Abstract
Background
Although the effect of bisphenol A on various health outcomes has been extensively examined, few studies have investigated its effect on asthma.
Objective
We hypothesized that exposure to bisphenol A in school-age children was associated with wheezing and asthma.
Methods
Participants included 127 children aged 7–8 years without a previous asthma diagnosis in an elementary school in Seoul, Korea. Three surveys were conducted, each 2 years apart. Bisphenol A concentration was measured at the baseline survey, and PC20, which is defined as the methacholine concentration that induces a decrease in FEV1 of 20% from baseline, was measured at every survey. Associations between bisphenol A concentration at 7–8 years of age and wheezing, asthma, and PC20 at ages up to 11–12 years were examined using generalized estimating equations, a marginal Cox regression model, and a linear mixed model.
Results
The log-transformed creatinine-adjusted urinary bisphenol A concentration at 7–8 years was positively associated with wheezing (odds ratio, 2.48; 95% confidence interval, 1.15–5.31; P = .02) and asthma (hazard ratio, 2.13; 95% confidence interval, 1.51–3.00; P<.001) at ages up to 11–12 years. Bisphenol A was also negatively associated with PC20 (ß = −2.33; P = .02). When stratified by sex, the association between bisphenol A and asthma remained significant only in girls (hazard ratio, 2.45; 95% confidence interval, 2.18–2.76; P<.001).
Conclusion
Increased urinary bisphenol A concentrations at 7–8 years old were positively associated with wheezing and asthma and negatively associated with PC20 at ages up to 11–12 years.
Introduction
Asthma is one of the most common childhood diseases with prevalence of 9.1% in the United States and 7.6% in Korea [1]–[3]. The global prevalence of asthma in children has risen significantly over the recent decades [4], [5]. The exact cause of this increase is not known, but associations with increasing urbanization have been reported [6], [7]. Furthermore, the increase in global asthma prevalence has occurred within approximately the same timeframe as the widespread use of industrial chemicals like bisphenol A (BPA) [8]. BPA is one of the chemicals produced in the highest volumes worldwide [9] and is used in the production of polycarbonate plastics and epoxy resins. Polycarbonate plastics are used to make products such as water bottles, toys, dental sealants, and compact discs, whereas epoxy resins are used to coat the insides of cans for food and beverages [8], [10]. Human exposure to BPA is extensive, and 95% of the United States population has detectable urinary BPA concentrations [11].
Previous studies have shown that BPA could have various health effects, including diabetes [12], [13], coronary artery stenosis [14], [15], heart rate variability and blood pressure [16], abnormal liver function [17], childhood neurobehavioral problems [18], oxidative stress and inflammation [10], male sexual dysfunction [19], [20], decreased semen quality [21], [22], and adverse birth outcomes [23]. Especially in women, BPA has been associated with abnormal pubertal development [24], [25], externalizing behaviors [26], recurrent miscarriages [27], and premature delivery [28].
Studies have also reported a potential association between BPA exposure and asthma. Animal studies suggest that BPA might affect the development of asthma-related conditions by promoting allergic immune responses [29]–[33]. BPA has also been shown to promote eosinophilic bronchial inflammation and airway responsiveness in mice [9], [34] and production of airway secretary proteins, which is one of the hallmarks of asthma, in rhesus monkeys [35]. In humans, a relationship between prenatal urinary BPA and wheezing has been reported among children under the age of 3 years [36]. These findings are supported by a reported association between pre- and postnatal BPA exposure and wheezing and asthma development in preschool children [37].
However, to the best of our knowledge, there is little evidence regarding the effects of BPA exposure on asthma in school-age children. Furthermore, examining the association in Korea, where relatively low BPA concentration of school-age children (1.2 µg/L) compared to that of USA (2.7 µg/L) had been reported, gives extra information [38], [39]. In the present study, we hypothesized that exposure to BPA in school-age children is associated with asthma-related outcomes such as wheezing, asthma, and PC20, which is defined as the methacholine concentration that causes a decrease in FEV1 of 20% from baseline.
Materials and Methods
Study sample and data collection
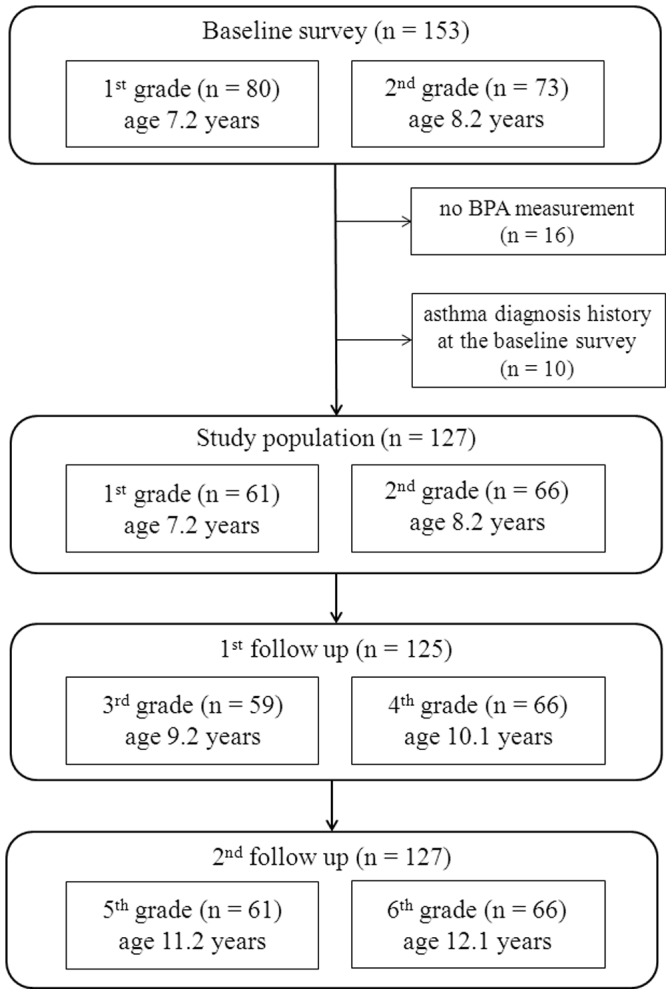
In 2005, all the 1st grade (n = 92) and 2nd grade children (n = 96) in an elementary school in Seoul, Korea, were invited to the study. Of a total of 188 children aged 7–8 years, parents of 153 schoolchildren agreed to enroll for the baseline survey, which consisted of a methacholine challenge test, urinary BPA measurement, and the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire, answered by the parents or guardian. Of the original sample, the participants without a BPA measurement (n = 16) or with a previous asthma diagnosis (n = 10) at baseline were subsequently excluded from the analysis, resulting in 127 children. In 2007, 125 of the 127 children who were then aged 9–10 years participated in the first follow-up survey, and, in 2009, all of the original 127 children who were then aged 11–12 years participated in the second follow-up survey (Figure 1). The follow-up surveys consisted of the ISAAC questionnaire and the methacholine challenge test.
