Abstract
Purpose
The purpose of this investigation was to estimate and document the reliability and validity of the Anterior Knee Pain Scale (AKPS) and to estimate its relative prediction accuracy of anterior knee pain in young females.
Methods
Data from a prospective, epidemiologic study to diagnose patellofemoral knee pain among female athletes (n = 499) using the Anterior Knee Pain Scale (AKPS). Data were treated in 4 phases (descriptive phase, reliability phase, scale refinement phase) and a final validation stage that was focused on an effort to test and document the validation of the AKPS short form and perform head-to-head comparisons of the 6-item short form with the original, 13-item form.
Results
The AKPS was reduced from 13 items (αCoeff = 0.77, σSEM = 0.004) to 6 items (αCoeff = 0.78, σSEM = 0.004). Point-biserial correlations with patel-lofemoral pain diagnosis were comparable: r [498] = 0.70 (R2 = 0.49, short form) and r [498] = 0.71 (R2 = 0.51, long form), as was sensitivity: 84 % (short form) and 80 % (long form), and specificity: 89 % (short form) and 90 % (long form; AUC = 0.94 both).
Conclusion
The current analyses indicate that a subset of measures from the AKPS is responsive to patellofemoral pain symptoms and may support screening for related diagnoses. A simpler and quicker scale optimized for diagnostic accuracy could reduce the demand on patients, clinicians and research teams focused on the identification and management of patellofemoral pain.
Keywords: Patellofemoral pain syndrome, Anterior knee pain, Patient-reported outcomes, Scale development, Knee injury
Introduction
There are an estimated 30 million school-aged youth who participate in organized sports in the USA [1]. This represents a 21 % increase over the past decade [24]. Of these 30 million participants, 34 % of middle school and 38 % of high school-aged participants will become injured and seek medical treatment at a cost of $1.8 billion dollars per annum in the USA [1, 18]. In young girls, the knee is the most common joint injured [1, 22]. Up to fifty-four per cent of athletes experience some form of knee pain each year [6, 9]. Girls are more likely than boys to sustain a knee injury [22, 25, 34]. Adolescent girls suffer anterior knee pain two to ten times more frequently than similar aged males [27]. The symptoms of anterior knee pain may cause up to 74 % of females to limit their sport participation or even cease participation altogether [3, 10, 38]. The symptoms of knee pain and injury also initiate unfavourable body composition changes in young girls and may be related to increased risk of more severe injury as they mature [26, 28]. The high recurrence rates and relatively poor results of treatment and long-term prognosis of patellofemoral pain indicate that preventive strategies may be the most useful approach to reduce morbidity associated with this condition [3, 7, 30].
The Anterior Knee Pain Scale (AKPS) was developed with a focus on determination of the most relevant questions to ascertain patellofemoral pain [20]. These authors based their scale development on the modified Larson scale [21, 32] and systematically developed their questions based on three criteria. “(1) Some questions should specifically address anterior knee pain symptoms; (2) the patient should complete the questionnaire independently; and (3) the total scores should be easily and quickly calculated”. The development of this highly respected knee scale also related objective measures of patellar alignment and position to subjective questions. The resultant AKPS is a 13-item self-report questionnaire that evaluates subjective responses to specific activities and symptoms that are thought to correlate with anterior knee pain syndrome. The AKPS is scored from a minimum score of 0 to a maximum score of 100 points. Lower scores indicate greater pain and disability [20].
The AKPS has been previously utilized to support large-scale prospective mechanistic and epidemiological investigations in youth [27]; however, its use in younger populations has required modifications that include terminology definitions (e.g. define “atrophy”) to help clarify the meaning of the questionnaire to its targeted audience [20]. The objective of this project was to investigate and document the reliability and validity of the modified Anterior Knee Pain Scale (AKPS) relative to the prediction accuracy of patellofemoral pain diagnosis in young females. Our corollary purpose was to evaluate these instruments at the subscale and item levels to determine the most relevant items to develop a reduced scale to support the diagnosis and classification of anterior knee pain in adolescents. The hypothesis was that the modified AKPS scale items would show a consistent relationship with patellofemoral pain diagnosis. The corollary hypothesis was that reduced subscale items would provide valid response to patellofemoral pain diagnosis in young girls.
Materials and methods
The data utilized for this investigation was derived from a large prospective epidemiology study focused on the determination of the pathomechanics that underlie patellofemoral pain incidence in young females. For the current investigation, female basketball, soccer and volleyball players (n = 499) were recruited from a single county public school district in Kentucky consisting of five middle schools and 4 high schools. All athletes between the ages of 11.0–18.1 years (mean 14.1 ± 1.8 years) who were enrolled in the project and completed both pre- and postseason (n = 1,021 completed visits) screenings relative to their sport were included in the study analysis (n = 499). The demographics of the study participants are included in Table 1.
Table 1.
