Abstract
Despite the notion that monozygotic (identical) twins share 100% identical genetic information, genetic differences among monozygotic twin pairs do occur and can be explained by mechanisms occurring during post-zygotic events. Despite such twins being fundamentally “identical”, these post-zygotic genetic changes may give rise to phenotypic differences and genetic diseases. Consequently, studies of monozygotic twin pairs discordant for specific genetic diseases represent an important tool for the identification of disease genes. We used array comparative genomic hybridization (aCGH) and methylation arrays to search for genetic and epigenetic differences in blood drawn from four monozygotic twin pairs discordant for testicular germ cell tumors. No consistent differences were identified. A larger twin study would be required to achieve confident discovery of very subtle differences between monozygotic twins discordant for testicular germ cell tumors.
Keywords: Testicular germ cell tumor, twin study, epigenetics, familial cancer, array CGH, methylation
Testicular germ cell tumors (TGCT) are the most common malignancies occurring in young, white men. Epidemiologic studies demonstrate a rising incidence of TGCT during the last several decades, and implicate unknown environmental factors in the etiology of this neoplasm [1]. However, the observation that TGCT has a tendency to cluster in families (with very high TGCT relative risks among sons of affected fathers and brothers of affected sibs) and the discovery through genomewide association studies (GWAS) of comparatively strong TGCT risk variants in or near an increasing number of genes (including KITLG, BAK1, SPRY4, TERT, ATF7IP, and DMRT1) has now shown that TGCT is truly, in part, due to genetic factors. The prevailing hypothesis is that the combined effect of multiple common, low-penetrance genetic variants forms the heritable substrate for testicular cancer. To date, there are 30 published variants in 18 genomic regions which have achieved GWAS levels of statistical significance [2-9], and two candidate genes (AFCz gr/gr; PDE11A) which have been implicated in TGCT susceptibility [10,11]. Cumulatively, the GWAS risk alleles published to date account for ~15% of the excess familial risk to brothers of men with TGCT and ~22% of the excess familial risk to sons of men with TGCT [9]. Thus, a significant fraction of TGCT’s genetic susceptibility remains undiscovered, and additional gene discovery efforts are warranted.
Monozygotic (identical) twins discordant for TGCT offer the possibility of identifying post-zygotic genetic or epigenetic differences that may explain disease discordance [12]. Much of the literature related to monozygotic twins who are discordant for specific diseases pre-dates the availability of current genomic technologies. Nonetheless, this research strategy is now being productively applied in the neuropsychiatry domain [14-16], autoimmune disease [17-19], and cancer or inherited cancer susceptibility disorders [20-25]. In some instances, relatively small sample sizes have permitted important observations. Here we report on the genomic analysis of four identical twin pairs discordant for TGCT.
Seven hundred twenty-four subjects from 147 multiple-case families were enrolled in the NCI Clinical Genetics Branch Familial Testicular Germ Cell Tumor Study (NCI Protocol 02-C-0178; NCT-00039598) after recruitment/ascertainment through physician and self-referral. We confirmed the cancer diagnoses by reviewing medical records, pathology reports, and/or stored histological material. Written informed consent was obtained from all participants, and the study was approved by NCI’s institutional review board [13]. Aliquots of frozen whole blood from the twin pairs underwent DNA extraction using the Autogen™ system (Holliston, MA), with an added RNase A step in preparation for the array comparative genomic hybridization (aCGH).
aCGH was employed to adjudicate any possible gains or losses within the chromosomal struture of the respective twin pairs that could be linked to tumor development. Purified DNA samples were tested on Agilent SurePrint G3™ Human CGH microarrays, 4x180K, following the manufacturer’s recommendations. Data were analyzed using Nexus software (BioDis-covery™, Hawthorne, CA).
