | 0.07 | 0.172 | −0.18 | 0.35 | 0.594 | 0.06 | 0.34 | 0.850 |
| White (vs. Non-White) | 0.09 | 0.06 | 0.139 | −0.17 | 0.28 | 0.537 | 0.27 | 0.26 | 0.305 |
| Education | 0.00 | 0.07 | 0.993 | −0.97 | 0.25 | < .001 | 0.93 | 0.26 | < .001 |
| Family Income | −0.15 | 0.06 | 0.020 | 0.40 | 0.29 | 0.162 | −0.38 | 0.26 | 0.146 |
| Work Full-/Part-time | −0.03 | 0.06 | 0.532 | 0.01 | 0.22 | 0.948 | −0.02 | 0.18 | 0.919 |
| Self-Rated Physical Health | −0.28 | 0.06 | < .001 | 0.07 | 0.24 | 0.762 | −0.01 | 0.21 | 0.963 |
| BMI | −0.07 | 0.06 | 0.239 | 0.23 | 0.23 | 0.316 | −0.19 | 0.21 | 0.362 |
| Parity | 0.05 | 0.06 | 0.396 | 0.13 | 0.25 | 0.619 | −0.16 | 0.22 | 0.469 |
| KAN-DO Study (vs. AMP) | −0.14 | 0.06 | 0.029 | 0.01 | 0.38 | 0.988 | 0.02 | 0.39 | 0.963 |
| Control arm (vs. Intervention) | 0.06 | 0.05 | 0.214 | −0.10 | 0.21 | 0.617 | 0.14 | 0.19 | 0.457 |
Latent Class Growth Analysis of Postpartum Depressive Symptoms
The model fit of trajectories of postpartum depressive symptoms was compared by testing for two to four classes (subgroups; see Table 4). BIC decreased with increasing number of classes. The 4-class model had a smaller BIC (10362.60) than the 3-class model and better entropy (.76) than the 3-class model (.73). However, the 4-class model yielded one additional group of participants, with a sample size 18, who had dramatic changes in depressive symptoms, suggesting this class may not truly represent a meaningful group. Thus, based on the principle of parsimony and substantive interpretability, we chose the 3-class model as the final solution. In Figure 1, we present the three trajectory groups showing the heterogeneity in experiencing postpartum depressive symptoms. Table 5 presents the relations of demographic characteristic to the classes (subgroups) of depressive symptoms trajectories.
Table 4.
Summary of latent class growth analysis model fit statistics (N = 844)
| Models | BIC | Entropy | % of the Smallest Class |
|---|---|---|---|
| 2-class | 10378.89 | .72 | 13.5% |
| 3-class | 10364.53 | .73 | 7.3% |
| 4-class | 10362.60 | .76 | 2.1% |
Note. BIC = Bayesian Information Criterion; lower values demonstrate better model fit. Higher value of entropy indicated greater precision of classification.
Table 5.