Demographic characteristics of participants (N = 499)
| Variable | n | (%) |
|---|---|---|
| Child gender | ||
| Female | 499 | 100 |
| Child ethnicity | ||
| African American | 39 | 7.8 |
| Caucasian | 431 | 86.4 |
| Hispanic | 8 | 1.6 |
| Asian | 10 | 2 |
| American Indian | 8 | 1.6 |
| Education level | ||
| Middle school | 242 | 48.5 |
| High school | 257 | 51.5 |
| Pubertal status | ||
| Prepubertal | 27 | 5.4 |
| Pubertal | 249 | 49.9 |
| Post-pubertal | 223 | 44.7 |
| Sport participation | ||
| Soccer | 132 | 26.5 |
| Volleyball | 143 | 28.7 |
| Basketball | 224 | 44.8 |
Procedures
Parental consent and athlete assent were obtained prior to data collection. Subjects were tested prior to the start of and following their competitive seasons. Testing consisted of completion of the Anterior Knee Pain Scale (AKPS), International Knee Documentation Committee (IKDC) form, standardized history and physician-administered physical examination to determine the presence of patellofemoral pain. To determine reliability and stability measures over time, a sub-sample of athletes was selected (both positive and negative for patellofemoral pain diagnosis) for use in analyses of repeated measures.
AKPS scale screening
The initial injury screening process included the Anterior Knee Pain Scale (AKPS) questionnaire [20]. The scale is composed of 13 items that evaluate subjective symptoms and functional limitations. Minimum score is 0 points and maximum score is 100 points. An athlete with no sign of anterior knee pain would have a score of 100. All subjects with a positive AKPS (score less than 100) underwent further assessment to determine patellofemoral pain diagnosis. The AKPS is reported to be responsive, valid and demonstrate high test–retest reliability [8, 37].
Patellofemoral pain diagnosis
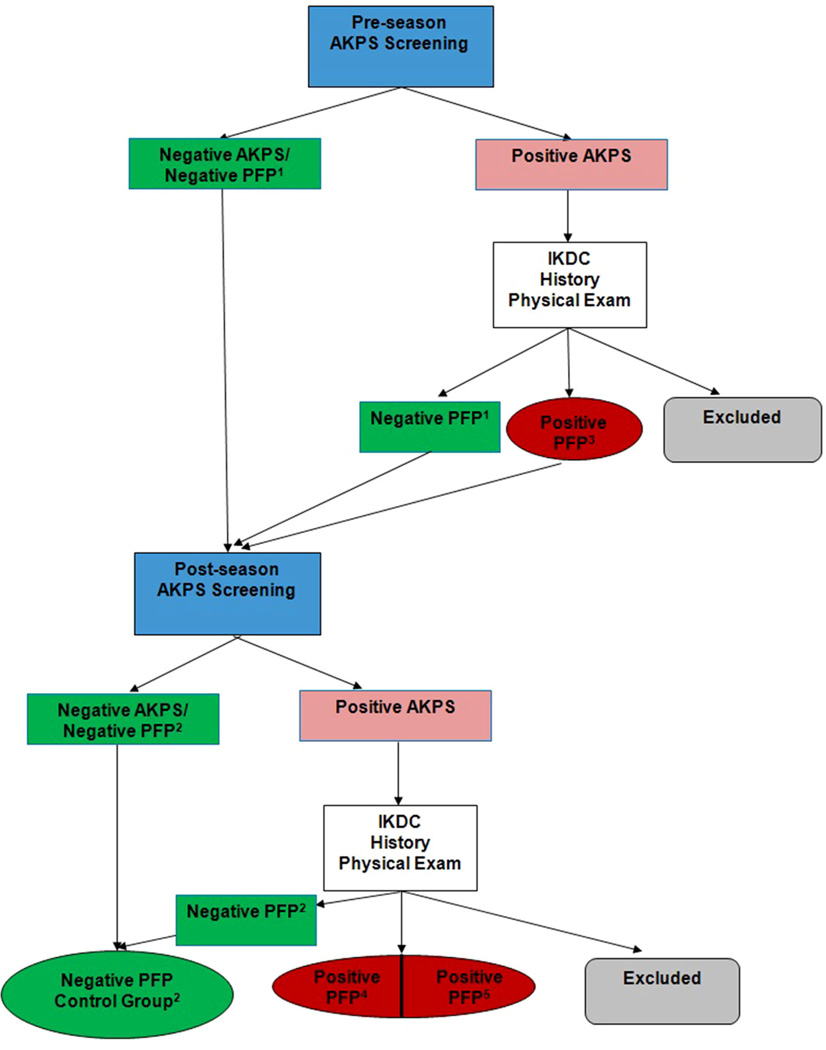
If any athlete provided an AKPS score <100, they underwent further assessment, which included an International Knee Documentation Committee (IKDC) score for the right and left knee, a personal interview regarding current and prior knee symptoms, limitations, history and a knee physical examination by the same investigator (Fig. 1). The standardized personal interview included questions regarding the subject’s severity of knee pain, participation time missed due to knee pain, timing of knee pain with activity, post-play knee pain, duration of knee pain, symptoms of knee instability and if the athlete had been evaluated by her personal physician or a specialist for the knee pain. The physical examination included palpation for tenderness at: medial patellofemoral ligament (MPFL), medial and lateral patellofemoral joint, medial and lateral femoral–tibial joint line, medial or lateral plica within patellofemoral joint, Gerdy’s tubercle and iliotibial band, pes anserine bursa, distal pole of patella, tibial tubercle, Hoffa’s fat pad, quadriceps tendon and patella tendon. Clinical tests for ligament instability, meniscal tear and patella apprehension and mobility were also performed.
