Abstract
The indication for hepatocellular carcinoma (HCC) is expanding in living donor liver transplantation (LDLT). Early detection and effective management of recurrence has become an important issue in LDLT for HCC. This study aimed to find an optimal screening protocol in terms of screening interval and screening tools by analyzing recurrence pattern after LDLT for HCC. A total of 205 LDLT patients in two centers from February 1999 to October 2010 was reviewed. Recurrence appeared in 55 cases. Six risk factors for recurrence were identified: preoperative alpha-fetoprotein >400, Edmonson grade 3 or 4, tumor size >7 cm, tumor number ≥7, minimal tumor necrosis in the transarterial chemoembolization group and positive micro-vascular invasion. Four groups with different ranges of index scores showed different recurrence-free survival and median time to recurrence. Group I showed low and late recurrence. Groups II and III showed linearly increased rate of recurrence until 18 months. Group IV showed very early recurrence within 6 months. Across the groups, extra-hepatic recurrence developed in more than 40% of cases and multi-organ recurrence rate was 20%. The screening interval should be different based on the risk of recurrence. Screening should include work-up for extra-hepatic recurrence as well as intra-hepatic recurrence.
Graphical Abstract
Keywords: Carcinoma, Hepatocellular, Living Donors, Liver Transplantation, Recurrence, Screening
INTRODUCTION
Liver transplantation (LT) is an established curative therapeutic option for hepatocellular carcinoma (HCC) as it provides complete oncologic resection and correction of the underlying liver dysfunction. However, the long-term survival of HCC patients is unsatisfactory in some cases because of HCC recurrence after LT.
Several preoperative selection criteria including the Milan and University of California San Francisco (UCSF) criteria have been proposed to select patient subgroups to show comparable outcomes with non-HCC patients (1, 2). However, some patients who are not categorized by these criteria can show favorable outcome. Therefore, if patients with advanced HCC have no other effective treatment modality, and they and/or family members request living donor LT (LDLT), even with high chance of recurrence, the attending clinician does not have strong grounds to not grant the request. Because the indication of LDLT for HCC is expanding recently and the aggressiveness of tumor biology may not be readily recognized preoperatively in fast-track of LDLT, this may result in higher HCC recurrence in LDLT unlike DDLT (3).
Recurrence of HCC after LT results in significantly diminished survival. The prognosis after HCC recurrence depends on the time to recurrence and site of recurrence (4). Early recurrence on multiple sites is one of the poor prognostic factors. However, some patients have a good prognosis if they are appropriately treated after the recurrence (5). Therefore, early detection based on a well-designed screening protocol and earlier treatment may improve the long-term prognosis in recurrent HCC. However, few studies have sought to develop an adequate surveillance tool after LT for HCC.
This study sought to identify risk factors associated with HCC recurrence after LDLT and to suggest an optimal screening protocol in terms of screening interval and screening tools by analyzing the pattern of recurrence.
MATERIALS AND METHODS
Patients
From February 1999 to October 2010, 289 patients underwent LT for HCC at Seoul National University Hospital and Samsung Medical Center, Korea. Among them, 205 LDLT cases were retrospectively reviewed. The exclusion criteria were patients with deceased donor LT cases, patients with and patients who died from other factors than tumor recurrence within 6 months. On the basis of imaging studies, patients who met the Milan criteria were selected for LT. Magnetic resonance imaging (MRI), chest computed tomography (CT), bone scan and 18F-fluorodeoxyglucose positron emission tomography (18-FDG-PET) scans were performed preoperatively in all patients. We excluded patients with extrahepatic metastasis and major vascular invasion in this study. If patients were beyond the Milan criteria but strongly desired LDLT, we conducted the transplantations considering recipients' expected survival benefit from transplantation and tumor biologic factors based on the principle of "donor safety first" (6).
Demographics and definitions
Demographics and tumor characteristics were evaluated retrospectively by review of a clinical database and review of pathologic reports of explant livers. Tumor size was measured as the largest diameter of the major tumor (cm) irrespective of viability. Microvascular invasion was defined pathologically as microscopic vascular invasion of small vessels within the parenchyma of the liver. In case the waiting time was longer than 3 months, patients commonly underwent transarterial chemoembolization (TACE) as a bridge to LT. Post-transarterial chemoembolization tumor necrosis rate was evaluated by dividing the sum of the diameter of necrotic tissue by the sum of the nodule diameters.
Follow-up protocol after LT
All patients were followed up every 1 or 2 weeks for 2 postoperative months and every 3 to 6 weeks thereafter. The serum level of alpha-fetoprotein (AFP) was measured during every visit. Abdomino-pelvic CT or MRI was performed every 6 months for the first postoperative year and annually thereafter, or in case of increasing AFP levels. If an abdominal image did not reveal a recurrent lesion despite suspicion of recurrence, bone scanning, chest CT and 18-FDG PET were used.
Risk factor analysis
Ten variables were analyzed to determine the risk factors for HCC recurrence after LT. The pre-operative demographic characteristics included age, sex, serum AFP level, model for end-stage liver disease (MELD) score and pre-transplant adjuvant TACE. Factors related to tumor pathologic characteristics included tumor size, number of tumor lesions, Edmondson-Steiner grade, microvascular invasion and post-TACE tumor necrosis rate. Kaplan-Meier estimates of disease-free survival and recurrence were calculated and compared with the log-rank test. Hazard ratios (HR) were estimated using Cox proportional-hazards methodology and estimates are reported as HR (95% confidence interval). Forward stepwise selection using likelihood ratios for entry and exit criteria were used to develop the final multivariate Cox proportional hazards model. A P value<0.05 was considered statistically significant. The most significant cut-off values of continuous variables in final model (AFP, size and number) were obtained by multiple sessions of multivariate analysis using various cut-off values.