Covariates of Latent Depressive Symptoms Trajectory Groups (Multinomial Logistic Regression; N = 844)
| Increasing Symptoms vs. Stable-Low Symptoms | Increasing Symptoms vs. Decreasing Symptoms | Decreasing Symptoms vs. Stable-Low Symptoms | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Est. | SE | p | Est. | SE | p | Est. | SE | p | |
| Age | 0.02 | 0.03 | 0.427 | −0.02 | 0.04 | 0.627 | 0.04 | 0.05 | 0.340 |
| Married | −0.68 | 0.43 | 0.110 | −0.19 | 0.47 | 0.683 | −0.49 | 0.59 | 0.412 |
| White (vs. Non-White) | 0.33 | 0.35 | 0.335 | 0.32 | 0.38 | 0.395 | 0.01 | 0.48 | 0.978 |
| Education | −0.10 | 0.10 | 0.345 | 0.02 | 0.12 | 0.855 | −0.12 | 0.15 | 0.428 |
| Family Income | −0.19 | 0.13 | 0.135 | −0.17 | 0.15 | 0.275 | −0.02 | 0.20 | 0.909 |
| Work Full-/Part-time | −0.02 | 0.30 | 0.956 | −0.02 | 0.35 | 0.952 | 0.01 | 0.44 | 0.991 |
| Self-Rated Physical Health | −0.42 | 0.17 | 0.013 | −0.43 | 0.20 | 0.036 | 0.01 | 0.25 | 0.974 |
| BMI | −0.01 | 0.02 | 0.709 | 0.00 | 0.03 | 0.973 | −0.01 | 0.03 | 0.814 |
| Parity | −0.03 | 0.15 | 0.862 | 0.01 | 0.18 | 0.941 | −0.04 | 0.21 | 0.854 |
| KAN-DO Study (vs. AMP) | −0.52 | 0.32 | 0.109 | −0.48 | 0.37 | 0.202 | −0.04 | 0.47 | 0.932 |
| Control arm (vs. Intervention) | 0.21 | 0.27 | 0.432 | 0.26 | 0.31 | 0.398 | −0.05 | 0.39 | 0.893 |
Class 1 (the “stable-low symptoms group”) included 696 individuals (82.5%), with 63.1% white and a mean age of 31.93 (SD = 5.15). This class was marked by consistently reporting the lowest EPDS score over time. The average depression scores at the five time points were 5.75 (SD = 3.42), 5.78 (SD = 3.10), 5.96 (SD = 3.44), 5.07 (SD = 3.25) and 5.49 (SD = 3.44).
Class 2 (the “decreasing symptoms group”) included 62 individuals (7.3 %), with 66.1% white and a mean age of 29.83 (SD = 6.31). This class was characterized by a decreasing score during the entire follow-up period. The average scores were 16.36 (SD = 3.01), 13.50 (SD = 3.34), 8.65 (SD = 3.21), 8.03 (SD = 4.00), and 6.13 (SD = 3.72), which may reflect gradual resolution of depressive symptoms.
Class 3 (the “increasing symptoms group”) comprised 86 women (10.2 %), with 62.8% white and a mean age of 31.10 (SD = 5.75). The symptom profile of this class was characterized by a moderate increase in score over time. The average scores were 11.42 (SD = 3.91), 13.67 (SD = 3.36), 14.00 (SD = 4.47), 14.96 (SD = 2.37) and 14.93 (SD =3.26), suggesting that women in this group may be experiencing a clinical level of PPD.
Multinomial logistic regression analysis (Table 5) was performed simultaneously with the LCGA to compare the differences in the covariates for each pair of classes. We found that women in the increasing symptoms group, relative to those in the other two groups (decreasing symptoms and stable-low symptoms), were less likely to report good physical health at baseline. Otherwise, there were no significant differences in covariate relationships between any groups.
Discussion and Conclusions
The present study examined the change in depressive symptoms over two years postpartum among overweight or obese mothers, and assessed the demographic characteristics (e.g., SES) and health covariates for trajectories of depressive symptom scores, as measured by the EPDS. First, the overall trajectory of depressive symptom scores over two years of postpartum appears to be relatively stable over time (EPDS scores between 6 and 8, on average, at each of the five time points). We did find, however, that compared to mothers with higher educational attainment, mothers with lower educational attainment reported a more rapid increase in depressive symptoms in the two years following childbirth. Second, there was heterogeneity in the pattern of the scores over time among overweight and obese mothers, and three latent classes (subgroups) were identified based on the shape and average depressive symptom scores endorsed over time: stable-low symptoms, decreasing symptoms and increasing symptoms. Health status primarily distinguished between individuals in the increasing symptoms group and the other two groups (decreasing symptoms and stable-low symptoms groups), with women who reported poorer overall health status more likely to belong to the increasing symptoms group.