Fig. 1.
Diagnosis pathway used to determine patellofemoral pain outcome. 1Negative patellofemoral pain pretest; 2negative patellofemoral pain post-test; 3positive patellofemoral pain pretest; 4positive patellofemoral pain post-test; 5negative patellofemoral pain pretest; positive patellofemoral pain post-test
Subjects were diagnosed with active patellofemoral pain if they presented with AKPS score <100; knee pain with or shortly following activity and also if anterior knee tenderness was present at the MPFL; medial patella facet tenderness and/or lateral patella facet tenderness; Hoffa’s fat pad syndrome with fat pad swelling and tenderness over the medial and/or lateral fat pad; and plica if tenderness was present over a palpable fibrous longitudinal band between the patella and femoral condyle.
The Cincinnati Children’s Hospital Medical Center Institutional Review Board approved the data collection procedures and consent forms. IRB approval number is 2009-0602.
Statistical analysis
The current study was a retrospective analysis of an existing prospective dataset obtained from adolescent athletes during a prescreening evaluation of lower extremity function prior to and following their competitive sport seasons. Data analysis consisted of four discrete stages: a descriptive phase, a reliability phase, a scale refinement phase and a validation phase. The criterion for statistical significance was set at α = 0.05 level across all analyses. Data were analysed using SAS version 9.2 and Winsteps version 3.68 software.
Descriptive phase
Traditional descriptive statistics were first computed for all 13 items, individually. Spearman correlations were used to evaluate associations among the items and with respect to the AKPS total score. Response patterns, monotonicity and polarity were also investigated for each item. Due to the insufficient number of response frequencies, a decision was made to convert the polytomous response patterns into a binary response format for analysis. In addition, Rasch measures of endorsability were generated for each item complete with standard errors (precision) and item-level fit statistics.
Reliability phase
Cronbach’s alpha was first calculated to estimate internal consistency of the 13-item scale. Standard errors of measurement were computed for each item at baseline and then averaged to provide an overall estimate of item-level precision for the entire scale.
Scale refinement phase
In an effort to construct a smaller, more efficient form of the AKPS, a subset of 6 AKPS items was identified from the information obtained in descriptive and reliability phases. Reliability estimates were then recomputed using the reduced, 6-item subset of items to document more formally the statistical properties of the reduced AKPS scale. Exploratory factor analysis with a varimax was then used to verify the dimensionality of the new 6-item scale.
Validation phase
A head-to-head comparison of the 6-item short form with the original, 13-item form was conducted as follows: A Spearman-rho correlation coefficient was computed to estimate degree of relationship between the two forms; a point-biserial correlation coefficient was computed between AKPS total scores and patellofemoral pain physician diagnosis (yes, no) to estimate the criterion-related validity; and finally, estimates of sensitivity and specificity were generated using area under the curve values to estimate the predictive validity for both forms of the scale.
Results
Descriptive phase
AKPS total scores ranged from a low of 0 to a high of 13 across all 499 children. Rasch difficulty estimates ranged from −3.29 (easy to endorse) to 3.00 (difficult to endorse). Point-measure correlations ranged from 0.33 to 0.90 (moderate to very high) with standard errors of 0.18–0.31, respectively, for the Rasch estimates (see Table 2).
Table 2.
