Abstract
Background
This prospective analysis evaluated the efficacy of a contingency management (CM) intervention to improve the psychological health of non-treatment seeking, homeless, substance-dependent, men who have sex with men in Los Angeles. It was hypothesized that administration of CM would be associated with reductions in participants’ symptoms of psychological and emotional distress.
Methods
One hundred and thirty-one participants were randomized into either a voucher-based contingency management (CM; n = 64) condition reinforcing substance abstinence and prosocial/health-promoting behaviors, or to a control condition (n = 67). Participants’ symptoms of psychological and emotional distress were assessed at intake and at 12-months post-randomization.
Results
Participants randomized into the CM intervention exhibited significantly lower levels of psychological distress in all measured symptom domains up to one year post randomization, reductions not evidenced in the control arm. Omnibus tests resultant from seemingly unrelated regression analysis confirmed that CM was significantly associated with reductions in symptoms of psychological and emotional distress, even when controlling for biomarker-confirmed substance use outcomes (χ2(9) = 17.26; p < 0.05).
Conclusions
Findings demonstrate that a CM intervention reduced symptoms of psychological and emotional distress among a sample of non-treatment seeking, homeless, substance-dependent men who have sex with men.
Keywords: Contingency Management, Homeless, Dual Diagnosis, Substance Use, MSM, Psychological Distress
Introduction
Men who have sex with men (MSM), homeless individuals, and those with a substance use disorder all demonstrate increased levels of psychological distress when compared to other populations (Herrell et al., 1999; Cochran and Mays 2000a; Cochran and Mays 2000b; Sandfort, de Graff, Bijl, and Schnabel, 2001; Slade, Grove, and Burgess 2011; Nguyen, Liu, Hernandez, and Stinson 2012). Psychological distress has been associated with both initiation of and relapse into substance use (Castellani, Wedgeworth, Wootton, & Rugle, 1997; Daughters, Lejuez, Kahler, Strong, & Brown, 2005; Laudet, Becker, & White, 2009; Hassel, Nordfjærn, and Hagen 2013) making improved psychological health an important goal for interventions promoting substance abstinence. Recent evidence suggests that contingency management (CM) interventions designed to reduce substance use may also work to reduce symptoms of psychological and emotional distress (McDonell et al. 2013; Petry, Alessi, and Rash 2013).
Contingency Management Interventions
Contingency management interventions rely on principles of operant conditioning (Skinner, 1953) to instill and sustain targeted behaviors, directly pitting the reinforcing value of non-drug reinforcers against the reinforcing value of the substance(s) of abuse. To be effective, the positive reinforcement schedule of a CM intervention must be powerful enough to override the positive reinforcement provided by the euphoric effects of drug use, the activities associated with such euphoria, and/or other reinforcing drug effects. Contingency management interventions have shown both short-term and sustained efficacy in reducing substance use and increasing health-promoting behaviors among MSM (Reback et al. 2010), and have reduced substance use among the homeless (Schumacher et al. 2007; Tracy et al. 2007) and the dually diagnosed (Messina, Farabee, & Rawson, 2003; Drake, O’Neal, & Wallach, 2008; Mancino, McGaugh, Feldman, Poling, & Oliveto, 2010).
Furthermore, in contrast to the common finding that treatment outcomes for substance abuse and dependence are diminished among those with greater severity of psychiatric symptoms and among those with concomitant psychiatric disorders (Charney, Palacios-Boix, Negrete, Dobkin, & Gill, 2005; Compton, Cottler, Jacobs, Ben-Abdallah, & Spitznagel, 2003), CM is associated with greater reductions in substance use and increased retention rates in participants with high psychiatric severity compared to standard treatment (Weinstock, Alessi, & Petry, 2007). CM has also demonstrated efficacy compared to standard substance abuse treatments in producing abstinence among drug abusers with comorbid psychiatric condition(s) (Drake, O’Neal, & Wallach, 2008), with particularly strong findings for cocaine- and opioid-dependent individuals with post-traumatic stress disorder (Mancino et al., 2010) cocaine abusers with antisocial personality disorder (Messina et al., 2003), and substance-dependent, homeless MSM with antisocial personality disorder (Fletcher & Reback 2013).
