Abstract
Impaired fetal abdominal blood flow may lead to smaller kidneys and subsequent impaired kidney function in later life. In a prospective cohort study among 923 pregnant women and their children, we measured fetal growth, kidney volumes, and umbilical and cerebral artery blood flow (median gestational age of 30.3 weeks; 95% range, 28.5–32.7 weeks). We used a higher umbilical/cerebral artery pulsatility index ratio as an indicator of preferential fetal blood flow to the upper body parts at the expense of the intra-abdominal organs. At a median age of 5.9 years (95% range, 5.7–6.6 years), we measured childhood kidney volumes, creatinine and cystatin C blood levels, microalbuminuria, BP, and eGFR. A preferential fetal blood flow to the upper body parts at the expense of the intra-abdominal organs associated only with a smaller combined kidney volume in childhood. Fetal combined kidney volume positively associated with childhood combined kidney volume and eGFR, and inversely associated with childhood creatinine and cystatin C levels (all P values <0.05), but did not associate with childhood microalbuminuria and BP. Children within the highest tertile of fetal umbilical/cerebral ratio and the lowest tertile of fetal combined kidney volume had the lowest eGFR (difference, −6.36 ml/min per 1.73 m2; 95% confidence interval, −11.78 to −0.94 compared with children within the middle tertiles). These data suggest that impaired fetal blood to the abdominal organs and smaller fetal kidney size are associated with subclinical changes in kidney outcomes in school-aged children.
The third trimester of pregnancy is a critical period for fetal kidney development.1 Nephrogenesis continues until 36 weeks of gestation, after which the induction of nephron numbers ceases.2 A permanent reduction of kidney size and number of nephrons leads to a smaller glomerular filtration surface area, which might predispose the individual to decreased kidney function in childhood and subsequently to kidney disease and hypertension in adulthood.3,4 This hypothesis is supported by studies showing consistent associations of low birth weight with higher risks of kidney disease and hypertension in later life.5,6 Although the observed effect estimates from these studies were small, they are important from an etiologic perspective.5,6 In addition, post mortem studies showed that the nephron number is lower in hypertensive individuals than in normotensive controls7 and is positively correlated with birth weight and kidney size.8,9 Animal studies demonstrated a reduction in nephron number as a result of vascular placental insufficiency.10 Placental insufficiency is an important risk factor for fetal growth restriction and low birth weight.11 We recently demonstrated that increased third trimester placental insufficiency is associated with a higher BP in childhood.12 Placental insufficiency is characterized by a preferential fetal blood flow to the brain at the expense of the trunk.13 This fetal blood flow redistribution is caused by higher peripheral and lower cerebral arterial resistance,11 and can be measured as a higher umbilical artery pulsatility index (PI) and lower cerebral artery PI, respectively. This combination leads to a higher ratio of these measures (higher umbilical/cerebral (U/C) ratio).14 It is unknown whether and to what extent impaired abdominal or kidney blood flow and kidney growth restriction during fetal life lead to risk factors for kidney disease in later life.
In this population-based prospective cohort study among 923 pregnant women and their children, we evaluated the associations of third trimester fetal blood flow redistribution, at the expense of the abdominal organs, and smaller fetal kidney size with kidney function outcomes in school-aged children. We also explored whether any association was explained by childhood kidney size.
Results
Participant Characteristics
Maternal, fetal, and child characteristics are shown in Table 1. More descriptive data are given in the Supplemental Material. Participant characteristics according to tertiles of U/C ratio and fetal kidney volume are given in Supplemental Tables 1 and 2, respectively. Supplemental Figures 1 and 2 give the correlations of gestational age and estimated fetal weight with fetal kidney volume/estimated fetal weight.
Table 1.
Participant characteristics (N=923)
| Characteristic | Value |
|---|---|
| Maternal characteristics | |
| Age, yr | 32.2 (23.4–39.4) |
| Height, cm | 171 (6.3) |
| Prepregnancy weight, kg | 69.0 (13.0) |
| Prepregnancy body mass index, kg/m2 | 23.6 (4.2) |
| Parity≥1, % | 348 (37.7) |
| Education level, % | |
| Primary/secondary | 315 (34.1) |
| Secondary or higher | 608 (65.9) |
| Smoking during pregnancy, % | |
| Yes | 198 (21.5) |
| No | 745 (78.5) |
| Folic acid supplement use, % | |
| Yes | 839 (90.9) |
| No | 84 (9.1) |
| Pregnancy-induced hypertension, % | |
| Yes | 52 (5.6) |
| No | 871 (94.4) |
| Preeclampsia, % | |
| Yes | 29 (3.1) |
| No | 894 (96.9) |
| Fetal characteristics | |
| General | |
| Gestational age at measurement, wk | 30.3 (28.5–32.7) |
| Estimated fetal weight, g | 1634 (263) |
| Blood flow distribution | |
| Umbilical artery PI | 0.97 (0.16) |
| Middle cerebral artery PI | 1.97 (0.33) |
| U/C ratio middle cerebral artery | 0.50 (0.11) |
| Fetal kidney biometrics, cm3 | |
| Right kidney volume | 10.64 (3.07) |
| Left kidney volume | 9.94 (2.76) |
| Combined kidney volume | 20.56 (5.48) |
| Birth and infant characteristics | |
| Gestational age at birth, wk | 40.3 (36.4–42.4) |
| Birth weight, g | 3534 (509) |
| Boys, % | 464 (50.3) |
| Childhood characteristics | |
| Age at follow-up, y | 5.9 (5.7–6.6) |
| Height, cm | 119 (5.2) |
| Weight, kg | 22.6 (3.2) |
| Body mass index, kg/m2 | 15.9 (1.4) |
| Body surface area, m2 | 0.86 (0.07) |
| Kidney volume left, cm3 | 61.4 (12.6) |
| Kidney volume right, cm3 | 59.5 (11.7) |
| Kidney volume combined, cm3 | 120.9 (22.1) |
| Creatinine, µmol/L | 36.8 (4.9) |
| Cystatin C, µg/L | 790 (74) |
| eGFR, ml/min per 1.73 m2 | 120.2 (15.8) |
| eGFR/cm3 kidney volume | 1.02 (0.19) |
| Microalbuminuria, %a | 62 (7.1) |
| Systolic BP, mmHg | 102.2 (7.7) |
| Diastolic BP, mmHg | 60.1 (6.3) |
Values are means (SD), medians (95% range), or n (%). Observed data before multiple imputation are presented in Supplemental Table 8.