Figure 1. Overview of study population sampling and follow-up.
Written informed consent was obtained from parents or guardians of all participating children, and the study protocols were reviewed and approved by the Institutional Review Board at the Dankook University Medical Center.
Exposure assessment
All participating children were asked to fast for more than 8 h before the survey. Spot urine samples (50 mL) were collected between 0900 and 1200 h from participants at the baseline survey (n = 127) in conical tubes (SPL Lifesciences, Pocheon, Gyunggi-do, Korea). Urine samples were stored at −20°C in the freezer and sent to the laboratory (NeoDin Medical Institute, Seoul, Korea) within 90 min. Urine samples were buffered using 30 µL of 2M sodium acetate (pH 5.0), and a mixture of 10 µL ß-glucuronidase/sulfatase (Sigma, St. Louis, MO, USA) and 25 µL BPA (RING-13C12, 99%, Cambridge Isotope Lab, Inc., Tewksbury, MA, USA) was added. The samples were incubated at 37°C for 3 h to deconjugate the glucuronidated BPA, and 100 µL of 2N HCl was added after incubation. The extract was dehydrated with nitrogen gas and then reconstituted with 1 mL of HPLC-grade H2O in a 2 mL glass vial. Each batch of samples included a quality control sample and a blank. We added the quality control sample in pooled urine with a mixture of BPA standard. Liquid-liquid extraction was performed with Agilent Eclipse plus C18, 3.5 µm, 2.1×100 mm. The mobile phase was 60∶40 (v/v) acetonitrile:water, and the flow rate was 0.4 mL/min. Total BPA, including the free and conjugated forms, was measured using a high performance liquid chromatography-mass selective detector (HPLC-MS/MS, Agilent Triple Quad 6410, Santa Clara, CA, USA). The BPA concentrations in all the urinary samples were above the limit of detection (0.005 µg/L). The concentration of urinary BPA was adjusted for creatinine measured from the same urine sample to eliminate the influence caused by the different urinary excretion rates between participants [11].
Outcome measures
Wheezing was defined using the ISAAC question “Has your child had wheezing or whistling in the chest in the last 12 months?”. Children were considered to have asthma (current asthma) when either of the following criteria was met: 1) wheezing or the use of asthma medication in the previous 12 months combined with a PC20≤8 mg/mL or 2) wheezing or the use of asthma medication in the previous 12 months combined with a history of an asthma diagnosis or a history of wheezing. Incident asthma was defined as the first detection of current asthma without having satisfied the criteria of current asthma at any previous survey.
The response to the methacholine challenge is expressed as PC20. To evaluate PC20, which is an indicator of airway hyperresponsiveness, participants inhaled increasing concentrations of methacholine (0.625, 1.25, 2.5, 5, 12.5, and 25 mg/dL) using a nebulizer until the FEV1 measured by a portable spirometer (Microspiro HI-298, Chest Corporation, Tokyo, Japan) decreased by at least 20% from the baseline value. The PC20 was calculated using a log-dose response curve [40].
Covariates
The parental asthma history was reported on the baseline questionnaire. Fetal tobacco smoke exposure was defined as active maternal smoking or the report of a smoker in the home during pregnancy. Environmental tobacco smoke exposure was defined as active maternal smoking during the first year after delivery, maternal smoking at the time of the survey, or the report of a smoker in the home from delivery until the time of the survey. Pet ownership was defined as having ever kept dogs or cats as pets from delivery until the time of the surveys.
Statistical analyses
Urinary BPA concentration was adjusted for creatinine measured from the same urine sample (i.e., urinary BPA concentration divided by urinary creatinine concentration) and log-transformed to approximate a normal distribution. The associations between urinary BPA concentration at 7–8 years of age and the dichotomous outcome variable, e.g., wheezing and current asthma, were analyzed using generalized estimating equations (GEE) with a logit link. A marginal Cox model with a robust sandwich estimator of variance was applied to analyze the association between BPA exposure and risk of incident asthma considering the grade-at-enrollment dependence due to the possibility of clustering within the grade. The proportional hazards assumption was tested using a time-dependent explanatory variable. For those with incident asthma, the time at risk was considered as the number of years from the baseline survey to the mid-point between the previous survey and the survey when the incident asthma was observed and, for those without incident asthma, as the number of years between the baseline survey and the last follow-up survey. Due to the difficulty of assigning the exact time at risk and the relatively long period between the surveys, the association between BPA concentration and incident asthma was also analyzed using a logistic regression model.
The associations between urinary BPA concentration at 7–8 years of age and PC20 at the 3 time points (7–8, 9–10, and 11–12 years of age) were analyzed in two steps. First, a generalized additive mixed model was constructed to graphically examine the linearity of the association. Then, a linear mixed model using repeated-measures analysis and a random effect of grade-at-enrollment was constructed to analyze the relationship between BPA concentration at 7–8 years of age and PC20 at 3 time points. Logistic and linear regression models were used to analyze the association between BPA concentration and wheezing, current asthma, and PC20 at each time point.
The child’s sex, parental asthma history, fetal tobacco smoke exposure, and pet ownership were selected as covariates based on earlier literature reviews [36], [37]. Potential confounders, such as environmental tobacco smoke exposure, history of breastfeeding, cockroach sensitization, and maternal education level were evaluated using bivariate analyses. Covariates that predicted wheezing at P≤. 20 in the bivariate analyses were added to the initial multivariable GEE model and retained if the estimate of the association between BPA at 7–8 years of age and wheezing changed >10%, which resulted in the child’s sex, parental asthma history, fetal tobacco smoke exposure, environmental tobacco smoke exposure, and pet ownership as the covariates in the analysis. The GEE with a logit link, logistic regression, and linear regression models were also adjusted for grade at enrollment.
In the secondary analyses, potential interaction was tested by adding cross product term between BPA concentration and each covariate in the main analysis. The participants were stratified into subgroups based on sex and analyzed using the marginal Cox model for clustered data and a linear mixed model.
SAS version 9.3 (SAS Institute Inc., Cary, NC, USA) was used for statistical analyses, and R version 2.14.2 (The Comprehensive R Archive Network: http://cran.r-project.org) was used for visualization. Two-sided P values <.05 were used to indicate statistical significance.
Results
Of the 127 participants, 54.3% were male, 4.7% had a parental asthma history, 17.3% experienced fetal tobacco smoke exposure, and 26.8% experienced environmental tobacco smoke exposure. Difference between baseline characteristics of children who had current asthma during the study period and those of children who did not was not observed (Table 1). When comparing the children that were included in the analysis with those excluded, there were no differences except for a slightly higher level of cockroach sensitization in the children that were included in the analysis (Table S1 in File S1).