Grouping according to the risk index (number of risk factors)
The risk index (total risk) was developed using the regression coefficients from statistically significant risk factors for recurrence in the multivariate Cox model. A total risk of each patient was calculated after sum of the regression coefficients of each independent risk factor. The practical risk index was calculated as exp ([1.708 if preoperative serum AFP level>400]+[0.81 if tumor grade 3 or 4]+[0.794 if tumor size>7 cm]+[1.275 if tumor number≥7]+[1.168 if Post-TACE tumor necrosis≤ 60%]+[0.667 if positive microvascular invasion]). If no risk factors are present, the index score is equal to 1. The possible maximal risk index score is 615.2. Four groups were developed based upon the range of practical risk index to show most significant survival difference. Group I was defined as those patients without any risk factors (index score of 1). Patients with an index score from 1.1-10.0 were categorized as group II. Group III patients had index scores between 10.1 and 40.0. Patients with score>40.0 were categorized as group IV.
Ethics statement
This study was approved by the institutional review board of Seoul National University (IRB No. 1110-052-381). Informed consent was waived by the board.
RESULTS
Demographics and tumor characteristics
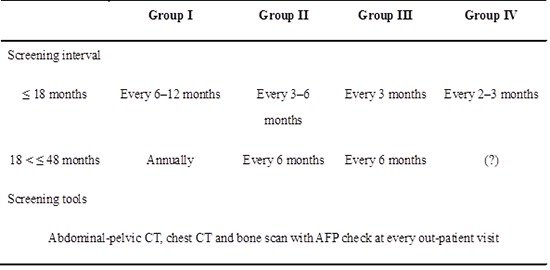
Baseline demographics and tumor characteristics are shown in Table 1. The mean age was 52±8 yr. The majority of patients were men (82%). Hepatitis B was the most common cause of the liver disease in 183 patients (89.3%). The median preoperative level of serum AFP was 27.0 ng/mL (range 1.0-95.725.5 ng/mL). The mean MELD score was 15.84±6.86 (range 7-44). The mean number of tumors was 2.35±2.04 (range 1-10). The mean diameter of the largest tumor was 3.54±3.1 cm (range 0.5-25 cm). Microvascular invasion was found in 22.4% of patients. One hundred thirty four patients (65.4%) had received pre-transplant TACE. Among them, the tumor necrosis rate was total (100%) in 10.4%, partial (60.1%-99.9%) in 26.9% and minimal (≤60%) in 62.7%.
Table 1.
Baseline and pathologic characteristics of 205 patients with hepatocellular carcinoma who underwent living donor liver transplantation
AFP, alpha-fetoprotein; HBV, hepatitis B; HCV, hepatitis C; MELD, model for end-stage liver disease; TACE, transarterial chemoembolization.
Post-operative complications in the donors
In this study, there was no donor mortality. The morbidity rate was 10% (6 out of 58 donors) in the beyond UCSF criteria group. The most common complications was biliary complications including bile leakage for the resection margin (n=5), followed by intraperitoenal bleeding (n=1) and ileus (n=1). Among these complications, there was no complication which was more than grade 3A according to the Clavien grading system.
Recurrence after LT
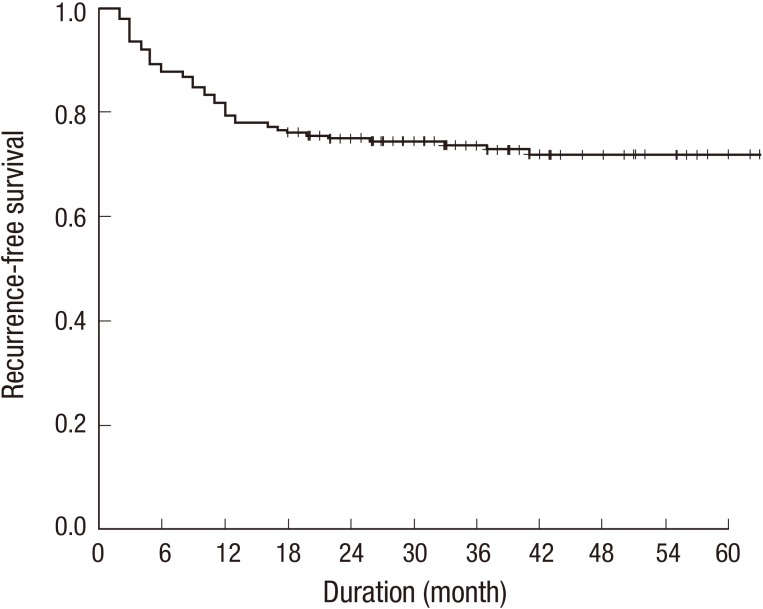
The 1-, 2-, and 5-yr patients' survival rates were 93%, 86%, and 75%, and grafts' survival rates were 100%, 100%, and 97%. Recurrence occurred in 55 cases (26.8%). One-year, 3-yr, and 5-yr recurrence-free survival (RFS) was 79.5%, 73.6%, and 71.8%, respectively (Fig. 1). Most recurrence occurred within 18 months. The majority of recurrences were extrahepatic: 43.6% of extrahepatic sites only, 36.4% of intrahepatic sites only and 20% of both sites. Extrahepatic sites presented most commonly in the bone (45.8%) and the lung (37.5%).
