Abstract
Endoscopic hemostasis is the first-line treatment for upper gastrointestinal bleeding (UGIB). Although several factors are known to be risk factors for rebleeding, little is known about the use of antithrombotics. We tried to verify whether the use of antithrombotics affects rebleeding rate after a successful endoscopic hemostasis for peptic ulcer disease (PUD). UGIB patients who underwent successful endoscopic hemostasis were included. Rebleeding was diagnosed when the previously treated lesion bled again within 30 days of the initial episode. Of 522 UGIB patients with PUD, rebleeding occurred in 93 patients (17.8%). The rate of rebleeding was higher with aspirin medication (P=0.006) and after a long endoscopic hemostasis (P<0.001). Of all significant variables, procedure time longer than 13.5 min was related to the rate of rebleeding (OR, 2.899; 95% CI, 1.768-4.754; P<0.001) on the logistic regression analysis. The rate of rebleeding after endoscopic hemostasis for PUD is higher in the patients after a long endoscopic hemostasis. Endoscopic hemostasis longer than 13.5 min is related to rebleeding after a successful endoscopic hemostasis for PUD.
Keywords: Hemostasis, Endoscopic, Peptic Ulcer, Rebleeding, Upper Gastrointestinal Bleeding
INTRODUCTION
Upper gastrointestinal bleeding (UGIB) remains one of the more common emergencies, despite recent advances in endoscopic techniques. The first-line therapy for UGIB is endoscopic hemostasis. However, even if this treatment is successful, subsequent rebleeding is not a rare event. Studies carried out to determine the predictors of rebleeding in patients with nonvariceal UGIB have revealed the following influential factors such as persistence of endoscopic stigmata, a large ulcer, failure to use a proton pump inhibitor (PPI) after the hemostasis, epinephrine monotherapy, postprocedure use of heparin, and liver cirrhosis (1, 2, 3). In addition, a recent Korean study found that the significant risk factors were a lower hemoglobin level (≤9 g/dL), a relatively inexperienced therapeutic endoscopist (i.e., a career of <2 yr), injection of large volumes of epinephrine (>15 mL), epinephrine monotherapy, and comorbidities such as chronic renal disease or liver cirrhosis (4). However, some lesions rebleed despite the absence of any of these above factors.
While little is known about the effect of antithrombotics on the rate of rebleeding, the worldwide increase in the elderly population means that their use has become an important issue in gastrointestinal (GI) endoscopy. A Japanese study has shown that GI bleeding occurs more frequently in Japanese patients who take aspirin, ticlopidine, and/or warfarin than in those without these antithrombotics (5). That study found that the bleeding occurred in the esophagus or stomach, but not in the lower GI tract. Aspirin is known to irreversibly inhibit the action of cyclooxygenase-1, suppress both tissue prostaglandin synthesis and platelet production of thromboxane A2, and increase the risk of bleeding (6). In addition, warfarin increases the rate of major extracranial hemorrhage, especially when there is a history of GI bleeding, concurrent use of antiplatelet or nonsteroidal anti-inflammatory drugs, genetically different warfarin metabolism, a high international normalized ratio (INR), comorbid illnesses, or a long duration of medication (7). The aim of this study was to determine the risk factors for rebleeding after successful endoscopic hemostasis therapy for peptic ulcer disease (PUD) relative to the use of antithrombotics.
MATERIALS AND METHODS
Patients
UGIB patients due to PUD who underwent successful endoscopic hemostasis between August 2005 and September 2012 at our center were included in this study. Exclusion criteria were the failure of endoscopic hemostasis, cause of bleeding other than PUD, uncertain endoscopic findings, patients under 18 yr-old, or lack of the follow-up data. Bleedings from malignancy were also excluded. The data were collected on the patient's past medical history and types of medication at the time of UGIB. All of the patients provided written informed consent prior to undergoing the procedure, and were followed up for more than 30 days after the hemostasis.