Contingency Management and Psychological Health
Studies of CM interventions promoting substance abstinence have reported concomitant reductions in symptoms of psychological distress (e.g., Higgins et al. 2003) even though improvement in psychological distress has never been a targeted outcome. In a sample of stimulant-dependent participants with comorbid serious mental illness, those randomized to receive CM showed significant improvements across multiple symptom domains and were less likely to report psychiatric hospitalizations when compared to the non-contingent control group (McDonell et al. 2013). The observed reductions in psychological symptoms did not persist through follow-up, however, and no attempt was made to control for reductions in stimulant use achieved during the intervention. Another recent study revealed significant reductions in psychological symptoms for participants randomized to receive CM, improvements that were sustained through 9-month follow-up (Petry, Alessi, and Rash 2013). In this instance, substance use was shown to mediate the association between the CM interventions and the reductions in psychological distress.
Questions remain as to whether CM interventions can produce improvements in psychological health, or if the observed reductions in symptom complaints are epiphenomenal to substance use (or other) outcomes. Furthermore, the mechanism underlying any association between CM and symptoms of psychological and emotional distress is currently unspecified. In pursuit of such a mechanism, this prospective analysis sought to examine whether the positive reinforcers administered during a CM intervention could mitigate psychological complaints in a sample of homeless, substance-dependent MSM. It was predicted that random assignment to receive CM would be associated with reductions in participants’ symptoms of psychological and emotional distress.
Method
Participants
Participants were recruited from a community-based, low-intensity, health education/risk reduction HIV prevention program serving homeless, substance-using MSM in the Hollywood/West Hollywood area of LAC. Primary outcomes are reported elsewhere (Reback et al., 2010). Eligibility criteria were active participants in the HIV prevention program, as defined by verified attendance in a minimum of three groups or counseling sessions; at least 18 years of age; substance-dependent verified by the Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, 1996); non-treatment seeking; homeless; and self-reported sex with a man in the previous 12 months. Exclusion criteria were: inability to provide informed consent or display understanding of the study procedures, or having a serious and untreated psychiatric condition (i.e., unmedicated psychosis or mania). Participant sociodemographic characteristics are presented in Table 1.
Table 1.
Participant Demographic Characteristics (N = 131)
| Characteristic | CM (n = 64) n (%) or Median (range) |
Control (n = 67) n (%) or Median (range) |
Total (N = 131) n (%) or Median (range) |
|---|---|---|---|
| Race/Ethnicity | |||
| Caucasian/white | 35 (54.7%) | 35 (52.2%) | 70 (53.4%) |
| Non-Caucasian/white | 29 (45.3%) | 32 (47.8%) | 61 (46.6%) |
| HIV-Status | |||
| HIV-positive | 17 (26.6%) | 20 (29.9%) | 37 (28.3%) |
| Age | |||
| Years | 36 (20–60) | 37 (21–58) | 37 (20–60) |
Procedures
Friends Research Institute’s Institutional Review Board provided oversight for all study activities. Participants were recruited from April 2005 through February 2008 using flyers available at the community site, and through word of mouth. Once potential participants provided consent, intake interviews were conducted to determine study eligibility and collect baseline data (e.g., sociodemographics, recent substance use, psychological health). All potential participants received a $50 gift certificate to a local retail or grocery store. Following intake and consent, participants were randomized into either a CM or control condition for a 24-week intervention with follow-up evaluations at 7, 9, and 12 months. Participants also received a $50 gift certificate for completing each 7-, 9-, and 12-month follow-up assessment.
Intervention
All participants attended twice-weekly visits in which they provided urine and breathalyzer data for abstinence biomarker testing. Participants in both conditions earned voucher points for attending scheduled study visits and HIV prevention program activities. Participants could earn a maximum of 364 points (equivalent to $364 in purchases at the onsite store) if they completed all study and service program activities.