Table 1. Baseline characteristics of the study participants stratified by children who had current asthma during the study period and children who did not [n (%)].
| Characteristic | Children with asthma (n = 18) | Children without asthma (n = 109) | P value* |
| Sex | .53 | ||
| Boy | 11 (61.1) | 58 (53.2) | |
| Girl | 7 (38.9) | 51 (46.8) | |
| Parental asthma history | .09 | ||
| No | 14 (77.8) | 99 (90.8) | |
| Yes | 1 (5.6) | 5 (4.6) | |
| Missing | 3 (16.7) | 5 (4.6) | |
| Fetal tobacco smoke exposure† | .94 | ||
| No | 15 (83.3) | 90 (82.6) | |
| Yes | 22 (16.7) | 19 (17.4) | |
| Environmental tobacco smoke exposure§ | .50 | ||
| No | 12 (66.7) | 81 (74.3) | |
| Yes | 6 (33.3) | 28 (25.7) | |
| Pet ownership‡ | .45 | ||
| No | 15 (83.3) | 82 (75.2) | |
| Yes | 3 (16.7) | 27 (24.8) | |
| Breast-fed | .11 | ||
| No | 5 (27.8) | 35 (32.1) | |
| <3 months | 4 (22.2) | 18 (16.5) | |
| 3–5 months | 0 (0) | 16 (14.7) | |
| ≥6months | 4 (22.2) | 30 (27.5) | |
| Did not answer | 5 (27.8) | 10 (9.2) | |
| Cockroach sensitization | .67 | ||
| No | 17 (94.4) | 103 (94.5) | |
| Yes | 0 (0) | 3 (2.8) | |
| Did not answer | 1 (5.6) | 3 (2.8) | |
| Maternal education | .67 | ||
| < High school | 3 (11.9) | 13 (11.9) | |
| High school | 7 (38.9) | 51 (46.8) | |
| >High school | 5 (27.8) | 34 (31.2) | |
| Did not answer | 3 (16.7) | 11 (10.1) | |
| Paternal education | .19 | ||
| < High school | 3 (16.7) | 6 (5.5) | |
| High school | 6 (33.3) | 50 (45.9) | |
| >High school | 6 (33.3) | 43 (33.3) | |
| Did not answer | 3 (16.7) | 3 (9.2) |
* P value was estimated based on Chi-square test or Fisher’s exact test.
Active maternal smoking during pregnancy or presence of a smoker in the home during pregnancy.
Active maternal smoking during the first year after delivery, current maternal smoking, or presence of a smoker in the home after delivery until the present time.
Having had a pet dog or cat after delivery until the present time.
Size of the wheal produced by the cockroach antigen ≥3 mm and larger than size of the wheal produced by histamine.
The geometric mean of urinary BPA concentration was 1.02 µg/L, 1st quartile 0.63 µg/L, median 0.97 µg/L, 3rd quartile 1.67 µg/L, and maximum 21.37 µg/L. The distribution of urinary BPA concentrations was positively skewed. In the present study, 9 children were assessed to have current asthma only at 9–10 years, 7 children only at 11–12 years, while 2 children both at 9–10 years and 11–12 years of age. The one-unit increase in log-transformed, creatinine-adjusted urinary BPA concentration measured at 7–8 years of age was associated with wheezing (odds ratio [OR], 2.48; 95% confidence interval [CI], 1.15–5.31; P = .02) and current asthma (OR, 2.35; 95% CI, 1.03–5.32; P = .04) at ages up to 11–12 years. A relationship between urinary BPA concentration and the risk of incident asthma was also observed (hazard ratio [HR], 2.13; 95% CI, 1.51–3.00; P<.001; Table 2). A statistically significant association was also observed between BPA concentration and incident asthma in the logistic regression model (OR, 2.44; 95% CI, 1.11–5.36; P = .03).
Table 2. Association of urinary BPA concentrations (log transformed, µg/g creatinine) at 7–8 years with wheezing and asthma over 11–12 years of age, by longitudinal analyses.
| Outcome | No.* | OR† or HR‡ (95% CI) | P value |
| Wheeze | 28/335 | 2.48 (1.15–5.31) † | .02 |
| Current Asthma | 20/252 | 2.35 (1.03–5.32) † | .04 |
| Incident Asthma | 18/127 | 2.13 (1.51–3.00) ‡ | <.001 |
HR, hazard ratio.
* Number with outcome/total number for analysis.
Generalized estimating equation with a logit link model adjusted for gender, parental asthma history, fetal and environmental tobacco smoke exposure, pet ownership, and grade at enrollment.
Marginal Cox model considering grade-at-enrollment clustering adjusted for gender, parental asthma history, fetal and environmental tobacco smoke exposure, and pet ownership.
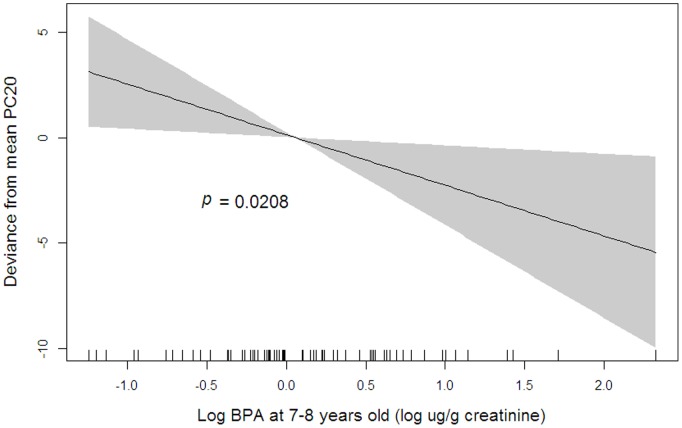
The penalized regression spline showed an almost linear association between BPA at 7–8 years of age and PC20 at ages up to 11–12 years (Figure 2). In the linear mixed model, the association between BPA at 7–8 years of age and PC20 at ages up to 11–12 years was significant (ß = −2.33; P = .02).
Figure 2. Relationship between urinary BPA concentration and PC20.
Penalized regression spline of log-transformed urinary BPA concentrations at 7–8 years on PC20 at ages up to 11–12 years. Solid lines, spline curve; shaded area, 95% confidence intervals. The model is adjusted for gender, parental asthma history, fetal and environmental tobacco smoke exposure, and pet ownership.
The analysis of the associations between BPA at 7–8 years of age and wheezing, PC20, and current asthma at each time point resulted in significant relationships with wheezing, PC20, and current asthma at 9–10 years of age only (Table 3). When the interaction term between BPA and each covariate was added to the multivariable model, significant interactions were not found. When stratified by sex, a significant association between BPA and incident asthma (HR, 2.45; 95% CI, 2.18–2.76; P<.001) and a marginally significant association between BPA and PC20 (ß = −2.59, P = .09; Table S2 in File S1) were observed only in girls.
