Abstract
Background and objective
There is little evidence that electronic medical record (EMR) use is associated with better compliance with clinical guidelines on initiation of antiretroviral therapy (ART) among ART-eligible HIV patients. We assessed the effect of transitioning from paper-based to an EMR-based system on appropriate placement on ART among eligible patients.
Methods
We conducted a retrospective, pre-post EMR study among patients enrolled in HIV care and eligible for ART at 17 rural Kenyan clinics and compared the: (1) proportion of patients eligible for ART based on CD4 count or WHO staging who initiate therapy; (2) time from eligibility for ART to ART initiation; (3) time from ART initiation to first CD4 test.
Results
7298 patients were eligible for ART; 54.8% (n=3998) were enrolled in HIV care using a paper-based system while 45.2% (n=3300) were enrolled after the implementation of the EMR. EMR was independently associated with a 22% increase in the odds of initiating ART among eligible patients (adjusted OR (aOR) 1.22, 95% CI 1.12 to 1.33). The proportion of ART-eligible patients not receiving ART was 20.3% and 15.1% for paper and EMR, respectively (χ2=33.5, p<0.01). Median time from ART eligibility to ART initiation was 29.1 days (IQR: 14.1–62.1) for paper compared to 27 days (IQR: 12.9–50.1) for EMR.
Conclusions
EMRs can improve quality of HIV care through appropriate placement of ART-eligible patients on treatment in resource limited settings. However, other non-EMR factors influence timely initiation of ART.
Keywords: Medical Records, HIV, Guidelines adherence, Developing countries, Quality of healthcare
Introduction
Electronic medical record (EMR) systems have been shown to significantly improve the quality of healthcare through improved availability of high quality data for clinical decision making.1 2 Additionally, EMRs improve adherence to treatment guidelines, resulting in better management of chronic illnesses3 4 which often require collection of complex data that is longitudinal.5 The easy retrieval of electronic data and automated reports through EMRs can provide information on compliance or non-compliance with key conditions in the clinical guidelines and timeliness of laboratory tests to monitor disease progression and response to treatment.4 Studies conducted in sub-Saharan Africa (SSA) have shown improvement in time-dependent events following the introduction of EMRs, such as time to process and analyze laboratory specimens, patient waiting time, and duration of hospitalization.5–7 Expansion of health systems in many African countries has been hampered by weak infrastructure, lack of adequate skilled health workers, lack of or poor policies, and inadequate funding. EMRs provide a unique opportunity to enhance clinical care by integrating systems that have been demonstrated to work in developed countries.8 9 As HIV remains a major public health problem in SSA, which is home to two-thirds of the world's 34 million HIV-infected persons, substantial global funding for the management of this disease has led to increased investment in EMRs in order to manage the complex data for monitoring the lifelong treatment of those infected.10 11
The wide-scale availability of antiretroviral therapy (ART) has significantly reduced HIV-related morbidity and mortality since 2000.12–14 As of December 2011, 54% of 14.8 million patients eligible for ART globally were receiving ART. The majority (75%, n=6 million) of those receiving ART were in SSA.14 As of September 2012, approximately 600 000 patients were receiving ART out of 1.5 million HIV-infected persons in Kenya.15 WHO guidelines define conditions for ART eligibility based on the clinical presentation of the patient (WHO staging) and on the immunological status assessed using CD4 T-cell count.16–18 Despite the global decline in mortality among HIV-infected patients, the number of deaths still remains high in SSA as many eligible patients are not initiated on ART or are initiated late, when the disease is in advanced stages. This is evident through advanced clinical signs or low baseline CD4 T-cell count indicative of a weakened immune system.19 Although CD4 T-cell count testing is a routine laboratory measurement for patients enrolled in HIV care programs, test results are not always available for clinical management of patients due to breakdown of flow cytometry equipment, lack of reagents, or poor recording and can contribute to late or inappropriate initiation of ART.20 21 Clinicians may also fail to recognize immunological treatment failure which may delay necessary changes in ART regimens.