Upper gastrointestinal endoscopic procedure
Endoscopic procedures were performed by 10 GI faculties (staffs more than 3 yr of career on therapeutic endoscopy) and trainees (GI fellows) using endoscope (GIF-H260; Olympus, Tokyo, Japan) at our center. Endoscopic procedures performed between 8:30 am and 6:00 pm from Monday to Friday were defined as a routine procedure. Others were classified as an emergency procedure.
Types of endoscopic hemostasis
The method of endoscopic hemostasis was solely decided by the attending GI endoscopist according to one's own preference. The types of endoscopic hemostasis of our center consist of epinephrine injection, electrocauterization, hemoclipping, and others (histoacryl injection, endoscopic band ligation, etc.). Epinephrine injection was performed using 0.9% NaCl (9 mL) and 1:1,000 epinephrine (1 mL) mixtures. Electrocauterization was performing using a coagrasper (Olympus, CD-120 U, Tokyo, Japan) under the power of 80W intensity. Clipping was performed using a hemoclip (135-degree angle, Hx-610-135; Olympus Optical Co., Ltd., Tokyo, Japan). After the procedure, intravenous PPI (pantoprazole) were administered continuously for 72 hr as recommended by the guideline (8). Patients were hospitalized for at least 72 hr after the endoscopic hemostasis, and were discharged with oral PPI medication. PPIs were continued at least 4-8 weeks with the cessation of antithrombotics.
Rebleeding after endoscopic hemostasis
Second look endoscopy was carried out when there was a suspicious sign of rebleeding such as hematemesis, melena, or a reduction in hemoglobin level by more than 2.0 g/dL per day. Rebleeding was diagnosed when the lesion bled again within 30 days of the initial endoscopic hemostasis. In cases of rebleeding, endoscopic hemostasis was performed according to the preference of the attending endoscopist. The types of endoscopic hemostasis for rebleeding were similar to those of the initial methods such as epinephrine injection, electrocauterization, hemoclipping, and others (histoacryl injection, endoscopic band ligation, etc.).
Statistical analysis
Patients with and without rebleeding were compared with respect to demographic, clinical, and endoscopic variables using the chi-square test for categorical variables and t-test for continuous variables. When the data were not normally distributed or when the sample size was small, the Mann-Whitney U-test or Fisher's exact test was used instead of t-test or chi-square test. Median value with ranges was shown using the Mann-Whitney test for two groups. The rate of rebleeding was assessed by case-control analysis. A receiver operating characteristic (ROC) curve was constructed by plotting sensitivity (true-positive rate) against 1-specificity (false-positive rate) over all possible threshold levels of procedure time which is related to rebleeding. Logistic regression analysis was performed to verify the significance of allergic disease according to rebleeding using odds ratio (OR) and 95% of CI (confidence interval). A P-value of less than 0.05 was considered statistically significant.
Ethics statement
The study was approved by institutional review board (IRB) of Konkuk University School of Medicine which confirmed that the study was in accordance with the ethical guidelines of the Helsinki Declaration (KUH1010448). After the IRB approval, this study was registered as ClinicalTrials.gov ID: KCT0000640 (https://cris.nih.go.kr/cris).
RESULTS
Characteristics of the patients with respect to the presence of rebleeding
Of the 522 UGIB patients due to PUD who fulfilled the inclusion criteria, 122 patients (23.4%) were taking antithrombotics. Rebleeding occurred in 93 (17.8%) of the 522 patients. Proportions of underlying diseases did not differ between the patients with and without rebleeding (Table 1).
Table 1.
