Abstract
Nephrotic syndrome is recognized by the presence of proteinuria in excess of 3.5 g/24 h along with hypoalbuminemia, edema, hyperlipidemia (hypertriglyceridemia and hypercholesterolemia), and lipiduria. Each component has been investigated individually over the past four decades with some success. Studies published recently have started unraveling the molecular basis of proteinuria and its relationship with other components. We now have improved understanding of the threshold for nephrotic-range proteinuria and the pathogenesis of hypertriglyceridemia. These studies reveal that modifying sialylation of the soluble glycoprotein angiopoietin-like 4 or changing key amino acids in its sequence can be used successfully to treat proteinuria. Treatment strategies on the basis of fundamental relationships among different components of nephrotic syndrome use naturally occurring pathways and have great potential for future development into clinically relevant therapeutic agents.
Keywords: podocyte, nephrotic syndrome, proteinuria, lipids, FSGS, diabetic nephropathy
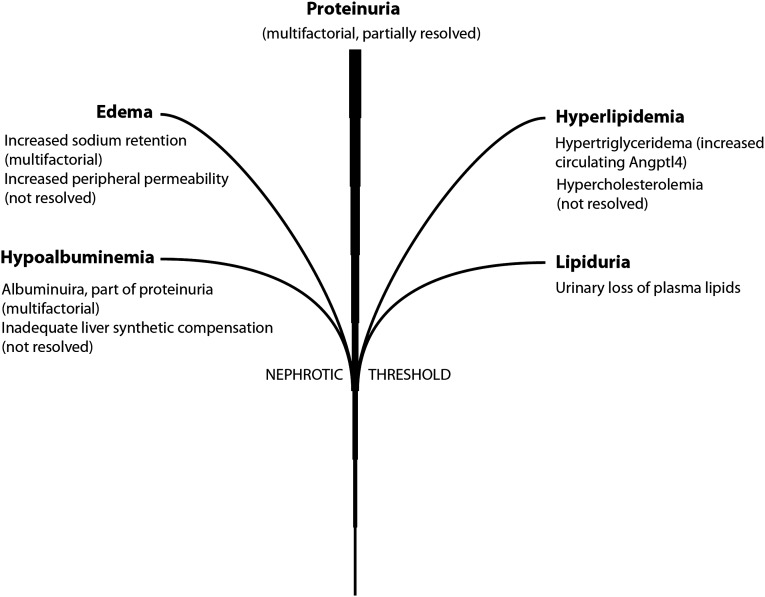
Nephrotic syndrome is a hallmark of glomerular disease and characterized by the presence of proteinuria in excess of 3.5 g/24 h, hypoalbuminemia, and variable amounts of hyperlipidemia (hypertriglyceridemia and hypercholesterolemia), lipiduria, and edema1 (Figure 1). In children, nephrotic-range proteinuria is defined by urinary protein excretion rates >40 mg/h per meter2. Patients with primary glomerular diseases (e.g., minimal change disease [MCD], FSGS, and membranous nephropathy) and systemic disorders (e.g., diabetes mellitus, systemic lupus erythematosis, and amyloidosis) can present with nephrotic syndrome. The principle driving force in nephrotic syndrome is proteinuria, because other components develop only after proteinuria reaches a certain threshold. Substantial research effort has been committed to understanding the pathogenesis of each individual component. The purpose of this review is to discuss in broad terms what is understood about each component and then consider what remains to be investigated. Next, molecular connections, if known, between proteinuria and the other components will be discussed. Finally, novel therapeutic strategies derived from the study of nephrotic syndrome will be outlined.
Figure 1.
The nephrotic syndrome tree is shown. The trunk depicts increasing proteinuria, and the branches represent other components that appear when proteinuria crosses the nephrotic-range threshold.