There is no published evidence that EMRs can improve adherence to clinical guidelines on placement of ART-eligible patients on treatment in resource-limited settings. The purpose of this study was to assess the effect of transitioning from the use of paper-based to an EMR-based system for HIV patient data management on timely initiation of ART among eligible patients and timely performance of CD4 T-cell count test as described in the Kenya national HIV treatment guidelines.22
Methods
This study was conducted at 17 out of 122 rural health facilities in Siaya County in Western Kenya providing HIV care and treatment services. The 17 government-owned clinics are among 20 facilities where the Kenya Medical Research Institute (KEMRI) provides data management and information and communications technology (ICT) support. Three clinics that were excluded from this study did not have electric power or a secure location for a computer at the time of the study. All these facilities have transitioned from the use of paper-based to EMR-based systems for management of patient data. EMRs were installed at the facilities on varying dates between September 2009 and June 2012. The clinics included four district hospitals (level 4, headed by a physician and provides full inpatient and outpatient care, offering access to select specialized services), 11 health centers (level 3, headed by a clinical officer and provides the lowest level of inpatient care, in addition to outpatient and maternity services), and two dispensaries (level 2, headed by a nurse and provides the lowest level of facility-based outpatient services).23
ART eligibility and appropriate placement of patients on ART
The Kenyan Ministry of Health (K-MOH) guidelines for ART22 were adapted from the WHO guidelines which were published in 2007 and revised in 2010.24 The K-MOH guidelines recommend using the patient's clinical status (WHO staging) and CD4 cell count as key determinants when assessing eligibility for placement of patients on ART. In this paper, appropriate placement refers to the guideline-based initiation of ART among eligible patients.
WHO clinical staging
The WHO clinical staging uses clinical parameters to categorize HIV infection into four stages that reflect disease severity and prognosis.18 24 WHO clinical stages I and II are often associated with early HIV infection and manifest as conditions such as minor skin diseases and upper respiratory tract infections. WHO clinical stages III and IV are associated with advanced HIV disease and may manifest as one or more diseases such as extrapulmonary tuberculosis, esophageal candidiasis, or Kaposi sarcoma and are used to confirm eligibility for initiation of ART. WHO staging is used mainly to help clinicians make decisions on ART eligibility in health facilities which have no immediate access to CD4 T-cell count testing.
CD4 T-cell count and ART eligibility
CD4 T-cell counts serve as the most important laboratory-based measurement of the state of immunosuppression among patients with HIV and is a main prognostic indicator of patients starting ART.22 The current K-MOH guidelines, which were implemented in 2011, recommend ART initiation among patients aged 2 years or older with the following conditions: (i) CD4 ≤350 cells/µL, and stage I or II disease; and (ii) WHO stage III and IV irrespective of CD4 cell count. The K-MOH guidelines recommend initiation of ART for all HIV-infected children under the age of 2 years, irrespective of immunological status measured using CD4 T-cell counts.
Study population
The study population consisted of male and female patients aged 2 years or older, enrolled in HIV care not more than 1 year prior to the implementation of an EMR at the clinic. For example, we excluded patients enrolled in HIV care before June 2008 at clinics where an EMR was installed in June 2009. We also excluded ART-eligible patients who were initiated on ART within 2 months of EMR installation as we considered this to be the learning and transition period. Finally, we excluded patients who had already initiated ART treatment elsewhere prior to transferring into the participating health facility due to unavailability of data on baseline CD4 measurements prior to ART initiation and date of ART eligibility.
Paper-based system
In the paper-based system, patient data were captured using a K-MOH approved Comprehensive Care Clinic Card (MOH 257) which collected data on: demographic and contact details of the patient, treatment support information, HIV testing and treatment history, allergies, HIV treatment eligibility and ART regimen (first or second line ART), vital signs, co-infections (including tuberculosis screening and treatment status and other opportunistic infections), laboratory test results for treatment monitoring (including CD4 T-cell counts, hemoglobin, and alanine aminotransferase (ALT)), treatment outcomes (including death, transfer-out, loss to follow-up, and interrupted treatment), and appointment date for the next visit. Additional notes were recorded on plain paper and filed together with the MOH 257 in the patient charts.
Treatment data from MOH 257 were manually transcribed into the national ART register, and used mainly to provide summary statistics for routine reporting to K-MOH. The date of next visit recorded on the MOH 257 was used for scheduling patient visits for each clinic day. The clinicians read through the patient notes during each clinic visit to review trends in vital signs, patient promptness with appointments, CD4 T-cell counts, and other laboratory-based treatment monitoring parameters.