DNA methylation profiling utilized the Illumina HumanMethylation450 BeadChip Kit™ (Illu-mina, Inc., San Diego, CA), and used the manufacturer’s instructions. Liquid handling robotics (Tecan Group Ltd., Männedorf, Switzerland) allowed the testing in a batch format with other specimens. Data were processed and analyzed using R software with the Pattern Match™ program to look for methyation patterns specific to the DNA of the cancer patients. Pairwise Student t-tests were performed using M values (assuming a normal data distribution) converted from beta values in Partek™ (Partek Inc., Saint Louis, MO).
For both CGH and methylation datasets, only minimal differences between each sibling pair were observed. Nexus quality score ranges for aCGH were acceptable (0.14 - 0.18) for all samples. Scatter plots showed no gross abnormalities in any of the samples (Figure 1). Even though minor aCGH differences did exist (Figure 1), there were no consistent, focal gains or losses of chromosomal segments among all four twin pairs.
Figure 1.
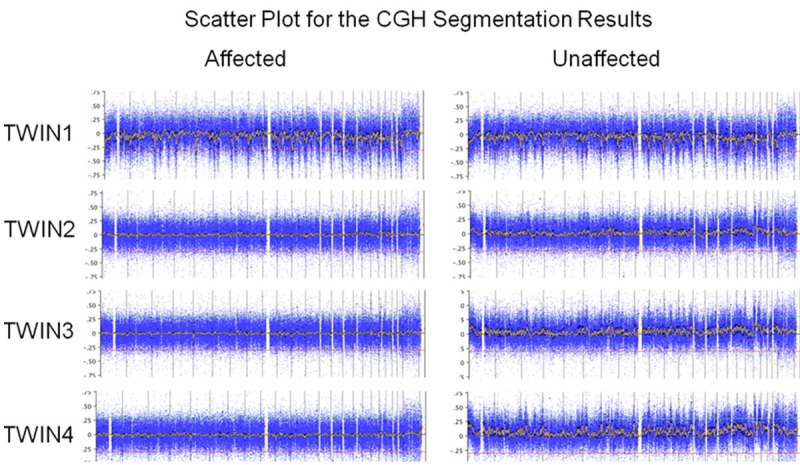
Comparison of the affected and unaffected twins shows no obvious differences in segmentation.
The methylation data as analyzed by R showed that, when looking for differential methylation between the affected and unaffected twin pairs, no significant adjusted p-values for pairwise t-tests were identified in any of the four twin sets. All the targets with p < 0.05 had very small beta value differences (-0.02 to 0.02). Accounting for the false discovery rate due to multiple statistical comparisons, none of the adjusted p-value were statistically significant. These data suggest that there were no reproducible methylation targets that were associated with the prescence of TGCT in our subjects. Many of the differences between twin pairs probably arose from stochastic noise in the assays. These results were confirmed by manual inspection of the data in genome browsers.
We considered two hypotheses in our data analysis: (1) there might be a single aberration shared among all four affected pairs to account for the occurence of TGCT; or (2) both twins of a pair might have a predisposing aberration that require a second hit to create the cancer. However, no evidence to support either hypothesis was found. Our analysis was complicated by observing that all detected CNVs were in known CNV regions, thus reducing the likelihood that any of these aberrations were biologically signifigant. A much larger twin study will be required to achieve confident discovery of very subtle but statistically significant differences between affected and unaffected twins. We present this report of our initial experience with this novel gene discovery strategy to remind investigators of the potential value inherent in this study design now that we have at our disposal a wide array of genomic technologies which can help tease apart these subtle differences. Finally, we hope that this report might stimulate referral of additional TGCT discordant identical twin pairs as the basis for an expanded analysis, which we are eager to pursue.
Acknowledgements
We express our gratitude to Miia Suuriniemi and Holly Stevenson for performing the aCGH and methylation assays, respectively, and to Janet Bracci and Jennifer Restrepo, for their support of this clinical research protocol. This study was supported by funding from the Intramural Research Program of the US National Cancer Institute, and through a support services contract with Westat Inc. (HHSN261200655004C). We are also deeply grateful to the participants in our clinical research protocol, without whom none of this work would have been possible. The research performed by Drs. Kratz, Edelman, Wang, Melter and Greene was supported by the Intramural Research Program of the US National Cancer Institute.