Defined as levels between 2.5 and 25.0 mg/mmol (boys) and 3.5 and 25.0 mg/mmol (girls).
Fetal Blood Flow, Fetal Kidney Volume, and Childhood Kidney Outcomes
Scatterplots for the correlations between fetal and childhood kidney volumes, fetal blood flow patterns, and childhood kidney function outcomes are shown in Supplemental Figures 3–5.
Table 2 shows that a higher third trimester fetal U/C ratio, which reflects a preferential blood flow to the upper body parts at the expense of the intra-abdominal organs, was associated with a smaller childhood combined kidney volume (−2.46 cm3 per 1 SD score increase in ratio; 95% confidence interval [95% CI], −3.89 to −1.04; basic model). This fetal blood flow pattern was not associated with childhood creatinine and cystatin C levels, eGFR, microalbuminuria, or BP. The effect estimates were only slightly modified by additional adjustment for confounders or childhood kidney size. Table 3 shows that a larger third trimester fetal combined kidney volume was associated with larger childhood combined kidney volume (3.89 cm3 per 1 SD score increase in volume; 95% CI, 3.61 to 4.16), lower creatinine levels (−1.18 µmol/L per 1 SD score increase in volume; 95% CI, −1.60 to −0.77), lower cystatin C levels (−18 µg/L per 1 SD score increase in volume; 95% CI, −25 to −12), and higher eGFR (4.40 ml/min per 1.73 m2 per 1 SD score increase in volume; 95% CI, 3.06 to 5.75), but not with microalbuminuria and BP at 6 years of age. These effect estimates were similar after additional adjustment for potential confounders and combined childhood kidney volume. Supplemental Tables 3 and 4 provide additional results showing the effects of stepwise adjustment of the associations of the third trimester fetal U/C ratio and fetal combined kidney volume with childhood kidney outcomes. In addition, Supplemental Tables 5 and 6 give the R2 values for the effect estimates for the associations of third trimester fetal U/C ratio and third trimester fetal combined kidney volume with childhood kidney outcomes. The R2 values were all between 0.20 and 0.25.
Table 2.
Associations of third trimester U/C ratioa with kidney outcomes at 6 years of age (n=879)
| Model | Difference in Kidney Size | Difference in Kidney Function | Difference in BP | ||||
|---|---|---|---|---|---|---|---|
| Combined Kidney Volume (cm3) | Creatinine (µmol/L) | Cystatin C (µg/L) | eGFR (ml/min per 1.73 m2) | Microalbuminuria | Systolic (mmHg) | Diastolic (mmHg) | |
| Basic | −2.46 (−3.89 to −1.04)b | 0.14 (−0.27 to 0.55) | 4 (−3 to 10) | −0.67 (−2.00 to 0.68) | 0.75 (0.55 to 1.01) | 0.27 (−0.26 to 0.81) | 0.04 (−0.41 to 0.49) |
| Confounder | −2.58 (−4.01 to −1.14)b | 0.24 (−0.18 to 0.66) | 4 (−3 to 11) | −1.03 (−2.39 to 0.34) | 0.71 (0.52 to 0.97)c | 0.30 (−0.25 to 0.85) | 0.05 (−0.41 to 0.50) |
| Childhood kidney volume | NA | 0.10 (−0.32 to 0.52) | 3 (−3 to 10) | −0.29 (−1.66 to 1.08) | 0.72 (0.52 to 1.00) | 0.21 (−0.37 to 0.78) | −0.02 (−0.50 to 0.45) |
Values are regression coefficients (95% CIs) based on multiple regression models as well as odds ratios (95% CIs) for microalbuminuria based on logistic regression models, and reflect the difference for each outcome for fetal blood flow characteristics. The basic model is adjusted for gestational age at third trimester measurement, third trimester estimated fetal weight, child sex, current age, and body surface area. The confounder model is additionally adjusted for maternal age, parity, educational level, prepregnancy body mass index, smoking status during pregnancy, maternal pregnancy complications (hypertension, preeclampsia), folic acid use during pregnancy, gestational age, and gestational age–adjusted birth weight. The childhood kidney volume model is additionally adjusted for combined childhood kidney volume. NA, not applicable.
U/C ratio SD = 0.11.
P<0.01.
P<0.05.
Table 3.