Fig. 1.
Recurrence free survival rate of 205 patients with hepatocellular carcinoma who underwent living donor liver transplantation.
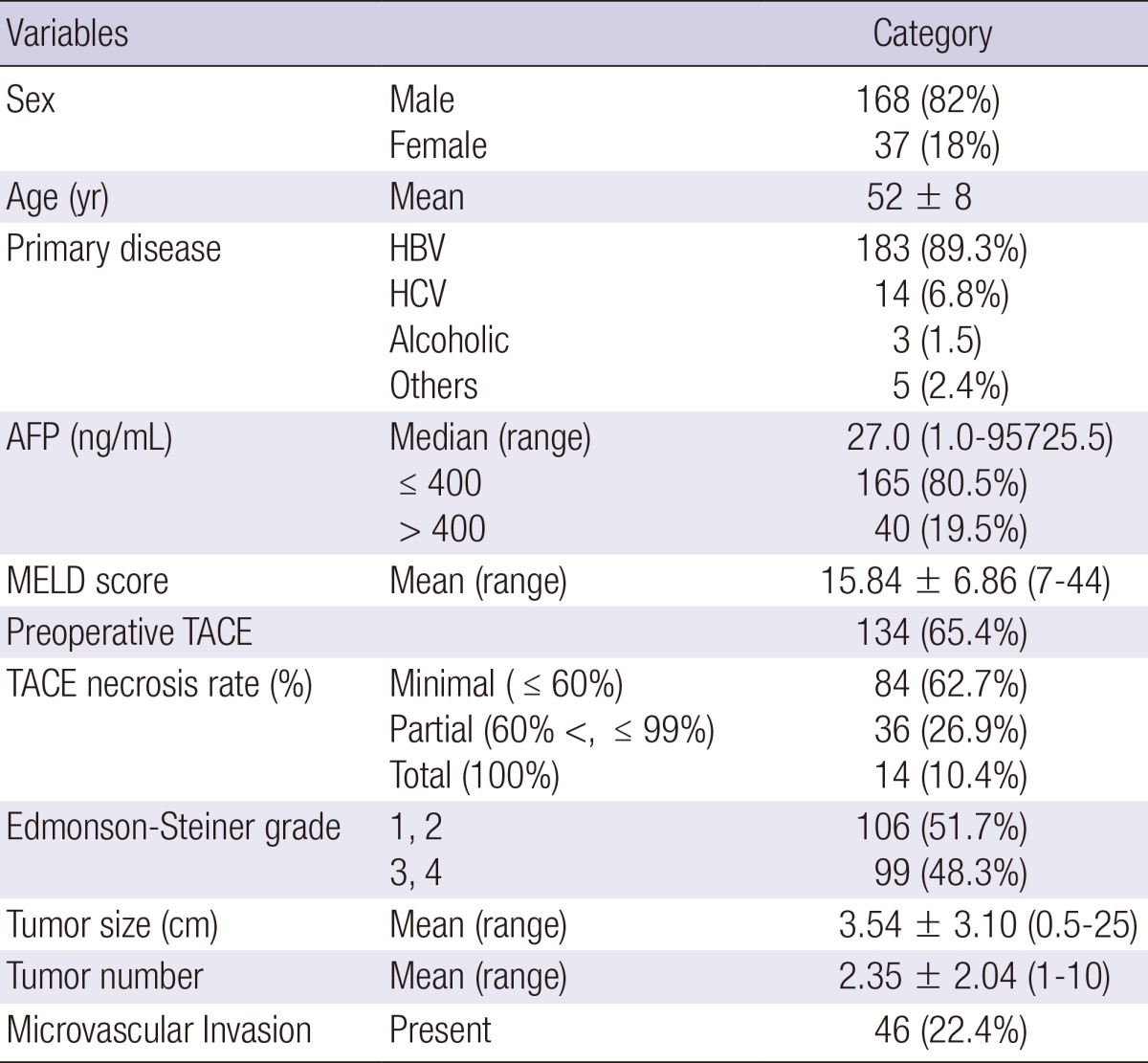
Risk factors for HCC recurrence
The data are presented in Table 2. Six risk factors for post-LT HCC recurrence were identified in multivariate analysis: preoperative AFP >400 ng/mL, Edmonson grade 3 or 4, tumor size >7 cm, tumor number≥7, minimal tumor necrosis in the TACE group and positive microvascular invasion.
Table 2.
Multivariate analysis for risk factors for post-LT HCC recurrence
AFP, alpha-fetoprotein; CI, confidence interval; HCC, hepatocellular carcinoma; LT, liver transplantation; TACE, transarterial chemoembolization.
Groups by risk index
Stratification of patients into the four groups was based on the risk index. It yielded 51 patients in group I, 109 patients in group II, 33 patients in group III and 12 patients in group IV.