The first important contribution made by this study is the identification of the heterogeneity in the patterns of depressive symptoms experienced by overweight and obese mothers postpartum. Indeed, the overall trajectory or average depressive symptom scores observed among overweight and obese mothers in the current study did not meet a clinical diagnosis of PPD. This may lead one to conclude that overweight or obese women in general have very low risk of PPD. However, assessment of the variation within the study participants identified a subgroup of women (“increasing symptoms”) who met the criterion for PPD, with the depressive symptom score remaining high up-to and beyond 12 months postpartum among these women. While little is known about PPD trajectories beyond the first year postpartum in overweight and obese women, several studies have been conducted in the general population of new mothers. Although the trajectories of depression symptoms vary across studies, likely due to differing study design, (e.g., sample size and length of follow-up), similar patterns were not uncommon, namely, an elevated number of depressive symptoms even beyond the first year, in some women (Mora et al., 2009; Ramos-Marcuse et al., 2010). Our study confirmed the continuation of clinically significant levels of PPD symptoms beyond the first year in approximately 10% of a population of overweight and obese mothers. Similar to Mora et al. (2009), we also identified 7% of the women in the current study to be in the decreasing symptoms group based on their PPD symptoms trajectory which was high in the beginning of the assessment but decreased over time. The trajectory for this group is consistent with the general impression that PPD-symptoms decrease or resolve within six months postpartum, possibly due to clinical intervention. It is worth noting that this group constitutes less than half of the women who experienced PPD symptoms, suggesting the importance of early recognition of PPD symptoms, and clinical attention.
Another interesting finding is the role the covariates may play in the depressive symptoms experienced by overweight or obese women. In the context of the overall trajectory outlined through LGM, in addition to low income and poor physical health being associated with a higher level of depressive symptoms at baseline, we also found that lower maternal education -predicted an increasing EPDS score over time. Women with lower levels of education may experience more financial stress, which could contribute to an increased number, or longer persistence, of PPD symptoms (see Liu & Tronick, 2013). Our results and those of others highlight the importance of monitoring and evaluating PPD symptoms, especially among those women with lower education and poorer overall health, who may not differentiate PPD from being moody or from physical sickness. Support services for stress management and for maintaining regular physical activities for these new mothers may be needed to ensure a healthy transition from the postpartum period.
Women in the increasing symptoms group had a poorer rating of health status at baseline than their counterparts, consistent with the findings from previous research (Eastwood, Phung, & Barnett, 2011). Decreased energy levels and increased fatigue are not only associated with an increased likelihood to report an overall lower health status but also with an increase in symptoms of clinical depression. This may lead to higher levels of PPD symptoms as participants overlooked their depressive symptoms, or attributed symptoms of PPD to their physical health problems.
Physically activity, in general, has been shown to decrease depressive symptoms (Cooney et al., 2013), although this association may differ across situations (e.g., household chores, occupational requirements, and leisure time) among postpartum women (Demissie, et al, 2011; Teychenne & York, 2013). Similarly, there are some studies of the association between nutrition/diet and PPD (see Ellsworth-Browers & Corwin, 2013). In the present study, we did not see a protective effect of participating in an intervention that targeted behaviors related to diet and physical activity. Available data for this analysis of PPD symptoms trajectories did not contain information on diet and physical activity measures, so we were unable to assess if participants in the intervention made meaningful improvements in these areas. Future studies, both observational and interventions are needed to specifically address the role of physical activity and diet in overweight and obese women as relating to PPD.
Strengths and Limitations
The strengths of our study include the large sample size; the racial and economic diversity of our sample; the repeated measurements during the first two years postpartum; the use of the EPDS, which has been validated for measurement of both postpartum and non-postpartum depressive symptoms; and the use of two complementary techniques for longitudinal data analysis. We employed both LGM and LCGA to delineate an overall trend as well as identify subgroups of women with differential depressive symptoms trajectories. The two approaches were generally concordant. LGM showed an overall moderate (sub-clinical) level of depressive symptoms, which remained stable over time, while in the subgroups identified using LGCA, groups with increasing and decreasing symptoms over time were observed.
The application of these methods to the study of PPD is relatively unique. Such applications can help elucidate factors associated with the dynamics of symptom change over time. Continued research on the role of stressors such as economic stress, financial concerns, and limited access to health care may help to clarify why women of lower education have disproportionate burden of depressive symptoms during the postpartum period.