Transition to EMR system
The EMR system, also referred to as Comprehensive Care Centre Patient Application Database (C-PAD), was developed in 2007. The C-PAD EMR version used for this study was a standalone application developed using Visual Basic for Applications (VBA) and an MS-Access database.
Clinicians record data on the paper-based MOH 257 form during each patient encounter. Each clinic has a data entry clerk who enters these data into C-PAD immediately after the visit. These data are used to generate summary reports that are available for the clinician's review during the weekly clinical review meetings that are also attended by nurses and data clerks. The system has been programmed to ensure that mandatory variables such as demographic data, vital signs, medication, and key laboratory measurements are entered. If these essential variables, including demographic data, vital signs, medication, and laboratory measurements were missing from the MOH 257 form, the data clerks contacted the clinician to ensure that missing data were provided and entered into the EMR, as functionally required by the EMR system. To update the system's database, historical treatment data from the paper-based system were entered retrospectively for all patients who had been initiated on treatment prior to the EMR system installation.
For comparison purposes, retrospective data from the paper systems were entered into the C-PAD system at the participating health facilities.
Outcome measures
The following outcomes were analyzed to measure the quality of HIV care received: (1) proportion of patients eligible for ART based on CD4 count or WHO clinical staging who initiate therapy; (2) time from eligibility for ART to actual ART; and (3) time from ART initiation to the first CD4 T-cell count test following ART.
We compared these outcomes before (paper-based system) and after (C-PAD EMR) the EMR system was introduced in the facilities. For each site, the date of C-PAD installation was used to compare the outcome measures during the paper-based versus the EMR based data management.
Statistical analysis
We included records of patients that were eligible for ART based on the Kenyan ART treatment guidelines.22 We excluded patients that did not have an ART eligibility date but had an ART initiation date, and records with an earlier date of ART initiation compared to the ART eligibility date. We included records of patients who were enrolled in HIV care using a paper-based system and who subsequently became eligible for ART after the installation of EMRs since the duration of follow-up for the majority of these patients was much longer on the paper system than follow-up on EMR before they became eligible for ART.
In univariate analysis, frequencies and proportions were reported for categorical variables and median and IQR were reported for continuous variables. The survivor function measurement was used to calculate median time to event. Patients who had not encountered the anticipated time-based events were censored on the date of the last visit. Kaplan–Meier survival graphs were used to compare time-to-event analysis (time from eligibility to ART initiation and time from ART initiation to first CD4 cell count) between the paper-based and the EMR system. The log rank test of equality was used to test for differences in the rate of occurrence of the time-based events between the paper-based system and the EMR system. Pearson's χ2 test was used to test for the statistical difference between proportions of eligible patients that were not receiving ART (under-treated) and those that were receiving ART, before and after implementation of the EMR system.
Potential associations between EMR use and ART initiation were also assessed in bivariate analysis using logistic regression expressed as OR and corresponding 95% CIs. All variables in table 2 were entered into a multiple logistic regression model, irrespective of their statistical significance level, to identify predicators that were independently and significantly associated with EMR use and ART initiation. Cox proportional hazards regression models, expressed in HRs and corresponding 95% CI, were used to identify factors associated with time to ART initiation and time to CD4 cell count test. All variables in table 2 were entered into a Cox proportional hazards regression model, irrespective of their statistical significance level, to test for factors independently associated with the time from eligibility for ART to initiation of ART and time to first CD4 T-cell test using adjusted HRs (aHRs) and corresponding 95% CI. We allowed for potential site-level clustering using generalized estimating equations in the logistic and Cox regression models. Stata V.12.1 was used to perform the statistical analysis.
Table 2.