Table 3. Association of urinary BPA concentrations (log transformed, µg BPA/g creatinine) at 7–8 years with wheezing, PC20, and current asthma at 7–8, 9–10, and 11–12 years of age.
| Log BPA (µg/g creatinine) at 7–8 y | |||||||||
| Wheeze* | PC20 † | Current asthma* | |||||||
| Age (years) | No.‡ | OR (95%CI) | P value | No.§ | ß (SE) | P value | No.‡ | OR (95%CI) | P value |
| 7–8 | 8/120 | 3.08 (0.86–11.09) | .09 | 64 | −2.01 (1.22) | .11 | NA | ||
| 9–10 | 11/121 | 4.24 (1.35–13.28) | .01 | 19 | −6.37 (2.26) | .02 | 11/125 | 3.64 (1.23–10.76) | .02 |
| 11–12 | 9/122 | 1.80 (0.69–4.71) | .23 | 14 | −3.64 (2.50) | .20 | 9/127 | 1.87 (0.72–4.86) | .20 |
*Logistic regression model adjusted for gender, parental asthma history, fetal and environmental tobacco smoke exposure, pet ownership, and grade at enrollment.
Linear regression model adjusted for gender, parental asthma history, fetal and environmental tobacco smoke exposure, pet ownership, and grade at enrollment.
Number with outcome/total number for analysis.
Total number for analysis.
For the sensitivity analysis, we conducted the analyses after including the children who had been diagnosed with asthma before the baseline survey (n = 10). This did not change the result substantially (Table S3 in File S1). When excluding the children who satisfied the criteria of current asthma at the baseline survey, BPA concentration at 7–8 years of age was significantly associated with increased risk of incident asthma (HR, 1.64; 95% CI, 1.10–2.45; P = .02). Significant association of BPA with PC20 at 9–10 years and marginally significant association with wheezing at 9–10 years of age was also observed. The trend of association between BPA and current asthma was similar although attenuated, partly due to small sample size (Table S4 in File S1).
Discussion
In the present study, we found associations between the urinary BPA concentration in the earlier years of children in elementary school and wheezing, asthma, and PC20 in the later years. A potential modifying effect of sex on these associations was also observed.
Previous studies have reported that prenatal or postnatal exposure to BPA is associated with an increased risk of wheezing and asthma. One birth cohort study of 398 mother-child pairs demonstrated that prenatal urinary BPA concentrations above, versus below, the median are associated with the child’s wheezing at 6 months (OR, 2.27; 95% CI, 1.28–4.06) but not at older ages until 3 years of age [36]. Another birth cohort study of 568 mother-child pairs showed that urinary BPA concentrations at 3 years are associated with wheezing at 5 and 6 years of age, and urinary BPA concentrations at 7 years are associated with wheezing at 7 years of age. A one-unit increase in log-transformed, creatinine-adjusted urinary BPA concentrations at 3, 5, and 7 years is associated with asthma at a single assessment by a physician between 5 and 12 years of age (OR, 1.5; 95% CI, 1.1–2.0 for BPA at 3 years; OR, 1.4; 95% CI, 1.0–1.9 for BPA at 5 years; OR, 1.5; 95% CI, 1.0–2.1 for BPA at 7 years of age) [37]. Our results are similar to the previous findings, although the effect size is relatively large in the current study, which may be explained by the differences in outcome definition, study population, and adjusting covariates.
In the current study, urinary BPA at 7–8 years was associated with asthma-related outcomes such as wheezing, asthma, and PC20 at 9–10 years, but not at 7–8 years or 11–12 years of age. Due to the lack of mechanistic studies investigating the time lag between BPA exposure and occurrence of asthma-related outcomes, we have no definite explanation for this finding. Pubertal stage may play a role; it has been reported that pubertal stage is related to the development and progression of asthma [41]–[44]. Alternatively, observed null association with current asthma at 11–12 years of age might reflect the fact that only a small number of incident asthma cases occur in later years in elementary school, and the incidence of wheezing and asthma continues to decline from childhood to adolescence or greater non-differential misclassification due to longer time interval [45]. Further research considering the pubertal stage is warranted.
The mechanism behind the present findings is still unclear; however, the oxidative stress pathway with BPA exposure could be suggested as a possible explanation. BPA is known to cause oxidative stress in rats [46]–[49] and humans [10], and growing evidence indicates that oxidative stress and subsequent mitochondrial dysfunction are associated with BPA-induced damage [50], [51]. Increased production of reactive oxygen species and decreased anti-inflammatory capacity could enhance the susceptibility to the insults, such as air pollution, which results in chronic airway inflammation and asthma [52], [53].
The results of the present study also suggest that the effects of BPA on asthma-related outcomes might be mediated, at least in part, by an endocrine-disrupting mechanism. It was reported that the prevalence of asthma is higher in boys before puberty and in girls and women after puberty [54]. Changes in hormonal status, such as with estrogen, have been suggested as one possible factor causing this phenomenon [45], [55]. Estrogen has been demonstrated to encourage T-helper 2 (TH2) polarization, class switching of B cells to the production of immunoglobulin E, and the degranulation of mast cells [56]–[59]. In epidemiologic studies, early menarche is associated with a higher prevalence of asthma in adult women [60], and the diagnosis of asthma increases in postmenopausal women who receive hormone replacement therapy [61]. Meanwhile, BPA acts imperfectly as estrogen in numerous organs [62], and female mice that were exposed to BPA prenatally demonstrate increased airway and lung inflammation, whereas the male mice exposed to BPA prenatally did not [63]. The results of these studies and ours suggest that BPA affects asthma-related outcomes by disrupting the endocrine system. However, the mechanisms underlying the sex-specific effect of and susceptibility to BPA are not yet fully understood [29], [55], [64].
BPA concentration in the present study was markedly lower than the previously reported BPA concentration in the United States [11], [38]. Geographic variance of the BPA concentration has been reported not only in the children [38], [39] but also in different age group population [11], [17], [65], [66]. The observed lower BPA concentration in the present study might also be attributable, in part, to the study design using overnight fasting spot urine samples [67], [68]. However, it has been reported that urinary BPA concentration did not decrease rapidly with fasting time [69], and another study following five fasting individual’s spot urine BPA concentration has also demonstrated the decline of BPA concentration with gentle slopes during the first 24 h and fluctuated at lower levels during the next 24 h [70]. This might be due to accumulation of BPA in body tissue, such as fat or exposure to nonfood source and could lead to reduction in the variability of BPA concentration and potential misclassification [71]. Due to these traits, fasting urinary BPA concentration has been used as an indicator of exposure in the previous studies [16], [72]. Further, the random variation in BPA concentrations may have shifted the association toward the null.