Associations of third trimester fetal kidney dimensionsa with kidney outcomes at 6 years of age (n=870)
| Model | Difference in Kidney Size | Difference in Kidney Function | Difference in BP | ||||
|---|---|---|---|---|---|---|---|
| Combined Kidney Volume (cm3) | Creatinine (µmol/L) | Cystatin C (µg/L) | eGFR (ml/min per 1.73 m2) | Microalbuminuria | Systolic (mmHg) | Diastolic (mmHg) | |
| Basic | 3.89 (3.61 to 4.16)b | −1.18 (−1.60 to −0.77)b | −18 (−25 to −12)b | 4.40 (3.06 to 5.75)b | 1.05 (0.90 to 1.22) | −0.32 (−0.89 to 0.26) | −0.24 (−0.49 to 0.01) |
| Confounder | 3.96 (2.43 to 5.49)b | −1.22 (−1.63 to −0.80)b | −18 (−25 to −12)b | 4.45 (3.08 to 5.83)b | 1.06 (0.78 to 1.44) | −0.29 (−0.89 to 0.31) | −0.18 (−0.67 to 0.32) |
| Childhood kidney volume | NA | −0.87 (−1.29 to −0.45)b | −16 (−22 to −9)b | 3.21 (1.85 to 4.56)b | 0.97 (0.70 to 1.34) | −0.26 (−0.89 to 0.38) | −0.08 (−0.60 to 0.44) |
Values are regression coefficients (95% CIs) based on multiple regression models as well as odds ratios (95% CIs) for microalbuminuria based on logistic regression models, and reflect the difference for each outcome for fetal blood flow characteristics. The basic model is adjusted for gestational age at third trimester measurement, third trimester estimated fetal weight, child sex, current age, and body surface area. The confounder model is additionally adjusted for maternal age, parity, educational level, prepregnancy body mass index, smoking status during pregnancy, maternal pregnancy complications (hypertension, preeclampsia), folic acid use during pregnancy, gestational age, and gestational age–adjusted birth weight. The childhood kidney volume model is additionally adjusted for combined childhood kidney volume. NA, not applicable.
Combined fetal kidney volume SD = 5.48.
P<0.01.
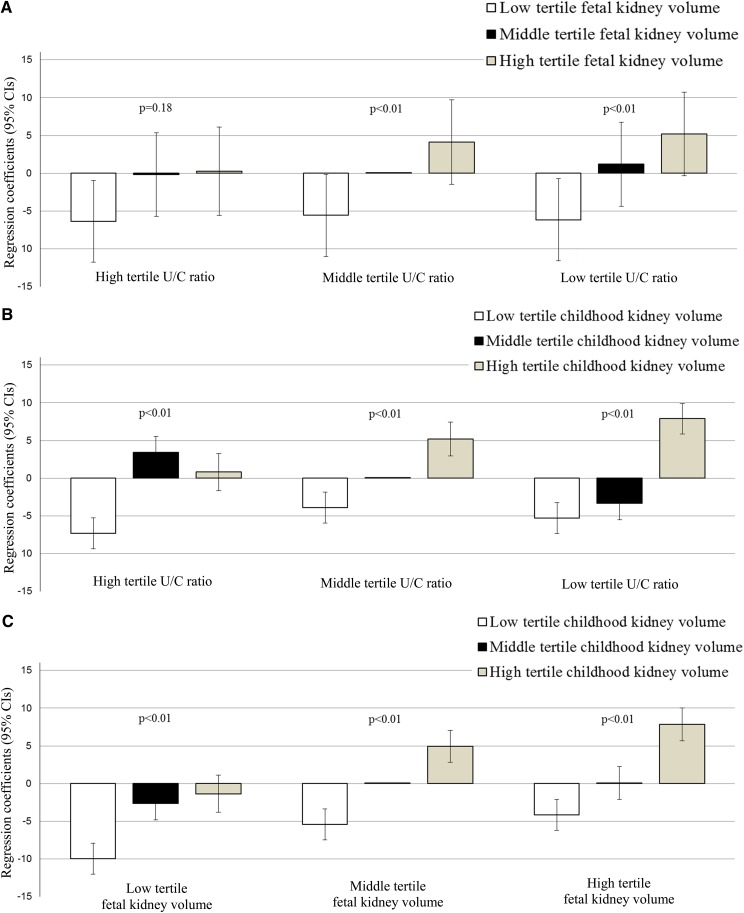
Figure 1A shows the combined effects for fetal blood flow and fetal kidney volume on childhood eGFR. Children within the highest tertile of fetal U/C ratio and lowest tertile of fetal combined kidney volume had the lowest eGFR (difference, −6.36 ml/min per 1.73 m2; 95% CI, −11.78 to −0.94) compared with children within the middle tertiles, whereas children within the lowest tertile of fetal U/C ratio and the highest tertile of fetal combined kidney volume had the highest eGFR at school age (P for interaction<0.05). Figure 1B gives the combined effects for fetal blood flow and childhood combined kidney volume on childhood eGFR. Children within the highest tertile of fetal U/C ratio and the lowest tertile of childhood combined kidney volume had the lowest eGFR. This interaction was not statistically significant. Similarly, Figure 1C gives the combined effects for fetal combined kidney volume and childhood combined kidney volume on childhood eGFR. The lowest eGFR was observed in children within the lowest tertile of both fetal combined kidney volume and childhood combined kidney volume. This interaction was statistically not significant. In addition, the interaction terms were statistically not significant for childhood cystatin C levels, microalbuminuria, and BP as outcomes (data not shown).
Figure 1.
Associations of fetal blood flow, fetal combined kidney volume, and childhood kidney volume with childhood eGFR (n=613). Bars represent regression coefficients (95% CIs) based on multiple regression models and reflect the associations of fetal blood flow and kidney volume (A), fetal blood flow and childhood kidney volume (B), and fetal and childhood kidney volume (C) (tertiles) with childhood eGFR. Models are adjusted for maternal age, parity, education level, prepregnancy body mass index, smoking status during pregnancy, folic acid use during pregnancy, maternal pregnancy complications (hypertension, preeclampsia), gestational age at third trimester measurement, third trimester estimated fetal weight, child sex, gestational age, and gestational age–adjusted birth weight, and current age. P<0.01 for the interaction between fetal blood flow and fetal combined kidney volume for the association with childhood eGFR. The P value for the interaction between fetal blood flow and childhood combined kidney volume and for interaction between fetal combined kidney volume and childhood combined kidney volume is not significant.
Results of the sensitivity analyses are given in the Supplemental Material. We observed similar results when we used gestational age–adjusted birth weight as an index of the final nephron number instead of fetal kidney volume (Supplemental Figure 6). Lower gestational age–adjusted birth weight was associated with smaller childhood kidneys with a lower eGFR. The interactions between the U/C ratio and gestational age–adjusted birth weight for the associations with childhood kidney outcomes were not significant. In addition, no differences in results were observed in the final models when we used eGFR/cm3 kidney volume instead of eGFR (data not shown).
