Abstract
Background
The explicit use of race in medical decision-making is contested. Researchers have hypothesized that physicians use race in care when they are uncertain.
Objectives
To investigate whether physician anxiety due to uncertainty is associated with a higher propensity to use race in medical decision-making.
Research Design
A national cross-sectional survey of general internists
Subjects
A national sample of 1738 clinically active general internists drawn from the SK&A physician database
Measures
Anxiety Due to Uncertainty (ADU) is a 5-item measure of emotional reactions to clinical uncertainty. Bonham and Sellers Racial Attributes in Clinical Evaluation (RACE) scale includes 7 items that measure self-reported use of race in medical decision-making. We used bivariate regression to test for associations between physician characteristics, ADU and RACE. Multivariate linear regression was performed to test for associations between ADU and RACE while adjusting for potential confounders.
Results
The mean score on ADU was 19.9 (SD=5.6). Mean score on RACE was 13.5 (SD=5.6). After adjusting for physician demographics, physicians with higher levels of ADU scored higher on RACE (+β=0.08 in RACE, p=0.04, for each 1-point increase in ADU), as did physicians who understand “race” to mean biological or genetic ancestral, rather than sociocultural, group. Physicians who graduated from a US medical school, completed fellowship, and had more white patients, scored lower on RACE.
Conclusions
This study demonstrates positive associations between physicians’ anxiety due to uncertainty, meanings attributed to race, and self-reported use of race in medical decision-making. Future research should examine the potential impact of these associations on patient outcomes and healthcare disparities.
Keywords: Medical Decision-Making, Race & Ethnicity, Uncertainty
Introduction
The appropriate use of race in medical decision-making remains contested, in part because of the disagreement over the clinical utility of race (1–4). Some believe that ignoring race is detrimental to understanding differences in risk-factor profiles, disease prevalence and severity. They contend that race correlates with a person’s genetic ancestry which may facilitate testing, diagnosis, and treatment (5). Others do not view race as a useful categorization of genetic or biological information about the response to drugs, diagnosis, or causes of disease (6). Some researchers contend that racial group health differences are not based upon biological or genetic differences, but that members of racial minority groups may develop worse health from recurrent encounters with racism that lead to greater activation of the physiological stress response (7, 8). Others have more recently suggested that racism can lead to epigenetic changes, which may be passed down across generations (9).
Given the diversity of perspectives, researchers have begun to investigate how physicians use race in their medical decision-making (10). When probed, physicians express uncertainty about how and whether race should be used in medical decision-making (11, 12). Some clinical guidelines make recommendations by race (e.g., hypertension treatment) (13–15); however, recommendations regarding race often vary across guidelines for the same condition (e.g., prostate and colorectal cancer screening guidelines (14–17)). Additionally, race is often factored into the results of medical tests (e.g., glomerular filtration rate, lung function). Studies have found that providers frequently employ race in their decision-making, even in the midst of ambiguity regarding what race measures (18).
Uncertainty is common in medicine. It may be due to ambiguous patient presentations, multiple diagnoses and treatment possibilities, variation in treatment efficacy across individuals, and poor communication between doctors and patients (19–21). Some of these scenarios are more common when physicians treat patients whose backgrounds differ from their own background. Individuals from different cultural backgrounds convey and interpret symptoms differently. Additionally, there is considerable evidence that racial and ethnic minorities experience poorer communication with physicians than white patients, particularly in racially discordant doctor-patient relationships (22–25). Patients from minority groups may be less likely to trust physicians and confide in them (26–28), and studies show that among socially marginalized patients, physicians have lower levels of trust in minorities than in whites (29).
Anxiety due to uncertainty is associated with physician characteristics, such as gender, clinical experience, and specialty (30, 31). It also affects physician behaviors, such as test ordering (32, 33). Cognitive psychology suggests that stress, anxiety, and uncertainty activate implicit biases and stereotyping (34, 35). Uncertainty may also be associated with explicit or deliberate use of race. For example, in the face of an uncertain patient presentation, physicians may draw on data collected at the population level and “statistically discriminate.” i.e., uncritically apply population data to individuals (36, 37). If physician uncertainty is higher in visits of racial/ethnic minority patients, and reactions to uncertainty, such as anxiety, systematically lead to different physician behaviors and choices (38, 39), we might expect to see different treatment for patients from different racial backgrounds (21, 40).