Exposure to BPA is thought to be mainly from dietary route [67] and the observed associations could be confounded by the chemicals that were taken with BPA. For instance, mercury and BPA share common exposure source such as canned tuna fish [73], [74]. Although exposure to mercury has been associated with immunotoxic effects [75]–[78], we could not find previous literature supporting the association between exposure to mercury and asthma. Further study exploring the co-exposure of BPA and other environmental risk factors including phthalate, other phenolic compounds, heavy metals, and persistent organic compounds is warranted to assess potential effect modification or confounding [79].
The present study has some strengths. First, the longitudinal study design addressed the potential of temporal ambiguity and recall bias. Second, the use of the objective methacholine challenge test provided a more accurate diagnosis and reduced the potential of misclassification. Furthermore, the reliability of the results was demonstrated by the consistency of results between the parent-reported presence of wheezing and asthma and the results from the objective methacholine challenge test.
The major limitation in the current study is the small sample size. In addition, the selection of participants from one elementary school may have resulted in drawbacks in generalizability. Future studies should include a more representative sample of sufficient size to confirm the findings of the present study. Although PC20 is a commonly used indicator for airway hyperresponsiveness, its use is limited in participants whose decrease in FEV1 is less than the cut-off value before the maximal concentration is reached [80], which happens with the majority of the participants in epidemiologic studies [81]. However, despite the weakness regarding censoring, previous studies have reported that PC20 correlates well with other indicators of airway hyperresponsiveness [82]–[84] and can be used as a reliable indicator of airway hyperresponsiveness [85], [86]. Lastly, due to the lack of a BPA measurement before 7–8 years of age, the possibility that the observed association is due to earlier exposure and that the BPA exposure at 7–8 years of age is reflective of this could not be assessed. Further studies are required to confirm the temporal specifics regarding vulnerability.
We found that the urinary BPA concentration at 7–8 years was associated with wheezing, asthma, and PC20 at ages up to 11–12 years. These findings provide information about the health effects of BPA exposure in school-age children and support public health initiatives to protect the health of a susceptible population such as children.
Supporting Information
This file contains Table S1, Table S2, Table S3, and Table S4. Table S1, Baseline characteristics of the study population included and excluded in the current study. Table S2, Association of urinary BPA concentrations (log transformed, µg BPA/g creatinine) at 7–8 years with incident asthma and PC20 over 11–12 years of age stratified by gender. Table S3, Association of urinary BPA concentrations (log transformed, µg BPA/g creatinine) at 7–8 years with wheezing, PC20, and asthma at 7–8, 9–10, and 11–12 years of age, including the children who had been diagnosed with asthma before 7–8 years of age. Table S4, Association of urinary BPA concentrations (log transformed, µg BPA/g creatinine) at 7–8 years with wheezing, PC20, and current asthma at 7–8, 9–10, and 11–12 years of age, excluding the children who satisfied the criteria of current asthma at the baseline survey.
(PDF)
Data set.
(CSV)
Acknowledgments
The authors thank the research workers, technicians, and participating children and their families. Without them, this work would not have been possible.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
This research was funded by the Korean Ministry of Environment. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Hong S, Son DK, Lim WR, Kim SH, Kim H, et al. (2012) The prevalence of atopic dermatitis, asthma, and allergic rhinitis and the comorbidity of allergic diseases in children. Environ Health Toxicol 27: e2012006 10.5620/eht.2012.27.e2012006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lee SI (2010) Prevalence of Childhood Asthma in Korea: International Study of Asthma and Allergies in Childhood. Allergy Asthma Immunol Res 2: 61 10.4168/aair.2010.2.2.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ (2009) Status of childhood asthma in the United States, 1980–2007. Pediatrics 123 Suppl 3S131–S145 10.1542/peds.2008-2233C [DOI] [PubMed] [Google Scholar]
- 4. Hansen TE, Evjenth B, Holt J (2013) Increasing prevalence of asthma, allergic rhinoconjunctivitis and eczema among schoolchildren: three surveys during the period 1985–2008. Acta Paediatr Oslo Nor 1992 102: 47–52 10.1111/apa.12030 [DOI] [PubMed] [Google Scholar]
- 5. Van Schayck OCP (2013) Global strategies for reducing the burden from asthma. Prim Care Respir J J Gen Pract Airw Group 22: 239–243 10.4104/pcrj.2013.00052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Masoli M, Fabian D, Holt S, Beasley R, Global Initiative for Asthma (GINA) Program (2004) The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy 59: 469–478 10.1111/j.1398-9995.2004.00526.x [DOI] [PubMed] [Google Scholar]
- 7. Wong GWK, Chow CM (2008) Childhood asthma epidemiology: insights from comparative studies of rural and urban populations. Pediatr Pulmonol 43: 107–116 10.1002/ppul.20755 [DOI] [PubMed] [Google Scholar]
- 8. Kwak ES, Just A, Whyatt R, Miller RL (2009) Phthalates, Pesticides, and Bisphenol-A Exposure and the Development of Nonoccupational Asthma and Allergies: How Valid Are the Links? Open Allergy J 2: 45–50 10.2174/1874838400902010045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nakajima Y, Goldblum RM, Midoro-Horiuti T (2012) Fetal exposure to bisphenol A as a risk factor for the development of childhood asthma: an animal model study. Environ Health Glob Access Sci Source 11: 8 10.1186/1476-069X-11-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yang YJ, Hong YC, Oh SY, Park MS, Kim H, et al. (2009) Bisphenol A exposure is associated with oxidative stress and inflammation in postmenopausal women. Environ Res 109: 797–801 10.1016/j.envres.2009.04.014 [DOI] [PubMed] [Google Scholar]