Discussion
In a normal, low-risk population–based cohort study, third trimester fetal blood flow redistribution, at the expense of the trunk and abdominal organs, was associated with smaller kidney volume, whereas a smaller third trimester fetal kidney size was associated with lower kidney function in school-aged children. All differences were small and without clinical consequences at school age. Fetal blood flow and fetal kidney size were not associated with childhood BP.
An adverse fetal environment may lead to smaller kidneys with a reduced number of nephrons.15 These kidney adaptations may lead to a reduced glomerular filtration surface area, hyperfiltration, and eventually glomerular sclerosis and CKD.2,3 Thus far, this hypothesis is mainly supported by studies showing associations of low birth weight with higher risks of kidney disease and hypertension in adulthood.5,6 In addition, post mortem studies showed that the nephron number is lower in children with a low birth weight, or small kidney size, and in adults with primary hypertension.7–9 Studies in rats showed that fetal growth restriction, induced by bilateral uterine artery ligation, leads to an increased risk of kidney disease and higher BP in adulthood.16,17 In a study among 7457 adults aged 20–30 years in Norway, intrauterine growth restriction was associated with low-normal kidney function.18 Another study among 82 participants born before 32 weeks of gestation in The Netherlands observed no consistent associations of preterm birth in combination with intrauterine growth restriction with kidney function in young adulthood.19
Animal studies showed a reduction in glomerular and nephron number as a result of vascular placental insufficiency.10,20 In a previous study within the same cohort, we observed that fetal blood flow redistribution at the expense of the abdominal organs leads to smaller fetal kidneys.21 In this follow-up study, we observed that fetal blood flow redistribution is also associated with smaller kidneys in children. Surprisingly, we observed that fetal blood redistribution at the expense of the abdominal organs was associated with a lower risk of microalbuminuria, independent of potential confounders and childhood kidney size. We could not explain this finding. Fetal blood flow redistribution was not associated with other kidney function outcomes. We measured fetal blood flow through the umbilical arteries, which reflects the arterial resistance and blood flow to the intra-abdominal arteries, including the descending aorta and renal artery.22 Future detailed studies focused on the directly measured renal artery blood flow might give more information about the fetal and childhood consequences of impaired fetal kidney blood flow.
A recent cross-sectional study, among 257 healthy children in Italy aged>6 months, indicated that childhood kidney size was inversely correlated with creatinine levels.23 In line with that study, we observed an inverse association of fetal kidney size with creatinine and cystatin C levels in childhood, and a positive association with eGFR. We previously observed that small fetal kidney size tends to track throughout early childhood.24 In this study, we observed that the associations of fetal kidney volume with childhood kidney function outcomes were independent of childhood kidney size. These findings suggest that fetal kidney size may have permanent subclinical effects, independent of later kidney growth, on kidney function in later life. Fetal kidney size was not associated with childhood microalbuminuria or BP. It might be that differences in these more clinical markers of kidney dysfunction appear at older ages.
The results of this study are important from an etiologic perspective. Our findings suggest that suboptimal abdominal blood flow and kidney growth in fetal life have persistent subclinical renal consequences. However, the observed effect estimates were small and reflect subclinical changes in kidney function in school-aged children. None of the children had a known clinical kidney disease. Therefore, the results of this study are without direct clinical consequence. Longitudinal studies reported tracking of risk factors for kidney and cardiovascular disease during childhood.25,26 In addition, the consequences of impaired kidney growth might not yet be fully detectable in early childhood, but might become more evident in later life. It was previously suggested that fetal adverse adaptations can be compensated for many years until hypertension occurs.5
The biologic mechanisms underlying the observed associations may include mechanisms other than smaller kidneys with a lower number of nephrons.4 Animal studies showed alterations in the renin-angiotensin system in rats with experimentally induced intrauterine growth restriction at adult age. These differences were not present at younger age.27 Several markers of the renin-angiotensin system were increased in participants with intrauterine growth restriction and hypertension.27 An accumulating body of evidence suggests that an adverse intrauterine environment might cause epigenetic alterations that in turn influence kidney growth and function.4 Finally, a mismatch between fetal and postnatal growth may also lead to insufficient kidney function for an individual metabolic load. This might specifically be the case in children with fetal growth restriction and smaller fetal kidneys, but with a postnatal catch-up growth. Further studies are needed to examine the combined effects of impaired fetal kidney growth and postnatal catch-up growth on childhood kidney outcomes.