Recurrence pattern according to the groups
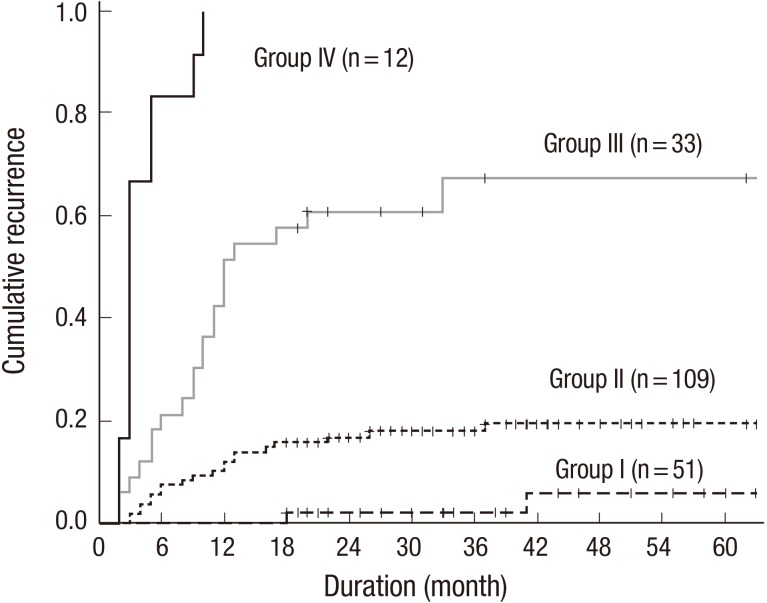
Fig. 2 depicts the data concerning the cumulative recurrence rate and timing of recurrence according to group. Significant differences were noted between groups. One-year cumulative recurrence rate of group I, II, III and IV were 0%, 11%, 51%, and 100%, respectively. Group I showed very low (n=2, 3.9%) and late recurrence after 18 months. Mean time to recurrence was 29 months (range, 18-41 months). In groups II and III, the mean time to recurrence was 11 and 10 months (range, 2-37 months) respectively. Most recurrences developed within the first 18 months in a temporally linear manner. Group IV showed an early recurrence pattern, within 6 months in most cases (mean time to recurrence, 4 months; range, 2-10 months).
Fig. 2.
Cumulative recurrence rates according to group based on the risk index. Group I shows very low and late recurrence after 18 months. In groups II and III, most recurrences develop within the first 18 months in a temporally linear manner. Group IV shows an early recurrence pattern within 6 months in most cases.
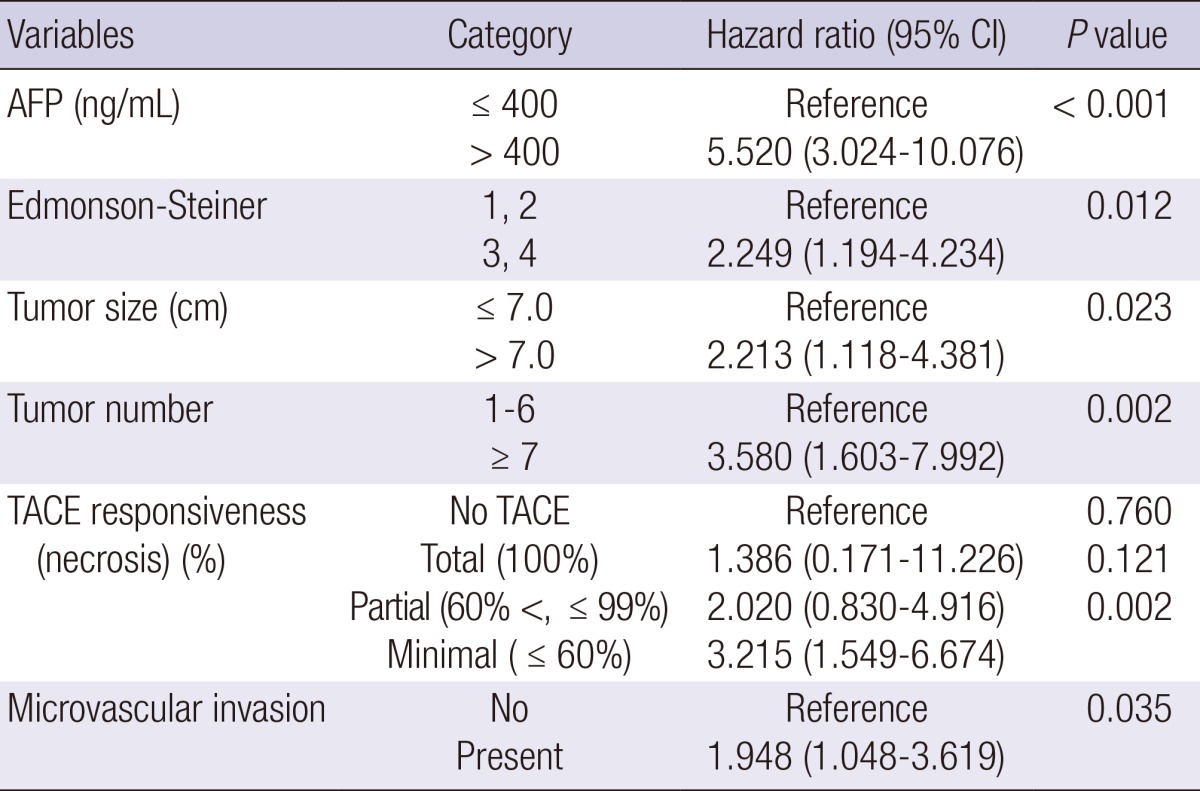
We analyzed the data concerning recurrence sites according to the groups. The findings were similar to those for recurrence pattern. Extrahepatic recurrence was more common than intrahepatic recurrence. Across the groups, extrahepatic recurrence was developed in 43.7% of patients, combined recurrence rates was 20%. However, the liver was most common single organ to show initial recurrence. Only intrahepatic recurrence was appeared initially in 35% of group II, 23.8% of group III and 66.7% of group IV. Two bony late recurrences were developed in group I. Combined or multi-organ recurrence was more than 25% in group II (25%) and III (25.8%) (Table 3).