Those randomized into the CM condition earned additional voucher points for engaging in targeted, verifiable health-promoting/prosocial behaviors (e.g., scheduling an appointment with a healthcare provider or social services agency, volunteering or doing community service, seeking or gaining employment, enrolling in a GED program) and for substance abstinence. Points were awarded for urinalysis-/breathalyzer-confirmed abstinence from amphetamine, methamphetamine, PCP, and cocaine metabolites, and breath alcohol measured < 0.05. Study procedures, interventions, and primary outcomes are described more fully elsewhere (Reback et al., 2010).
Measures
Psychiatric and Substance Use Disorders
The SCID was administered as one of the baseline screening measures to determine substance dependence, mood, anxiety, thought and/or antisocial personality disorder(s).
Substance Abstinence
Urine drug screens using a six-panel Food and Drug Administration-approved urinalysis test (Accutest, JANT Pharmacal, Inc.) and an alcohol breathalyzer test (Alco-Sensor III, Intoximeters Inc.) were administered at all study visits. Urine was screened for amphetamines, methamphetamine, cocaine, PCP, THC, and opiate metabolites; breathalyzer tested for alcohol consumption. Substance use testing occurred twice weekly on two nonconsecutive days and results were provided to participants during the same visit. Participants were defined as abstinent for any specific visit if their urine samples were free of metabolites for methamphetamine, cocaine, amphetamines, and PCP, and their breathalyzer results indicated a blood alcohol level less than 0.05. Participants were labeled as either abstinent or non-abstinent for each study visit attended. Participants who failed to appear at a scheduled study visit were coded as non-abstinent. The substance abstinence variable employed in this study is the number of study visits yielding clean urinalysis/breathalyzer results divided by all possible visits (i.e., proportional substance abstinence during the intervention period). Full substance abstinence outcomes have been reported elsewhere (Reback et al., 2010). In brief, participants randomized into the CM condition were estimated to be approximately twice as likely to submit urine and breathalyzer samples free from substance biomarkers when compared to participants in the control condition.
Psychological and Emotional Distress
Self-reported symptoms of psychological and emotional distress were measured using the Brief Symptom Inventory (BSI: Derogatis & Melisaratos, 1983), which was administered to assess cognitive, behavioral, and emotional distress. The nine BSI subscales measuring specific domains of psychological and emotional distress were compiled according to authors’ instructions.
Statistical Analysis
The study utilized a two-group randomized, controlled experimental design. All data were analyzed using an “intent to treat” model, meaning all participants were included in hypothesis testing regardless of study retention or their exposure to their assigned condition. Student’s t-tests were used to compare psychological symptoms across study arms. Seemingly unrelated regression equations (SUREs) (Fiebig 2003; Beasley 2008; Kubáček 2013) were used to estimate the associations between randomization into the CM intervention (dichotomous; 1 = CM) and self-reported symptoms of psychological and emotional distress (i.e., scores on the subscales of the BSI). SUREs are identical to normal OLS regression, except that multiple dependent variables can be included, instead of just one. All regression models were estimated simultaneously (allowing for correlated errors across symptom domains and the performance of omnibus tests of association across symptom domains), and included the following statistical controls: a) domain-specific symptom complaints at baseline (i.e., the somatization model included the baseline somatization symptom scores; the obsessive-compulsive model included baseline symptom scores of obsessive-compulsive disorder; etc.), b) proportional substance abstinence during the intervention phase of the study (see: Method/Measures/Substance Abstinence), and c) participant sociodemographics relevant to psychological symptom complaints (i.e., race/ethnicity, Bratter and Eschbach 2005; age, Mirowsky and Ross 2012; and HIV status, Ciesla and Roberts 2001). SURE analysis techniques have previously been used for the analysis of the BSI and other measures of psychological distress (e.g., Rowe, La Greca, and Alexandersson, 2010; Muennig et al., 2011) as the application of such oblique estimation techniques preserves more of the natural variation across subscales compared to the use of omnibus measures such as the BSI’s Global Severity Index (GSI), which collapses all unique variation across the symptom domains into a single value. Domain-specific results are important when studying individuals undergoing treatment for substance use, as both continued use and substance abstinence after dependence may produce serious and contrasting symptoms of psychological distress (e.g., increases in somatization, decreases in depression) that would be obscured by summary measures like the GSI. Results are reported as significant beginning at p ≤ 0.05, and all statistical tests were carried out using Stata 13SE.