Some methodologic considerations need to be discussed. The main strength of this study is its population-based prospective design from fetal life onward. Follow-up measurements at 6 years of age were obtained in 75% of the children. Mothers of children without follow-up measurements were more frequently multiparous, were lower educated, and smoked during pregnancy. Their children had a lower birth weight. Thus, the remaining children with follow-up measurements may be healthier than the original study population. Our results would be biased if the associations of fetal characteristics with childhood kidney outcomes would differ between those with and without follow-up measurements. This seems unlikely, but cannot be excluded. However, because of our relatively healthy population, further studies are needed to determine whether the observed associations are generalizable to high-risk populations. We evaluated fetal blood flow and fetal kidney volume at one time point during late pregnancy. Although the intraobserver and interobserver variability are adequate and mean values are in line with previous studies, misclassification as a result of measurement error cannot be excluded. However, this would most likely have been caused by random error, which reduces the power of the study and may have led to an underestimation of the evaluated associations. We did not study abnormal blood flow distribution. Because our study was embedded in a low-risk healthy population, our main focus was to study the renal consequences of variation in fetal blood flow within a normal range. Therefore, we used continuous data and tertiles of blood flow distribution. Fetal kidney volume was evaluated around 30 weeks of gestational age. Because nephrogenesis continues until 36 weeks of gestational age, our measurements did not reflect the final nephron number.2 Evaluation of fetal kidney size until 36 weeks of gestational age might have been more representative of the final nephron number. We observed similar results when we used gestational age–adjusted birth weight as a surrogate for the final nephron number instead of third trimester kidney volume. It is not known whether birth weight is a better proxy for the fetal nephron number than fetal kidney size.28 We used kidney size as a measure of kidney development because the nephron number cannot be studied in vivo. Kidney size is correlated with the number of glomeruli and can be used in epidemiologic studies as a measure of kidney development.28 However, nephron enlargement as a result of hyperfiltration may attenuate the differences in childhood kidney volume and may lead to an underestimation of the associations of interest.29 We estimated the glomerular filtration using blood creatinine levels. Blood cystatin C levels might be more accurate in estimating glomerular filtration. Compared with creatinine, cystatin C is freely filtered, is produced more constantly, and is less dependent on children’s body weight, height, and sex.30 In this study, we observed similar results for creatinine and cystatin C levels. We used the urine albumin/creatinine ratio to evaluate albuminuria in a random urine sample.31 Because the within-subject variation in urinary albumin excretion is large, the variability would probably be lower if we collected first morning void samples instead of random samples during the day32; however, this was not possible in this study. We evaluated multiple associations, which might have led to chance findings as a result of multiple testing. However, because the kidney-related outcomes were correlated, we did not adjust for multiple testing. Finally, although we had information about a large number of confounders, the influence of residual confounding should be considered, as in any observational study.
In conclusion, fetal blood redistribution at the expense of the intra-abdominal organs and smaller fetal kidneys are associated with subclinical changes in kidney outcomes in a healthy population of school-aged children. Although these findings suggest that fetal kidney developmental adaptations affect kidney function throughout the life course, the effect estimates were small and likely to be without clinical consequences in childhood. Further studies are needed to identify the underlying biologic mechanisms and the long-term consequences of the observed associations.
Concise Methods
Design and Study Population
This study was embedded in the Generation R Study, a population-based prospective cohort study from fetal life onward in Rotterdam, The Netherlands. All children were born between April 2002 and January 2006. Enrollment was aimed at early pregnancy at the routine fetal ultrasound examination in pregnancy but was allowed until the birth of the child. In total, 9778 mothers and their children were included in this study. More detailed assessments of fetal and postnatal growth and development were conducted in a random subgroup of 1232 Dutch mothers and children (response, 80%).33 Twin pregnancies (n=15) and pregnancies leading to perinatal death (n=2) were excluded from the analysis, leading to 1215 singleton live births. Third trimester blood flow distribution and fetal kidney measurements were successfully performed in 1201 singleton live born children, of whom 925 children (77%) visited the research center for follow-up measurements at the median age of 5.9 years (95% range, 5.7–6.6). Childhood kidney measurements were successfully performed in 923 children (Supplemental Figure 7 provides a study flow chart). Nonresponse analysis showed that compared with mothers of children not included in the analysis, mothers of children included in the study were older, were more highly educated, smoked less frequently during pregnancy, were more frequently nulliparous, and used folic acid supplements. Furthermore, children included in the study had a higher birth weight and gestational age at birth and more often were girls (Supplemental Table 7). The Medical Ethics Committee of the Erasmus University Medical Center approved this study.
Third Trimester Fetal Measurements
Third trimester fetal ultrasound examinations were performed at a median gestational age of 30.3 weeks (95% range, 28.5–32.7).
Fetal Growth
Gestational age was established by first trimester ultrasound measurements.34 Fetal head circumference, abdominal circumference, and femur length were measured and estimated fetal weight was calculated using the formula by Hadlock et al.35
Fetal Blood Flow Distribution
We measured fetal blood flow distribution as inverse of the corresponding resistance indices in the umbilical and cerebral artery by pulsed wave Doppler, as previously described.11 The PI in a fetal artery reflects the difference between the peak systolic and minimum diastolic velocities divided by the mean velocity during the cardiac cycle and is inversely related to the flow in this artery. Thus, a higher PI reflects a lower flow in this artery. Color imaging was used to optimize placement of the pulsed wave Doppler gate in every measurement. For each measurement, three consecutive uniform waveforms, during fetal apnea and without fetal movement, were recorded and the mean of these measurements was used for further analysis. Umbilical artery PI was determined in a free-floating loop of the umbilical cord. A raised umbilical artery PI indicates increased vascular resistance and lower blood flow in the lower body parts.36 Middle cerebral artery Doppler measurements were performed with color Doppler visualization of the circle of Willis in the fetal brain, and flow velocity waveforms were obtained in the proximal part of the cerebral arteries. Reductions in the middle cerebral artery PI are a valid indicator of fetal blood redistribution in favor of the brain.22 Fetal blood redistribution in favor of the brain at the expense of the trunk, including the abdominal organs, is indicated by a higher ratio between the umbilical artery PI and the cerebral artery PI (higher U/C ratio).14 Intraobserver and interobserver analyses showed good reproducibility for all Doppler measurements, as previously described (all intraclass correlation coefficients>0.80).13 The mean (SD) PIs observed in our study were in line with a previous longitudinal study focused on serial measurements.37
Fetal Kidney Dimensions
In a sagittal plane, the maximum longitudinal kidney lengths were measured placing the calipers on the outer edges of the caudal and cranial side.21 Anteroposterior and transverse kidney diameters were measured perpendicular to each other, outer to outer, in an axial plane. The cross-sectional area in which the kidney appeared symmetrically round at its maximum width was used.38 Kidney volume was calculated using the equation of an ellipsoid as follows: volume (in cubic centimeters)=0.523×length×width×depth (all in millimeters).39 Combined kidney volume was calculated by summing right and left kidney volume.