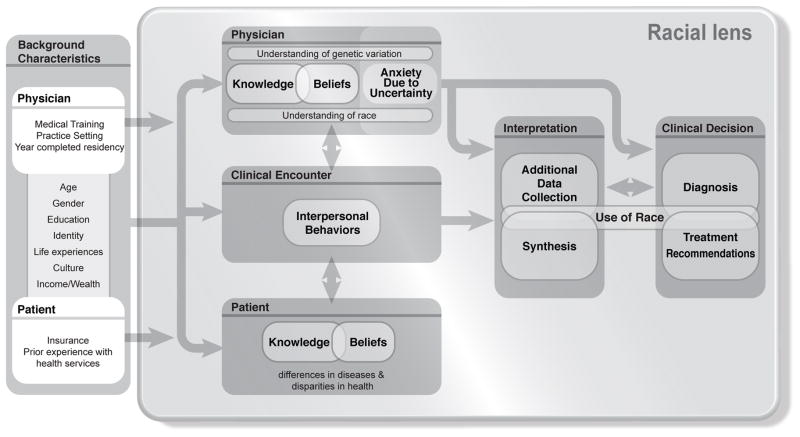
In this study, we investigate the association between anxiety due to uncertainty and self-reported use of race in medical decision-making. The study is part of the Physicians Understanding of Human Genetic Variation (PUHGV) study which examines the relationship between race and genetics in medical decision making (41). We have modified the conceptual model from the parent study (Figure 1) to show the hypothesized relationship between physicians’ anxiety due to uncertainty (ADU) and medical decision-making
Figure 1.
Conceptual Model
Methods
Study Design and Setting
As part of the PUGHV study, the “Health Professionals Genetics Education Needs Exploration Survey” (HP GENE) was developed through focus groups, cognitive interviews, and pilot testing (41). From April–December 2010, the HP GENE survey was administered via the web and mail to a national sample of 2122 clinically active general internists. The sample was drawn from the SK&A AMA Masterfile physician database in 2 batches. First, a general random sample (n=1929) was selected from the overall database. This was supplemented by a sample of physicians who graduated from historically black medical schools (n=193) in an effort to increase the representation of black physicians in the overall sample and improve the study’s ability to detect differences between black and white physicians. We excluded physicians who were not currently practicing general internists according to their office staff or did not have a current United States (U.S.) mail address, and identified a sample size of 1,738 eligible physicians. The institutional review boards at the National Human Genome Research Institute, Johns Hopkins University, and Miami University of Ohio approved the survey.
Measurements
Anxiety Due to Uncertainty
Our main predictor variable is anxiety due to uncertainty. The Anxiety due to Uncertainty scale quantifies emotional reactions to conditions of clinical practice and has been shown to be highly valid and reliable in similar populations (30, 31). The 5 items are: 1) The uncertainty of patient care often troubles me; 2) I find the uncertainty involved in patient care disconcerting; 3) I usually feel anxious when I am not sure of the diagnosis; 4) Uncertainty in patient care makes me uneasy; and 5) I am quite comfortable with the uncertainty in patient care. Each item is rated on a 6-point Likert scale from 0=strongly disagree to 5=strongly agree. The last item is reverse coded for consistency. The individual items are summed for an overall score with higher scores indicating higher anxiety due to uncertainty.
Use of Race in Medical Decision-Making
Our main outcome variable was use of race in medical decision-making. We measured self-reported use of race with the Bonham and Sellers Racial Attributes in Clinical Evaluation (RACE) scale. This scale consists of 7 items which load on a single factor and have high internal consistency (Cronbach’s α=0.86) (41). The items are: 1) I consider information from patients about their racial background; 2) I consider my patients’ race to better understand their genetic predisposition; 3) I consider my patients’ race when making decisions about which medications to prescribe; 4) I consider my patients’ race in determining genetic risk for common, complex diseases (e.g., kidney disease or diabetes); 5) I consider my patients’ race in making medication dosage decisions; 6) I consider my patients’ race when determining age of initiation of screening for certain diseases; and 7) I consider my patients’ race in determining how aggressively to treat particular diseases. Each item is rated on a 5-point Likert scale, from 0=none of the time and 4=all of the time. The 7 items are summed to produce an overall score with higher scores reflecting greater use of race in medical decision-making.
