Abstract
Objective
As healthcare systems and providers move toward meaningful use of electronic health records, longitudinal care plans (LCPs) may provide a means to improve communication and coordination as patients transition across settings. The objective of this study was to determine the current state of communication of LCPs across settings and levels of care.
Materials and methods
We conducted surveys and interviews with professionals from emergency departments, acute care hospitals, skilled nursing facilities, and home health agency settings in six regions in the USA. We coded the transcripts according to the Agency for Healthcare Research and Quality (AHRQ) ‘Broad Approaches’ to care coordination to understand the degree to which current practice meets the definition of an LCP.
Results
Participants (n=22) from all settings reported that LCPs do not exist in their current state. We found LCPs in practice, and none of these were shared or reconciled across settings. Moreover, we found wide variation in the types and formats of care plan information that was communicated as patients transitioned. The most common formats, even when care plan information was communicated within the same healthcare system, were paper and fax.
Discussion
These findings have implications for data reuse, interoperability, and achieving widespread adoption of LCPs.
Conclusions
The use of LCPs to support care transitions is suboptimal. Strategies are needed to transform the LCP from vision to reality.
Keywords: Longitudinal Care Plan, Electronic Health Record, Care Coordination, Meaningful Use
Background and significance
A longitudinal care plan (LCP) is a holistic, dynamic, and integrated plan that documents important disease prevention and treatment goals and plans. An LCP is patient-centered, reflecting a patient's values and preferences, and is dependent upon bidirectional communications. Electronic systems can pull together the various elements of the LCP dynamically to create an appropriate view for the relevant provider and/or patient/family member and provide actionable information to identify and achieve the individual's health and wellness goals along the spectrum of care. However, today most patients do not have an LCP established. This means that there is no standard way in which a patient's care plan is communicated from one setting or level of care to the next.
Communication gaps in care coordination, care transitions, and the content and reliability of information transferred across settings have been identified as threats to patient safety.1 2 From the provider's perspective, insufficient information at the time of transfer can lead to time-consuming telephone clarifications, care delays, provider stress, and increased risk of rehospitalization.3 Information that is transferred across settings is often incomplete, ambiguous, and delayed.4 Jeffs et al5 found that from the patient’s perspective, deficiency of information and lack of patient and family member involvement in care transition planning are common threats to safe transitions. Health information technology (IT) has been identified as a potential solution,1 6 7 but, even within a fully integrated electronic medical record (EMR) system, communication and information transfer can be suboptimal.8 An LCP supported by health IT systems could ensure that the right information is available to key stakeholders.
While the concept of the LCP was developed some time ago,9–13 barriers to widespread adoption and use persist and include lack of clarity related to nomenclature, regulatory requirements, content, communication and messaging standards, care plan governance, and care team member ownership and participation.14–21 An LCP may be especially beneficial in helping ensure cohesive transitions across care settings and effective self-care management, both of which have represented important care gaps.19 22–24 An LCP that is comprised of structured data would allow electronic systems to pull together the various elements dynamically to create an appropriate view for all care team members and to provide actionable information to identify and achieve the individual's health and wellness goals. Such a system would support measuring coordination activities and the effect of these activities on patient outcomes. LCP reconciliation at each care transition provides a means to improve communication and coordination. However, inconsistent definitions are a barrier to objective measurement. The concept of an LCP is referenced in the Affordable Care Act and HITECH, but distinctions are not made between care plan and plan of care and the phrases are often used interchangeably in the industry. The Stage 2 Meaningful Use (MU) requirements describe the plan of care as ‘the structure used to define the management actions for the various conditions, problems, or issues.’25 The MU regulation includes communication of LCP components such as patient problems, goals, patient instructions, allergies, medications, and responsible clinicians. Patient goals and instructions are optional fields and are not required for Stage 2. However, they are proposed for Stage 3. The Standards and Interoperability (S&I) Framework (a collaborative working to facilitate exchange of health information) has convened stakeholders to define and make a clear distinction between the two concepts. The phrase care plan is used when referencing an LCP and plan of care relates to a discipline-specific set of related problems or health concerns. The S&I Framework describes a hierarchical structure of care plan components with different layers of complexity. Care plans are at the highest level and used longitudinally. Plans of care are used within a single discipline or setting, and treatment plans relate to a single problem or health concern.26 Using this framework, each patient can have one care plan but many plans of care and many treatment plans (see table 1). As the number of problems, providers, and sites increase, overall coordination of different provider-specific treatment plans, discipline-specific plans of care, and the production of a master care plan (eg, an LCP) are needed.