Proteinuria
Several genes expressed in podocytes have now been directly or indirectly implicated in the pathogenesis of proteinuria. They can be classified as slit diaphragm-related, cell matrix interface–related, cytoskeleton-related, podocyte surface proteins, transcriptional factors, and podocyte-secreted proteins.2 Many of the structural proteins among these categories were discovered when screening for mutations in patients with disease (e.g., nephrin for congenital nephrotic syndrome of the Finnish type3 and podocin for FSGS4). These genes are best viewed as disease-related genes, with proteinuria being a major component of the associated disease. Others were discovered through mutagenesis studies in mice (e.g., neph1).5,6 In most cases, these genes do not single-handedly explain the development of proteinuria. Transcriptional factors, like WT1, came into light from a combination of genetics7 and animal model8 studies, whereas the role of ZHX proteins was discovered through differential gene expression studies in animal models.2,9 Among podocyte-secreted proteins implicated in human disease, the roles of angiopoietin-like 4 (Angptl4) and vascular endothelial growth factor in proteinuria were established through the study of experimental models.10–12 A hyposialylated form of Angptl4 secreted from podocytes is directly implicated in the pathogenesis of proteinuria in MCD and accounts for most of the cardinal manifestations of this disease, including glucocorticoid sensitivity, selective proteinuria, loss of glomerular basement membrane (GBM) charge, and classic morphologic changes.1,11 Despite demonstration that loss of GBM charge in MCD is caused by binding of Angptl4, it is not known whether complex interaction of this protein with heparan sulfate proteoglycans and other GBM proteins or actual loss of GBM charge is responsible for proteinuria. Vascular endothelial growth factor has been implicated in human thrombotic microangiopathy.13 The added dimension of podocyte-secreted proteins is their ability to reach out to binding partners on the surface of glomerular endothelial cells and potentially participate in feedback loops within the glomerulus.14 In addition to podocyte-secreted proteins, high plasma levels of the soluble urokinase receptor are being investigated for their role in the pathogenesis of FSGS.15
A new dimension recently added to this field is the systemic response to proteinuria when it reaches nephrotic range. A circulating sialylated form of Angptl4 secreted predominantly from adipose tissue, skeletal muscle, and heart reduces proteinuria, at least in part, by binding to glomerular endothelial αvβ5 integrin.12 Thematically, it opens up a new area of investigation to study how other organs reduce established proteinuria by secreting proteins into the circulation. Angptl4 is the first of several such proteins that are likely to be identified in the future.
Edema
The onset of edema in nephrotic syndrome occupies a clinical spectrum that varies from subacute to acute onset in many patients with FSGS or membranous nephropathy, explosive onset (often overnight) in MCD, and complete absence in many patients with HIV-related collapsing glomerulopathy. From a pathophysiology standpoint, edema requires a combination of hypoalbuminemia, renal salt retention, and increased peripheral capillary permeability, because there are numerous clinical situations involving a single component that are not associated with edema. The variability of edema in different clinical situations may be directly related to differences between these pathogenic components. The best studied aspect and indeed, the primary target of diuretic therapy is renal tubular salt retention.16 In order of diuretic efficacy, transporters in the thick ascending loop of Henle, distal tubule, collecting duct, and proximal tubule have been targeted to reduce edema. Recent studies suggest that the proteolytic activation of collecting duct epithelial sodium channel may be mediated by plasmin converted from filtered plasminogen.17,18 Treatment of edema with albumin infusions is generally not practiced, except in selected cases of refractory anasarca. Perhaps the least understood part of edema is increased peripheral capillary permeability, and no current therapy targets this aspect. This area has tremendous potential for investigation, and mechanistic studies may reveal useful clues for treating patients with refractory edema. Investigating the explosive onset of edema in MCD could provide insight into additional molecular mechanisms in nephrotic syndrome, because there is a potential for glomerular or peripherally secreted proteins in the pathogenesis of this phenomenon.