Basal characteristics of the patients according to the presence of rebleeding
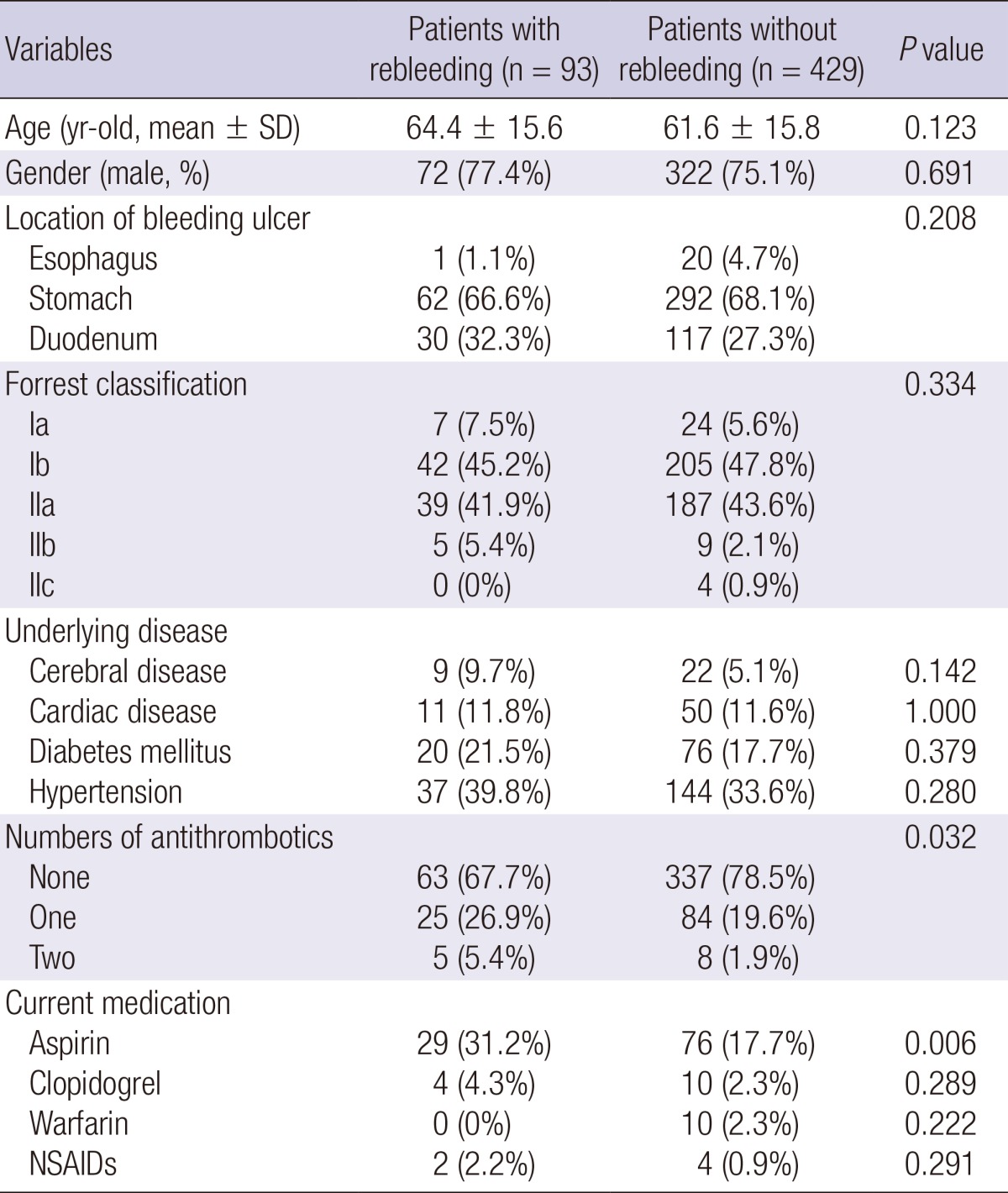
SD, standard deviation; NSAID, non-steroidal anti-inflammatory drug.
Of the 30 patients on antithrombotics who experienced rebleeding, only a 73 yr-old male was taking clopidogrel alone without aspirin. The other 29 patients (96.7%) were taking aspirin including 4 patients with a combination of aspirin and clopidogrel. All of the aspirin-taking patients were taking 100 mg a day. According to the Mann-Whitney test, there was no difference in the onset of rebleeding after the initial endoscopic hemostasis between the patients who taking aspirin at the time of UGIB (median of 3.5 days ranging from 1-18 days) and patients without aspirin (median of 2.5 days ranging from 1-26 days, P=0.209).