Table 1.
S&I Framework definitions related to longitudinal care plans26
| Care plan | Over arching, longitudinal blueprint of all sites and all team members’ (including patients) prioritized concerns, goals, and interventions |
| Plan of care (POC) | Discipline-specific set of related problems or health concerns. Different plans of care require reconciliation into a single care plan. Examples: acute care POC and home care POC |
| Treatment plan | Focuses on a specific health concern and typically managed by one clinician. Example: physical therapy treatment plan |
| Health concerns (used by S&I Framework in lieu of ‘problems’) | The issues, current status, and ‘likely course’ identified by the patient or team members that require intervention(s) to achieve the patient’s goals of care, any issue of concern to the individual or team member |
| Goal | A defined outcome or condition to be achieved in the process of patient care. Includes patient defined goals (eg, prioritization of health concerns, interventions, longevity, function, comfort) and clinician-specific goals to achieve desired and agreed upon outcomes |
| Patient instructions | Information or directions to the patient and other providers including how to care for the individual's condition, what to do at home, when to call for help, any additional appointments, testing, and changes to the medication list or medication instructions, clinical guidelines, and a summary of best practice. Detailed list of actions required to achieve the patient’s goals of care |
| Responsible clinicians | Parties who manage and/or provide care or service as specified and agreed to in the care plan, including clinicians, other paid and informal caregivers, and the patient |
| Interventions | Actions taken to maximize the prospects of achieving the patient’s or providers’ goals of care, including the removal of barriers to success. Instructions are a subset of interventions |
| Outcomes | Status, at one or more points in time in the future, related to established care plan goals |
MU requirements for care plans are minimal, focusing on acute and outpatient provider settings, and documentation of patient problems, goals, patient instructions, and responsible clinicians. Data elements that could improve communication across transitions are currently proposed for future stages27 28 and include patient preferences, diagnostic and therapeutic plans related to patient goals, pending tests, information on follow-up care, the self-care management plan, and orders for treatments and interventions.
Practice and workflow challenges are barriers to LCP implementation. To date, care plans have rarely been patient centered. A care plan within a given healthcare facility is an essential foundation for a meaningful LCP that can transcend individual facilities. Yet most research to date has focused on the development of plans of care used by a single discipline, such as nurses or physicians, or within a single setting, such as an acute care hospital (ACH) or home healthcare agency.29–32 There is limited consensus regarding workflows including the process for patient-centered collaboration and patient involvement in problem identification, goal setting, and reconciliation.29–33 While interdisciplinary plans of care are a requirement for accreditation and reimbursement30 34 and certain elements are a requirement for Stage 2 MU,7 11 there is lack of clarity regarding which data elements constitute a care plan and a dearth of best practices for sharing, updating, and reconciliation.33
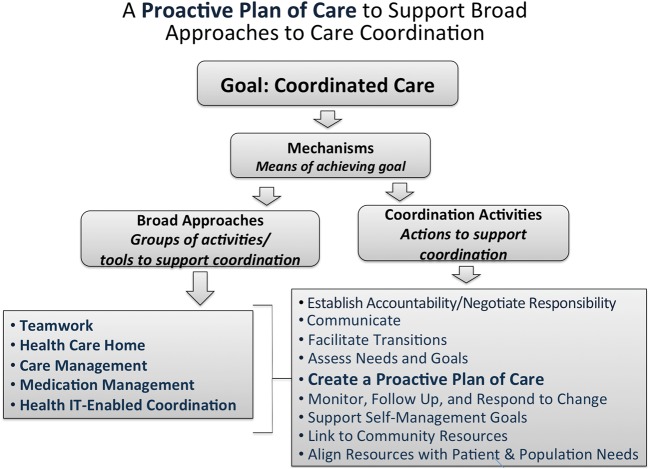
The Agency for Healthcare Research and Quality Care Coordination Framework
The Agency for Healthcare Research and Quality (AHRQ) Care Coordination Measurement Framework defines coordination as a mechanism to achieve care goals. The delivery of high-quality healthcare that is aligned with patients’ and families’ needs and preferences is guided by five ‘Broad Approaches’ in the framework that support care coordination. In addition, the framework identifies nine activities that facilitate coordination within each of the Broad Approaches (see figure 1). One of these activities is creating a plan of care. However, a plan of care that is developed and used within a single setting will not facilitate care coordination. An LCP used across the Broad Approaches and as a tool to improve care coordination is needed to tie the approaches together and to facilitate transitions across settings and levels of care.