Disclosure of conflict of interest
None to declare.
References
- 1.McGlynn KA, Trabert B. Adolescent and adult risk factors for testicular cancer. Nat Rev Urol. 2012;9:339–349. doi: 10.1038/nrurol.2012.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rapley EA, Turnbull C, Al Olama AA, Dermitzakis ET, Linger R, Huddart RA, Renwick A, Hughes D, Hines S, Seal S, Morrison J, Nsengimana J, Deloukas P UK Testicular Cancer Collaboration. Rahman N, Bishop DT, Easton DF, Stratton MR. A genome-wide association study of testicular germ cell tumor. Nat Genet. 2009;41:807–810. doi: 10.1038/ng.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kanetsky PA, Mitra N, Vardhanabhuti S, Li M, Vaughn DJ, Letrero R, Ciosek SL, Doody DR, Smith LM, Weaver J, Albano A, Chen C, Starr JR, Rader DJ, Godwin AK, Reilly MP, Hakonarson H, Schwartz SM, Nathanson KL. Common variation in KITLG and at 5q31.3 predisposes to testicular germ cell cancer. Nat Genet. 2009;41:811–815. doi: 10.1038/ng.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turnbull C, Rapley EA, Seal S, Pernet D, Renwick A, Hughes D, Ricketts M, Linger R, Nsengimana J, Deloukas P, Huddart RA, Bishop DT, Easton DF, Stratton MR, Rahman N UK Testicular Cancer Collaboration. Variants near DMRT1, TERT and ATF7IP are associated with testicular germ cell cancer. Nat Genet. 2010;42:604–607. doi: 10.1038/ng.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kanetsky PA, Mitra N, Vardhanabhuti S, Vaughn DJ, Li M, Ciosek SL, Letrero R, D'Andrea K, Vaddi M, Doody DR, Weaver J, Chen C, Starr JR, Håkonarson H, Rader DJ, Godwin AK, Reilly MP, Schwartz SM, Nathanson KL. A second independent locus within DMRT1 is associated with testicular germ cell tumor susceptibility. Hum Mol Genet. 2011;20:3109–17. doi: 10.1093/hmg/ddr207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kratz CP, Han SS, Rosenberg PS, Berndt SI, Burdett L, Yeager M, Korde LA, Mai PL, Pfeiffer R, Greene MH. Variants in or near KITLG, BAK1, DMRT1, and TERT-CLPTM1L predispose to familial testicular germ cell tumour. J Med Genet. 2011;48:473–476. doi: 10.1136/jmedgenet-2011-100001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schumacher FR, Wang Z, Skotheim RI, Koster R, Chung CC, Hildebrandt MA, Kratz CP, Bakken AC, Bishop DT, Cook MB, Erickson RL, Fosså SD, Greene MH, Jacobs KB, Kanetsky PA, Kolonel LN, Loud JT, Korde LA, Le Marchand L, Lewinger JP, Lothe RA, Pike MC, Rahman N, Rubertone MV, Schwartz SM, Siegmund KD, Skinner EC, Turnbull C, Van Den Berg DJ, Wu X, Yeager M, Nathanson KL, Chanock SJ, Cortessis VK, McGlynn KA. Testicular germ cell tumor susceptibility associated with the UCK2 locus on chromosome 1q23. Hum Mol Genet. 2013;22:2748–53. doi: 10.1093/hmg/ddt109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chung CC, Kanetsky PA, Wang Z, Hildebrandt MA, Koster R, Skotheim RI, Kratz CP, Turnbull C, Cortessis VK, Bakken AC, Bishop DT, Cook MB, Erickson RL, Fosså SD, Jacobs KB, Korde LA, Kraggerud SM, Lothe RA, Loud JT, Rahman N, Skinner EC, Thomas DC, Wu X, Yeager M, Schumacher FR, Greene MH, Schwartz SM, McGlynn KA, Chanock SJ, Nathanson KL. Meta-analysis identifies four new loci for testicular germ cell tumor. Nat Genet. 