Hypercholesterolemia
Nephrotic patients have elevated total and LDL cholesterol levels, largely related to an acquired LDL receptor deficiency, which limits the removal of cholesterol-rich LDL particles from the circulation.19 This reduction in uptake of extracellular cholesterol stimulates cholesterol biosynthesis by upregulating hepatic 3-hydroxy-3-methyl glutaryl-CoA reductase expression and activity in the nephrotic liver. Increased hepatic activity of Acyl-CoA cholesterol acyltransferase-2, an enzyme responsible for esterification of cholesterol, is also noted. Presence of normal LDL receptor mRNA expression in the nephrotic liver suggests a post-transcriptional etiology. A recent study in experimental animals suggests that increased hepatic degradation of the LDL receptor by proprotein convertase subtilisin/kexin type 9 and inducible degrader of the LDL receptor may be involved.20 Also, urinary loss of plasma proteins like lecithin–cholesterol acyltransferase may also contribute to hypercholesterolemia. However, the precise sequence of events and the molecular relationship of these changes with proteinuria remain unknown.
Hypertriglyceridemia
Hypertriglyceridemia results from impaired clearance of triglycerides in very low-density lipoprotein and chylomicrons because of inactivation of endothelium-bound lipoprotein lipase (LPL) activity by the circulating glycoprotein Angptl4, which reduces the conversion of circulating triglycerides to free fatty acids (FFAs).12 Circulating sialylated Angptl4 is mostly secreted from skeletal muscle, adipose tissue, and heart to reduce proteinuria through glomerular endothelial binding, but it also causes hypertriglyceridemia as a side effect. Interaction of Angptl4 with LPL converts the active dimeric form of this protein into inactive monomers. Both dimers and monomers of LPL are lost in the urine in nephrotic syndrome. Proteinuria and hypertriglyceridemia are linked by two negative feedback loops, which are discussed below.
Hypoalbuminemia
Hypoalbuminemia results from urinary losses of albumin during proteinuria, insufficient compensation by hepatic synthesis, and perhaps, increased albumin catabolism. The major enigma in the pathogenesis of hypoalbuminemia is the inability of the nephrotic liver to increase albumin synthesis to compensate for urinary losses, although a normal liver synthesizes 12–14 g albumin/d and can increase production 3-fold in times of demand.21 Whereas a lot of importance was traditionally placed on reduced plasma oncotic pressure resulting from hypoalbuminemia, it has now become clear that changes in FFA binding to albumin are equally important.12 Plasma FFAs are noncovalently bound to albumin through six high-affinity sites and several low-affinity sites.14 During proteinuria, patients lose, for unclear reasons, albumin with lower FFA content, resulting in the accumulation of albumin with higher FFA content.12,22,23 This loss, along with the development of hypoalbuminemia, results in a high plasma FFA-to-albumin ratio, which in turn, drives FFA uptake in skeletal muscle, heart, and adipose tissue.12 This event is primarily responsible for the development of hypertriglyceridemia and as discussed below, an attempt of these organs to reduce proteinuria through the secretion of Angptl4 into the circulation.
Lipiduria
Lipiduria is thought to be secondary to hyperlipidemia, and it mostly results from filtration of HDL particles because of their relatively small size.24 These lipids are found in oval fat bodies (sloughed tubular cells with lipids), fatty casts, or free-floating lipid globules. Components that have high amounts of esterified cholesterol have a Maltese cross appearance under polarized light.