Limitations include the fact that this is a secondary analysis of data from women in two different postpartum intervention studies. In spite of the longitudinal data available, any inferences about causation based on this data must be drawn with caution since neither study assessed depression prior to or during pregnancy; it is possible that some women had depressive symptoms prior to baseline. Finally, although it could be considered a limitation that not all women contributed data to all the time points, Mplus employs an expectation maximization (EM) algorithm to deal with missing data and thereby limit potential biases (Duncan, Duncan, & Strycker, 2006).
Implications for Practice and/or Policy
Similar to findings from studies of new mothers in general, this study suggests that for some overweight and obese women postpartum depressive symptoms do not resolve quickly. Screening for depression in new mothers during the early postpartum months is quite common, but these practices may need to be extended through the well-child visits up to two years postpartum. Women with lower education or poor subjective health status are at the highest risk for a pattern of increasing depressive symptoms during the two years following childbirth; thus, these women should be targets of such screening efforts. Women with PPD may experience symptom reduction from behavioral (Horowitz & Goodman, 2005; Reay, Fisher, Robertson, Adams, & Owen, 2006) or pharmacological treatment (Ng, Hirata, Yeung, Haller, & Finley, 2010). In addition to such clinical interventions, increased social support may benefit women experiencing PPD symptoms (Xie, He, Koszycki, Walker, & Wen, 2009).
Future studies should look at the variability in the number of depressive symptoms over time, even at the sub-clinical level; increases over time may indicate a need for intervention. In particular, this should include investigations of protective factors, such as social support and evaluation of the effects of depressive symptoms over time on subsequent health and psychosocial outcomes in the women and their children and interpersonal family dynamics.
Acknowledgments
Funding Source: The work on this study was supported by grants from the National Institute of Health (NIH), National Institute of Diabetes, Digestive and Kidney Diseases (R01-DK064986 and R01-DK-07549).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Disclosure Statement: The authors have no conflicts of interest to disclose.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th ed. American Psychiatric Association; Arlington, VA: 2013. [Google Scholar]
- Bollen KA, Curran PJ. Latent curve models: A structural equation perspective. John Wiley & Sons.; Hoboken, NJ: 2006. [Google Scholar]
- Boury JM, Larkin KT, Krummel DA. Factors related to postpartum depressive symptoms in low-income women. Women Health. 2004;39(3):19–34. doi: 10.1300/J013v39n03_02. doi: 10.1300/J013v39n03_02. [DOI] [PubMed] [Google Scholar]
- Brugha TS, Morrell CJ, Slade P, Walters SJ. Universal prevention of depression in women postnatally: cluster randomized trial evidence in primary care. Psychological Medicine. 2011;41(04):739–748. doi: 10.1017/S0033291710001467. doi: doi:10.1017/S0033291710001467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bugdayci R, Sasmaz CT, Tezcan H, Kurt AO, Oner S. A cross-sectional prevalence study of depression at various times after delivery in Mersin province in Turkey. Journal of women's health (2002) 2004;13(1):63–68. doi: 10.1089/154099904322836465. [DOI] [PubMed] [Google Scholar]
- Burke L. The impact of maternal depression on familial relationship. International Review of Psychiatry. 2003;15:243–255. doi: 10.1080/0954026031000136866. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Cohn JF, Flanagan C, Popper S, Meyers T. Course and correlates of postpartum depression during the transition to parenthood. Development and Psychopathology. 1992;4(01):29–47. doi: doi:10.1017/S095457940000554X. [Google Scholar]
- Carter AS, Baker CW, Brownell KD. Body mass index, eating attitudes, and symptoms of depression and anxiety in pregnancy and the postpartum period. Psychosom Med. 2000;62(2):264–270. doi: 10.1097/00006842-200003000-00019. [DOI] [PubMed] [Google Scholar]
- Christ O, Schlueter E. Latent growth curve models. In: Ritzer G, editor. Blackwell encyclopedia of sociology. Vol. 6. Blackwell Publishing; Malden, MA: 2007. pp. 2542–2546. [Google Scholar]
- Clark S, Muthén B. Relating Latent Class Analysis Results to Variables Not Included in the Analysis. 2009 from http://www.statmodel.com/download/relatinglca.pdf.