Table 3.
Recurrecne sites according to groups
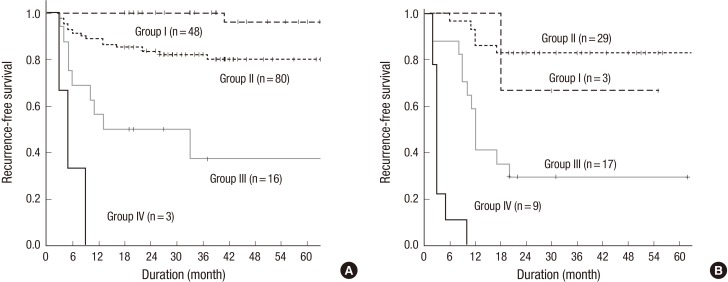
Comparison of the grouping system with UCSF criteria
To validate the presently developed grouping system, the patients were divided according to the UCSF criteria. One hundred forty seven patients (71.7%) met the UCSF criteria. For these patients, the 5-yr RFS of group I, II, III, and IV was 96%, 80%, 37.5%, and 0%, respectively. For patients who did not meet the UCSF criteria, the 5-yr RFS of group I, II, III, and IV were 66.7%, 82.8%, 29.4%, and 0%, respectively (Fig. 3).
Fig. 3.
Recurrence free survival rates according to UCSF criteria. (A) Recurrence free survival rates of patients who met UCSF criteria according to group. (B) Recurrence free survival rates of patients who were outside of UCSF criteria according to group.
Initial detection method for HCC recurrence
The data are summarized in Table 4. Elevated serum AFP was reason for suspicion of HCC recurrence in 60.0% of cases. HCC recurrence was detected during the follow-up radiologic examination in 16.4% of cases. An abnormal physical examination or symptom was the next most-prevalent reason for suspicion of HCC (23.6%). The elevation of serum AFP was the main reason for suspicion of HCC across the recurrence sites except for the bone. Half of the patients with a recurrence in bone initially complained of bone pain without an elevation of serum AFP.
Table 4.
Initial detection method according to recurrence sites
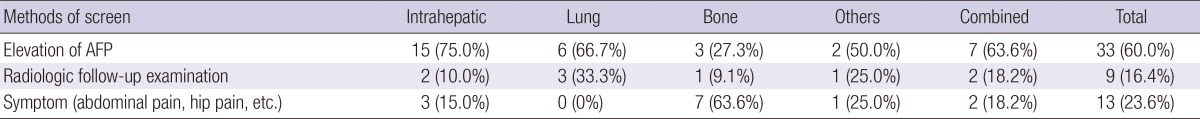
AFP, alpha-fetoprotein.
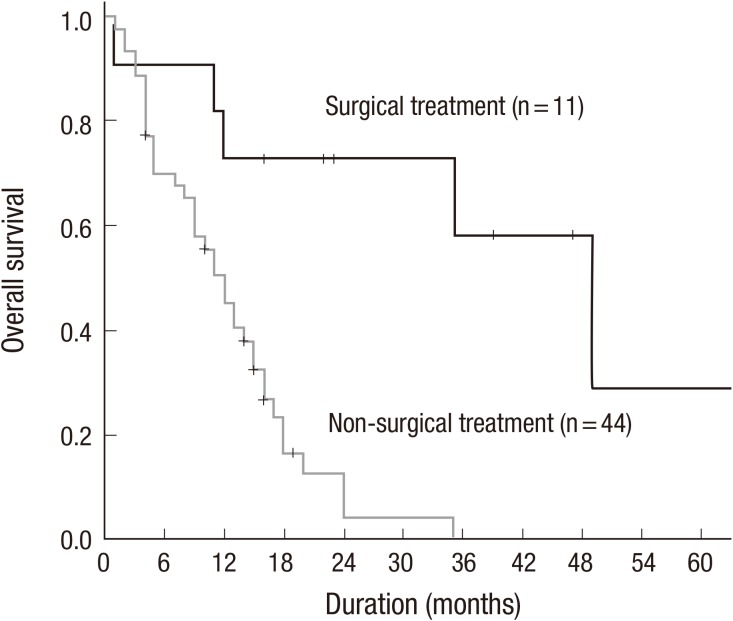
Survival from recurrence
The prognosis after recurrence according to the patient group was statistically different (P=0.031). However, there was no significant difference in prognosis according to recurrent sites. All recurrences in the graft liver were initially treated with TACE and pulmonary recurrences were treated with chemotherapy. Most bone recurrences were treated with radiotherapy and/or chemotherapy. The 2-yr survival rate after recurrence of group II and III was 31.9% and 16.2%, respectively. The mean survival time of group II and III after recurrence was 28 months and 16 months, respectively. Especially, nine patients in groups II and III underwent surgical treatments for recurrent lesions, including intra- and extra-hepatic mass resection, retransplantation for intrahepatic recurrence, wedge resection for pulmonary metastases and metastatectomy for bony metastasis. In this surgical resection group, the 2-yr survival rate after recurrence of group II and III was 80.0% and 75.0%, respectively. The mean survival time of group II and III after recurrence was 50 months and 38 months, respectively. Surgical treatment of recurrent HCC was also an independent predictor of long-term survival after tumor relapse in multivariate analysis (P<0.01; Fig. 4).
Fig. 4.
Surgical treatment significantly improves the overall survival after tumor recurrence.