Molecular Links between Proteinuria and Other Components of Nephrotic Syndrome
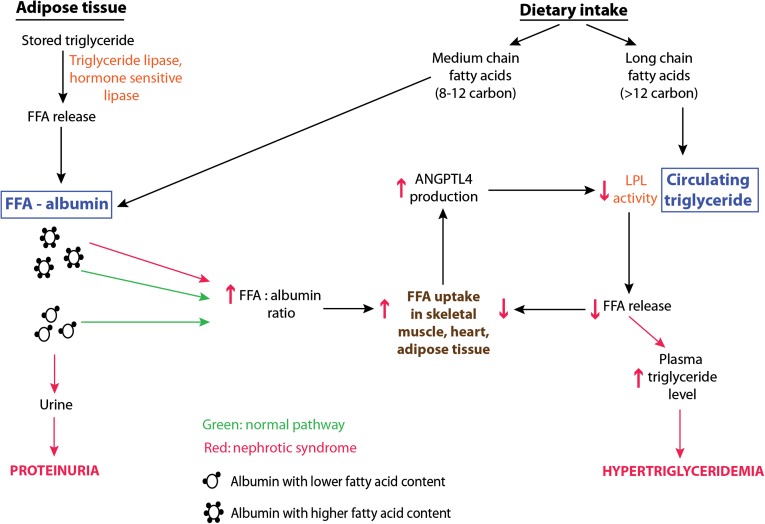
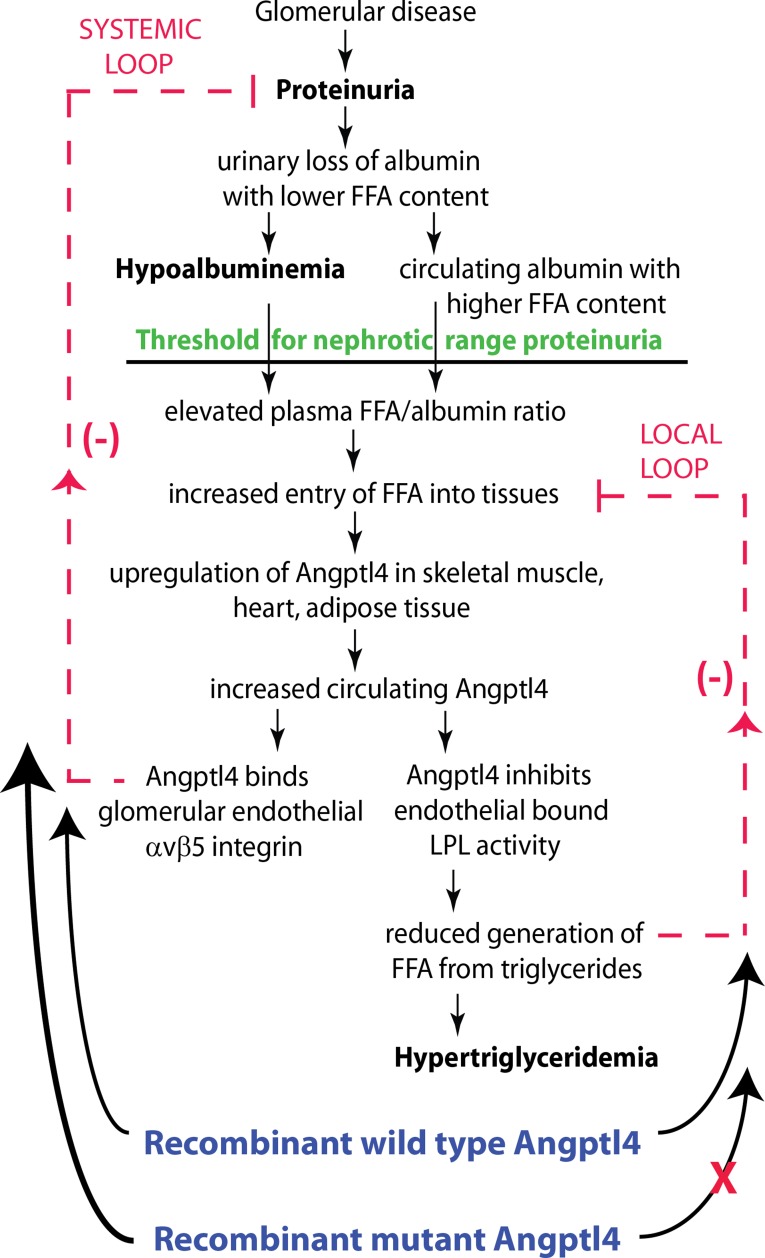
There are large gaps of knowledge in our understanding of the molecular relationship between proteinuria, the primary driver in nephrotic syndrome, and most of the other components. Only the link between proteinuria and hypertriglyceridemia has been clearly elucidated.12,14 This relationship is strongly influenced by the link between FFA and albumin. FFAs are a major fuel source for skeletal muscle and heart, and they are stored in adipose tissue as triglycerides. Under normal conditions, FFA uptake in these organs relies on a combination of FFA released by LPL-mediated hydrolysis of circulating triglyceride and albumin-bound FFAs that are derived from diet (medium-chain FFA) or lipolysis of stored triglyceride in adipose tissue in the fasting state (Figure 2). These organs also have high expression for LPL, Angptl4, and peroxisome proliferator-activated receptor (PPAR) family members, which regulate Angptl4 expression in response to FFA uptake. In nephrotic syndrome, there is urinary loss of albumin with low FFA content, leading to retention of albumin with high FFA content, which alters the FFA uptake balance in favor of albumin-bound FFA. Increase in uptake of albumin-bound FFA induces local Angptl4 upregulation, likely through PPARs, which then inactivates LPL in the same tissues, leading to reduction in the formation of FFA from triglycerides and consequently, hypertriglyceridemia. This change in balance between two sources of FFA can be viewed as a product of a local negative feedback loop (Figure 3). However, this local feedback loop is subservient to a much larger systemic negative feedback loop to reduce proteinuria. Indeed, Angptl4 released from the skeletal muscle, heart, and adipose tissue into the circulation also binds to glomerular endothelial αvβ5 integrin to reduce proteinuria. Patients with all causes of nephrotic syndrome studied have elevated plasma Angptl4 levels.12 Studies in diabetic rats using low doses of recombinant human Angptl4 suggest a