In 19 of these 30 patients (63.3%), hematemesis was main symptom of the rebleeding. Melena was main symptom of the rebleeding in other 10 patients, whereas one patient showed decreased hemoglobin level more than 2.0 g/dL per day. All except one of the subjects required transfusion of red blood cells (RBCs). The exception was a 72 yr-old patient with a current history of ischemic heart disease whose hemoglobin level was stable (13.2 g/dL). Since he showed a sudden reduction in hemoglobin level from 17.5 to 13.2 g/dL within 24 hr, RBC was transfused to prevent any perfusion defect on the recently damaged cardiac muscles.
Link between the use of antithrombotics and rebleeding
The most commonly used antithrombotic medication was aspirin in both groups. Of the 93 patients who experienced rebleeding, 25 were taking one antithrombotic and five were taking two different antithrombotics at the time of the initial UGIB. Of the 429 patients who did not experience rebleeding after the initial endoscopic hemostasis, 84 were taking one antithrombotic and 11 were taking two antithrombotics. The proportion of patients taking antithrombotics was higher among those with rebleeding (P=0.032). Among the antithrombotics being used, the rate of rebleeding was higher among the patients taking aspirin medication (P=0.006).
Rate of rebleeding relative to the endoscopic procedure
There was no significant difference between the patients with and without rebleeding with regard to the method of endoscopic hemostasis, emergency endoscopy, and the amount of experience of the attending endoscopist (Table 2). The procedure time was significantly longer in those with rebleeding than in those without rebleeding (P<0.001).
Table 2.
Link between rebleeding and the type of endoscopic hemostasis
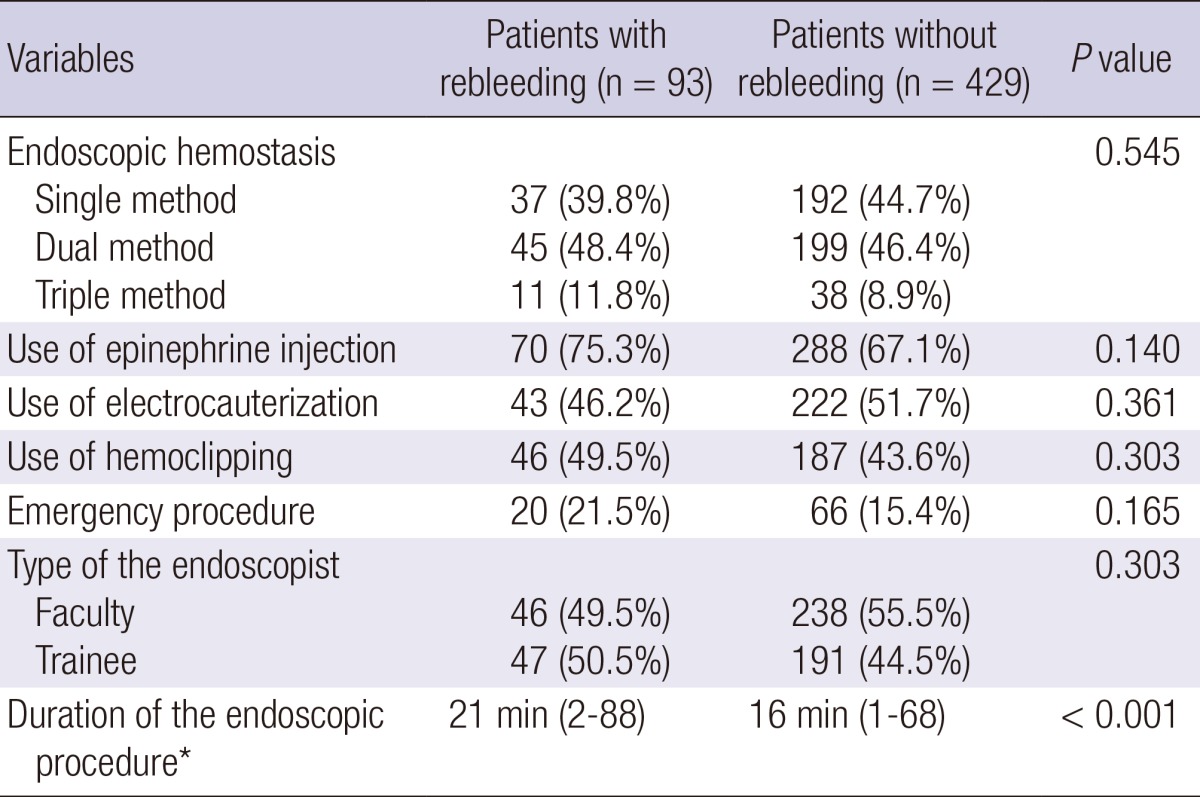
*Median with ranges was shown using the Mann-Whitney test since the data were not normally distributed.