Association between electronic medical record (EMR) and antiretroviral therapy (ART) initiation among eligible patients, location, year
| Variable | ART initiation | |||
|---|---|---|---|---|
| OR (95% CI) | p Value | Adjusted OR (95% CI) | p Value | |
| Paper based system | Ref | Ref | ||
| EMR system | 1.44 (1.23 to 1.68) | <0.01 | 1.22 (1.16 to 1.33) | <0.01 |
| Male | Ref | Ref | ||
| Female | 1.22 (1.10 to 1.36) | <0.01 | 1.04 (0.91 to 1.18) | 0.35 |
| Age (years) | 1.00 (1.00 to 1.00) | 0.53 | 1.01 (1.00 to 1.01) | <0.01 |
| WHO stage 1 | Ref | Ref | ||
| WHO stage 2 | 0.93 (0.30 to 2.84) | 0.89 | 0.91 (0.25 to 3.35) | 0.89 |
| WHO stage 3 | 0.01 (0.00 to 0.05) | <0.01 | 0.16 (0.00 to 0.05) | <0.01 |
| WHO stage 4 | 0.01 (0.00 to 0.03) | <0.01 | 0.01 (0.00 to 0.04) | <0.01 |
| Level 2 facility | Ref | Ref | ||
| Level 3 facility | 1.12 (0.53 to 2.38) | 0.76 | 1.07 (0.90 to 1.28) | 0.46 |
| Level 4 facility | 0.64 (0.29 to 1.41) | 0.27 | 0.79 (0.68 to 0.92) | <0.01 |
Ethical considerations
The study was approved by the Associate Director for Science at the Division of Global HIV/AIDS of the US Centers for Disease Control and Prevention (CDC) and the KEMRI institutional review board. Individual patient data were de-identified by the KEMRI staff responsible for primary data collection prior to analysis.
Results
Of the 11 637 patients aged 2 years or older enrolled in HIV care programs not more than 1 year prior to the implementation of the EMR, a total of 7308 patients were eligible for ART based on their CD4 T-cell count or WHO staging. We further excluded records from one patient who had no ART eligibility date but had an ART initiation date. In addition, we excluded nine records that had an earlier ART initiation date than the date of ART eligibility. Among the remaining 7298 eligible patients, 54.8% (n=3998) were enrolled in HIV care using a paper-based system while 45.2% (n=3300) were enrolled after the implementation of an EMR (table 1). In total, 5990 (82.1% of eligible patients) were receiving ART, including 3595 (60.0%) women and 2395 (40.0%) men. The median age of patients enrolled using paper based systems was 31.6 years (IQR: 25.3–40.3) compared to 31.6 years (IQR: 24.8–40.5) for patients enrolled after transitioning to EMR. Median baseline CD4 T-cell count after enrollment in HIV care was 324 cells/µL (IQR: 202–486).
Table 1.
Number of patients, by health facility, enrolled on HIV care, eligible for antiretroviral therapy (ART) and those initiated on ART using paper and electronic medical record (EMR) systems
| Facility ID | Facility level* | EMR installation date | Paper | EMR | ||||
|---|---|---|---|---|---|---|---|---|
| Enrolled in HIV care | Eligible for ART | Initiated on ART: n (%)† | Enrolled in HIV care | Eligible for ART | Initiated on ART: n (%)† | |||
| 1 | 3 | 11/1/2011 | 114 | 62 | 58 (93.5) | 55 | 30 | 29 (96.7) |
| 2 | 4 | 8/1/2010 | 1343 | 875 | 717 (81.9) | 1153 | 700 | 627 (89.6) |
| 3 | 2 | 10/1/2011 | 208 | 127 | 101 (79.5) | 37 | 11 | 10 (90.9) |
| 4 | 4 | 12/1/2009 | 601 | 356 | 296 (83.1) | 886 | 455 | 400 (87.9) |
| 5 | 3 | 11/1/2011 | 101 | 55 | 53 (96.4) | 46 | 22 | 20 (90.9) |
| 6 | 3 | 12/1/2010 | 232 | 161 | 144 (89.4) | 284 | 189 | 159 (84.1) |
| 7 | 2 | 10/1/2011 | 253 | 126 | 118 (93.7) | 49 | 18 | 15 (83.3) |
| 8 | 3 | 8/1/2010 | 595 | 349 | 297 (85.1) | 308 | 176 | 158 (89.8) |
| 9 | 4 | 9/1/2009 | 1478 | 1082 | 802 (74.1) | 1743 | 1164 | 961 (82.6) |
| 10 | 3 | 11/1/2011 | 204 | 100 | 84 (84.0) | 20 | 3 | 3 (100.0) |
| 11 | 4 | 12/1/2009 | 658 | 506 | 340 (67.2) | 844 | 532 | 421 (79.1) |
| 12 | 3 | 6/1/2012 | 1 | 1 | 0 (0.0) | 0 | 0 | 0 (0.0) |
| 13 | 3 | 6/1/2012 | 96 | 60 | 54 (90.0) | 0 | 0 | 0 (0.0) |
| 14 | 3 | 6/1/2012 | 159 | 61 | 55 (90.2) | 6 | 0 | 0 (0.0) |
| 15 | 3 | 7/1/2012 | 30 | 20 | 14 (70.0) | 1 | 0 | 0 (0.0) |
| 16 | 3 | 6/1/2012 | 73 | 33 | 30 (90.9) | 0 | 0 | 0 (0.0) |
| 17 | 3 | 7/1/2012 | 59 | 24 | 24 (100.0) | 0 | 0 | 0 (0.0) |
| Total | 6205 | 3998 | 3187 (79.7) | 5432 | 3300 | 2803 (84.9) | ||
*Facility level: 2, dispensary; 3, health center; 4, district hospital. A detailed description of facility types is provided in the Methods section.