Covariates of interest
The survey collected demographic information (e.g., age, race, gender), as well as information about nativity, location of medical school, genetics coursework, fellowship training, years in practice post-residency, current level of clinical work, and the estimated racial composition of each physician’s patient panel. Respondents were also asked “What does the term ‘race’ mean to you?” and instructed to choose 1 item that best represents the term from 10 choices: 1) biological group; 2) cultural group; 3) genetic ancestral group; 4) lifestyle/behavioral group; 5) population group; 6) religious group; 7) social identity group; 8) species; 9) none of the above; or 10) other. These responses were grouped into biological group (responses 1 and 8), genetic ancestral group (response 3), sociocultural group (responses 2,4,5,6, and 7), and none of above/other (responses 9 and 10), hereafter referred to as physicians’ meaning of race.
Statistical Analysis
We used bivariate linear regression to determine whether physicians’ demographic characteristics, practice experience, and meaning of race were associated with anxiety due to uncertainty (ADU). We also used bivariate regression to determine whether physician characteristics, practice experience, and meaning of race were associated with scores on the RACE scale. Finally, we examined the association of anxiety due to uncertainty with RACE, adjusting for potential confounders (variables associated with either ADU or the RACE scale with p-values <0.10 in unadjusted analyses). For those variables that were collinear (e.g. age and years in practice), we included only the variable with the larger unadjusted coefficient in the multivariate regression models. Analyses were performed using SAS enterprise version 5.1.
Results
Among the 1738 eligible physicians, 787 completed the survey for a response rate of 45%. There were no statistically significant differences between respondents and non-respondents with regard to age or gender. We could not compare the racial composition of responders and non-responders because the SK& A physician database vendor used graduation from a historically black medical school as a proxy for race, and this method was found to be unreliable.
Table 1 shows characteristics of the sample. The mean age of respondents was 49 years. The majority of physicians were male, white, born in the United States, and had graduated from a U.S. medical school. The method used to oversample black physicians was not successful; only 6% of the sample was African-American. While 89% of U.S. medical graduates (USMGs) were born in the U.S., only 13% of international medical graduates (IMGs) were born in the U.S. Compared to their white colleagues, a higher proportion of physicians from all minority groups were foreign born; they also had significantly fewer years in clinical practice (5–6 years less) and cared for more non-white patients (Data not shown). Eighty-seven percent of respondents identified their specialty as general internal medicine. This rose to 94% when those who identified themselves as hospitalists were included as generalists. Respondents spent greater than 85% of their time in clinical practice and had patient panels that were predominantly white. Most physicians considered races to be genetic ancestral groups (61.6%). Far fewer physicians thought races were biological groups (20%) or sociocultural groups (16.1%).
Table 1.
Characteristics of Physician Respondents, HPGENE Survey
| Characteristic | (N=787) |
|---|---|
| Mean Age, years (SD) | 48.6 (9.7) |
| Male,% | 65.3 |
| Race, % | |
| White | 65.5 |
| Black | 6.0 |
| Asian | 19.8 |
| Other | 8.7 |
| U.S. Born, % | 70.9 |
| U.S. Medical Graduate (USMG),% | 75.5 |
| Had Genetics Coursework in Med School, % | 76.0 |
| General Internist,% | 87.1 |
| Fellowship Trained, % | 10.6 |
| Mean Practice Experience, years (SD) | 16.9 (9.8) |
| Mean Number of Clinical Days/Week (SD) | 4.3 (0.97) |
| Mean % Non-white Patients in Panel (SD) | 37.9 (24.2) |
| Meaning of Race,% | |
| Genetic Ancestral Group | 61.6 |
| Biological Group | 20.0 |
| Sociocultural Group | 16.1 |
| None of Above/Other | 2.3 |
The mean score on the Anxiety Due to Uncertainty (ADU) scale was 19.9 (SD 5.6, median 20.0). The range of ADU was 5–30. In unadjusted analyses (Table 2), older age and more years in practice were associated with lower anxiety due to uncertainty; female gender, Asian race, being foreign born, being an IMG, and spending more days per week seeing patients were associated with higher ADU. Being African-American (versus White), having had genetics coursework, fellowship training, and percent of non-white patients in physician panels were not associated with anxiety due to uncertainty. Physicians who understood the term “race” to mean biological or genetic ancestral group did not score differently on ADU from those who understood race to mean a sociocultural group; however, the few physicians who chose none of the response choices or “other” to define race scored significantly lower on ADU.