The optimal cut-off value with regard to the duration of endoscopic hemostasis was 13.5 min with area under the ROC curve of 0.644 (P<0.001). Of all significant variables, procedure time longer than 13.5 min was significantly related to rebleeding (OR, 2.899; 95% CI, 1.768-4.754; P<0.001) on the logistic regression analysis (Table 3).
Table 3.
Significant variables related to rebleeding
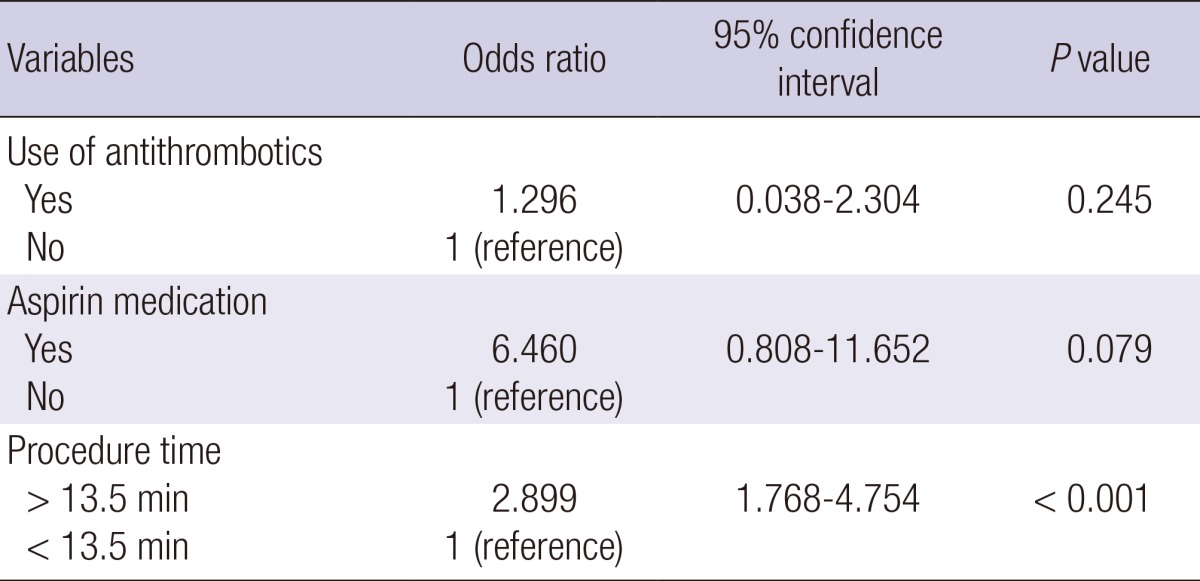
Data were analyzed by logistic regression analysis.
Rate of rebleeding according to the endoscopist
There was no significant difference in the rate of rebleeding (P=0.574) among the patients of different GI endoscopists. The duration of endoscopic hemostasis was significantly higher when performed by trainee (P<0.001). Median procedure time of trainee was 17.1 min (2-88 min), while that of experienced endoscopist was 11.3 min (1-60 min). The type of organ differed significantly between the endoscopists (P<0.001), because some of them were major in pancreaticobiliary diseases and some received calls from intensive care units.