†The percentages in parentheses are calculated using the number of patients initiated on ART as the numerator, and the number of patients eligible for ART as the denominator.
ART initiation among eligible patients
Use of EMR was significantly associated with an improved ART initiation among patients compared to the paper-based system (OR=1.44, 95% CI 1.23 to 1.68) (table 2). After adjusting for patient's sex, age, WHO stage, and level of health facility, EMR was independently associated with a 22% increase in the odds of initiating ART among eligible patients (aOR=1.22, 95% CI 1.12 to 1.33) compared to paper-based systems. After excluding the six clinics that had no patients eligible for ART during the data collection period (facility IDs 12, 13, 14, 15, 16, and 17) the odds of ART initiation among eligible patients was OR=1.49 (95% CI 1.28 to 1.71) and aOR=1.21 (95% CI 1.10 to 1.32).
During the period in which the facility used the paper-based system, 20.3% (n=811) of patients were eligible for ART but were not receiving ART versus 15.1% (n=497) of patients who were eligible for ART after implementation of EMR system (χ2=33.5; p<0.01).
Time from ART eligibility to actual initiation of ART
The median time from ART eligibility to initiation was 29.1 days (IQR: 14.1–62.1) in the paper-based system compared to 27 days (IQR: 12.9–50.1) in the EMR system. The median time to ART initiation remained unchanged after excluding the clinics with no patients eligible for ART. However, the IQR got narrower in the paper group. Median time (excluding facility ID 12, 13, 14, 15, 16, and 17) was 29.1 days (IQR: 30.0–63.9) for paper, and 27.0 days (IQR: 12.9–50.1) for EMR. Of the patients eligible for ART, 84.5% (95% CI 82.4% to 86.4%) had initiated ART 3 months from date of eligibility using the paper-based system compared to 90.2% (95% CI 88.4% to 91.7%) using the EMR system (figure 1). EMR use was associated with a 25% increase in HR of initiation of ART among eligible patients (HR=1.25; 95% CI 1.02 to 1.52). After adjusting for patient's sex, age, WHO stage, and level of health facility, the adjusted HR of ART initiation after implementation of an EMR was 1.36 (95% CI 1.20 to 1.53).
Figure 1.
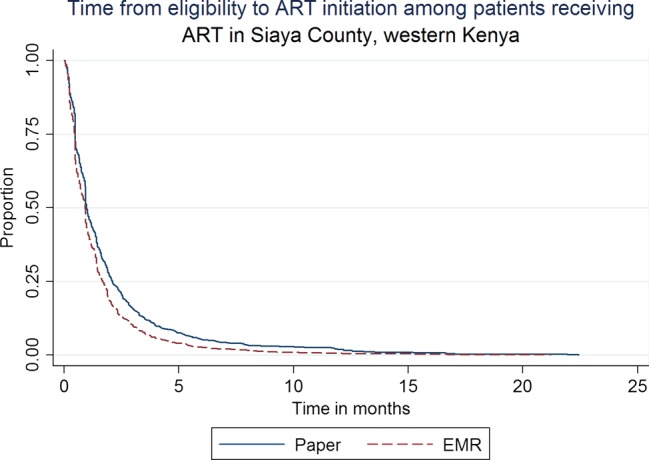
Time from eligibility to ART initiation.