Results
All participants met criteria for at least one substance dependence disorder (a criterion for study eligibility). As revealed by the SCID, the most prevalent non-substance dependence psychiatric disorders at baseline were major depressive disorder (35.4%), antisocial personality disorder (34.4%), post-traumatic stress disorder (31.3%), and panic disorder (26.7%; Table 2). When assessing psychiatric disorder and substance use disorder comorbidity, 109 out of the 131 (83.2%) participants were dually diagnosed with at least one non-substance dependence psychiatric disorder and one substance dependency.
Table 2.
Psychiatric Disorders at Baseline (N = 131)
| Psychiatric Disorder | n (%) |
|---|---|
| Substance Induced Psychotic Disorder | 22 (16.8%) |
| Bipolar I Disorder | 13 (9.9%) |
| Major Depressive Disorder | 46 (35.4%) |
| Panic Disorder | 35 (26.7%) |
| Social Phobia | 16 (12.2%) |
| Obsessive Compulsive Disorder | 23 (17.6%) |
| Post Traumatic Stress Disorder | 41 (31.3%) |
| General Anxiety Disorder | 14 (10.7%) |
| Antisocial Personality Disorder | 45 (34.4%) |
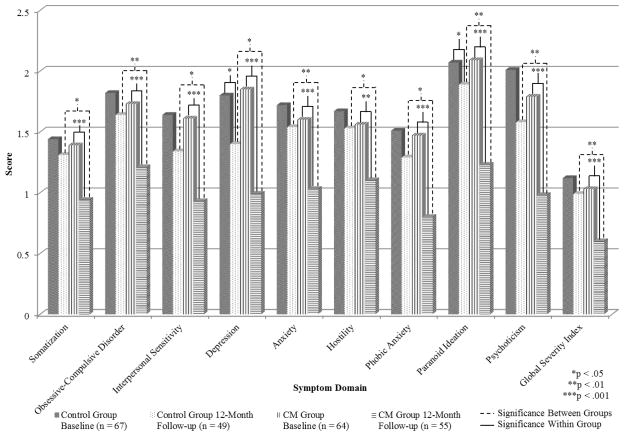
Participant symptoms of psychological and emotional distress at baseline and 12-month follow-up are presented in Figure 1. Participants in the CM condition exhibited significant reductions in reported symptoms across all nine BSI subscales, while participants in the control group demonstrated significant reductions in only the depression and paranoid ideation subscales. Furthermore, by 12-month follow-up participants randomized into the CM condition exhibited significantly lower scores on all measured subscales when compared to participants in the control condition (note: there were no significant differences in symptoms across groups at baseline). Symptom complaints reduced an average of 0.62 points for participants in the CM condition (min = 0.37, hostility; max = 0.89, depression), and reduced an average of 0.22 points for participants in the control condition (min = 0.06, hostility; max = 0.38, depression); the smallest reduction in symptoms observed in the CM group is equal in magnitude to the largest reduction observed in the control group.
Figure 1.
Participant reported symptoms of psychological and emotional distress at baseline and 12-month follow-up evaluations.