The preferences with regard to the use of epinephrine injection (P<0.001) and electrocauterization (P<0.001) differed significantly among the GI endoscopists, resulting in different proportion of single or combination therapies (P<0.001) and in the duration of the endoscopic hemostasis procedure (P<0.001). Although it was not statistically significant, one endoscopist who had a low preference for electrocauterization (22.2%) showed the highest rebleeding rate (27.8%) among all endoscopists. The other endoscopist who preferred single method (75.7%) without epinephrine injection showed shortest duration of procedure (7 min).
DISCUSSION
The rate of rebleeding after endoscopic hemostasis for UGIB is higher in the patients after a long endoscopic hemostasis in this study. Notably, the rate of rebleeding did not differ significantly between the GI endoscopists who performed the hemostasis, while it did differ with use of epinephrine injection and electrocauterization leading to a significant difference in the duration of the endoscopic hemostasis procedure.
Interesting finding of the present study is that the duration of endoscopic hemostasis was significantly related to the rate of rebleeding. It may be that the duration of endoscopic hemostasis can be influenced by the nature of the bleeding lesion, leading to a difficult procedure. In addition, most of the endoscopists in the present study had a preferred hemostatic method, regardless of the patient's condition, and the site, location, and characteristics of the bleeding lesion. The preferences for the use epinephrine injection and electrocauterization were significantly different among GI endoscopists, although there was no significant difference in the rate of rebleeding. This can be explained by our previous study showing that the preference for a specific method depends more on the personal experience and prior mentoring of the clinician than on the published guidelines (9).
Of the antithrombotics being used by the patients in the present study, aspirin was the most frequently prescribed drugs, and as such, most GI endoscopists are aware of its impact on GI bleeding. We previously showed that Eastern endoscopists do not typically perform endoscopic biopsy procedures while patients are receiving warfarin, and do not perform polypectomies on patients who are currently taking aspirin due to the risk of bleeding (10). In that study, we found that Eastern endoscopists tend to believe that aspirin increases the risk of bleeding in Asians than the Caucasians. This is consistent with Japanese studies showing that the incident rates of gastroduodenal mucosal injury and bleeding are significantly higher among Asians who are taking antiplatelet medication (5, 11).
A recent Korean study showed that warfarin increases the frequencies of both rebleeding and thromboembolic events (12). Our study is consistent with a previous study showed that mild to moderate anticoagulation medication does not increase the rate of rebleeding following endoscopic therapy for nonvariceal UGIB (13). In that study, the INR was not a predictor of rebleeding for UGIB, the need for RBC transfusion, requirement for surgery, length of hospitalization, or death. On the other hand, in the present study it was not possible to determine why the patients taking clopidogrel did not show a higher rate of rebleeding. Although it is well known that combination medication with aspirin and a PPI is superior for preventing rebleeding than clopidogrel alone (14), it remains to be established whether monotherapy with clopidogrel can induce more severe drug-induced ulcers that might lead to frequent UGIB.
The most up-to-date safety and efficacy data have to led to the current recommendation for hemostasis in UGIB of mechanical or ablation therapy, with or without epinephrine injection (15). More recently, monotherapy using either mechanical or ablation therapy has replaced the combination method, as shown in the present study. Monotherapy was used in 77.9% of cases in a recent study, whereas combination therapy was used for only 21.5% with a heat probe being the most commonly used device for endoscopic hemostasis (16). Yet another study revealed a changing trend in the favored endoscopic hemostasis procedure between the periods 1995-2000 and 2006-2009 (17), such that while injection and intravenous H2 blocker were predominantly used during the former period, hemoclipping and intravenous PPI were the preferred procedures during the latter. The greater number of cases of severe GI bleeding in the 2006-2009 resulted in the outcome of endoscopic hemostasis not differing between two times periods despite the intervening advances in medical procedure.