AKPS item statistics
| Item | Number reporting symptoms |
Number reporting no symptoms |
13-item AKPS scale | 6-item AKPS short form | ||||
|---|---|---|---|---|---|---|---|---|
| Difficulty | Model SE |
Point measure |
Difficulty | Model SE |
Point measure |
|||
| 1 | 413 | 86 | −0.26 | 0.18 | 0.74 | |||
| 2 | 439 | 60 | 0.63 | 0.19 | 0.65 | |||
| 3 | 432 | 67 | 0.38 | 0.19 | 0.66 | 0.40 | 0.19 | 0.70 |
| 4 | 410 | 89 | −0.49 | 0.18 | 0.78 | |||
| 5 | 391 | 108 | −1.00 | 0.18 | 0.80 | −1.02 | 0.19 | 0.82 |
| 6 | 369 | 130 | −1.78 | 0.20 | 0.83 | |||
| 7 | 410 | 89 | −0.36 | 0.18 | 0.75 | −0.36 | 0.19 | 0.77 |
| 8 | 420 | 79 | −0.03 | 0.18 | 0.70 | |||
| 9 | 337 | 162 | −3.29 | 0.25 | 0.90 | −3.57 | 0.18 | 0.90 |
| 10 | 446 | 53 | 0.89 | 0.20 | 0.56 | 0.94 | 0.26 | 0.61 |
| 11 | 454 | 45 | 1.20 | 0.20 | 0.55 | 1.27 | 0.21 | 0.59 |
| 12 | 485 | 14 | 3.00 | 0.31 | 0.33 | |||
| 13 | 449 | 50 | 1.00 | 0.20 | 0.63 | |||
| Correlation between total score and PFP diagnosis | 0.72 (R2 = 0.52) | 0.72(R2 = 0.52) | ||||||
| Area under the curve (AUC) | 0.95 | 0.93 | ||||||
SE standard error, N = 499 patients
Reliability phase
Internal consistency for the 13-item, binary scale was α = 0.92 (very high) using Cronbach’s alpha, with an average standard error of measurement (SEM) across all 13 items of 0.003.
Scale refinement phase
A subset of six AKPS items (3, 5, 7, 9, 10, 11) was identified as yielding a smaller, more efficient form of the scale without loss of clinical or diagnostic ability. As can be seen from Table 2, Rasch difficulty (endorsability) estimates ranged from a low of −3.57 (easy to endorse) to a high of 1.27 (somewhat difficult to endorse) with point-measure correlations ranging from 0.59 to 0.90, with standard errors of 0.18–0.26. The internal consistency estimate for the 6-item AKPS short form was α = 0.88, with an average SEM = 0.004, indicating high precision for the 6-item scale. Exploratory factor analysis of the 6-item set confirmed the presence of a single, underlying factor.
Validation phase
The correlation between the 6-item short form and 13-item original form was calculated to be r(n = 1,021) = 0.96 with point-biserial calculations between total score for each form calculated to be r(n = 1,021) = 0.72, evidencing high criterion-related validity for both forms. Area under the curve (AUC) values were 0.95 (original form) and 0.93 (reduced form), respectively. When attempting to correctly identify patellofemoral pain physician diagnosis, a score of 4 on the short form and 10 on the original form yielded 82 % sensitivity and 91 % specificity.
Discussion
The most important finding of the present study was that a subset of measures from the AKPS is responsive to patellofemoral pain symptoms and may support screening for related diagnoses. The importance of these results is highlighted by the fact that thirty million school-aged youth participate in organized sports in the USA resulting in approximately four million sports-related injuries per year [1, 5, 12, 14]. Given the high prevalence of knee pain in this population, it is apparent that researchers must determine if the currently utilized outcome and diagnostic questionnaires originally developed for adults remain accurate for this target population. Surgeons and clinicians have long sought a self-reported outcome measure that was targeted specifically towards anterior knee pain and recommended the tool measure both pain and disability during the key activities of running, walking, ascending or descending stairs, squatting, jumping, kneeling and prolonged sitting [13, 37]. The Kujala Anterior Knee Pain scale (AKPS) addressed each of these functional components with the exception of kneeling. The current study represents the potential to develop more efficient scales optimized for diagnostic accuracy. The maintained validity of relationship to patellofemoral pain diagnosis could support clinicians in identification and management of the disorder.
When Kujala et al. developed the Anterior Knee Pain Scale in 1993, they did so with three basic principals in mind: (1) to specifically assess anterior knee pain symptoms, (2) the patient should be able to complete the questionnaire independently and (3) the total score should be easy to calculate [20]. To test the original questionnaire, it was administered to four groups of subjects: (1) those with reported anterior knee pain, (2) subjects with history of patella subluxation, (3) subjects with history of patella dislocation and (4) healthy controls with no prior anterior knee pain. They found that questions 1, 4, 6, 8, 9 and 11 were able to differentiate between all groups [20]. Overall, they found that question #11 (abnormal painful knee movement) best distinguished between groups; however, given that two groups had undergone subluxation or dislocation of the patella, it may not be the question but the inherent condition itself. The current study found that the 13-item AKPS scale is both a valid and reliable instrument. Specifically, the internal consistency was high supporting the usage of the AKPS to support clinical diagnosis of patellofemoral pain.