Seemingly unrelated regression analysis was used to simultaneously regress all nine BSI subscales onto substance abstinence, domain-specific symptom complaints at baseline, and participant sociodemographics (Table 3). Results indicate that randomization into the CM condition was associated with significantly greater reductions in psychological symptoms across all nine subscales, compared to the control condition. The smallest difference across study conditions was observed in the somatization subscale (b = −0.32; p ≤ 0.05), while the largest difference was observed in the paranoid ideation subscale (b = −0.61; p ≤ 0.001). An omnibus test of significance across all nine subscales (the primary purpose of the SURE analysis) reveals that randomization into the CM condition was associated with significantly greater reductions in symptom complaints relative to the control condition (χ2(9) = 17.26; p < 0.05). Substance abstinence (included as a statistical control) was associated with significant reductions in only the phobic anxiety subscale (b = −0.67; p = 0.03), and as a covariate failed to reach α ≤ 0.05 in the omnibus test of simultaneous significance across the 9 subscales (χ2(9) = 12.02; p = 0.21).
Table 3.
Associations between participant symptom complaints at 12-month follow-up and randomization into the contingency management intervention (n = 104)a
| Somatization b (95% CI) |
Obsessive-Compulsive b (95% CI) |
Interpersonal Sensitivity b (95% CI) |
Depression b (95% CI) |
Anxiety b (95% CI) |
Hostility b (95% CI) |
Phobic Anxiety b (95% CI) |
Paranoid Ideation b (95% CI) |
Psychoticism b (95% CI) |
|
|---|---|---|---|---|---|---|---|---|---|
| CM Intervention | −0.32* ([−0.62] – [−0.01]) | −0.40** ([−0.70] – [−0.11]) | −0.38* ([−0.71] – [−0.05]) | −0.40* ([−0.73] – [−0.06]) | −0.45** ([−0.76] – [−0.14]) | −0.38* ([−.74] – [−0.02]) | −0.44* ([−0.80] – [−0.09]) | −0.61*** ([−0.94] – [−0.29]) | −0.55** ([−0.93] – [−0.17]) |
| R2 | 0.26 | 0.23 | 0.25 | 0.22 | 0.38 | 0.17 | 0.23 | 0.36 | 0.26 |
nControl = 49; nCM = 55
≤ 0.05;
p ≤ 0.01;
p ≤ 0.001; all sig. tests 2-tailed
Statistical controls: Substance abstinence during intervention phase (urinalysis/breathalyzer confirmed), baseline symptom complaints (domain-specific), participant race/ethnicity, age, and HIV status
CM Omnibus test of significance (i.e., contingency management intervention b = 0 across all symptom domains): χ2(9) = 17.26; p < 0.05
Discussion
Findings showed that this low-cost CM intervention that reduced substance use and encouraged pro-social health behaviors had concomitant and significant impacts on relieving a broad range of psychological symptoms. By treatment end, participants randomized to receive CM demonstrated significantly reduced symptoms across all nine BSI domains compared to those randomly assigned to the control condition. By 12-month follow-up, CM participants reported symptoms that were less severe than the normative psychiatric inpatient data in seven of the nine symptom domains.
One question raised by these findings is whether CM had a direct effect in reducing psychological symptoms. Results show that substance abstinence achieved during the intervention phase did not significantly contribute to reductions in psychological symptom complaints in this sample (as evidenced by the non-significant omnibus test result following the SURE analysis). This finding contrasts with prior evidence suggesting that substance abstinence achieved during a CM intervention mediates the relationship between exposure to CM and reductions in psychological distress (Petry et al. 2013). Though the specific mechanism underlying the association between CM and psychological health cannot be determined through the present analyses, we suggest that the positive reinforcement received during a CM intervention may mitigate some of the negative psychological and somatic effects of substance use and/or substance withdrawal.
That participants enrolled in a CM intervention exhibit reduced symptoms of psychological distress (e.g., McLellan et al. 1985; Higgins et al. 2003; McDonnell et al. 2013; Petry et al. 2013) strongly supports future studies that attempt to isolate the specific mechanism of action producing reductions in psychological symptoms from CM. The outcomes presented here are particularly encouraging, as they are robust (occurring across all measured subscales of the BSI), direct (unmediated by substance use outcomes), and durable (lasting through 12-month follow-up).