- Connell AM, Dishion TJ, Deater-Deckard K. Variable-and Person-Centered Approaches to the Analysis of Early Adolescent Substance Use: Linking Peer, Family, and Intervention Effects with Developmental Trajectories. Merrill-Palmer Quarterly: Journal of Developmental Psychology. 2006;52(3):421–448. doi: doi:10.1353/mpq.2006.0025. [Google Scholar]
- Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh F, R. Exercise for depression. Cochrane Database of Systematic Reviews. 2013;9 doi: 10.1002/14651858.CD004366.pub6. doi: 10.1002/14651858.CD004366.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox JL, Chapman G, Murray D, Jones P. Validation of the Edinburgh postnatal depression scale (EPDS) in non-postnatal women. Journal of Affective Disorders. 1996;39(3):185–189. doi: 10.1016/0165-0327(96)00008-0. doi: 10.1016/0165-0327(96)00008-0. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry. 1987;150(6):782–786. doi: 10.1192/bjp.150.6.782. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Davis EM, Stange KC, Horwitz RI. Childbearing, stress and obesity disparities in women: a public health perspective. Matern Child Health J. 2012;16(1):109–118. doi: 10.1007/s10995-010-0712-6. doi: 10.1007/s10995-010-0712-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demissie Z, Siega-Riz AM, Evenson KR, Herring AH, Dole N, Gaynes BN. Journal of Women's Health. 2011;20(7):1025–1034. doi: 10.1089/jwh.2010.2091. doi:10.1089/jwh.2010.2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan SC, Duncan TE, Strycker LA. Alcohol use from ages 9 to 16: a cohort-sequential latent growth model. Drug Alcohol Depend. 2006;81:77–81. doi: 10.1016/j.drugalcdep.2005.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC. An introduction to latent growth curve modeling. Behavior Therapy. 2004;35(2):333–363. [Google Scholar]
- Eastwood JG, Phung H, Barnett B. Postnatal depression and socio-demographic risk: Factors asscoiated with Edinburgh Depression Scale scores in a metropolitan area of New South Wales, Australia. Australian and New Zealand Journal of Psychiatry. 2011;45:1010–1046. doi: 10.3109/00048674.2011.619160. [DOI] [PubMed] [Google Scholar]
- Edwards RC, Thullen MJ, Isarowong N, Shiu C, Henson L, Hans SL. Supportive relationships and the reajectory of depressive symptoms among young, African American Mothers. Journal of Family Psychology. 2012;26(4):585–594. doi: 10.1037/a0029053. [DOI] [PubMed] [Google Scholar]
- Ellsworth-Bowers ER, Corwin EJ. Nutrition and the psychoneuroimmunology of postpartum depression. Nutr Res Rev. 2013;25(1):180–192. doi: 10.1017/S0954422412000091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8(3):430–457. [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal Depression: A Systematic Review of Prevalence and Incidence. Obstetrics & Gynecology. 2005;106(5, Part 1):1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. 1010.1097/1001.AOG.0000183597.0000131630.db. [DOI] [PubMed] [Google Scholar]
- Gunderson EP. Childbearing and obesity in women: weight before, during, and after pregnancy. Obstet Gynecol Clin North Am. 2009;36(2):317–332. ix. doi: 10.1016/j.ogc.2009.04.001. doi: 10.1016/j.ogc.2009.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz JA, Goodman J. A Longitudinal Study of Maternal Postpartum Depression Symptoms. Research and Theory for Nursing Practice. 2004;18(2-3):149–163. doi: 10.1891/rtnp.18.2.149.61285. doi: 10.1891/rtnp.18.2.149.61285. [DOI] [PubMed] [Google Scholar]