lower threshold to participate in the systemic rather than the local feedback loop. Overall, it seems that the local feedback loop reduces the effectiveness of the systemic feedback loop by limiting the extent of Angptl4 upregulation. Overall, the antiproteinuric and hypertriglyceridemia-inducing effects of Angptl4 are dependent on high uptake of albumin-bound FFA in peripheral organs and indirectly dependent on disproportionate retention of albumin with high FFA content in nephrotic syndrome.
Figure 2.
Schematic illustration of the two sources of FFA available for uptake by skeletal muscle, heart, and adipose tissue in the normal and nephrotic state. Green shows normal conditions, and red illustrates changes in nephrotic syndrome. The balance shifts significantly to albumin-bound FFA because of retention of albumin with high FFA content in nephrotic syndrome. Angptl4 secreted from these organs reduces the conversion of triglycerides to FFA by inactivating LPL, thereby reducing use of triglycerides and resulting in hypertriglyceridemia.
Figure 3.
Schematic illustration of negative feedback loops in the link between proteinuria, hypoalbuminemia, and hypertriglyceridemia mediated by Angptl4 and FFA. Plasma FFAs are noncovalently bound to albumin. Because of the preferential loss of albumin with low FFA content in nephrotic syndrome, there is a relative increase in circulating albumin with higher FFA content. Because glomerular disease progresses to severe proteinuria, hypoalbuminemia develops, and the combination of high albumin FFA content and lower plasma albumin levels increases the FFA-to-albumin ratio. It promotes entry of FFA into skeletal muscle, heart, and adipose tissue, which causes upregulation of Angptl4 at least partially mediated by PPARs. Angptl4 secreted from these organs participates in two feedback loops. In the systemic loop, it binds to glomerular endothelial αvβ5 integrin and reduces proteinuria. In a local loop, it inactivates LPL in the same organs from which it is secreted to reduce the uptake of FFA, thereby curtailing a stimulus for its own upregulation. Reproduced from reference 14, with permission.