DISCUSSION
Tumor recurrence is a significant cause of death in LT patients with HCC. Therefore, a postoperative screening tool that enables early optimal treatment for recurrence would be very beneficial. At present, there are several staging systems or criteria to predict recurrence after LT in patients with HCC. These staging systems or criteria are mainly used for selecting subgroups of patients that have favorable outcomes (1, 2, 7, 8). However, in this study, we focused on HCC recurrence after LT in terms of recurrence pattern and recurrence rate. To this end, we used all available information including postoperative pathological features as well as pre-operative factors to stratify the risk of recurrence and evaluate the pattern of recurrence, in an effort to develop an optimal screening tool for HCC recurrence after LT.
Presently, one preoperative factor (AFP > 400 ng/mL) and five pathologic factors (Edmonson grade 3 or 4, tumor size>7 cm, tumor number≥7, minimal tumor necrosis in TACE patients and positive microvascular invasion) were identified as independent risk factors for post-LT HCC recurrence. These factors have been reported as significant risk factors to reflect tumor biology and to predict recurrence after LT in previous studies. Golden selection criteria such as Milan and UCSF criteria are based on tumor number and size (1, 2). Some expanded criteria include AFP (6, 9). The significance of tumor histological grade was reported in another study (10). TNM staging and up-to-seven criteria stress the importance of microvascular invasion in predicting recurrence (11). The direct benefit of pre-LT TACE is controversial. Some previous studies have suggested a direct beneficial effect of TACE in patients waiting for LT (12, 13, 14). Presently, however, the TACE group showed an inferior outcome to the non-TACE group (data not shown). Instead, survival was stratified by TACE responsiveness, which seemed to reflect tumor biology. The overall RFS of the total necrosis group was significantly higher than that of the minimal necrosis group (P=0.029) and minimal tumor necrosis in the TACE group was a significant risk factor for HCC recurrence after LT (P=0.002). The combination of these well known risk factors used in this study differentiated the risk of HCC recurrence better than any other criteria or staging system. By applying the risk index from these risk factors, we could stratify patients into four clinically and statistically important groups to predict post-LT HCC recurrence.
There were significant differences in RFS between sequential risk groups across the UCSF criteria. Some groups who met UCSF criteria developed HCC recurrence commonly and some groups who were outside UCSF criteria had favorable outcomes. The RFS of groups III and IV was less than 40% at 5 yr, even within the UCSF criteria group, and the RFS of group II exceeded 80% at 5 yr, despite not meeting USCF criteria.
The cumulative recurrence rate was significantly different by the groups. One-year cumulative recurrence rates of group I, II, III and IV were 0%, 11%, 51%, and 100%, respectively. The more interesting finding in this study was that the recurrence pattern as well as recurrence rate was stratified by risk index. Group I showed late recurrence (i.e., after 18 months). Groups II and III showed an intermediate recurrence pattern with a linear increase within 18 months. Group IV showed an early recurrence pattern (within 6 months).
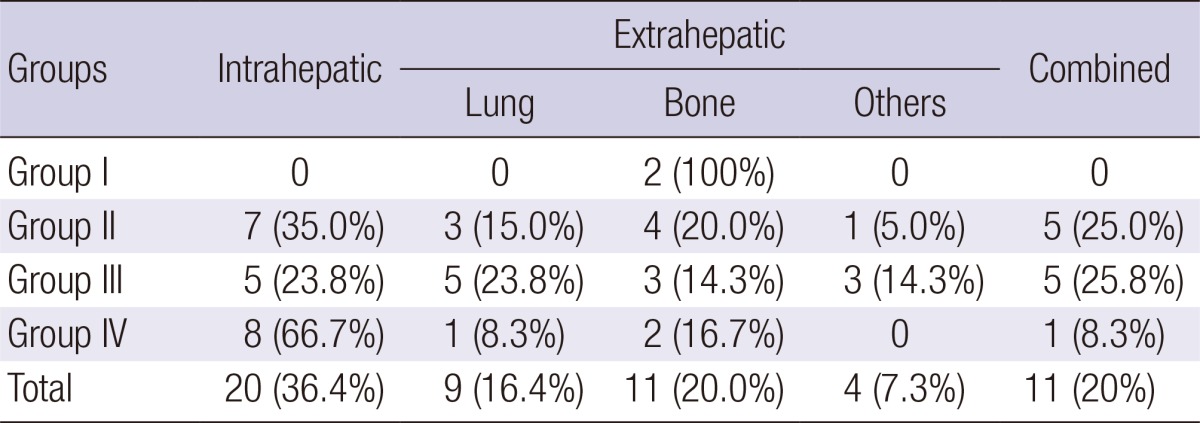
Based on the difference of recurrence rate and time to recurrence, we suggest a tailored screening interval which can be used to establish cost-effective post-LT screening (Table 5). In group I (i.e., very low risk patients), strict surveillance is seemingly not necessary, since, presently, only two recurrences developed after 18 months. Therefore, HCC screening could be safely done at every 6-12 months until 18 months and annually later. In groups II and III, almost 90% of recurrence occurred within 18 months, with a 3-month linear increase 2% (group II) and 9% (group III) during this period. Therefore, a strict surveillance every 3-6 months in group II and every 3 months in group III is needed within 18 months. After 18 months, screening every 6 months may be sufficient. Group IV patients displayed very poor outcome, with most recurrence developing within 6 months. For such patients, screening every 2-3 months for the first 18 months is prudent. Furthermore, no conclusion regarding the benefit of screening after 18 months in group IV patients is possible, since there were no survivors after 18 months in this group in our patient cohort. We suggest that group I-III patients follow generally accepted protocol after 48 months. The benefit of LDLT for patients with advanced HCC exceeding Milan criteria remains relatively small, and in group IV it is uncertain whether any benefit exist at all. Rather than screening, exclusion before LT or adjuvant preventive strategy may be better alternatives in this group.