Table 2.
Association of Physician Characteristics with Anxiety Due to Uncertainty (ADU)
| Characteristic | Unadjusted β1 | P-value |
|---|---|---|
| Age | −0.07 | 0.002 |
| Female vs. Male | 1.28 | 0.003 |
| Race vs. White | ||
| Black | 1.24 | 0.154 |
| Asian | 2.66 | <.0001 |
| Other | 0.76 | 0.300 |
| Foreign born vs. U.S. born | 2.20 | <.0001 |
| IMG vs. USMG | 2.88 | <.0001 |
| Genetics Coursework in Med School | 0.24 | 0.617 |
| No Fellowship vs. Any Fellowship | 0.15 | 0.823 |
| Years in Practice | −0.08 | <.001 |
| Clinical Days per Week | 0.59 | 0.005 |
| % Non-white Patients in Panel | 0.01 | 0.105 |
| Meaning of Race, vs. Sociocultural Group % | ||
| Biological Group | 0.20 | 0.769 |
| Genetic Ancestral Group | 0.32 | 0.579 |
| None of Above/Other | −3.44 | 0.016 |
β coefficient gives the change in ADU for every 1 unit increase (e.g., every additional year or day in practice) or between the indicated group and reference group (e.g., female vs. male)
The mean of the RACE scale was 13.5 (SD 5.6, median 13.0, range 0–28). In bivariate analyses, ADU was positively associated with the self-reported use of race in medical decision-making (B=0.14, p<0.001). Additionally, black or Asian race, being foreign born, being an IMG, the amount of time seeing patients per week, and having a higher percentage of non-white patients in one’s panel were positively associated with RACE (p<0.05). Physicians’ definitions of race were also associated with the RACE scale, such that those who understood race to mean biological or genetic ancestral groups used race more than those who understood races to mean sociocultural groups. Fellowship training was marginally associated with RACE (p<0.10); those who were not fellowship trained reported using race more than those with fellowship training. Age, gender, genetics coursework, and years in practice were not associated with RACE in bivariate analyses. (Data not shown)
After adjustment for potential confounders (Table 3), the association between anxiety due to uncertainty and use of race as measured by the RACE scale remained statistically significant. For every 1 point increase in ADU, the score on the RACE scale increased by 0.08. Variables significantly associated with more self-reported use of race in the multivariate model included being an IMG, not having done a fellowship, and the percent of non-white patients in physician’s panel. Understanding the term race to mean a biological or genetic ancestral group rather than a sociocultural group was also associated with greater use of race. The associations between years in medical practice and self-reported use of race was positive and of borderline statistical significance (p =0.063) in multivariate analyses. Gender, physician race, nativity, and the amount of time seeing patients each week were not associated with RACE after controlling for potential confounders. The overall R-squared for the model was 0.10.
Table 3.