Limitations and Conclusions
The findings reported here are limited by the relatively small sample size and highly specialized population. It is unknown if similar outcomes would be replicated in studies among other out-of-treatment populations. Studies relying on samples exhibiting less severe symptoms at intake may not achieve the magnitude of reductions presented here. Furthermore, attempts to replicate these results in other countries or social milieus may uncover potentially different patterns of results, as the experience and expression of psychological distress is recognized to vary widely across cultures (American Psychiatric Association, 2013). Results are also limited by the lack of statistical control for concurrent psychiatric treatment, as well as the lack of statistical control for any health-promoting/prosocial behaviors enacted during the course of the intervention. Achievement of health-promoting/prosocial behaviors during the intervention may have had unique effects such as reduced shame, increased self-efficacy, and/or increased approach and activation behavior (Hopko, Lejuez, Ruggiero, and Eifert 2003), each of which could contribute to reductions in psychological distress. Furthermore, substance abstinence was not measured during the interim periods between each follow-up evaluation. Coefficient estimates may be biased if patterns of abstinence during these interim periods differ substantially from results achieved during the intervention period. Finally, this and virtually all prior studies examining the association between administration of CM and reductions in psychological symptoms of distress have relied on the BSI for the assessment of participant psychological health. Not only is the BSI not intended as a clinical diagnostic instrument, but the repeated use of the same instrument over time and across studies may unintentionally bias the extant literature towards whatever shortcomings exist in the BSI. Use of other instruments (CES-D, Radloff 1977; PHQ-9, Kroenke and Spitzer 2002; etc.) would help safeguard against such bias, and may help to isolate the specific effect of CM on symptoms of psychological distress.
The finding that CM augments reductions in psychological and emotional distress symptoms is encouraging. Future work should not only seek to replicate these results, but might include psychotropic medications as well as adherence to such medications as both a statistical control and a target for contingent reinforcement. These findings demonstrate that CM interventions targeting substance abstinence and prosocial/health-promoting behaviors can reduce symptoms of psychological and emotional distress.
Acknowledgments
Funding for this study was provided by NIDA Grant RO1 DA015990. Funding for the HIV prevention program was provided by Los Angeles County Department of Public Health, Division of HIV/STD Programs (DHSP; formerly Office of AIDS Programs and Policy) Contract H-700861. CJR and SS acknowledge additional support from the NIMH Grant P30 MH58107. NIDA, DHSP, or NIMH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Conflicts of Interest
The authors declare no conflicts of interest.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Beasley TM. Seemingly Unrelated Regression (SUR) models as a solution to path analytic models with correlated errors. Multiple Linear Regression Viewpoints. 2008;34:1–7. [Google Scholar]
- Bratter JL, Eschbach K. Race/Ethnic Differences in Nonspecific Psychological Distress: Evidence from the National Health Interview Survey*. Social Science Quarterly. 2005;86:620–644. [Google Scholar]
- Castellani B, Wedgeworth R, Wootton E, Rugle L. A bi-directional theory of addiction: Examining coping and the factors related to substance relapse. Addictive Behaviors. 1997;22:139–144. doi: 10.1016/s0306-4603(96)00026-3. [DOI] [PubMed] [Google Scholar]
- Charney DA, Palacios-Boix J, Negrete JC, Dobkin PL, Gill KJ. Association between concurrent depression and anxiety and six-month outcome of addiction treatment. Psychiatric Services. 2005;56:927–933. doi: 10.1176/appi.ps.56.8.927. [DOI] [PubMed] [Google Scholar]