Table 5.
Suggested tailored screening protocol for post-LT HCC recurrence
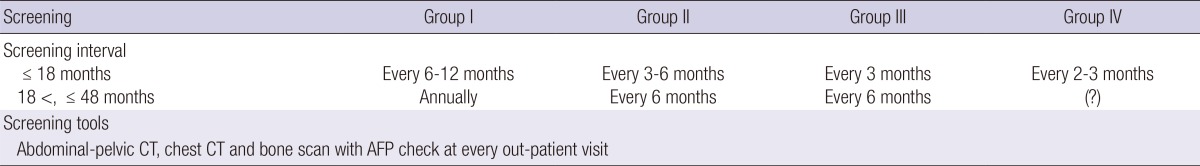
AFP, alpha-fetoprotein; CT, computed tomography.
The most common pattern of HCC recurrence after partial hepatectomy is solitary intrahepatic recurrence (15, 16). However, extrahepatic recurrence can be more frequent than intrahepatic or combined recurrence in the setting of LT (17). In our study, across the groups, extrahepatic recurrence developed in over 40% of patients, most commonly in the bone (45.8%) and lungs (37.5%), with a combined recurrence rate of 20%. Therefore, an optimal tool to detect extrahepatic HCC recurrence should be included in a follow-up protocol. AFP is inexpensive to perform and is an important follow-up tool for detection of HCC recurrence. Increased AFP level was most common reason (60%) for detection in this study because routine imaging work-ups were not often performed. However, one study conducted using a strictly regular imaging follow-up protocol reported that the elevation of AFP without any symptoms and radiologic abnormality was reason for suspicion of HCC recurrence in only 30% of cases (18). Furthermore, in our study, 32.7% of patients showed a normal range of AFP level at the time of recurrence. Abnormal symptoms or radiologic abnormality upon follow-up examination were the reasons for suspicion of HCC recurrence in 40% of cases in the present study. Especially, in half of the patients who developed recurrence in the bone, recurrence was typically due initially to bone pain in the absence of elevated serum AFP. Therefore, AFP appears to be insufficient to screen for HCC recurrence after LT. 18F-FDG PET/CT was more sensitive to detect bone or lymph node metastasis than bone scan or CT. However, 18F-FDG PET/CT is not suitable as a screening tool after LT, because of its limitations for small lesions, intrahepatic lesions and brain lesions (18). Therefore, CT scans of the chest and abdomen and bone scan, as well as AFP, seem to be the most reasonable screening tool in all groups.
An important issue that arises out of the present study is whether the early detection of HCC recurrence by an aggressive screening protocol can indeed produce a better outcome. Surgical treatment of recurrent lesions has been associated with a better outcome (4, 5, 19). Analysis of the present cohort revealed that surgical treatment of recurrent HCC was also an independent predictor of long-term survival after tumor relapse in multivariate analysis. Furthermore, Ladabaum et al. (20) demonstrated that the cost-effectiveness of screening is greatly dependent on the survival benefit of surgical resection for recurrent disease. Therefore, optimal screening to detect resectable lesions earlier seems to be beneficial to increase survival in some patients. An analysis of the pattern of recurrence in a patient cohort supports the establishment of optimal screening protocol in terms of screening interval and screening tools. The screening interval needs to differ by risk of recurrence. Screening should include work-up for extra-hepatic recurrence as well as intra-hepatic recurrence, regardless of risk of recurrence. However, because the study design was a retrospective review for the small number of patients, further validation is required.
ACKNOWLEDGMENT
We thank Dr. W. Ray Kim (Mayo Clinic, Rochester, Minnesota) for helpful comments regarding the manuscript.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, Montalto F, Ammatuna M, Morabito A, Gennari L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693–699. doi: 10.1056/NEJM199603143341104. [DOI] [PubMed] [Google Scholar]
- 2.Yao FY, Ferrell L, Bass NM, Watson JJ, Bacchetti P, Venook A, Ascher NL, Roberts JP. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology. 2001;33:1394–1403. doi: 10.1053/jhep.2001.24563. [DOI] [PubMed] [Google Scholar]
- 3.Park MS, Lee KW, Suh SW, You T, Choi Y, Kim H, Hong G, Yi NJ, Kwon CH, Joh JW, et al. Living-donor liver transplantation associated with higher incidence of hepatocellular carcinoma recurrence than deceased-donor liver transplantation. Transplantation. 2014;97:71–77. doi: 10.1097/TP.0b013e3182a68953. [DOI] [PubMed] [Google Scholar]
- 4.Roayaie S, Schwartz JD, Sung MW, Emre SH, Miller CM, Gondolesi GE, Krieger NR, Schwartz ME. Recurrence of hepatocellular carcinoma after liver transplant: patterns and prognosis. Liver Transpl. 2004;10:534–540. doi: 10.1002/lt.20128. [DOI] [PubMed] [Google Scholar]
- 5.Shin WY, Suh KS, Lee HW, Kim J, Kim T, Yi NJ, Lee KU. Prognostic factors affecting survival after recurrence in adult living donor liver transplantation for hepatocellular carcinoma. Liver Transpl. 2010;16:678–684. doi: 10.1002/lt.22047. [DOI] [PubMed] [Google Scholar]