Subsequent testing of the AKPS on an adult population found that it had good content validity and was effective for identification of those patients with anterior knee pain [8, 37]. Test–retest reliability was shown to be high for the AKPS when given over a short period of time and also demonstrated moderate responsiveness and high reliability [8, 37]. Aside from the oversight of a question dealing with pain while kneeling, several other questions were determined to be ineffective in patients with anterior knee pain, including the questions dealing with limp, support, flexion deficiency and patellar subluxations [37]. A subsequent criticism of the AKPS was its focus on pain, rather than functional impairment [37]. In addition, previous research has shown that several questions (#11, #12, and #13; [20]) required clarification in order to be answered or subjects left those questions blank [37]. In addition, technical terms such as atrophy of the thigh and flexion may need further clarification when used in diagnostic scales to improve clarity for use in general populations [20].
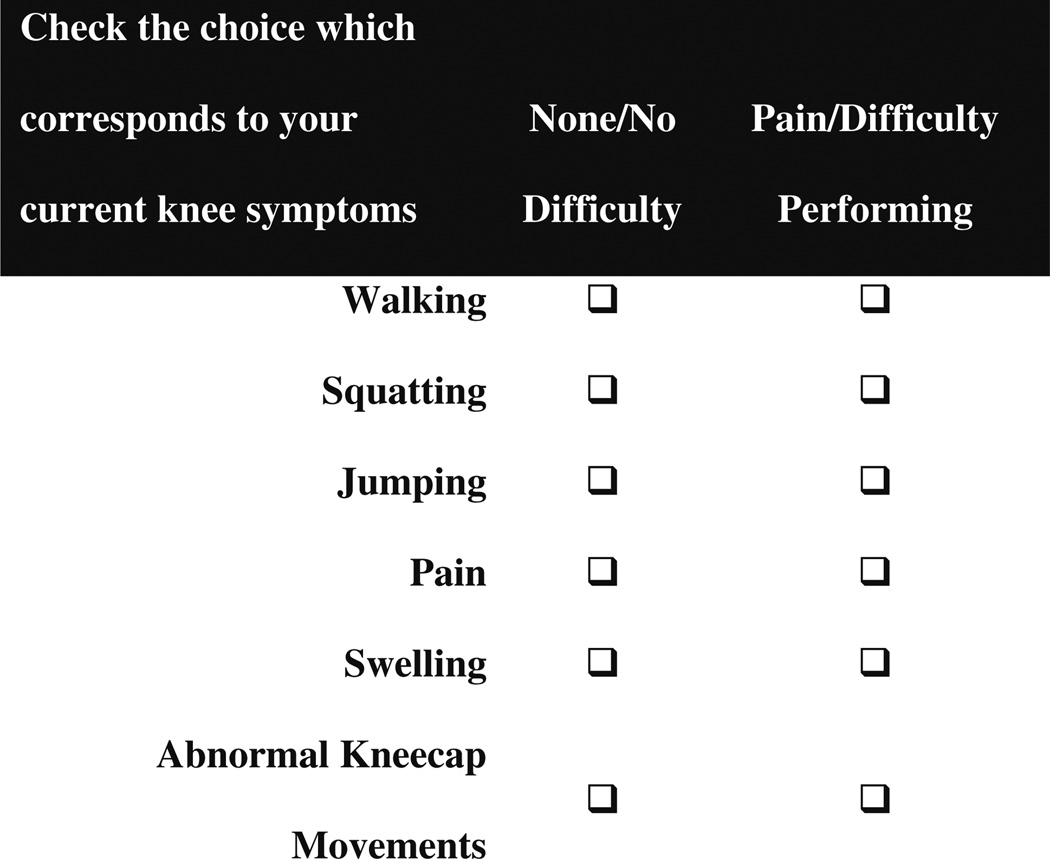
While the AKPS has been found to be effective and reliable in the adult population, modifications to the questionnaire to address the issues stated above, as well as to decrease the time necessary to complete, are appropriate to improve the functionality of the outcome measure. Similar to the IKDC and KOOS that have now had paediatric versions created [16, 19, 33], similar modifications may be warranted to the AKPS to make it easier to understand for the paediatric population. Thus, building from the highly reliable scale, we were able to perform a scale refine phase to build a subset of questions which yielded more efficient form of the scale without loss of clinical or diagnostic ability. We have provided as an example the reduced scale questionnaire derived from the previous scale that can be used to support the diagnosis of patellofemoral pain in younger populations (Fig. 2). Based on clinical input and Rasch analyses techniques, the proposed reduced scale provides a desired range of acceptability and maintained the internal consistency similar to the original 13-item scale. Likewise, validation steps using ROC calculations for full and reduced forms of the scale were extremely similar, indicating high predictive validity for patellofemoral pain diagnosis. Future research is warranted to determine the reliability and validity of the reduced scale used in children and adolescents. In addition, the time and cost savings should be measured against any reductions in scale diagnostic accuracy to help further guide its usage in clinical practice.
Fig. 2.