- Ciesla JA, Roberts JE. Meta-analysis of the relationship between HIV infection and risk for depressive disorders. American Journal of Psychiatry. 2001;158:725–730. doi: 10.1176/appi.ajp.158.5.725. [DOI] [PubMed] [Google Scholar]
- Cochran SD, Mays VM. Lifetime prevalence of suicidal symptoms and affective disorders among men reporting same-sex sexual partners: Results from the NHANES III. American Journal of Public Health. 2000a;90:573–578. doi: 10.2105/ajph.90.4.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran SD, Mays VM. Relation between psychiatric syndromes and behaviorally defined sexual orientation in a sample of the U.S. population. American Journal of Epidemiology. 2000b;151:516–523. doi: 10.1093/oxfordjournals.aje.a010238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Cottler LB, Jacobs JL, Ben-Abdallah A, Spitznagel EL. The role of psychiatric disorders in predicting drug dependence treatment outcomes. American Journal of Psychiatry. 2003;160:890–895. doi: 10.1176/appi.ajp.160.5.890. [DOI] [PubMed] [Google Scholar]
- Daughters SB, Lejuez CW, Kahler CW, Strong DR, Brown RA. Psychological distress tolerance and duration of most recent abstinence attempt among residential treatment-seeking substance abusers. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors. 2005;19:208–211. doi: 10.1037/0893-164X.19.2.208. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- Drake RE, O’Neal EL, Wallach MA. A systematic review of psychosocial research on psychosocial interventions for people with co-occurring severe mental and substance use disorders. Journal of Substance Abuse and Treatment. 2008;34:123–138. doi: 10.1016/j.jsat.2007.01.011. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I disorders - Patient Edition. 1996. (SCID-I/P, Version 2.0, 4/97 revision) [Google Scholar]
- Fiebig D. Seemingly Unrelated Regression. In: Baltagi BH, editor. A Companion to Theoretical Econometrics. Malden, MA: Blackwell Publishing LTD; 2003. pp. 101–121. [Google Scholar]
- Fletcher JB, Reback CJ. Antisocial personality disorder predicts methamphetamine treatment outcomes in homeless, substance-dependent men who have sex with men. Journal of Substance Abuse Treatment. 2013;45:266–272. doi: 10.1016/j.jsat.2013.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassel A, Nordfjærn T, Hagen R. Psychological and interpersonal distress among patients with substance use disorders: Are these factors associated with continued drug use and do they change during treatment? Journal of Substance Use. 2013;18:363–376. [Google Scholar]
- Herrell R, Goldberg J, True WR, Ramakrishnan V, Lyons M, Eisen S, Tsuang MT. Sexual orientation and suicidality: A co-twin control study in adult men. Archives of General Psychiatry. 1999;56:867–874. doi: 10.1001/archpsyc.56.10.867. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Sigmon SC, Wong CJ, et al. Community reinforcement therapy for cocaine-dependent outpatients. Archives of General Psychiatry. 2003;60:1043–1052. doi: 10.1001/archpsyc.60.9.1043. [DOI] [PubMed] [Google Scholar]
- Hopko DR, Lejuez CW, Ruggiero KJ, Eifert GH. Contemporary behavioral activation treatments for depression: Procedures, principles, and progress. Clinical Psychology Review. 2003;23:699–717. doi: 10.1016/s0272-7358(03)00070-9. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32:1–7. [Google Scholar]
- Kubáček L. Seemingly unrelated regression models. Applications of Mathematics. 2013;58:111–123. [Google Scholar]