- 6.Yang SH, Suh KS, Lee HW, Cho EH, Cho JY, Cho YB, Kim IH, Yi NJ, Lee KU. A revised scoring system utilizing serum alphafetoprotein levels to expand candidates for living donor transplantation in hepatocellular carcinoma. Surgery. 2007;141:598–609. doi: 10.1016/j.surg.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 7.Soejima Y, Taketomi A, Yoshizumi T, Uchiyama H, Aishima S, Terashi T, Shimada M, Maehara Y. Extended indication for living donor liver transplantation in patients with hepatocellular carcinoma. Transplantation. 2007;83:893–899. doi: 10.1097/01.tp.0000259015.46798.ec. [DOI] [PubMed] [Google Scholar]
- 8.Lee SG, Hwang S, Moon DB, Ahn CS, Kim KH, Sung KB, Ko GY, Park KM, Ha TY, Song GW. Expanded indication criteria of living donor liver transplantation for hepatocellular carcinoma at one large-volume center. Liver Transpl. 2008;14:935–945. doi: 10.1002/lt.21445. [DOI] [PubMed] [Google Scholar]
- 9.Zheng SS, Xu X, Wu J, Chen J, Wang WL, Zhang M, Liang TB, Wu LM. Liver transplantation for hepatocellular carcinoma: Hangzhou experiences. Transplantation. 2008;85:1726–1732. doi: 10.1097/TP.0b013e31816b67e4. [DOI] [PubMed] [Google Scholar]
- 10.Cillo U, Navaglia F, Vitale A, Molari A, Basso D, Bassanello M, Brolese A, Zanus G, Montin U, D'Amico F, et al. Clinical significance of alpha-fetoprotein mRNA in blood of patients with hepatocellular carcinoma. Clin Chim Acta. 2004;347:129–138. doi: 10.1016/j.cccn.2004.04.032. [DOI] [PubMed] [Google Scholar]
- 11.Mazzaferro V, Llovet JM, Miceli R, Bhoori S, Schiavo M, Mariani L, Camerini T, Roayaie S, Schwartz ME, Grazi GL, et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol. 2009;10:35–43. doi: 10.1016/S1470-2045(08)70284-5. [DOI] [PubMed] [Google Scholar]
- 12.Graziadei IW, Sandmueller H, Waldenberger P, Koenigsrainer A, Nachbaur K, Jaschke W, Margreiter R, Vogel W. Chemoembolization followed by liver transplantation for hepatocellular carcinoma impedes tumor progression while on the waiting list and leads to excellent outcome. Liver Transpl. 2003;9:557–563. doi: 10.1053/jlts.2003.50106. [DOI] [PubMed] [Google Scholar]
- 13.Roayaie S, Frischer JS, Emre SH, Fishbein TM, Sheiner PA, Sung M, Miller CM, Schwartz ME. Long-term results with multimodal adjuvant therapy and liver transplantation for the treatment of hepatocellular carcinomas larger than 5 centimeters. Ann Surg. 2002;235:533–539. doi: 10.1097/00000658-200204000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Majno PE, Adam R, Bismuth H, Castaing D, Ariche A, Krissat J, Perrin H, Azoulay D. Influence of preoperative transarterial lipiodol chemoembolization on resection and transplantation for hepatocellular carcinoma in patients with cirrhosis. Ann Surg. 1997;226:688–701. doi: 10.1097/00000658-199712000-00006. discussion-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Poon RT, Fan ST, Lo CM, Liu CL, Wong J. Long-term survival and pattern of recurrence after resection of small hepatocellular carcinoma in patients with preserved liver function: implications for a strategy of salvage transplantation. Ann Surg. 2002;235:373–382. doi: 10.1097/00000658-200203000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kamiyama T, Nakanishi K, Yokoo H, Kamachi H, Tahara M, Suzuki T, Shimamura T, Furukawa H, Matsushita M, Todo S. Recurrence patterns after hepatectomy of hepatocellular carcinoma: implication of Milan criteria utilization. Ann Surg Oncol. 2009;16:1560–1571. doi: 10.1245/s10434-009-0407-7. [DOI] [PubMed] [Google Scholar]
- 17.Lee KK, Kim DG, Moon IS, Lee MD, Park JH. Liver transplantation versus liver resection for the treatment of hepatocellular carcinoma. J Surg Oncol. 2010;101:47–53. doi: 10.1002/jso.21415. [DOI] [PubMed] [Google Scholar]
- 18.Kim YK, Lee KW, Cho SY, Han SS, Kim SH, Kim SK, Park SJ. Usefulness 18F-FDG positron emission tomography/computed tomography for detecting recurrence of hepatocellular carcinoma in posttransplant patients. Liver Transpl. 2010;16:767–772. doi: 10.1002/lt.22069. [DOI] [PubMed] [Google Scholar]
- 19.Schlitt HJ, Neipp M, Weimann A, Oldhafer KJ, Schmoll E, Boeker K, Nashan B, Kubicka S, Maschek H, Tusch G, et al. Recurrence patterns of hepatocellular and fibrolamellar carcinoma after liver transplantation. J Clin Oncol. 1999;17:324–331. doi: 10.1200/JCO.1999.17.1.324. [DOI] [PubMed] [Google Scholar]
- 20.Ladabaum U, Cheng SL, Yao FY, Roberts JP. Cost-effectiveness of screening for recurrent hepatocellular carcinoma after liver transplantation. Clin Transplant. 2011;25:283–291. doi: 10.1111/j.1399-0012.2010.01212.x. [DOI] [PubMed] [Google Scholar]