- 11. Calafat AM, Kuklenyik Z, Reidy JA, Caudill SP, Ekong J, et al. (2005) Urinary concentrations of bisphenol A and 4-nonylphenol in a human reference population. Environ Health Perspect 113: 391–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shankar A, Teppala S (2011) Relationship between urinary bisphenol A levels and diabetes mellitus. J Clin Endocrinol Metab 96: 3822–3826 10.1210/jc.2011-1682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Silver MK, O’Neill MS, Sowers MR, Park SK (2011) Urinary bisphenol A and type-2 diabetes in U.S. adults: data from NHANES 2003–2008. PloS One 6: e26868 10.1371/journal.pone.0026868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Melzer D, Gates P, Osborne NJ, Osborn NJ, Henley WE, et al. (2012) Urinary bisphenol a concentration and angiography-defined coronary artery stenosis. PloS One 7: e43378 10.1371/journal.pone.0043378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Melzer D, Osborne NJ, Henley WE, Cipelli R, Young A, et al. (2012) Urinary bisphenol A concentration and risk of future coronary artery disease in apparently healthy men and women. Circulation 125: 1482–1490 10.1161/CIRCULATIONAHA.111.069153 [DOI] [PubMed] [Google Scholar]
- 16. Bae S, Kim JH, Lim YH, Park HY, Hong YC (2012) Associations of bisphenol A exposure with heart rate variability and blood pressure. Hypertension 60: 786–793 10.1161/HYPERTENSIONAHA.112.197715 [DOI] [PubMed] [Google Scholar]
- 17. Lee MR, Park H, Bae S, Lim YH, Kim JH, et al. (2014) Urinary bisphenol A concentrations are associated with abnormal liver function in the elderly: a repeated panel study. J Epidemiol Community Health 68: 312–317 10.1136/jech-2013-202548 [DOI] [PubMed] [Google Scholar]
- 18. Braun JM, Kalkbrenner AE, Calafat AM, Yolton K, Ye X, et al. (2011) Impact of early-life bisphenol A exposure on behavior and executive function in children. Pediatrics 128: 873–882 10.1542/peds.2011-1335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Li D, Zhou Z, Qing D, He Y, Wu T, et al. (2010) Occupational exposure to bisphenol-A (BPA) and the risk of self-reported male sexual dysfunction. Hum Reprod Oxf Engl. 25: 519–527 10.1093/humrep/dep381 [DOI] [PubMed] [Google Scholar]
- 20. Li DK, Zhou Z, Miao M, He Y, Qing D, et al. (2010) Relationship between urine bisphenol-A level and declining male sexual function. J Androl 31: 500–506 10.2164/jandrol.110.010413 [DOI] [PubMed] [Google Scholar]
- 21. Meeker JD, Ehrlich S, Toth TL, Wright DL, Calafat AM, et al. (2010) Semen quality and sperm DNA damage in relation to urinary bisphenol A among men from an infertility clinic. Reprod Toxicol Elmsford N 30: 532–539 10.1016/j.reprotox.2010.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Li DK, Zhou Z, Miao M, He Y, Wang J, et al. (2011) Urine bisphenol-A (BPA) level in relation to semen quality. Fertil Steril. 95: 625–630.e1–e4 10.1016/j.fertnstert.2010.09.026 [DOI] [PubMed] [Google Scholar]
- 23. Chou WC, Chen JL, Lin CF, Chen YC, Shih FC, et al. (2011) Biomonitoring of bisphenol A concentrations in maternal and umbilical cord blood in regard to birth outcomes and adipokine expression: a birth cohort study in Taiwan. Environ Health Glob Access Sci Source 10: 94 10.1186/1476-069X-10-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wolff MS, Teitelbaum SL, Pinney SM, Windham G, Liao L, et al. (2010) Investigation of relationships between urinary biomarkers of phytoestrogens, phthalates, and phenols and pubertal stages in girls. Environ Health Perspect 118: 1039–1046 10.1289/ehp.0901690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wolff MS, Britton JA, Boguski L, Hochman S, Maloney N, et al. (2008) Environmental exposures and puberty in inner-city girls. Environ Res 107: 393–400 10.1016/j.envres.2008.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Braun JM, Yolton K, Dietrich KN, Hornung R, Ye X, et al. (2009) Prenatal bisphenol A exposure and early childhood behavior. Environ Health Perspect 117: 1945–1952 10.1289/ehp.0900979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sugiura-Ogasawara M, Ozaki Y, Sonta S, Makino T, Suzumori K (2005) Exposure to bisphenol A is associated with recurrent miscarriage. Hum Reprod Oxf Engl 20: 2325–2329 10.1093/humrep/deh888 [DOI] [PubMed] [Google Scholar]
- 28. Cantonwine D, Meeker JD, Hu H, Sánchez BN, Lamadrid-Figueroa H, et al. (2010) Bisphenol a exposure in Mexico City and risk of prematurity: a pilot nested case control study. Environ Health Glob Access Sci Source 9: 62 10.1186/1476-069X-9-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bonds RS, Midoro-Horiuti T (2013) Estrogen effects in allergy and asthma. Curr Opin Allergy Clin Immunol 13: 92–99 10.1097/ACI.0b013e32835a6dd6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lee MH, Chung SW, Kang BY, Park J, Lee CH, et al. (2003) Enhanced interleukin-4 production in CD4+ T cells and elevated immunoglobulin E levels in antigen-primed mice by bisphenol A and nonylphenol, endocrine disruptors: involvement of nuclear factor-AT and Ca2+. Immunology 109: 76–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sawai C, Anderson K, Walser-Kuntz D (2003) Effect of bisphenol A on murine immune function: modulation of interferon-gamma, IgG2a, and disease symptoms in NZB X NZW F1 mice. Environ Health Perspect 111: 1883–1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tian X, Takamoto M, Sugane K (2003) Bisphenol A promotes IL-4 production by Th2 cells. Int Arch Allergy Immunol 132: 240–247 doi:74305 [DOI] [PubMed] [Google Scholar]
- 33. Yan H, Takamoto M, Sugane K (2008) Exposure to Bisphenol A prenatally or in adulthood promotes T(H)2 cytokine production associated with reduction of CD4CD25 regulatory T cells. Environ Health Perspect 116: 514–519 10.1289/ehp.10829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Midoro-Horiuti T, Tiwari R, Watson CS, Goldblum RM (2010) Maternal bisphenol a exposure promotes the development of experimental asthma in mouse pups. Environ Health Perspect 118: 273–277 10.1289/ehp.0901259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Van Winkle LS, Murphy SR, Boetticher MV, VandeVoort CA (2013) Fetal exposure of rhesus macaques to bisphenol a alters cellular development of the conducting airway by changing epithelial secretory product expression. Environ Health Perspect 121: 912–918 10.1289/ehp.1206064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Spanier AJ, Kahn RS, Kunselman AR, Hornung R, Xu Y, et al. (2012) Prenatal exposure to bisphenol A and child wheeze from birth to 3 years of age. Environ Health Perspect 120: 916–920 10.1289/ehp.1104175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Donohue KM, Miller RL, Perzanowski MS, Just AC, Hoepner LA, et al. (2013) Prenatal and postnatal bisphenol A exposure and asthma development among inner-city children. J Allergy Clin Immunol 131: 736–742 10.1016/j.jaci.2012.12.1573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Lakind JS, Naiman DQ (2011) Daily intake of bisphenol A and potential sources of exposure: 2005–2006 National Health and Nutrition Examination Survey. J Expo Sci Environ Epidemiol 21: 272–279 10.1038/jes.2010.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hong SB, Hong YC, Kim JW, Park EJ, Shin MS, et al. (2013) Bisphenol A in relation to behavior and learning of school-age children. J Child Psychol Psychiatry 54: 890–899 10.1111/jcpp.12050 [DOI] [PubMed] [Google Scholar]