2013;45:680–685. doi: 10.1038/ng.2634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ruark E, Seal S, McDonald H, Zhang F, Elliot A, Lau K, Perdeaux E, Rapley E, Eeles R, Peto J, Kote-Jarai Z, Muir K, Nsengimana J, Shipley J UK Testicular Cancer Collaboration (UKTCC) Bishop DT, Stratton MR, Easton DF, Huddart RA, Rahman N, Turnbull C. Identification of nine new susceptibility loci for testicular cancer, including variants near DAZL and PRDM14. Nat Genet. 2013;45:686–689. doi: 10.1038/ng.2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nathanson KL, Kanetsky PA, Hawes R, Vaughn DJ, Letrero R, Tucker K, Friedlander M, Phillips KA, Hogg D, Jewett MA, Lohynska R, Daugaard G, Richard S, Chompret A, Bonaïti-Pellié C, Heidenreich A, Olah E, Geczi L, Bodrogi I, Ormiston WJ, Daly PA, Oosterhuis JW, Gillis AJ, Looijenga LH, Guilford P, Fosså SD, Heimdal K, Tjulandin SA, Liubchenko L, Stoll H, Weber W, Rudd M, Huddart R, Crockford GP, Forman D, Oliver DT, Einhorn L, Weber BL, Kramer J, McMaster M, Greene MH, Pike M, Cortessis V, Chen C, Schwartz SM, Bishop DT, Easton DF, Stratton MR, Rapley EA. The Y deletion gr/gr and susceptibility to testicular germ cell tumor. Am J Hum Genet. 2005;77:1034–1043. doi: 10.1086/498455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horvath A, Korde L, Greene MH, Libe R, Osorio P, Faucz FR, Raffin-Sanson ML, Tsang KM, Drori-Herishanu L, Patronas Y, Remmers EF, Nikita ME, Moran J, Greene J, Nesterova M, Merino M, Bertherat J, Stratakis CA. Functional phosphodiesterase 11A mutations may modify the risk of familial and bilateral testicular germ cell tumors. Cancer Res. 2009;69:5301–5306. doi: 10.1158/0008-5472.CAN-09-0884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zwijnenburg PJ, Meijers-Heijboer H, Boomsma DI. Identical but not the same: the value of discordant monozygotic twins in genetic research. Am J Med Genet Part B. 2010;153B:1134–1149. doi: 10.1002/ajmg.b.31091. [DOI] [PubMed] [Google Scholar]
- 13.Greene MH, Kratz CP, Mai PL, Mueller C, Peters JA, Bratslavsky G, Ling A, Choyke PM, Premkumar A, Bracci J, Watkins RJ, McMaster ML, Korde LA. Familial testicular germ cell tumors in adults: 2010 summary of genetic risk factors and clinical phenotype. Endocr Relat Cancer. 2010;17:R109–R121. doi: 10.1677/ERC-09-0254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dempster EL, Wong CC, Lester KJ, Burrage J, Gregory AM, Mill J, Eley TC. Genome-wide Methylomic Analysis of Monozygotic Twins Discordant for Adolescent Depression. Biol Psychiatry. 2014 doi: 10.1016/j.biopsych.2014.04.013. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong CC, Meaburn EL, Ronald A, Price TS, Jeffries AR, Schalkwyk LC, Plomin R, Mill J. Methylomic analysis of monozygotic twins discordant for autism spectrum disorder and related behavioural traits. Mol Psychiatry. 2014;19:495–503. doi: 10.1038/mp.2013.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Castellani CA, Awamleh Z, Melka MG, O'Reilly RL, Singh SM. Copy number variation distribution in six monozygotic twin pairs discordant for schizophrenia. Twin Res Hum Genet. 2014;17:108–120. doi: 10.1017/thg.2014.6. [DOI] [PubMed] [Google Scholar]