Time from ART initiation to first CD4 test following initiation
Among the 5990 patients receiving ART, 3458 (57.7%) had at least one CD4 T-cell count test after initiation of ART. The median time from ART initiation to first CD4 T-cell count test was 6.27 months (IQR: 4.27–10.70) and 6.17 months (IQR: 4.63–11.43) for paper and EMR based systems, respectively. Six months after ART initiation, 46.1% (95% CI 44.0% to 48.2%) of the patients receiving ART and enrolled using the paper-based system had had at least a CD4 T-cell count test compared to 45.5% (95% CI 43.1% to 47.9%) of patients using the EMR system (figure 2). EMR use was not significantly associated with the hazard of conducting the first CD4 test after initiation of ART (HR=0.94, 95% CI 0.68 to 1.28). After adjusting for sex, age, WHO stage, and facility level, aHR=0.98 (95% CI 0.74 to 1.28).
Figure 2.
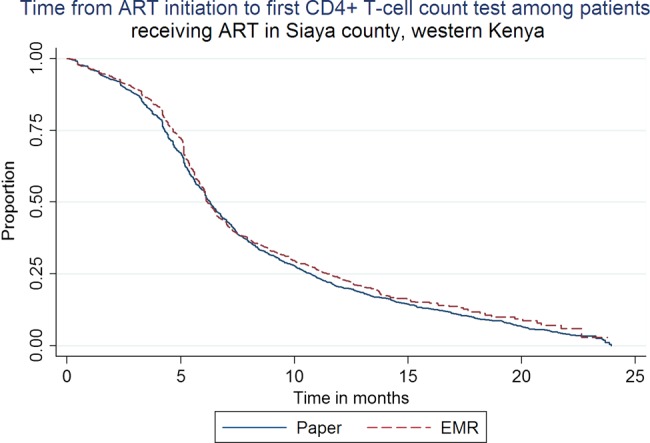
Time from ART initiation to first CD4+ T-cell test.
Discussion
EMR use was associated with a 22% increase in the odds of ART initiation among eligible patients enrolled into HIV care after transitioning from a paper-based system. Although the study showed a 7% reduction in the time from ART eligibility to ART initiation following the introduction of an EMR (from 29.1 days down to 27 days), this was not clinically significant. The study also showed that about 80% of patients eligible for ART had been initiated on therapy. Although this proportion is higher than the 56% coverage that UNAIDS reported for SSA at the end of 2011,14 some 20% of eligible patients are still not receiving ART which may mean under-treatment of these patients. Although EMR use was not significantly associated with a reduction in time to conduct a CD4 T-cell test following ART initiation, the duration using both paper and EMR systems was comparable to the 6 months recommended in the K-MOH treatment guidelines.22
EMR use increased the chances of patients turning up at the clinic for ART initiation but not how fast they came. The difference in time from ART eligibility to ART initiation between the EMR and paper groups was marginal, suggesting that EMR use did not influence timely initiation of ART despite the weekly generated list of eligible patients that were not receiving treatment. Non-EMR factors such as clinician behavior (provider practice)25 26 and the time for preparation of patients for ART, which includes adherence counseling prior to ART initiation to improve compliance to the treatment regimen22 and the patient's own readiness to initiate ART, could have contributed to the relatively unchanged time to treatment initiation. On the other hand, without a reminder (whether lists generated by an EMR or other systems), the need to thoroughly review patient notes to verify eligibility can be overwhelming to clinicians who may in some cases forget to initiate ART among eligible patients, resulting in a missed opportunity for appropriate ART initiation. This scenario is more likely in busy clinics or when the patient's clinical presentation does not indicate they are eligible for ART.
The missed opportunity of not providing appropriate treatment to 22% of the 4000 patients using paper-based system translates to 880 patients not being appropriately placed on treatment. It has been shown that late initiation of treatment results in poor outcomes, including increased mortality.27 Level 4 facilities seemed to be negatively associated with initiation of ART among eligible patients. This could be due to the high volume of patients receiving HIV care at these facilities served by a small number of overworked clinicians.