Childhood Kidney Outcomes
Childhood Kidney Dimensions
Left and right kidney biometrics were at the median age of 5.9 years (95% range, 5.7–6.6). We identified the left and right kidneys in the sagittal plane along its longitudinal axis. We performed measurements of maximal bipolar kidney length, width, and depth. Kidney width and depth were measured at the level of the hilum. The cross-sectional area in which the kidney appeared symmetrically round at its maximum width was used. We calculated left and right kidney volume by using the same ellipsoid equation as for fetal kidney volume.39 We previously reported good intraobserver and interobserver correlation coefficients.40
Childhood Kidney Function
Blood creatinine levels were measured with an enzymatic method on a Cobas c 502 analyzer (Roche Diagnostics, Germany), and cystatin C levels were measured by a particle enhanced immunoturbidimetric assay on a Cobas c 702 analyzer (Roche Diagnostics). Quality control samples demonstrated intra-assay and interassay coefficients of variation ranging from 0.51% to 1.37% and from 1.13% to 1.65%, respectively. The eGFR was calculated according to the revised Schwartz 2009 formula as follows: eGFR=36.5×height (in centimeters)/creatinine (in micromoles per liter).41 Urine creatinine levels (in millimoles per liter) and urine albumin levels (in milligrams per liter) were determined on a Beckman Coulter AU analyzer. Creatinine levels were measured according to the Jaffe method. We also calculated the albumin/creatinine ratio. Microalbuminuria was defined as an albumin/creatinine ratio between 2.5 and 25 mg/mmol for boys and between 3.5 and 25 mg/mmol for girls.42
Childhood BP
Systolic and diastolic BP were measured at the right brachial artery (four times with 1-minute intervals) using the Datascope Accutor Plus validated automatic sphygmometer (Paramus, NJ).43 A cuff was selected that was long enough to cover 90% of the arm length, with a cuff width to cover approximately 40% of the arm circumference.
Covariates
Information on maternal age, prepregnancy body mass index, parity, education level, smoking during pregnancy, folic acid use during pregnancy, and gestational hypertensive complications was obtained by questionnaires and registries. Maternal height was measured without shoes and the prepregnancy body mass index was calculated (in kilograms per square meter). Date of birth, infant sex, and birth weight were obtained from midwife and hospital registries. At 6 years of age, child height and weight were measured without shoes and heavy clothing, and the body surface area was calculated.
Statistical Analyses
First, we performed correlation analyses using scatterplots and Pearson correlation coefficients to explore the relation between gestational age with U/C ratio, fetal kidney volume, and fetal kidney volume/estimated fetal weight. We also performed correlation analyses for the relations between fetal blood flow patterns, fetal combined kidney volume, and childhood kidney outcomes. Second, the associations of fetal blood flow distribution and fetal combined kidney volume with childhood kidney outcomes were analyzed in a stepwise approach. We performed correlation analyses using scatterplots and Pearson correlation coefficients. Next we performed multiple linear regression models. The models were first adjusted for gestational age and estimated fetal weight at third trimester measurement, as well as child sex, current age, and body surface area (basic model). Analyses focused on eGFR were not further adjusted for body surface area because this is included in the Schwartz 2009 formula. These models were additionally adjusted for potential confounders including maternal age, parity, educational level, prepregnancy body mass index, smoking status during pregnancy, pregnancy complications (preeclampsia and pregnancy-induced hypertension), gestational age at birth, and gestational age–adjusted birth weight (confounder model). We additionally adjusted the confounder model for childhood combined kidney volume to explore whether any association was explained by childhood combined kidney volume (childhood kidney volume model). Third, we tested potential combined effects and interactions between fetal blood flow, fetal combined kidney volume, and childhood combined kidney volume for the associations with childhood eGFR by performing stratified (tertiles) regression analyses. We performed a sensitivity analysis using gestational age–adjusted birth weight as an additional index of the final nephron number instead of fetal kidney volume. To reduce the possibility of potential bias associated with missing data (<17%), missing values in maternal, fetal, and child covariates were imputed using the multiple imputations procedure with five imputations and these data sets were analyzed together. Further information about the methods of multiple imputations are given in the Supplemental Material. Observed data before multiple imputations are presented in Supplemental Table 8. All statistical analyses were performed using the Statistical Package for the Social Sciences for Windows (version 20.0; SPSS Inc., Chicago, IL).
Disclosures
None.
Supplementary Material
Acknowledgments
The Generation R Study is being conducted by the Erasmus University Medical Center and Erasmus University Rotterdam in close collaboration with the Rotterdam Municipal Health Service Rotterdam and the Rijnmond Stichting Artsenlaboratorium and Trombosedienst (Foundation Doctors Laboratory and Thrombosis). We gratefully acknowledge the contributions of the children and their parents, general practitioners, hospitals, midwives, and pharmacies in Rotterdam.
The Generation R Study receives financial support from the Erasmus University Medical Center and The Netherlands Organization for Health Research and Development. O.H.F. works in ErasmusAGE, a center for aging research across the life course funded by Nestlé Nutrition (Nestec, Ltd.), Metagenics, Inc., and AXA. Nestlé Nutrition (Nestec, Ltd.), Metagenics, Inc., and AXA had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review or approval of the manuscript. Additional support was provided by a grant from the Dutch Kidney Foundation (C08.2251). V.W.V.J. received an additional grant from The Netherlands Organization for Health Research and Development (VIDI 016.136.361).
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “The Life Cycle of the Kidney: Implications for CKD,” on pages 2388–2390.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2013070746/-/DCSupplemental.