Example of a reduced scale questionnaire derived from previous scale that can be used to support the diagnosis of patellofemoral pain in younger populations
While diagnostic criteria and validated patient-reported outcome tools used to assess knee function and symptoms have been developed for various knee disorders [4, 11, 15, 17, 21, 23, 31, 35], there have been few patient-reported knee outcome scales that have focused on patellofemoral pain [36]. There have been even fewer patient-reported tools developed that focused on the diagnostic differentiation and outcomes criteria for patellofemoral disorders [20]. To our knowledge, there are not any focused patellofemoral diagnostic tools developed and validated for use with children and adolescents. Without screening tools to improve accuracy of patellofemoral pain diagnosis and track outcomes in younger populations, a more complete understanding of underlying risk factors to incidence and aetiology of this condition will continue to be lacking [2, 29]. The gap in knowledge related to patellofemoral pain causal factors in youth limits the opportunity to intervene into the cascade of associated health concerns related to decreased fitness levels and obesity in adolescent and adult women [3, 26]. Likewise, the time commitment to use the AKPS for clinical research, combined with the unknown validity modified AKPS, may limit its utility in young, atrisk populations. The current report provides a potentially simpler and quicker scale optimized for diagnostic accuracy could reduce the demand on patients, clinicians and research teams focused on the identification and management of patellofemoral pain. In addition, the proposed scale may support screening large populations of young athletes in multi-centre trials to further advance management and potentially prevention of the patellofemoral pain disorder.
There are limitations to the current study. Patellofemoral pain in young athletes likely has a multi-factorial aetiology that may vary across different sports. The effects of sports played were not controlled or investigated in the current analyses. In addition, as both a strength and potential limitation, the current study was performed with athletes in a single county school district in a single laboratory that may limit the generalization to other sports or populations. Future investigations with larger and more diverse sampling will further support robust patellofemoral pain diagnostic models and will aid future investigations aimed to elucidate risk factors for this disorder.
Another limitation to consider is that the current analyses were limited to the accuracy of the clinical diagnoses of patellofemoral pain. While inter-rater error was controlled for by using trained a physician to perform all assessments, the complexity of this chronic disorder may create more diagnostic uncertainty relative to other acute knee injuries such as anterior cruciate ligament tear. Continued efforts to accurately classify patellofemoral pain into distinct injuries may allow for a better understanding of exact aetiologies contributing to the onset of this syndrome. However, the potential to improve diagnostic screening techniques with simplified scales that maintain or improve accuracy is the salient result of the current investigation.
Conclusions
The Anterior Knee Pain Scale (AKPS) has been previously utilized to support large-scale prospective mechanistic and epidemiological investigations in youth. The time commitment to use the AKPS for clinical research, combined with the unknown validity modified AKPS, may limit its utility in young, at-risk populations. A reduced six question AKPS shows similar reliability and validity to the original thirteen question scale and is simpler and quicker to complete.
Acknowledgments
The authors would like to thank Boone County Kentucky, School District, especially School Superintendent Randy Poe, for participation in this study. We would also like to thank Mike Blevins, Ed Massey, Dr. Brian Blavatt and the athletes of Boone County public school district for their participation in this study. All authors are independent of any commercial funder, had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. This work was supported by the National Institutes of Health/NIAMS Grants #R01-AR049735, #R01-AR05563 and #R01-AR056259.
Footnotes
This study was approved by the Cincinnati Children’s Hospital Institutional Review Board.
Conflict of interest The authors have no competing interests to declare.
Contributor Information
Gregory D. Myer, Email: greg.myer@cchmc.org, Division of Sports Medicine, Cincinnati Children’s Hospital Medical Center, 3333 Burnet Avenue; MLC 10001, Cincinnati, OH 45229, USA; Department of Pediatrics and Orthopaedic Surgery, University of Cincinnati, Cincinnati, OH, USA; Sports Medicine Sports Health and Performance Institute, The Ohio State University, Columbus, OH, USA; Micheli Center for Sports Injury Prevention, Boston, MA, USA.
Kim D. Barber Foss, Division of Sports Medicine, Cincinnati Children’s Hospital Medical Center, 3333 Burnet Avenue; MLC 10001, Cincinnati, OH 45229, USA Division of Health Sciences, Department of Athletic Training, College of Mount St. Joseph, Cincinnati, OH, USA.
Resmi Gupta, Division of Biostatistics and Epidemiology, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA.
Timothy E. Hewett, Division of Sports Medicine, Cincinnati Children’s Hospital Medical Center, 3333 Burnet Avenue; MLC 10001, Cincinnati, OH 45229, USA Department of Pediatrics and Orthopaedic Surgery, University of Cincinnati, Cincinnati, OH, USA; Sports Medicine Sports Health and Performance Institute, The Ohio State University, Columbus, OH, USA; Department of Physiology and Cell Biology, The Ohio State University, Columbus, OH, USA; Department Orthopaedic Surgery, The Ohio State University, Columbus, OH, USA; Department Biomedical Engineering, The Ohio State University, Columbus, OH, USA.