There are several limitations in our study including the lack of details on ulcer characteristics and various types of oral PPI medication used after the discharge. Since this study was based on the medical chart review, exact size of the bleeding ulcer or exact body mass index were missing. However, we assume that these factors would not have affected the result of our study, since even the Forrest classification did not differ between two groups. Recent studies have shown that the amount of bleeding is related to the rate of rebleeding (18, 19). It has been demonstrated that the initial presentation of either hematemesis or fresh red blood through a nasogastric tube are high risk factors for rebleeding (18), and that RBC transfusion is significantly related to subsequent rebleeding in nonvariceal UGIB patients (19). Most of the patients on antithrombotics who experienced rebleeding in the present study required RBC transfusion, and in most patients, the initial manifestations included hematemesis. Together these results suggest that these factors should be considered significant for predicting rebleeding, especially in patients after a long endoscopic hemostasis procedure.
In conclusion, a long endoscopic procedure time influence the occurrence of rebleeding after successful endoscopic hemostasis for UGIB. Procedure time longer than 13.5 min should be considered more carefully in terms of rebleeding than other disease-related factors or GI endoscopist-related factors. Careful monitoring is required after the long hemostasis procedure for PUD.
Footnotes
This work was supported by the National Research Foundation of Korea funded by the Korean Government (NRF 2012K2A2A4010622).
The authors declare that there is nothing to disclose except the acknowledgment that the study was supported by the National Research Foundation of Korea.
References
- 1.Seo YS, Kim YH, Ahn SH, Yu SK, Baik SK, Choi SK, Heo J, Hahn T, Yoo TW, Cho SH, et al. Clinical features and treatment outcomes of upper gastrointestinal bleeding in patients with cirrhosis. J Korean Med Sci. 2008;23:635–643. doi: 10.3346/jkms.2008.23.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chiu PW, Joeng HK, Choi CL, Kwong KH, Ng EK, Lam SH. Predictors of peptic ulcer rebleeding after scheduled second endoscopy: clinical or endoscopic factors? Endoscopy. 2006;38:726–729. doi: 10.1055/s-2006-925179. [DOI] [PubMed] [Google Scholar]
- 3.Travis AC, Wasan SK, Saltzman JR. Model to predict rebleeding following endoscopic therapy for non-variceal upper gastrointestinal hemorrhage. J Gastroenterol Hepatol. 2008;23:1505–1510. doi: 10.1111/j.1440-1746.2008.05594.x. [DOI] [PubMed] [Google Scholar]
- 4.Suk KT, Kim HS, Lee CS, Lee IY, Kim MY, Kim JW, Baik SK, Kwon SO, Lee DK, Ham YL. Clinical outcomes and risk factors of rebleeding following endoscopic therapy for nonvariceal upper gastrointestinal hemorrhage. Clin Endosc. 2011;44:93–100. doi: 10.5946/ce.2011.44.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suehiro T, Yakeishi Y, Sakai F, Matsuzaki K, Sanefuji K, Toyokawa T, Shioshita K, Sugie Y, Okudaira Y, Kano T, et al. Gastrointestinal bleeding associated with antithrombotic therapy in the elderly in Japan. Hepatogastroenterology. 2012;59:774–777. doi: 10.5754/hge09285. [DOI] [PubMed] [Google Scholar]
- 6.Sostres C, Lanas A. Gastrointestinal effects of aspirin. Nat Rev Gastroenterol Hepatol. 2011;8:385–394. doi: 10.1038/nrgastro.2011.97. [DOI] [PubMed] [Google Scholar]
- 7.Hylek EM. Complications of oral anticoagulant therapy: bleeding and nonbleeding, rates and risk factors. Semin Vasc Med. 2003;3:271–278. doi: 10.1055/s-2003-44463. [DOI] [PubMed] [Google Scholar]