- 17.Stefan M, Zhang W, Concepcion E, Yi Z, Tomer Y. DNA methylation profiles in type 1 diabetes twins point to strong epigenetic effects on etiology. J Autoimmun. 2014;50:33–7. doi: 10.1016/j.jaut.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Selmi C, Cavaciocchi F, Lleo A, Cheroni C, De Francesco R, Lombardi SA, De Santis M, Meda F, Raimondo MG, Crotti C, Folci M, Zammataro L, Mayo MJ, Bach N, Shimoda S, Gordon SC, Miozzo M, Invernizzi P, Podda M, Scavelli R, Martin MR, Lasalle JM, Gershwin ME. Genome-wide analysis of DNA methylation, copy number variation, and gene expression in monozygotic twins discordant for primary biliary cirrhosis. Front Immunol. 2014;5:128. doi: 10.3389/fimmu.2014.00128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Selmi C, Feghali-Bostwick CA, Lleo A, Lombardi SA, De Santis M, Cavaciocchi F, Zammataro L, Mitchell MM, Lasalle JM, Medsger T Jr, Gershwin ME. X chromosome gene methylation in peripheral lymphocytes from monozygotic twins discordant for scleroderma. Clin Exp Immunol. 2012;169:253–262. doi: 10.1111/j.1365-2249.2012.04621.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bateman CM, Alpar D, Ford AM, Colman SM, Wren D, Morgan M, Kearney L, Greaves M. Evolutionary trajectories of hyperdiploid ALL in monozygotic twins. Leukemia. 2014 doi: 10.1038/leu.2014.177. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21.Cazzaniga G, van Delft FW, Lo Nigro L, Ford AM, Score J, Iacobucci I, Mirabile E, Taj M, Colman SM, Biondi A, Greaves M. Developmental origins and impact of BCR-ABL1 fusion and IKZF1 deletions in monozygotic twins with Ph+ acute lymphoblastic leukemia. Blood. 2011;118:5559–5564. doi: 10.1182/blood-2011-07-366542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bateman CM, Colman SM, Chaplin T, Young BD, Eden TO, Bhakta M, Gratias EJ, van Wering ER, Cazzaniga G, Harrison CJ, Hain R, Ancliff P, Ford AM, Kearney L, Greaves M. Acquisition of genome-wide copy number alterations in monozygotic twins with acute lymphoblastic leukemia. Blood. 2010;115:3553–3558. doi: 10.1182/blood-2009-10-251413. [DOI] [PubMed] [Google Scholar]
- 23.Vogt J, Kohlhase J, Morlot S, Kluwe L, Mautner VF, Cooper DN, Kehrer-Sawatzki H. Monozygotic twins discordant for neurofibromatosis type 1 due to a postzygotic NF1 gene mutation. Hum Mutat. 2011;32:E2134–E2147. doi: 10.1002/humu.21476. [DOI] [PubMed] [Google Scholar]
- 24.Kaplan L, Foster R, Shen Y, Parry DM, McMaster ML, O'Leary MC, Gusella JF. Monozygotic twins discordant for neurofibromatosis 1. Am J Med Genet A. 2010;152A:601–606. doi: 10.1002/ajmg.a.33271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Galetzka D, Hansmann T, El Hajj N, Weis E, Irmscher B, Ludwig M, Schneider-Rätzke B, Kohlschmidt N, Beyer V, Bartsch O, Zechner U, Spix C, Haaf T. Monozygotic twins discordant for constitutive BRCA1 promoter methylation, childhood cancer and secondary cancer. Epigenetics. 2012;7:47–54. doi: 10.4161/epi.7.1.18814. [DOI] [PMC free article] [PubMed] [Google Scholar]