Richard F. Ittenbach, Division of Biostatistics and Epidemiology, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
References
- 1.Adirim TA, Cheng TL. Overview of injuries in the young athlete. Sports Med. 2003;33(1):75–81. doi: 10.2165/00007256-200333010-00006. [DOI] [PubMed] [Google Scholar]
- 2.Barber Foss KD, Myer GD, Chen SS, Hewett TE. Expected prevalence from the differential diagnosis of anterior knee pain in adolescent female athletes during preparticipation screening. J Athl Train. 2012;47(5):519–524. doi: 10.4085/1062-6050-47.5.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blond L, Hansen L. Patellofemoral pain syndrome in athletes: a 5.7-year retrospective follow-up study of 250 athletes. Acta Orthop Belg. 1998;64(4):393–400. [PubMed] [Google Scholar]
- 4.Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37(5):890–897. doi: 10.1177/0363546508330143. [DOI] [PubMed] [Google Scholar]
- 5.Burt CW, Overpeck MD. Emergency visits for sports-related injuries. Ann Emerg Med. 2001;37(3):301–308. doi: 10.1067/mem.2001.111707. [DOI] [PubMed] [Google Scholar]
- 6.Calmbach WL, Hutchens M. Evaluation of patients presenting with knee pain: Part I. History, physical examination, radiographs, and laboratory tests. Am Fam Physician. 2003;68(5):907–912. [PubMed] [Google Scholar]
- 7.Collins NJ, Crossley KM, Darnell R, Vicenzino B. Predictors of short and long term outcome in patellofemoral pain syndrome: a prospective longitudinal study. BMC Musculoskelet Disord. 2010;11:11. doi: 10.1186/1471-2474-11-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crossley KM, Bennell KL, Cowan SM, Green S. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil. 2004;85(5):815–822. doi: 10.1016/s0003-9993(03)00613-0. [DOI] [PubMed] [Google Scholar]
- 9.Fagan V, Delahunt E. Patellofemoral pain syndrome: a review on the associated neuromuscular deficits and current treatment options. Br J Sports Med. 2008;42(10):789–795. doi: 10.1136/bjsm.2008.046623. [DOI] [PubMed] [Google Scholar]
- 10.Fairbank JC, Pynsent PB, van Poortvliet JA, Phillips H. Mechanical factors in the incidence of knee pain in adolescents and young adults. J Bone Joint Surg Br. 1984;66(5):685–693. doi: 10.1302/0301-620X.66B5.6501361. [DOI] [PubMed] [Google Scholar]
- 11.Flandry F, Hunt JP, Terry GC, Hughston JC. Analysis of subjective knee complaints using visual analog scales. Am J Sports Med. 1991;19(2):112–118. doi: 10.1177/036354659101900204. [DOI] [PubMed] [Google Scholar]
- 12.Franklin CC, Weiss JM. Stopping sports injuries in kids: an overview of the last year in publications. Curr Opin Pediatr. 2012;24(1):64–67. doi: 10.1097/MOP.0b013e32834ec618. [DOI] [PubMed] [Google Scholar]
- 13.Harrison E, Magee D, Quinney H. Development of a clinical tool and patient questionnaire for evaluation of patellofemoral pain syndrome patients. Clin J Sport Med. 1996;6(3):163–170. doi: 10.1097/00042752-199607000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Ingram JG, Fields SK, Yard EE, Comstock RD. Epidemiology of knee injuries among boys and girls in US high school athletics. Am J Sports Med. 2008;36(6):1116–1122. doi: 10.1177/0363546508314400. [DOI] [PubMed] [Google Scholar]
- 15.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelborne KD. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 16.Iversen MD, Lee B, Connell P, Andersen J, Anderson AF, Kocher MS. Validity and comprehensibility of the international knee documentation committee subjective knee evaluation form in children. Scand J Med Sci Sports. 2010;20(1):e87–e95. doi: 10.1111/j.1600-0838.2009.00917.x. [DOI] [PubMed] [Google Scholar]
- 17.Kettelkamp DB, Thompson C. Development of a knee scoring scale. Clin Orthop Relat Res. 1975;107:93–99. doi: 10.1097/00003086-197503000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Knowles SB, Marshall SW, Bowling JM, Loomis D, Millikan R, Yang J, Weaver NL, Kalsbeek W, Mueller FO. A prospective study of injury incidence among North Carolina high school athletes. Am J Epidemiol. 2006;164(12):1209–1221. doi: 10.1093/aje/kwj337. [DOI] [PubMed] [Google Scholar]
- 19.Kocher MS, Smith JT, Iversen MD, Brustowicz K, Ogunwole O, Andersen J, Yoo WJ, McFeely ED, Anderson AF, Zurakowski D. Reliability, validity, and responsiveness of a modified International Knee Documentation Committee Subjective Knee Form (Pedi-IKDC) in children with knee disorders. Am J Sports Med. 2011;39(5):933–939. doi: 10.1177/0363546510383002. [DOI] [PubMed] [Google Scholar]