- 8.Chung IK, Lee DH, Kim HU, Sung IK, Kim JH Korean College of Helicobacter and Upper Gastrointestinal Research; Korean Association of Gastroenterology. Guidelines of treatment for bleeding peptic ulcer disease. Korean J Gastroenterol. 2009;54:298–308. doi: 10.4166/kjg.2009.54.5.298. [DOI] [PubMed] [Google Scholar]
- 9.Tang SJ, Lee SY, Hynan LS, Yan J, Riley FC, Armstrong L, Rodriguez-Frias E, Xu L, Pruna E, Lara LF, et al. Endoscopic hemostasis in nonvariceal upper gastrointestinal bleeding: comparison of physician practice in the East and the West. Dig Dis Sci. 2009;54:2418–2426. doi: 10.1007/s10620-008-0689-9. [DOI] [PubMed] [Google Scholar]
- 10.Lee SY, Tang SJ, Rockey DC, Weinstein D, Lara L, Sreenarasimhaiah J, Choi KW Korean Association for the Study of Intestinal Disease. Managing anticoagulation and antiplatelet medications in GI endoscopy: a survey comparing the East and the West. Gastrointest Endosc. 2008;67:1076–1081. doi: 10.1016/j.gie.2007.11.037. [DOI] [PubMed] [Google Scholar]
- 11.Yamamoto T, Sanaka M, Nagasawa K, Abe K, Fukami M, Nakayama S, Tsuchiya A, Ishii T, Kuyama Y. Gastroduodenal mucosal injury in patients on antiplatelet therapy. Thromb Res. 2007;120:465–469. doi: 10.1016/j.thromres.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 12.Lee JK, Kang HW, Kim SG, Kim JS, Jung HC. Risks related with withholding and resuming anticoagulation in patients with non-variceal upper gastrointestinal bleeding while on warfarin therapy. Int J Clin Pract. 2012;66:64–68. doi: 10.1111/j.1742-1241.2011.02827.x. [DOI] [PubMed] [Google Scholar]
- 13.Wolf AT, Wasan SK, Saltzman JR. Impact of anticoagulation on rebleeding following endoscopic therapy for nonvariceal upper gastrointestinal hemorrhage. Am J Gastroenterol. 2007;102:290–296. doi: 10.1111/j.1572-0241.2006.00969.x. [DOI] [PubMed] [Google Scholar]
- 14.Chan FK, Ching JY, Hung LC, Wong VW, Leung VK, Kung NN, Hui AJ, Wu JC, Leung WK, Lee VW, et al. Clopidogrel versus aspirin and esomeprazole to prevent recurrent ulcer bleeding. N Engl J Med. 2005;352:238–244. doi: 10.1056/NEJMoa042087. [DOI] [PubMed] [Google Scholar]
- 15.Barkun AN, Bardou M, Kuipers EJ, Sung J, Hunt RH, Martel M, Sinclair P International Consensus Upper Gastrointestinal Bleeding Conference Group. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010;152:101–113. doi: 10.7326/0003-4819-152-2-201001190-00009. [DOI] [PubMed] [Google Scholar]
- 16.Endo M, Higuchi M, Chiba T, Suzuki K, Inoue Y. Present state of endoscopic hemostasis for nonvariceal upper gastrointestinal bleeding. Dig Endosc. 2010;22:S31–S34. doi: 10.1111/j.1443-1661.2010.00976.x. [DOI] [PubMed] [Google Scholar]
- 17.Kawamura T, Yasuda K, Morikawa S, Itonaga M, Nakajima M. Current status of endoscopic management for nonvariceal upper gastrointestinal bleeding. Dig Endosc. 2010;22:S26–S30. doi: 10.1111/j.1443-1661.2010.00972.x. [DOI] [PubMed] [Google Scholar]
- 18.Maggio D, Barkun AN, Martel M, Elouali S, Gralnek IM Reason Investigators. Predictors of early rebleeding after endoscopic therapy in patients with nonvariceal upper gastrointestinal bleeding secondary to high-risk lesions. Can J Gastroenterol. 2013;27:454–458. doi: 10.1155/2013/128760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Restellini S, Kherad O, Jairath V, Martel M, Barkun AN. Red blood cell transfusion is associated with increased rebleeding in patients with nonvariceal upper gastrointestinal bleeding. Aliment Pharmacol Ther. 2013;37:316–322. doi: 10.1111/apt.12170. [DOI] [PubMed] [Google Scholar]