- Laudet AB, Becker JB, White WL. Don’t Wanna Go Through That Madness No More: Quality of Life Satisfaction as Predictor of Sustained Remission from Illicit Drug Misuse. Substance Use and Misuse. 2009;44:227–252. doi: 10.1080/10826080802714462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancino MJ, McGaugh J, Feldman Z, Poling J, Oliveto A. Effect of PTSD diagnosis and contingency management procedures on cocaine use in dually cocaine- and opioid-dependent individuals maintained on LAAM: A retrospective analysis. The American Journal on Addictions. 2010;19:169–177. doi: 10.1111/j.1521-0391.2009.00025.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonell MG, Srebnik D, Angelo F, McPherson S, Lowe JM, Sugar A, Ries RK. Randomized Controlled Trial of Contingency Management for Stimulant Use in Community Mental Health Patients With Serious Mental Illness. The American Journal of Psychiatry. 2013;170:94–101. doi: 10.1176/appi.ajp.2012.11121831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messina N, Farabee D, Rawson R. Treatment responsivity of cocaine-dependent patients with antisocial personality disorder to cognitive-behavioral and contingency management interventions. Journal of Consulting and Clinical Psychology. 2003;71:320–329. doi: 10.1037/0022-006x.71.2.320. [DOI] [PubMed] [Google Scholar]
- Mirowsky J, Ross CE. Social Causes of Psychological Distress. 2. New York: Transaction; 2012. [Google Scholar]
- Muennig P, Robertson D, Johnson G, Campbell F, Pungello EP, Neidell M. The effect of an early education program on adult health: The Carolina Abecedarian Project Randomized Controlled Trial. American Journal of Public Health. 2011;101:512. doi: 10.2105/AJPH.2010.200063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen CM, Liu WM, Hernandez JO, Stinson R. Problem-solving appraisal, gender role conflict, help-seeking behavior, and psychological distress among men who are homeless. Psychology of Men & Masculinity. 2012;13:270–282. [Google Scholar]
- Petry NM, Alessi SM, Rash CJ. Contingency management treatments decrease psychiatric symptoms. Journal of Consulting and Clinical Psychology. 2013;81:926–931. doi: 10.1037/a0032499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reback CJ, Peck JA, Dierst-Davies R, Nuno M, Kamien JB, Amass L. Contingency management among homeless, out-of-treatment men who have sex with men. Journal of Substance Abuse Treatment. 2010;39:255–263. doi: 10.1016/j.jsat.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe CL, La Greca AM, Alexandersson A. Family and individual factors associated with substance involvement and PTS symptoms among adolescents in greater New Orleans after Hurricane Katrina. Journal of Consulting and Clinical Psychology. 2010;78:806–817. doi: 10.1037/a0020808. [DOI] [PubMed] [Google Scholar]
- Sandfort TGM, de Graaf R, Bijl RV, Schnabel P. Same-sex sexual behavior and psychiatric disorders: Findings from the Netherlands Mental Health Survey and Incidence Study (NEMESIS) Archives of General Psychiatry. 2001;58:85–91. doi: 10.1001/archpsyc.58.1.85. [DOI] [PubMed] [Google Scholar]
- Schumacher JE, Milby JB, Wallace D, Meehan DC, Kertesz S, Vuchinich R, Usdan S. Meta-analysis of day treatment and contingency management dismantling research: Birmingham homeless cocaine studies (1990–2006) Journal of Consulting and Clinical Psychology. 2007;75:823–828. doi: 10.1037/0022-006X.75.5.823. [DOI] [PubMed] [Google Scholar]
- Skinner BF. Science and Human Behavior. New York: The Free Press; 1953. [Google Scholar]
- Slade T, Grove R, Burgess P. Kessler Psychological Distress Scale: Normative Data from the 2007 Australian National Survey of Mental Health and Wellbeing. Australian and New Zealand Journal of Psychiatry. 2011;45:308–316. doi: 10.3109/00048674.2010.543653. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 10. College Station, TX: StataCorp LP; 2007. [Google Scholar]
- Tracy K, Babuscio T, Nich C, Kulik B, Carroll KM, Petry NM, Rounsaville BJ. Contingency management to reduce substance use in individuals who are homeless with co-occurring psychiatric disorders. American Journal of Drug and Alcohol Abuse. 2007;33:253–258. doi: 10.1080/00952990601174931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstock J, Alessi SM, Petry NM. Regardless of psychiatric severity the addition of contingency management to standard treatment improves retention and drug use outcomes. Drug and Alcohol Dependence. 2007;87:288–296. doi: 10.1016/j.drugalcdep.2006.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]