Molecular Basis for Nephrotic-Range Proteinuria Threshold
Patients do not start manifesting the other components of nephrotic syndrome until they cross the nephrotic-range proteinuria threshold, which is usually defined as about 3.5 g/d in adults, but it is likely to be quite variable between different individuals and within the same individual among different components. Until recently, the molecular basis for this threshold was not known. It is, at present, only possible to explain the nephrotic threshold in the context of hypertriglyceridemia.12 Hypertriglyceridemia is dependent on the retention of albumin with high FFA content, resulting in a plasma FFA-to-albumin ratio that is high enough to induce upregulation of Angptl4 expression in skeletal muscle, heart, and adipose tissue. Studies in experimental animals reveal that, during mild proteinuria, plasma FFA-to-albumin ratio, plasma Angptl4 levels, peripheral organ Angptl4, and PPAR mRNA expression are similar to control nonproteinuric animals. During severe proteinuria, all these parameters are significantly elevated, suggesting that the threshold for nephrotic-range proteinuria, in the context of hypertriglyceridemia, correlates with the downstream effects of an increased plasma FFA-to-albumin ratio.
Therapeutic Strategies Developed from the Study of Nephrotic Syndrome
A central role played by Angptl4 in nephrotic syndrome makes it suitable as a therapeutic agent as well as a target.14,25 An important lesson learned from Angptl4 is its “Jekyll and Hyde” effect, because the same protein can have very different biologic effects on the basis of the presence or absence of sialic acid residues and the compartment in which it is secreted. Because circulating sialylated Angptl4 has an antiproteinuric effect, it is conceivable that injecting recombinant human Angptl4 or increasing the secretion of native Angptl4 from heart, skeletal muscle, and adipose tissue using PPAR agonists, glucocorticoids, FFA supplements, or β-adrenergic agonists could be of potential benefit in reducing proteinuria through the systemic feedback loop. However, these interventions run the risk of aggravating hypertriglyceridemia through the local feedback loop and could also reduce FFA uptake in the heart and skeletal muscle to below a threshold for organ dysfunction. In addition, all the drugs mentioned above have multiple side effects. Mutating Angptl4 at amino acid 40 or 39 to reduce its interaction with LPL bypasses the local feedback loop and allows for mutant recombinant human Angptl4 to very significantly reduce proteinuria in nephrotic animals with FSGS or diabetic nephropathy without affecting plasma triglyceride levels.12 This strategy is a novel futuristic treatment for all etiologies of proteinuria and nephrotic syndrome, especially if studies on the long-term administration of mutant human Angptl4 currently in progress also show improvement in the progression of CKD.
It is also clear that podocyte-secreted hyposialylated Angptl4 mediates proteinuria in MCD1,11 and also contributes to proteinuria in diabetic nephropathy.14 The effects of hyposialylated Angptl4 are most likely related to its binding to the GBM,11 but adverse consequences of glomerular endothelial binding are also possible.12 Converting hyposialylated Angptl4 to sialylated protein using N-acetyl-d-manosamine, a precursor of sialic acid that can be taken up and stored in podocytes, very significantly reduces proteinuria and has the potential for use in small maintenance doses to prevent relapse in MCD and as maintenance therapy for diabetic nephropathy.14
Future Interventions on the Basis of the Study of Nephrotic Syndrome
The proteinuria–hypertriglyceridemia relationship shows that other organs in the body make an attempt to reduce proteinuria by secreting specific proteins. This area of investigation would benefit from additional clinical studies in the future. Perhaps other unresolved or partially resolved components of nephrotic syndrome may also result from a similar systemic response involving other putative proteins. Identifying and modifying this circulating glomerulophilic proteome may hold the key to developing additional novel therapies for proteinuric kidney disease in the future.
Disclosures
S.S.C. is Founder, President, and Chief Executive Officer of GDTHERAPY LLC and filed patents related to the use of Angptl4 mutants (PCT/US2011/039255) and precursors of sialic acid, including N-acetyl-d-manosamine (PCT/US2011/039058), for the treatment of nephrotic syndrome. He may benefit financially from these patents in the future. C.M. declares no competing financial interests.