- 40. Sumino K, Sugar EA, Irvin CG, Kaminsky DA, Shade D, et al. (2012) Methacholine challenge test: diagnostic characteristics in asthmatic patients receiving controller medications. J Allergy Clin Immunol 130: 69–75.e6 10.1016/j.jaci.2012.02.025 [DOI] [PubMed] [Google Scholar]
- 41.Fu L, Freishtat RJ, Gordish-Dressman H, Teach SJ, Resca L, et al.. (2014) Natural progression of childhood asthma symptoms and strong influence of gender and puberty. Ann Am Thorac Soc. doi:10.1513/AnnalsATS.201402-084OC. [DOI] [PMC free article] [PubMed]
- 42. Clark NM, Dodge JA, Thomas LJ, Andridge RR, Awad D, et al. (2010) Asthma in 10- to 13-year-olds: challenges at a time of transition. Clin Pediatr (Phila) 49: 931–937 10.1177/0009922809357339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Protudjer JLP, Lundholm C, Bergström A, Kull I, Almqvist C (2014) Puberty and asthma in a cohort of Swedish children. Ann Allergy Asthma Immunol Off Publ Am Coll Allergy Asthma Immunol 112: 78–79 10.1016/j.anai.2013.10.015 [DOI] [PubMed] [Google Scholar]
- 44.Postma DS (2007) Gender differences in asthma development and progression. Gend Med 4 Suppl B: S133–S146. [DOI] [PubMed]
- 45. Almqvist C, Worm M, Leynaert B, working group of GA2LEN WP 2.5 Gender (2008) Impact of gender on asthma in childhood and adolescence: a GA2LEN review. Allergy 63: 47–57 10.1111/j.1398-9995.2007.01524.x [DOI] [PubMed] [Google Scholar]
- 46. Song S, Zhang L, Zhang H, Wei W, Jia L (2014) Perinatal BPA exposure induces hyperglycemia, oxidative stress and decreased adiponectin production in later life of male rat offspring. Int J Environ Res Public Health 11: 3728–3742 10.3390/ijerph110403728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Aboul Ezz HS, Khadrawy YA, Mourad IM (2013) The effect of bisphenol A on some oxidative stress parameters and acetylcholinesterase activity in the heart of male albino rats. Cytotechnology. doi:10.1007/s10616-013-9672-1. [DOI] [PMC free article] [PubMed]
- 48. Hassan ZK, Elobeid MA, Virk P, Omer SA, ElAmin M, et al. (2012) Bisphenol A induces hepatotoxicity through oxidative stress in rat model. Oxid Med Cell Longev 2012: 194829 10.1155/2012/194829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. D’Cruz SC, Jubendradass R, Mathur PP (2012) Bisphenol A induces oxidative stress and decreases levels of insulin receptor substrate 2 and glucose transporter 8 in rat testis. Reprod Sci Thousand Oaks Calif 19: 163–172 10.1177/1933719111415547 [DOI] [PubMed] [Google Scholar]
- 50. Tiwari D, Kamble J, Chilgunde S, Patil P, Maru G, et al. (2012) Clastogenic and mutagenic effects of bisphenol A: an endocrine disruptor. Mutat Res 743: 83–90 10.1016/j.mrgentox.2011.12.023 [DOI] [PubMed] [Google Scholar]
- 51. Anjum S, Rahman S, Kaur M, Ahmad F, Rashid H, et al. (2011) Melatonin ameliorates bisphenol A-induced biochemical toxicity in testicular mitochondria of mouse. Food Chem Toxicol Int J Publ Br Ind Biol Res Assoc 49: 2849–2854 10.1016/j.fct.2011.07.062 [DOI] [PubMed] [Google Scholar]
- 52. Esposito S, Tenconi R, Lelii M, Preti V, Nazzari E, et al. (2014) Possible molecular mechanisms linking air pollution and asthma in children. BMC Pulm Med 14: 31 10.1186/1471-2466-14-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Levy BD, Bonnans C, Silverman ES, Palmer LJ, Marigowda G, et al. (2005) Diminished lipoxin biosynthesis in severe asthma. Am J Respir Crit Care Med 172: 824–830 10.1164/rccm.200410-1413OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Vollmer WM, Osborne ML, Buist AS (1998) 20-year trends in the prevalence of asthma and chronic airflow obstruction in an HMO. Am J Respir Crit Care Med 157: 1079–1084 10.1164/ajrccm.157.4.9704140 [DOI] [PubMed] [Google Scholar]
- 55. Vink NM, Postma DS, Schouten JP, Rosmalen JGM, Boezen HM (2010) Gender differences in asthma development and remission during transition through puberty: the TRacking Adolescents’ Individual Lives Survey (TRAILS) study. J Allergy Clin Immunol 126: 498–504.e1–e6 10.1016/j.jaci.2010.06.018 [DOI] [PubMed] [Google Scholar]
- 56. Cai Y, Zhou J, Webb DC (2012) Estrogen stimulates Th2 cytokine production and regulates the compartmentalisation of eosinophils during allergen challenge in a mouse model of asthma. Int Arch Allergy Immunol 158: 252–260 10.1159/000331437 [DOI] [PubMed] [Google Scholar]
- 57. Jing H, Wang Z, Chen Y (2012) Effect of oestradiol on mast cell number and histamine level in the mammary glands of rat. Anat Histol Embryol 41: 170–176 10.1111/j.1439-0264.2011.01120.x [DOI] [PubMed] [Google Scholar]
- 58. Sakai T, Furoku S, Nakamoto M, Shuto E, Hosaka T, et al. (2010) The soy isoflavone equol enhances antigen-specific IgE production in ovalbumin-immunized BALB/c mice. J Nutr Sci Vitaminol (Tokyo) 56: 72–76. [DOI] [PubMed] [Google Scholar]
- 59. Zaitsu M, Narita SI, Lambert KC, Grady JJ, Estes DM, et al. (2007) Estradiol activates mast cells via a non-genomic estrogen receptor-alpha and calcium influx. Mol Immunol 44: 1977–1985 10.1016/j.molimm.2006.09.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Macsali F, Real FG, Plana E, Sunyer J, Anto J, et al. (2011) Early age at menarche, lung function, and adult asthma. Am J Respir Crit Care Med 183: 8–14 10.1164/rccm.200912-1886OC [DOI] [PubMed] [Google Scholar]
- 61. Barr RG, Wentowski CC, Grodstein F, Somers SC, Stampfer MJ, et al. (2004) Prospective study of postmenopausal hormone use and newly diagnosed asthma and chronic obstructive pulmonary disease. Arch Intern Med 164: 379–386 10.1001/archinte.164.4.379 [DOI] [PubMed] [Google Scholar]