Association of Physician Anxiety Due to Uncertainty and Other Characteristics with Use of Race in Medical Decision-Making (RACE)
| Characteristic | Adjusted β2 | P-value |
|---|---|---|
| Anxiety Due to Uncertainty | 0.08 | 0.039 |
| Age | --- | |
| Female vs. Male | 0.17 | 0.709 |
| Race vs. White | ||
| Black | 1.01 | 0.294 |
| Asian | 0.80 | 0.224 |
| Other | 0.06 | 0.943 |
| Foreign born vs. U.S. Born | 0.03 | 0.961 |
| IMG vs. USMG | 2.24 | 0.001 |
| Genetics Coursework in Med School | --- | |
| No Fellowship vs. Any Fellowship | 1.44 | 0.032 |
| Years in Practice | 0.04 | 0.063 |
| Clinical days per Week | 0.32 | 0.146 |
| % Non-white Patients | 0.03 | <.001 |
| Meaning of Race, vs. Sociocultural Group | ||
| Biological Group | 1.46 | 0.037 |
| Genetic Ancestral Group | 1.33 | 0.022 |
| None of Above/Other | 0.48 | 0.771 |
β coefficient gives the change in the RACE Score for every 1 unit increase (e.g., every additional point in ADU or percent of non-white patients) or between the indicated group and reference group (e.g., female vs. male).
Adjusted for anxiety due to uncertainty, gender, race, nativity, location of medical school, fellowship training, years in practice, clinical days per week, percent of nonwhite patients, and understanding of race --- Variable not included in the multivariate model
Discussion
To our knowledge, this is the first study to examine the association between physician anxiety due to uncertainty and use of race in medical decision-making. Using data from a national survey, we found that general internists with higher anxiety due to uncertainty report using race in medical decision-making at higher levels than those with lower anxiety due to uncertainty. We also found that internists who graduated from international medical schools (IMGs), were not fellowship trained, and had more non-white patients in their panels used race more than their counterparts who were U.S. medical graduates (USMGs), completed a fellowship, and had fewer non-white patients respectively. In addition, physicians who understood race to refer to a biological or genetic ancestral group used race more in decision-making than those who understood the term “race” to mean “sociocultural group.”
The cognitive psychology literature shows that under conditions of stress, individuals seek to preserve cognitive resources (34, 35). Physicians’ explicit or deliberate use of race may help to preserve cognitive resources under conditions of stress and anxiety. Although we found a relatively small effect of anxiety due to uncertainty on self-reported use of race, when one considers the number of patients seen by individual physicians over time, the effect of anxiety due to uncertainty on use of race may be amplified and contribute to differences in care between patient populations.
Because our survey did not collect performance metrics for physicians, we cannot determine whether the explicit use of race had any effect, positive or negative, on clinical outcomes, patient satisfaction, or health care disparities. Use of race in medical decision-making may benefit patients, particularly if race can efficiently and reliably convey useful information about a patient’s risk or response to treatment. The use of race is similar to the dilemma that physicians face whenever they seek to apply group-level data from research studies to individual patients. Use of race may also benefit patients if racial information can “sensitize” physicians to factors that may be relevant in a patient’s care and warrant further investigation. Culturally sensitive providers tend to be knowledgeable about differences between social groups, express humility and a lifelong commitment to self-evaluation, and refrain from assuming that any one patient represents a prototypical group member (42, 43).
The authors of the seminal Unequal Treatment report and others have hypothesized that uncertainty may contribute to health care disparities (21, 44). Although this study cannot test for such associations, it is important to cautiously highlight the potential links between anxiety due to uncertainty, the explicit use of race and undesirable outcomes. Many physicians seem to have low levels of explicit bias or prejudice (34, 45), and few mechanisms, beyond implicit bias, have been identified to explain how physicians may contribute to disparities. Race may be one of several patient characteristics on which physicians rely when they have more anxiety due to uncertainty. Studies suggest that family history and perceptions of patients’ psychosocial characteristics may be more important than race in physicians’ overall decision-making (46, 47). That said, physicians often assess members of minority groups less positively than whites on domains such as intelligence, social support, trustworthiness and adherence to medical advice (29, 47, 48). Further research is needed to refine our knowledge of how patient factors influence physician decision-making.
In addition to the lack of treatment and health outcome data, this study has several other limitations, including its cross-sectional design and use of self-reported measures that may be subject to social desirability bias. We also cannot tell which circumstances create more anxiety due to uncertainty, nor which disease categories, clinical scenarios or patient characteristics make physicians more or less prone to use race in medical decision-making. Furthermore, the RACE scale did not allow us to identify how physicians consider race (e.g., whether they consider it as a marker of self-efficacy, social support, social or environmental exposures, or biological predispositions), or the relative weight that physicians place on race versus other types of information when they are uncertain. Lastly, the response rate to our survey was low (45%) but similar to other studies of physicians (49, 50).