A key strength of our study is that it was conducted at multiple sites using the same K-MOH ART guidelines, hence a large sample size which improved the precision of the estimates. All 17 participating health facilities had similar administrative, managerial, and laboratory procedures as well as drug regimens.
Our study was not without limitations. Since the retrospective study was based on routinely collected data from rural health facilities, we had challenges with the data quality; for example, we excluded records that did not have an ART eligibility date but had an ART initiation date, or those with an earlier date of ART initiation than the ART eligibility date. Additionally, we excluded from analysis records which had an eligibility date later than the date of ART initiation. However, such records were less than 1% of all the records included in the analysis and therefore had minimal impact on the results. It was difficult to determine whether patients that had no recorded ART eligibility date but were on therapy (n=10) were actually over-treated. EMRs had only been in use for approximately 6 months in a few facilities, which potentially impacted on data quality. Appropriate initiation of ART as recommended in the clinical guidelines is influenced by several factors such as clinician's practice, patient's behavior and preference, and societal factors. These factors potentially confounded the true association of EMRs and ART initiation. The challenges reported in transitioning from paper to EMR systems were not unique to our study; limited technical skills, poor data quality, and poor infrastructure (including frequent power outages) were also reported by Fraser and Williams.8 9 Other temporal factors such as improved knowledge of health workers and better access to CD4 T-cell count testing equipment could have also contributed to the observed improvements over time.
The benefits of EMR use in improving quality of care can potentially be used to inform policies around the use of technology based solutions in clinical settings in SSA. In an environment of stiff competition for resources, there is a need for tangible evidence to convince decision makers to invest resources in technologies that have been shown to improve efficiency and adherence to treatment guidelines.
Conclusion
We found that EMRs can improve quality of HIV care through appropriate placement of ART-eligible patients on treatment in resource-limited settings. However, other non-EMR factors influence timely initiation of ART. There is room for improvement in adherence to clinical guidelines. Rigorous evaluation studies are needed to demonstrate associations between decision support systems implemented in EMRs and important quality of HIV care indicators such as retention on treatment.
Acknowledgments
The authors would like to acknowledge the KEMRI Director and his staff for the approval of this study and for reviewing and clearing the manuscript. We would also like to thank all staff at the 17 clinics in Siaya County that supported the data collection for this study.
Footnotes
Contributors: TO, AA-H, and NdK conceptualized and designed the study. AK, DK, and DK reviewed the clinical components of the study and manuscript. VS was the study statistician and developed the analysis programs. PL and NO provided oversight to the data management team that conducted the data collection, de-identification, and cleaning. All co-authors were involved in interpreting the results. TO and NdK drafted and revised the manuscript. All authors edited and reviewed the manuscript and gave their final approval for submission to the journal.
Funding: This publication was made possible by support from the US President's Emergency Plan for AIDS Relief (PEPFAR) through the US Centers for Disease Control and Prevention (CDC), Division of HIV/AIDS (DGHA), under the KEMRI/CDC Cooperative Agreement no. GH000048-04.
Disclaimer: The content and views in this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention (CDC) or the Kenya Medical Research Institute (KEMRI).
Competing interests: None.