- 20.Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159–163. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 21.Larson R. Rating sheet for knee function. Diseases of the knee joint. Churchill-Livingston, Edinburgh. 1974:29–30. [Google Scholar]
- 22.Louw QA, Manilall J, Grimmer KA. Epidemiology of knee injuries among adolescents: a systematic review. Br J Sports Med. 2008;42(1):2–10. doi: 10.1136/bjsm.2007.035360. [DOI] [PubMed] [Google Scholar]
- 23.Marshall JL, Fetto JF, Botero PM. Knee ligament injuries: a standardized evaluation method. Clin Orthop Relat Res. 1977;123:115–129. [PubMed] [Google Scholar]
- 24.McGuine T. Sports injuries in high school athletes: a review of injury-risk and injury-prevention research. Clin J Sport Med. 2006;16(6):488–499. doi: 10.1097/01.jsm.0000248848.62368.43. [DOI] [PubMed] [Google Scholar]
- 25.Messina DF, Farney WC, DeLee JC. The incidence of injury in Texas high school basketball. A prospective study among male and female athletes. Am J Sports Med. 1999;27(3):294–299. doi: 10.1177/03635465990270030401. [DOI] [PubMed] [Google Scholar]
- 26.Myer GD, Faigenbaum AD, Foss KB, Xu Y, Khoury J, Dolan LM, McCambridge TM, Hewett TE. Injury initiates unfavourable weight gain and obesity markers in youth. Br J Sports Med. 2013 doi: 10.1136/bjsports-2012-091988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Myer GD, Ford KR, Barber Foss KD, Goodman A, Ceasar A, Rauh MJ, Divine JG, Hewett TE. The incidence and potential pathomechanics of patellofemoral pain in female athletes. Clin Biomech. 2010;25(7):700–707. doi: 10.1016/j.clinbiomech.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Myer GD, Ford KR, Di Stasi SL, Barber Foss KD, Micheli LJ, Hewett TE. High knee abduction moments are common risk factors for patellofemoral pain (PFP) and anterior cruciate ligament (ACL) injury in girls: Is PFP itself a predictor for subsequent ACL injury? Br J Sports Med. 2014 doi: 10.1136/bjsports-2013-092536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nijs J, Van Geel C, Van der Auwera C, Van de Velde B. Diagnostic value of five clinical tests in patellofemoral pain syndrome. Man Ther. 2006;11(1):69–77. doi: 10.1016/j.math.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 30.Nimon G, Murray D, Sandow M, Goodfellow J. Natural history of anterior knee pain: a 14- to 20-year follow-up of nonoperative management. J Pediatr Orthop. 1998;18(1):118–122. [PubMed] [Google Scholar]
- 31.O’Donoghue DH. An analysis of end results of surgical treatment of major injuries to the ligaments of the knee. J Bone Joint Surg Am. 1955;37-A(1):1–13. passim. [PubMed] [Google Scholar]
- 32.Oretorp N, Gillquist J, Liljedahl SO. Long term results of surgery for non-acute anteromedial rotatory instability of the knee. Acta Orthop Scand. 1979;50(3):329–336. doi: 10.3109/17453677908989774. [DOI] [PubMed] [Google Scholar]
- 33.Ortqvist M, Roos EM, Brostrom EW, Janarv PM, Iversen MD. Development of the Knee Injury and Osteoarthritis Outcome Score for children (KOOS-Child): comprehensibility and content validity. Acta Orthop. 2012;83(6):666–673. doi: 10.3109/17453674.2012.747921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Powell JW, Barber-Foss KD. Sex-related injury patterns among selected high school sports. Am J Sports Med. 2000;28(3):385–391. doi: 10.1177/03635465000280031801. [DOI] [PubMed] [Google Scholar]
- 35.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–49. [PubMed] [Google Scholar]
- 36.Turba JE, Walsh WM, McLeod WD. Long-term results of extensor mechanism reconstruction. A standard for evaluation. Am J Sports Med. 1979;7(2):91–94. doi: 10.1177/036354657900700204. [DOI] [PubMed] [Google Scholar]
- 37.Watson CJ, Propps M, Ratner J, Zeigler DL, Horton P, Smith SS. Reliability and responsiveness of the lower extremity functional scale and the anterior knee pain scale in patients with anterior knee pain. J Orthop Sports Phys Ther. 2005;35(3):136–146. doi: 10.2519/jospt.2005.35.3.136. [DOI] [PubMed] [Google Scholar]
- 38.Witvrouw E, Lysens R, Bellemans J, Cambier D, Vanderstraeten G. Intrinsic risk factors for the development of anterior knee pain in an athletic population. A two-year prospective study. Am J Sports Med. 2000;28(4):480–489. doi: 10.1177/03635465000280040701. [DOI] [PubMed] [Google Scholar]