Physicians encounter uncertainty constantly, and this study finds several new associations with anxiety due to uncertainty. Anxiety due to uncertainty may not be altogether undesirable. A certain amount of anxiety due to uncertainty may push physicians to explore a broad array of potential diagnostic and treatment options in order to make good clinical decisions. The medical community is increasingly aware of the relationship between uncertainty, stress and activation of implicit biases (34, 37). However, this study demonstrates a new finding--the association between high anxiety due to uncertainty and greater explicit use of race in medical decision-making. Under conditions of stress, it is not clear which cognitive shortcut, is more likely to be used —implicit beliefs about racial groups or explicit beliefs about the clinical relevance of race. Additionally, the implications of both types of cognitive shortcuts for patient care remain largely unknown. Our study leaves questions unanswered; however, the associations we found suggest future research should seek to improve our understanding of physicians’ emotional reactions to uncertainty in clinical practice and their reliance on social categories to manage these emotional reactions. To address the main limitation of the current study, we will need research that links anxiety due to uncertainty to actual decisions (collected through use of clinical vignettes or direct observations of patient care) and patient outcomes for diverse populations. This work will reveal whether associations between anxiety due to uncertainty and use of race have implications for patient care and health outcomes.00
Acknowledgments
This research was supported [in part] by the Intramural Research Program of the National Human Genome Research Institute, National Institutes of Health, (VL. Bonham, ZIA HG200324-08). Dr. Cunningham was supported by the Greenwall Fellowship Program in Bioethics and Health Policy and Health Resources and Services Administration training grant (T32HP10025). Dr. Cooper is supported by a grant from the National Heart, Lung, and Blood Institute (K24 HL083113).
References
- 1.Barr DA. The practitioner’s dilemma: can we use a patient’s race to predict genetics, ancestry, and the expected outcomes of treatment? Ann Intern Med. 2005;143:809–15. doi: 10.7326/0003-4819-143-11-200512060-00009. [DOI] [PubMed] [Google Scholar]
- 2.Winker MA. Measuring race and ethnicity: why and how? JAMA. 2004;292:1612–4. doi: 10.1001/jama.292.13.1612. [DOI] [PubMed] [Google Scholar]
- 3.Braun L, Fausto-Sterling A, Fullwiley D, et al. Racial categories in medical practice: how useful are they? PLoS Med. 2007;4:e271. doi: 10.1371/journal.pmed.0040271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taylor AL, Wright JT. Should ethnicity serve as the basis for clinical trial design? Importance of race/ethnicity in clinical trials: lessons from the African-American Heart Failure Trial (A-HeFT), the African-American Study of Kidney Disease and Hypertension (AASK), and the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) Circulation. 2005;112:3654–60. doi: 10.1161/CIRCULATIONAHA.105.540443. [DOI] [PubMed] [Google Scholar]
- 5.Burchard EG, Ziv E, Coyle N, et al. The importance of race and ethnic background in biomedical research and clinical practice. N Engl J Med. 2003;348:1170–5. doi: 10.1056/NEJMsb025007. [DOI] [PubMed] [Google Scholar]
- 6.Cooper RS, Kaufman JS, Ward R. Race and genomics. J Gen Intern Med. 2003;348:1166–70. doi: 10.1056/NEJMsb022863. [DOI] [PubMed] [Google Scholar]
- 7.Das A. How does race get “under the skin”?: inflammation, weathering, and metabolic problems in late life. Soc Sci Med. 2013;77:75–83. doi: 10.1016/j.socscimed.2012.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krieger N. Methods for the scientific study of discrimination and health: an ecosocial approach. Am J Public Health. 2012;102:936–44. doi: 10.2105/AJPH.2011.300544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thayer ZM, Kuzawa CW. Biological memories of past environments: epigenetic pathways to health disparities. Epigenetics. 2011;6:798–803. doi: 10.4161/epi.6.7.16222. [DOI] [PubMed] [Google Scholar]