Ethics approval: US Centers for Disease Control, Atlanta, Georgia, USA; Kenya Medical Research Institute, Nairobi, Kenya.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Amoroso CL, Akimana B, Wise B, et al. Using electronic medical records for HIV care in rural Rwanda. Stud Health Technol Inform 2010;160(Pt 1):337–41 [PubMed] [Google Scholar]
- 2.Castelnuovo B, Kiragga A, Afayo V, et al. Implementation of provider-based electronic medical records and improvement of the quality of data in a large HIV program in Sub-Saharan Africa. PLoS ONE 2012;7:e51631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cebul RD, Love TE, Jain AK, et al. Electronic health records and quality of diabetes care. N Engl J Med 2011;365:825–33 [DOI] [PubMed] [Google Scholar]
- 4.Landis LZ, Mello-Thoms C, Gadabu OJ, et al. The feasibility of automating audit and feedback for ART guideline adherence in Malawi. J Am Med Inform Assoc 2011;18:868–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Were MC, Shen C, Tierney WM, et al. Evaluation of computer-generated reminders to improve CD4 laboratory monitoring in sub-Saharan Africa: a prospective comparative study. J Am Med Inform Assoc 2011;18:150–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alamo ST, Wagner GJ, Sunday P, et al. Electronic medical records and same day patient tracing improves clinic efficiency and adherence to appointments in a community based HIV/AIDS care program, in Uganda. AIDS Behav 2012;16:368–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Westbrook JI, Georgiou A, Dimos A, et al. Computerised pathology test order entry reduces laboratory turnaround times and influences tests ordered by hospital clinicians: a controlled before and after study. J Clin Pathol 2006;59:533–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fraser HS, Blaya J. Implementing medical information systems in developing countries, what works and what doesn't. AMIA Annu Symp Proc 2010;2010:232–6 [PMC free article] [PubMed] [Google Scholar]
- 9.Williams F, Boren SA. The role of the electronic medical record (EMR) in care delivery development in developing countries: a systematic review. Inform Prim Care 2008;16:139–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.GFATM. The Global Fund to fight AIDS, Tuberculosis and Malaria. http://www.theglobalfund.org/en/ 13 A.D. June 27 [cited 30 Jun 2013];
- 11.US Office of the Global AIDS Coordinator. US President's Emergency Plan for AIDS Relief. http://www.pepfar.gov/about/strategy/index.htm 13 A.D. June 27
- 12.Gargano JW, Laserson K, Muttai H, et al. The adult population impact of HIV care and antiretroviral therapy in a resource poor setting, 2003–2008. AIDS 2012;26:1545–54 [DOI] [PubMed] [Google Scholar]
- 13.Sidibe M. Antiretrovirals for prevention: realizing the potential. closing commentary by the executive director of UNAIDS. Curr HIV Res 2011;9:470–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.UNAIDS. Global report: UNAIDS report on the global AIDS epidemic 2012. 2013
- 15.US President's Emergency Plan for AIDS Relief. Unpublished Semi-Annual PEPFAR Report for Kenya: 2013. 2013 Mar 31
- 16.World Health Organizations. Geneva, Switzerland. Antiretroviral drugs for treating pregnant women and preventing HIV infection in infants: recommendations for a public health approach—2010 version. 2010
- 17.World Health Organizations. Geneva, Switzerland. Antiretroviral therapy for HIV infection in infants and children: Towards universal access. 2010
- 18.World Health Organizations. Geneva, Switzerland. Antiretroviral therapy for HIV infection in adults and adolescents. 2010
- 19.Maskew M, Brennan AT, Westreich D, et al. Gender differences in mortality and CD4 count response among virally suppressed HIV-positive patients. J Womens Health (Larchmt) 2013;22:113–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thairu L, Katzenstein D, Israelski D. Operational challenges in delivering CD4 diagnostics in sub-Saharan Africa. AIDS Care 2011;23:814–21 [DOI] [PubMed] [Google Scholar]
- 21.Varughese JK, Rosenberg MG, Kim K. HIV in the tropics: staging in the resource-limited setting. Curr Opin Infect Dis 2012;25:477–83 [DOI] [PubMed] [Google Scholar]
- 22.National AIDS and STI Control Program (NASCOP) MoHNK. Guidelines for Anti Retroviral Therapy in Kenya. 2006
- 23.Kenya National Coordinating Agency for Population and Development. Kenya Service Provision Assessment Survey 2010. 2011
- 24.World Health Organizations.Geneva.Switzerland. Towards universal access: scaling up priority HIV/AIDS interventions in the health sector: progress report 2010. 2010
- 25.Carroll AE, Anand V, Downs SM. Understanding why clinicians answer or ignore clinical decision support prompts. Appl Clin Inform 2012;3:309–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Downs SM, Anand V, Dugan TM, et al. You can lead a horse to water: physicians’ responses to clinical reminders. AMIA Annu Symp Proc 2010;2010:167–71 [PMC free article] [PubMed] [Google Scholar]
- 27.Mujugira A, Wester CW, Kim S, et al. Patients with advanced HIV type 1 infection initiating antiretroviral therapy in Botswana: treatment response and mortality. AIDS Res Hum Retroviruses 2009;25:127–33 [DOI] [PMC free article] [PubMed] [Google Scholar]