Acknowledgments
This work was supported by National Institutes of Health Grants T32-DK007545 (to C.M.), R01-DK077073 (to S.S.C.), R01-DK090035 (to S.S.C.), and R01-DK101637 (to S.S.C.).
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
References
- 1.Chugh SS, Clement LC, Macé C: New insights into human minimal change disease: Lessons from animal models. Am J Kidney Dis 59: 284–292, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clement LC, Liu G, Perez-Torres I, Kanwar YS, Avila-Casado C, Chugh SS: Early changes in gene expression that influence the course of primary glomerular disease. Kidney Int 72: 337–347, 2007 [DOI] [PubMed] [Google Scholar]
- 3.Kestilä M, Lenkkeri U, Männikkö M, Lamerdin J, McCready P, Putaala H, Ruotsalainen V, Morita T, Nissinen M, Herva R, Kashtan CE, Peltonen L, Holmberg C, Olsen A, Tryggvason K: Positionally cloned gene for a novel glomerular protein—nephrin—is mutated in congenital nephrotic syndrome. Mol Cell 1: 575–582, 1998 [DOI] [PubMed] [Google Scholar]
- 4.Boute N, Gribouval O, Roselli S, Benessy F, Lee H, Fuchshuber A, Dahan K, Gubler MC, Niaudet P, Antignac C: NPHS2, encoding the glomerular protein podocin, is mutated in autosomal recessive steroid-resistant nephrotic syndrome. Nat Genet 24: 349–354, 2000 [DOI] [PubMed] [Google Scholar]
- 5.Donoviel DB, Freed DD, Vogel H, Potter DG, Hawkins E, Barrish JP, Mathur BN, Turner CA, Geske R, Montgomery CA, Starbuck M, Brandt M, Gupta A, Ramirez-Solis R, Zambrowicz BP, Powell DR: Proteinuria and perinatal lethality in mice lacking NEPH1, a novel protein with homology to NEPHRIN. Mol Cell Biol 21: 4829–4836, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu G, Kaw B, Kurfis J, Rahmanuddin S, Kanwar YS, Chugh SS: Neph1 and nephrin interaction in the slit diaphragm is an important determinant of glomerular permeability. J Clin Invest 112: 209–221, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pelletier J, Bruening W, Kashtan CE, Mauer SM, Manivel JC, Striegel JE, Houghton DC, Junien C, Habib R, Fouser L, Fine RN, Silverman BL, Haber DA, Housman D: Germline mutations in the Wilms’ tumor suppressor gene are associated with abnormal urogenital development in Denys-Drash syndrome. Cell 67: 437–447, 1991 [DOI] [PubMed] [Google Scholar]
- 8.Barisoni L, Bruggeman LA, Mundel P, D’Agati VD, Klotman PE: HIV-1 induces renal epithelial dedifferentiation in a transgenic model of HIV-associated nephropathy. Kidney Int 58: 173–181, 2000 [DOI] [PubMed] [Google Scholar]
- 9.Liu G, Clement LC, Kanwar YS, Avila-Casado C, Chugh SS: ZHX proteins regulate podocyte gene expression during the development of nephrotic syndrome. J Biol Chem 281: 39681–39692, 2006 [DOI] [PubMed] [Google Scholar]
- 10.Eremina V, Sood M, Haigh J, Nagy A, Lajoie G, Ferrara N, Gerber HP, Kikkawa Y, Miner JH, Quaggin SE: Glomerular-specific alterations of VEGF-A expression lead to distinct congenital and acquired renal diseases. J Clin Invest 111: 707–716, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clement LC, Avila-Casado C, Macé C, Soria E, Bakker WW, Kersten S, Chugh SS: Podocyte-secreted angiopoietin-like-4 mediates proteinuria in glucocorticoid-sensitive nephrotic syndrome. Nat