- 10.Snipes SA, Sellers SL, Tafawa AO, et al. Is race medically relevant? A qualitative study of physicians’ attitudes about the role of race in treatment decision-making. BMC Health Serv Res. 2011;11:183. doi: 10.1186/1472-6963-11-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Frank D, Gallagher TH, Sellers SL, et al. Primary care physicians’ attitudes regarding race-based therapies. J Gen Intern Med. 2010;25(5):384–9. doi: 10.1007/s11606-009-1190-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bonham VL, Sellers SL, Gallagher TH, et al. Physicians’ attitudes toward race, genetics, and clinical medicine. Genetics in medicine. 2009;11:279–86. doi: 10.1097/GIM.0b013e318195aaf4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 14.Dominic OG, McGarrity T, Dignan M, et al. American College of Gastroenterology Guidelines for Colorectal Cancer Screening 2008. Am J Gastroenterol. 2009;104:2626–7. doi: 10.1038/ajg.2009.419. [DOI] [PubMed] [Google Scholar]
- 15.Wolf AM, Wender RC, Etzioni RB, et al. American Cancer Society guideline for the early detection of prostate cancer: update 2010. CA Cancer J Clin. 2010;60:70–98. doi: 10.3322/caac.20066. [DOI] [PubMed] [Google Scholar]
- 16.Moyer VA U S. Preventative Services Task Force. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157:120–34. doi: 10.7326/0003-4819-157-2-201207170-00459. [DOI] [PubMed] [Google Scholar]
- 17.U S. Preventative Services Task Force. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;149:627–37. doi: 10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- 18.Hunt LM, Truesdell ND, Kreiner MJ. Genes, race, and culture in clinical care: racial profiling in the management of chronic illness. Med Anthropol Q. 2013;27:253–71. doi: 10.1111/maq.12026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Atkinson P. Training for certainty. Soc Sci Med. 1984;19:949–56. doi: 10.1016/0277-9536(84)90324-1. [DOI] [PubMed] [Google Scholar]
- 20.Fox RC. The evolution of medical uncertainty. Milbank Mem Q. 1980;58:1–49. [PubMed] [Google Scholar]
- 21.Balsa AI, Seiler N, McGuire TG, et al. Clinical uncertainty and healthcare disparities. Am J Law Med. 2003;29:203–19. [PubMed] [Google Scholar]
- 22.Ghods BK, Roter DL, Ford DE, et al. Patient-physician communication in the primary care visits of African Americans and whites with depression. J Gen Intern Med. 2008;23:600–6. doi: 10.1007/s11606-008-0539-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson RL, Roter D, Powe NR, et al. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health. 2004;94:2084–90. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282:583–9. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 25.Roter DL, Stewart M, Putnam SM, et al. Communication patterns of primary care physicians. JAMA. 1997;277:350–6. [PubMed] [Google Scholar]
- 26.Doescher MP, Saver BG, Franks P, et al. Racial and ethnic disparities in perceptions of physician style and trust. Arch Fam Med. 2000;9:1156–63. doi: 10.1001/archfami.9.10.1156. [DOI] [PubMed] [Google Scholar]
- 27.Corbie-Smith G, Thomas SB, St George DM. Distrust, race, and research. Arch Intern Med. 2002;162:2458–63. doi: 10.1001/archinte.162.21.2458. [DOI] [PubMed] [Google Scholar]
- 28.Boulware LE, Cooper LA, Ratner LE, et al. Race and trust in the health care system. Public Health Rep. 2003;118:358–65. doi: 10.1016/S0033-3549(04)50262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moskowitz D, Thom DH, Guzman D, et al. Is primary care providers’ trust in socially marginalized patients affected by race? J Gen Intern Med. 2011;26:846–51. doi: 10.1007/s11606-011-1672-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gerrity MS, DeVellis RF, Earp JA. Physicians’ reactions to uncertainty in patient care. A new measure and new insights. Med Care. 1990;28(8):724–36. doi: 10.1097/00005650-199008000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Gerrity MS, White KP, DeVellis RF, et al. Physicians’ Reactions to Uncertainty: Refining the Constructs and Scales. Motiv Emot. 1995;19:175–91. [Google Scholar]