- Horowitz JA, Goodman JH. Identifying and Treating Postpartum Depression. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2005;34(2):264–273. doi: 10.1177/0884217505274583. doi: 10.1177/0884217505274583. [DOI] [PubMed] [Google Scholar]
- LaCoursiere D, Baksh L, Bloebaum L, Varner M. Maternal Body Mass Index and Self-Reported Postpartum Depressive Symptoms. Maternal and Child Health Journal. 2006;10(4):385–390. doi: 10.1007/s10995-006-0075-1. doi: 10.1007/s10995-006-0075-1. [DOI] [PubMed] [Google Scholar]
- LaCoursiere DY, Barrett-Connor E, O'Hara MW, Hutton A, Varner MW. The association between prepregnancy obesity and screening positive for postpartum depression. BJOG: An International Journal of Obstetrics & Gynaecology. 2010;117(8):1011–1018. doi: 10.1111/j.1471-0528.2010.02569.x. doi: 10.1111/j.1471-0528.2010.02569.x. [DOI] [PubMed] [Google Scholar]
- Liu CH, Tronick E. Re-concepturalising prenatal life stressors in predicting post-partum depression: Cumulative-, specific-, and domain-specific approaches to calculating risk. Paediatric and Perinatal Epidemiology. 2013;27:481–490. doi: 10.1111/ppe.12072. [DOI] [PubMed] [Google Scholar]
- Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: A meta-analysis. Am J epidemiol. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Luoma L, Tamminen T, Kaukonen P, Laippala P, Puura K, Salmelin R, Almqvist F. Logitudinal study of maternal depressive symptoms and child well-being. Journal of American Academy of Child and Adolescent Psychiatry. 2001;40(12):1367–1374. doi: 10.1097/00004583-200112000-00006. [DOI] [PubMed] [Google Scholar]
- Mayberry LJ, Horowitz JA, Declercq E. Depression Symptom Prevalence and Demographic Risk Factors Among U.S. Women During the First 2 Years Postpartum. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2007;36(6):542–549. doi: 10.1111/j.1552-6909.2007.00191.x. doi: 10.1111/j.1552-6909.2007.00191.x. [DOI] [PubMed] [Google Scholar]
- Milgrom J, Skouteris H, Worotniuk T, Henwood A, Bruce L. The association between ante- and postnatal depressive symptoms and obesity in both mother and child: a systematic review of the literature. Womens Health Issues. 2012;22(3):e319–328. doi: 10.1016/j.whi.2011.12.001. doi: 10.1016/j.whi.2011.12.001. [DOI] [PubMed] [Google Scholar]
- Mora PA, Bennett LM, Elo IT, Mathew L, Coyne JC, Culhane JF. Distinct trajectories of perinatal depressive symptomatology: Evidence from growth mixture modeling. Am J Epidemiol. 2009;169:24–32. doi: 10.1093/aje/kwn283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray L, Carothers AD. The validation of the Edinburgh Post-natal Depression Scale on a community sample. The British Journal of Psychiatry. 1990;157(2):288–290. doi: 10.1192/bjp.157.2.288. doi: 10.1192/bjp.157.2.288. [DOI] [PubMed] [Google Scholar]
- Muthén B, Muthén LK. Integrating person centered and variable centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism: clinical and experimental research. 2000;24(6):882–891. doi: 10.1111/j.1530-0277.2000.tb02070.x. [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide. Muthén & Muthén; Los Angeles, CA: 1998-2006. [Google Scholar]
- Ng RC, Hirata CK, Yeung W, Haller E, Finley PR. Pharmacologic Treatment for Postpartum Depression: A Systematic Review. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 2010;30(9):928–941. doi: 10.1592/phco.30.9.928. doi: 10.1592/phco.30.9.928. [DOI] [PubMed] [Google Scholar]