Med 17: 117–122, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clement LC, Macé C, Avila-Casado C, Joles JA, Kersten S, Chugh SS: Circulating angiopoietin-like 4 links proteinuria with hypertriglyceridemia in nephrotic syndrome. Nat Med 20: 37–46, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eremina V, Jefferson JA, Kowalewska J, Hochster H, Haas M, Weisstuch J, Richardson C, Kopp JB, Kabir MG, Backx PH, Gerber HP, Ferrara N, Barisoni L, Alpers CE, Quaggin SE: VEGF inhibition and renal thrombotic microangiopathy. N Engl J Med 358: 1129–1136, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chugh SS, Macé C, Clement LC, Del Nogal Avila M, Marshall CB: Angiopoietin-like 4 based therapeutics for proteinuria and kidney disease. Front Pharmacol 5: 23, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wei C, El Hindi S, Li J, Fornoni A, Goes N, Sageshima J, Maiguel D, Karumanchi SA, Yap HK, Saleem M, Zhang Q, Nikolic B, Chaudhuri A, Daftarian P, Salido E, Torres A, Salifu M, Sarwal MM, Schaefer F, Morath C, Schwenger V, Zeier M, Gupta V, Roth D, Rastaldi MP, Burke G, Ruiz P, Reiser J: Circulating urokinase receptor as a cause of focal segmental glomerulosclerosis. Nat Med 17: 952–960, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamm LL, Batuman V: Edema in the nephrotic syndrome: New aspect of an old enigma. J Am Soc Nephrol 14: 3288–3289, 2003 [DOI] [PubMed] [Google Scholar]
- 17.Passero CJ, Mueller GM, Rondon-Berrios H, Tofovic SP, Hughey RP, Kleyman TR: Plasmin activates epithelial Na+ channels by cleaving the gamma subunit. J Biol Chem 283: 36586–36591, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Svenningsen P, Bistrup C, Friis UG, Bertog M, Haerteis S, Krueger B, Stubbe J, Jensen ON, Thiesson HC, Uhrenholt TR, Jespersen B, Jensen BL, Korbmacher C, Skøtt O: Plasmin in nephrotic urine activates the epithelial sodium channel. J Am Soc Nephrol 20: 299–310, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vaziri ND: Molecular mechanisms of lipid disorders in nephrotic syndrome. Kidney Int 63: 1964–1976, 2003 [DOI] [PubMed] [Google Scholar]
- 20.Jin K, Park BS, Kim YW, Vaziri ND: Plasma PCSK9 in nephrotic syndrome and in peritoneal dialysis: A cross-sectional study. Am J Kidney Dis 63: 584–589, 2014 [DOI] [PubMed] [Google Scholar]
- 21.Rothschild MA, Oratz M, Schreiber SS: Albumin synthesis. 1. N Engl J Med 286: 748–757, 1972 [DOI] [PubMed] [Google Scholar]
- 22.Ghiggeri GM, Ginevri F, Candiano G, Oleggini R, Perfumo F, Queirolo C, Gusmano R: Characterization of cationic albumin in minimal change nephropathy. Kidney Int 32: 547–553, 1987 [DOI] [PubMed] [Google Scholar]
- 23.Lerique B, Moulin B, Delpero C, Purgus R, Olmer M, Boyer J: High-affinity interaction of long-chain fatty acids with serum albumin in nephrotic syndrome. Clin Sci (Lond) 89: 417–420, 1995 [DOI] [PubMed] [Google Scholar]
- 24.Blackburn V, Grignani S, Fogazzi GB: Lipiduria as seen by transmission electron microscopy. Nephrol Dial Transplant 13: 2682–2684, 1998 [DOI] [PubMed] [Google Scholar]
- 25.Kirk R: Nephrotic syndrome: Negative feedback loop reveals novel potential therapy. Nat Rev Nephrol 10: 63, 2014 [DOI] [PubMed] [Google Scholar]