References
- 1.Gluckman PD, Hanson MA, Cooper C, Thornburg KL: Effect of in utero and early-life conditions on adult health and disease. N Engl J Med 359: 61–73, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hinchliffe SA, Sargent PH, Howard CV, Chan YF, van Velzen D: Human intrauterine renal growth expressed in absolute number of glomeruli assessed by the disector method and Cavalieri principle. Lab Invest 64: 777–784, 1991 [PubMed] [Google Scholar]
- 3.Brenner BM, Garcia DL, Anderson S: Glomeruli and blood pressure. Less of one, more the other? Am J Hypertens 1: 335–347, 1988 [DOI] [PubMed] [Google Scholar]
- 4.Luyckx VA, Bertram JF, Brenner BM, Fall C, Hoy WE, Ozanne SE, Vikse BE: Effect of fetal and child health on kidney development and long-term risk of hypertension and kidney disease. Lancet 382: 273–283, 2013 [DOI] [PubMed] [Google Scholar]
- 5.Huxley R, Neil A, Collins R: Unravelling the fetal origins hypothesis: Is there really an inverse association between birthweight and subsequent blood pressure? Lancet 360: 659–665, 2002 [DOI] [PubMed] [Google Scholar]
- 6.White SL, Perkovic V, Cass A, Chang CL, Poulter NR, Spector T, Haysom L, Craig JC, Salmi IA, Chadban SJ, Huxley RR: Is low birth weight an antecedent of CKD in later life? A systematic review of observational studies. Am J Kidney Dis 54: 248–261, 2009 [DOI] [PubMed] [Google Scholar]
- 7.Keller G, Zimmer G, Mall G, Ritz E, Amann K: Nephron number in patients with primary hypertension. N Engl J Med 348: 101–108, 2003 [DOI] [PubMed] [Google Scholar]
- 8.Hughson M, Farris AB, 3rd, Douglas-Denton R, Hoy WE, Bertram JF: Glomerular number and size in autopsy kidneys: The relationship to birth weight. Kidney Int 63: 2113–2122, 2003 [DOI] [PubMed] [Google Scholar]
- 9.Mañalich R, Reyes L, Herrera M, Melendi C, Fundora I: Relationship between weight at birth and the number and size of renal glomeruli in humans: A histomorphometric study. Kidney Int 58: 770–773, 2000 [DOI] [PubMed] [Google Scholar]
- 10.Bassan H, Trejo LL, Kariv N, Bassan M, Berger E, Fattal A, Gozes I, Harel S: Experimental intrauterine growth retardation alters renal development. Pediatr Nephrol 15: 192–195, 2000 [DOI] [PubMed] [Google Scholar]
- 11.Gaillard R, Arends LR, Steegers EA, Hofman A, Jaddoe VW: Second- and third-trimester placental hemodynamics and the risks of pregnancy complications: The Generation R Study. Am J Epidemiol 177: 743–754, 2013 [DOI] [PubMed] [Google Scholar]
- 12.Gaillard R, Steegers EA, Tiemeier H, Hofman A, Jaddoe VW: Placental vascular dysfunction, fetal and childhood growth, and cardiovascular development: The Generation R Study. Circulation 128: 2202–2210, 2013 [DOI] [PubMed] [Google Scholar]
- 13.Verburg BO, Jaddoe VW, Wladimiroff JW, Hofman A, Witteman JC, Steegers EA: Fetal hemodynamic adaptive changes related to intrauterine growth: The Generation R Study. Circulation 117: 649–659, 2008 [DOI] [PubMed] [Google Scholar]
- 14.Scherjon SA, Kok JH, Oosting H, Wolf H, Zondervan HA: Fetal and neonatal cerebral circulation: A pulsed Doppler study. J Perinat Med 20: 79–82, 1992 [DOI] [PubMed] [Google Scholar]
- 15.Hinchliffe SA, Lynch MR, Sargent PH, Howard CV, Van Velzen D: The effect of intrauterine growth retardation on the development of renal nephrons. Br J Obstet Gynaecol 99: 296–301, 1992 [DOI] [PubMed] [Google Scholar]
- 16.Schreuder MF, van Wijk JA, Delemarre-van de Waal HA: Intrauterine growth restriction increases blood pressure and central pulse pressure measured with telemetry in aging rats. J Hypertens 24: 1337–1343, 2006 [DOI] [PubMed] [Google Scholar]
- 17.Schreuder MF, Van Wijk JA, Fodor M, Delemarre-van de Waal HA: Influence of intrauterine growth restriction on renal function in the adult rat. J Physiol Biochem 63: 213–219, 2007 [DOI] [PubMed] [Google Scholar]
- 18.Hallan S, Euser AM, Irgens LM, Finken MJ, Holmen J, Dekker FW: Effect of intrauterine growth restriction on kidney function at young adult age: The Nord Trøndelag Health (HUNT 2) Study. Am J Kidney Dis 51: 10–20, 2008 [DOI] [PubMed] [Google Scholar]
- 19.Keijzer-Veen MG, Kleinveld HA, Lequin MH, Dekker FW, Nauta J, de Rijke YB, van der Heijden BJ: Renal function and size at young adult age after intrauterine growth restriction and very premature birth. Am J Kidney Dis 50: 542–551, 2007 [DOI] [PubMed] [Google Scholar]
- 20.Moritz KM, Mazzuca MQ, Siebel AL, Mibus A, Arena D, Tare M, Owens JA, Wlodek ME: Uteroplacental insufficiency causes a nephron deficit, modest renal insufficiency but no hypertension with ageing in female rats. J Physiol 587: 2635–2646, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Verburg BO, Geelhoed JJ, Steegers EA, Hofman A, Moll HA, Witteman JC, Jaddoe VW: Fetal kidney volume and its association with growth and blood flow in fetal life: The Generation R Study. Kidney Int 72: 754–761, 2007 [DOI] [PubMed] [Google Scholar]
- 22.Wladimiroff JW, vd Wijngaard JA, Degani S, Noordam MJ, van Eyck J, Tonge HM: Cerebral and umbilical arterial blood flow velocity waveforms in normal and growth-retarded pregnancies. Obstet Gynecol 69: 705–709, 1987 [PubMed] [Google Scholar]