- 62. Braun JM, Hauser R (2011) Bisphenol A and children’s health. Curr Opin Pediatr 23: 233–239 10.1097/MOP.0b013e3283445675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Bauer SM, Roy A, Emo J, Chapman TJ, Georas SN, et al. (2012) The effects of maternal exposure to bisphenol A on allergic lung inflammation into adulthood. Toxicol Sci Off J Soc Toxicol 130: 82–93 10.1093/toxsci/kfs227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Tantisira KG, Colvin R, Tonascia J, Strunk RC, Weiss ST, et al. (2008) Airway responsiveness in mild to moderate childhood asthma: sex influences on the natural history. Am J Respir Crit Care Med 178: 325–331 10.1164/rccm.200708-1174OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Bushnik T, Haines D, Levallois P, Levesque J, Van Oostdam J, et al. (2010) Lead and bisphenol A concentrations in the Canadian population. Health Rep 21: 7–18. [PubMed] [Google Scholar]
- 66. Becker K, Göen T, Seiwert M, Conrad A, Pick-Fuss H, et al. (2009) GerES IV: phthalate metabolites and bisphenol A in urine of German children. Int J Hyg Environ Health. 212: 685–692 10.1016/j.ijheh.2009.08.002 [DOI] [PubMed] [Google Scholar]
- 67. Wilson NK, Chuang JC, Morgan MK, Lordo RA, Sheldon LS (2007) An observational study of the potential exposures of preschool children to pentachlorophenol, bisphenol-A, and nonylphenol at home and daycare. Environ Res 103: 9–20 10.1016/j.envres.2006.04.006 [DOI] [PubMed] [Google Scholar]
- 68. Völkel W, Colnot T, Csanády GA, Filser JG, Dekant W (2002) Metabolism and kinetics of bisphenol a in humans at low doses following oral administration. Chem Res Toxicol 15: 1281–1287. [DOI] [PubMed] [Google Scholar]
- 69. Stahlhut RW, Welshons WV, Swan SH (2009) Bisphenol A data in NHANES suggest longer than expected half-life, substantial nonfood exposure, or both. Environ Health Perspect 117: 784–789 10.1289/ehp.0800376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Christensen KLY, Lorber M, Koslitz S, Brüning T, Koch HM (2012) The contribution of diet to total bisphenol A body burden in humans: results of a 48 hour fasting study. Environ Int 50: 7–14 10.1016/j.envint.2012.09.002 [DOI] [PubMed] [Google Scholar]
- 71. Ye X, Wong LY, Bishop AM, Calafat AM (2011) Variability of urinary concentrations of bisphenol A in spot samples, first morning voids, and 24-hour collections. Environ Health Perspect 119: 983–988 10.1289/ehp.1002701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Ning G, Bi Y, Wang T, Xu M, Xu Y, et al. (2011) Relationship of urinary bisphenol A concentration to risk for prevalent type 2 diabetes in Chinese adults: a cross-sectional analysis. Ann Intern Med 155: 368–374 10.7326/0003-4819-155-6-201109200-00005 [DOI] [PubMed] [Google Scholar]
- 73. Cao XL, Corriveau J, Popovic S (2010) Bisphenol a in canned food products from canadian markets. J Food Prot 73: 1085–1089. [DOI] [PubMed] [Google Scholar]
- 74. Gerstenberger SL, Martinson A, Kramer JL (2010) An evaluation of mercury concentrations in three brands of canned tuna. Environ Toxicol Chem SETAC 29: 237–242 10.1002/etc.32 [DOI] [PubMed] [Google Scholar]
- 75. Vas J, Monestier M (2008) Immunology of mercury. Ann N Y Acad Sci 1143: 240–267 10.1196/annals.1443.022 [DOI] [PubMed] [Google Scholar]
- 76. Gardner RM, Nyland JF, Silbergeld EK (2010) Differential immunotoxic effects of inorganic and organic mercury species in vitro. Toxicol Lett 198: 182–190 10.1016/j.toxlet.2010.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Alves MFA, Fraiji NA, Barbosa AC, De Lima DSN, Souza JR, et al. (2006) Fish consumption, mercury exposure and serum antinuclear antibody in Amazonians. Int J Environ Health Res 16: 255–262 10.1080/09603120600734147 [DOI] [PubMed] [Google Scholar]
- 78. Nyland JF, Fillion M, Barbosa F, Shirley DL, Chine C, et al. (2011) Biomarkers of methylmercury exposure immunotoxicity among fish consumers in Amazonian Brazil. Environ Health Perspect 119: 1733–1738 10.1289/ehp.1103741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Vrijheid M, Slama R, Robinson O, Chatzi L, Coen M, et al. (2014) The human early-life exposome (HELIX): project rationale and design. Environ Health Perspect 122: 535–544 10.1289/ehp.1307204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Marcon A, Cerveri I, Wjst M, Antó J, Heinrich J, et al. (2014) Can an airway challenge test predict respiratory diseases? A population-based international study. J Allergy Clin Immunol 133: 104–110.e1–e4 10.1016/j.jaci.2013.03.040 [DOI] [PubMed] [Google Scholar]
- 81. Jayet PY, Schindler C, Künzli N, Zellweger JP, Brändli O, et al. (2005) Reference values for methacholine reactivity (SAPALDIA study). Respir Res 6: 131 10.1186/1465-9921-6-131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Aerts JG, Bogaard JM, Overbeek SE, Verbraak AF, Thio P (1994) Extrapolation of methacholine log-dose response curves with a Cumulative Gaussian Distribution function. Eur Respir J 7: 895–900. [PubMed] [Google Scholar]
- 83. Cockcroft DW, Berscheid BA (1983) Slope of the dose-response curve: usefulness in assessing bronchial responses to inhaled histamine. Thorax 38: 55–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Koh YY, Kang EK, Min YG, Kim CK (2002) The importance of maximal airway response to methacholine in the prediction of asthma development in patients with allergic rhinitis. Clin Exp Allergy J Br Soc Allergy Clin Immunol 32: 921–927. [DOI] [PubMed] [Google Scholar]
- 85. Sutherland ER, King TS, Icitovic N, Ameredes BT, Bleecker E, et al. (2010) A trial of clarithromycin for the treatment of suboptimally controlled asthma. J Allergy Clin Immunol 126: 747–753 10.1016/j.jaci.2010.07.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Weiss ST, Van Natta ML, Zeiger RS (2000) Relationship between increased airway responsiveness and asthma severity in the childhood asthma management program. Am J Respir Crit Care Med 162: 50–56 10.1164/ajrccm.162.1.9811005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This file contains Table S1, Table S2, Table S3, and Table S4. Table S1, Baseline characteristics of the study population included and excluded in the current study. Table S2, Association of urinary BPA concentrations (log transformed, µg BPA/g creatinine) at 7–8 years with incident asthma and PC20 over 11–12 years of age stratified by gender. Table S3, Association of urinary BPA concentrations (log transformed, µg BPA/g creatinine) at 7–8 years with wheezing, PC20, and asthma at 7–8, 9–10, and 11–12 years of age, including the children who had been diagnosed with asthma before 7–8 years of age. Table S4, Association of urinary BPA concentrations (log transformed, µg BPA/g creatinine) at 7–8 years with wheezing, PC20, and current asthma at 7–8, 9–10, and 11–12 years of age, excluding the children who satisfied the criteria of current asthma at the baseline survey.
(PDF)
Data set.
(CSV)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.