- 32.Allison JJ, Kiefe CI, Cook EF, et al. The association of physician attitudes about uncertainty and risk taking with resource use in a Medicare HMO. Med Decis Making. 1998;18:320–9. doi: 10.1177/0272989X9801800310. [DOI] [PubMed] [Google Scholar]
- 33.Carney PA, Yi JP, Abraham LA, et al. Reactions to uncertainty and the accuracy of diagnostic mammography. J Gen Intern Med. 2007;22:234–41. doi: 10.1007/s11606-006-0036-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Ryn M, Burgess DJ, Dovidio JF, et al. The Impact of Racism on Clinician Cognition, Behavior, and Clinical Decision Making. Du Bois Review. 2011;8:199–218. doi: 10.1017/S1742058X11000191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burgess DJ. Are providers more likely to contribute to healthcare disparities under high levels of cognitive load? How features of the healthcare setting may lead to biases in medical decision making. Med Decis Making. 2010;30:246–57. doi: 10.1177/0272989X09341751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McGuire TG, Ayanian JZ, Ford DE, et al. Testing for statistical discrimination by race/ethnicity in panel data for depression treatment in primary care. Health Serv Res. 2008;43:531–51. doi: 10.1111/j.1475-6773.2007.00770.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Balsa AI, McGuire TG, Meredith LS. Testing for statistical discrimination in health care. Health Serv Res. 2005;40:227–52. doi: 10.1111/j.1475-6773.2005.00351.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Seaburn DB, Morse D, McDaniel SH, et al. Physician responses to ambiguous patient symptoms. J Gen Intern Med. 2005;20:525–30. doi: 10.1111/j.1525-1497.2005.0093.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lutfey KE, Link CL, Grant RW, et al. Is certainty more important than diagnosis for understanding race and gender disparities? An experiment using coronary heart disease and depression case vignettes. Health Policy. 2009;89:279–87. doi: 10.1016/j.healthpol.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Balsa AI, McGuire TG. Prejudice, clinical uncertainty and stereotyping as sources of health disparities. J Health Econ. 2003;22:89–116. doi: 10.1016/s0167-6296(02)00098-x. [DOI] [PubMed] [Google Scholar]
- 41.Bonham V, Sellers SL, Woolford S. Physicians’ knowledge, use, and beliefs about race and genetics: new measures and new insights. Under Review. 2014 doi: 10.1186/1472-6963-14-456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chin MH, Humikowski CA. When is risk stratification by race or ethnicity justified in medical care? Acad Med. 2002;77:202–8. doi: 10.1097/00001888-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 43.Tervalon M, Murray-Garcia J. Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved. 1998;9:117–25. doi: 10.1353/hpu.2010.0233. [DOI] [PubMed] [Google Scholar]
- 44.Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 45.Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Med Care. 2008;46:678–85. doi: 10.1097/MLR.0b013e3181653d58. [DOI] [PubMed] [Google Scholar]
- 46.Lutfey KE, Campbell SM, Renfrew MR, et al. How are patient characteristics relevant for physicians’ clinical decision making in diabetes? An analysis of qualitative results from a cross-national factorial experiment. Soc Sci Med. 2008;67:1391–9. doi: 10.1016/j.socscimed.2008.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van Ryn M, Burgess D, Malat J, et al. Physicians’ perceptions of patients’ social and behavioral characteristics and race disparities in treatment recommendations for men with coronary artery disease. Am J Public Health. 2006;96:351–7. doi: 10.2105/AJPH.2004.041806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Soc Sci Med. 2000;50:813–28. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- 49.VanGeest JB, Johnson TP, Welch VL. Methodologies for improving response rates in surveys of physicians: a systematic review. Eval Health Prof. 2007;30:303–21. doi: 10.1177/0163278707307899. [DOI] [PubMed] [Google Scholar]
- 50.Kellerman SE, Herold J. Physician response to surveys. A review of the literature. Am J Prev Med. 2001;20:61–7. doi: 10.1016/s0749-3797(00)00258-0. [DOI] [PubMed] [Google Scholar]