- 23.Di Zazzo G, Stringini G, Matteucci MC, Muraca M, Malena S, Emma F: Serum creatinine levels are significantly influenced by renal size in the normal pediatric population. Clin J Am Soc Nephrol 6: 107–113, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Geelhoed JJ, Verburg BO, Nauta J, Lequin M, Hofman A, Moll HA, Witteman JC, van der Heijden AJ, Steegers EA, Jaddoe VW: Tracking and determinants of kidney size from fetal life until the age of 2 years: The Generation R Study. Am J Kidney Dis 53: 248–258, 2009 [DOI] [PubMed] [Google Scholar]
- 25.Chen X, Wang Y: Tracking of blood pressure from childhood to adulthood: A systematic review and meta-regression analysis. Circulation 117: 3171–3180, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Singh A, Satchell SC: Microalbuminuria: Causes and implications. Pediatr Nephrol 26: 1957–1965, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grigore D, Ojeda NB, Robertson EB, Dawson AS, Huffman CA, Bourassa EA, Speth RC, Brosnihan KB, Alexander BT: Placental insufficiency results in temporal alterations in the renin angiotensin system in male hypertensive growth restricted offspring. Am J Physiol Regul Integr Comp Physiol 293: R804–R811, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Luyckx VA, Brenner BM: The clinical importance of nephron mass. J Am Soc Nephrol 21: 898–910, 2010 [DOI] [PubMed] [Google Scholar]
- 29.Hoy WE, Bertram JF, Denton RD, Zimanyi M, Samuel T, Hughson MD: Nephron number, glomerular volume, renal disease and hypertension. Curr Opin Nephrol Hypertens 17: 258–265, 2008 [DOI] [PubMed] [Google Scholar]
- 30.Andersen TB, Eskild-Jensen A, Frøkiaer J, Brøchner-Mortensen J: Measuring glomerular filtration rate in children; Can cystatin C replace established methods? A review. Pediatr Nephrol 24: 929–941, 2009 [DOI] [PubMed] [Google Scholar]
- 31.de Jong PE, Curhan GC: Screening, monitoring, and treatment of albuminuria: Public health perspectives. J Am Soc Nephrol 17: 2120–2126, 2006 [DOI] [PubMed] [Google Scholar]
- 32.Miller WG, Bruns DE, Hortin GL, Sandberg S, Aakre KM, McQueen MJ, Itoh Y, Lieske JC, Seccombe DW, Jones G, Bunk DM, Curhan GC, Narva AS, National Kidney Disease Education Program-IFCC Working Group on Standardization of Albumin in Urine : Current issues in measurement and reporting of urinary albumin excretion. Clin Chem 55: 24–38, 2009 [DOI] [PubMed] [Google Scholar]
- 33.Jaddoe VW, van Duijn CM, Franco OH, van der Heijden AJ, van Iizendoorn MH, de Jongste JC, van der Lugt A, Mackenbach JP, Moll HA, Raat H, Rivadeneira F, Steegers EA, Tiemeier H, Uitterlinden AG, Verhulst FC, Hofman A: The Generation R Study: Design and cohort update 2012. Eur J Epidemiol 27: 739–756, 2012 [DOI] [PubMed] [Google Scholar]
- 34.Verburg BO, Steegers EA, De Ridder M, Snijders RJ, Smith E, Hofman A, Moll HA, Jaddoe VW, Witteman JC: New charts for ultrasound dating of pregnancy and assessment of fetal growth: Longitudinal data from a population-based cohort study. Ultrasound Obstet Gynecol 31: 388–396, 2008 [DOI] [PubMed] [Google Scholar]
- 35.Hadlock FP, Harrist RB, Carpenter RJ, Deter RL, Park SK: Sonographic estimation of fetal weight. The value of femur length in addition to head and abdomen measurements. Radiology 150: 535–540, 1984 [DOI] [PubMed] [Google Scholar]
- 36.Albaiges G, Missfelder-Lobos H, Parra M, Lees C, Cooper D, Nicolaides KH: Comparison of color Doppler uterine artery indices in a population at high risk for adverse outcome at 24 weeks’ gestation. Ultrasound Obstet Gynecol 21: 170–173, 2003 [DOI] [PubMed] [Google Scholar]
- 37.Ebbing C, Rasmussen S, Kiserud T: Middle cerebral artery blood flow velocities and pulsatility index and the cerebroplacental pulsatility ratio: Longitudinal reference ranges and terms for serial measurements. Ultrasound Obstet Gynecol 30: 287–296, 2007 [DOI] [PubMed] [Google Scholar]
- 38.Jeanty P, Dramaix-Wilmet M, Elkhazen N, Hubinont C, van Regemorter N: Measurements of fetal kidney growth on ultrasound. Radiology 144: 159–162, 1982 [DOI] [PubMed] [Google Scholar]
- 39.Geelhoed JJ, Taal HR, Steegers EA, Arends LR, Lequin M, Moll HA, Hofman A, van der Heijden AJ, Jaddoe VW: Kidney growth curves in healthy children from the third trimester of pregnancy until the age of two years. The Generation R Study. Pediatr Nephrol 25: 289–298, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Geelhoed JJ, Kleyburg-Linkers VE, Snijders SP, Lequin M, Nauta J, Steegers EA, van der Heijden AJ, Jaddoe VW: Reliability of renal ultrasound measurements in children. Pediatr Nephrol 24: 1345–1353, 2009 [DOI] [PubMed] [Google Scholar]
- 41.Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL: New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20: 629–637, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Donaghue KC, Chiarelli F, Trotta D, Allgrove J, Dahl-Jorgensen K, International Society for Pediatric and Adolescent Diabetes : ISPAD Clinical Practice Consensus Guidelines 2006-2007. Microvascular and macrovascular complications. Pediatr Diabetes 8: 163–170, 2007 [DOI] [PubMed] [Google Scholar]
- 43.Wong SN, Tz Sung RY, Leung LC: Validation of three oscillometric blood pressure devices against auscultatory mercury sphygmomanometer in children. Blood Press Monit 11: 281–291, 2006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.