- O'hara MW, Swain AM. Rates and risk of postpartum depression—a meta-analysis. International Review of Psychiatry. 1996;8(1):37–54. doi: doi:10.3109/09540269609037816. [Google Scholar]
- Østbye T, Krause KM, Brouwer RJ, Lovelady CA, Morey MC, Bastian LA, McBride CM. Active Mothers Postpartum (AMP): rationale, design, and baseline characteristics. Journal of women's health (2002) 2008;17(10):1567–1575. doi: 10.1089/jwh.2007.0674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Østbye T, Zucker NL, Krause KM, Lovelady CA, Evenson KR, Peterson BL, Brouwer RJN. Kids and Adults Now! Defeat Obesity (KAN-DO): Rationale, design and baseline characteristics. Contemporary Clinical Trials. 2011;32(3):461–469. doi: 10.1016/j.cct.2011.01.017. doi: 10.1016/j.cct.2011.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Wichman AL, MacCallum RC, Briggs NE. Latent growth curve modeling. Sage Publications; Thousand Oaks, CA: 2008. [Google Scholar]
- Ramos-Marcuse F, Oberlander SE, Papas MA, McNary SW, Hurley KM, Black MM. Stability of maternal depressive symptoms among urban, low-income, African American adolescent mothers. J. Affect. Disord. 2010;122(1-2):68–75. doi: 10.1016/j.jad.2009.06.018. [DOI] [PubMed] [Google Scholar]
- Reay R, Fisher Y, Robertson M, Adams E, Owen C. Group interpersonal psychotherapy for postnatal depression: a pilot study. Archives of Women's Mental Health. 2006;9(1):31–39. doi: 10.1007/s00737-005-0104-x. doi: 10.1007/s00737-005-0104-x. [DOI] [PubMed] [Google Scholar]
- Reck C, Stehle E, Reinig K, Mundt C. Maternity blues as a predictor of DSM-IV depression and anxiety disorders in the first three months postpartum. Journal of Affective Disorders. 2009;113(1–2):77–87. doi: 10.1016/j.jad.2008.05.003. doi: 10.1016/j.jad.2008.05.003. [DOI] [PubMed] [Google Scholar]
- Schwarz G. Estimating Dimension of a Model. Annals of Statistics. 1978;6(2):461–464. [Google Scholar]
- Small R, Brown S, Lumley J, Astbury J. Missing voices: What women say and do about depression after childbirth. Journal of Reproductive and Infant Psychology. 1994;12(2):89–103. doi: 10.1080/02646839408408872. [Google Scholar]
- Sutter-Dallay AL, Cosnefroy O, Glatigny-Dallay E, Verdoux H, Rascle N. Evolution of perinatal depressive symptoms from pregnancy to two years postpartum in a low-risk sample: the MATQUID cohort. J Affect Disord. 2012;139(1):23–29. doi: 10.1016/j.jad.2011.08.018. doi: 10.1016/j.jad.2011.08.018. [DOI] [PubMed] [Google Scholar]
- Teychenne M, York R. Physical activity, sedentary behavior, and postnatal depression symptoms-a review. American Journal of Preventive Medicine. 2013;45(2):217–227. doi: 10.1016/j.amepre.2013.04.004. [DOI] [PubMed] [Google Scholar]
- Vernon MM, Young-Hyman D, Looney SW. Maternal stress, physical activity, and body mass index during new mothers' first year postpartum. Women Health. 2010;50(6):544–562. doi: 10.1080/03630242.2010.516692. doi: 10.1080/03630242.2010.516692. [DOI] [PubMed] [Google Scholar]
- Wu YP, Selig JP, Roberts MC, Steele RG. Trajectories of postpartum maternal depressive symptoms and children's social skills. J Child Fam Study. 2011;20:414–423. [Google Scholar]
- Xie R-H, He G, Koszycki D, Walker M, Wen SW. Prenatal Social Support, Postnatal Social Support, and Postpartum Depression. Annals of Epidemiology. 2009;19(9):637–643. doi: 10.1016/j.annepidem.2009.03.008. doi: http://dx.doi.org/10.1016/j.annepidem.2009.03.008. [DOI] [PubMed] [Google Scholar]