Figure 1.
The AHRQ Care Coordination Framework (adapted from Atlas et al, 2011).34a
Objective
The purpose of this study was to explore the current state of documentation, communication, and reconciliation of care plan data across settings and levels of care from the perspectives of providers in six geographic regions in the USA. We employed the AHRQ Broad Approaches as a structure for the qualitative interviews to understand the degree to which current practice meets the definition of an LCP.
Methods
Site and participants
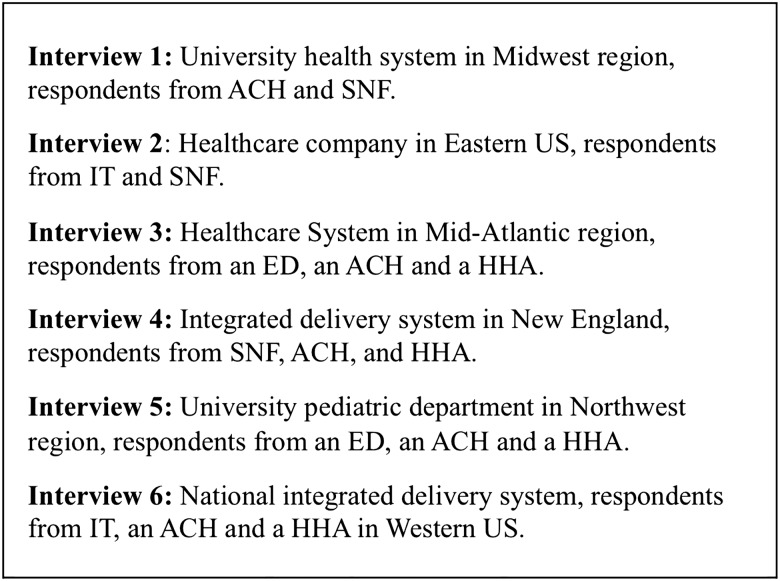
We conducted audio-taped group interviews and administered surveys to explore communication and reconciliation of care plan data and information across settings and levels of care. Twenty-four sites in six geographic regions (see figure 2) were selected by the National Quality Forum (NQF) Care Coordination Technical Expert Panel (TEP) and represent relatively high levels of electronic capabilities. Healthcare system leadership within each region identified informants from the following types of healthcare facilities (determined by the TEP): emergency department (ED), ACH, skilled nursing facility (SNF), and home health agency (HHA). Leadership were asked to identify clinicians involved in the care transition process and IT staff to help us fully understand the current state.
Figure 2.
Characteristics of respondent sites. ACH, acute care hospital; ED, emergency department; HHA, home healthcare agency; IT, information technology department; SNF, skilled nursing facility.
Informants were then recruited by email invitation from the principal investigator (DWB). The study was designated as exempt by the Partners HealthCare Institutional Review Board. Site agreement and informed consent were secured. Based on the work of the IMPACT (Improving Massachusetts Post-Acute Care Transfers) Project that suggests that there are setting-specific data elements needed to support care transitions,35 we focused on the following transitions: SNF to ED/ACH, ACH to HHA, and ACH to SNF. Through a survey to each participating organization, we used the Stage 2 MU plan of care data element requirements from the rule (ie, problems, goals, medications, patient instructions, responsible clinicians, and allergies) and additional data elements consistent with the definition of an LCP to identify elementary readiness for communication and exchange of care plans.36 More detailed approaches and tools were explored in the group interviews.
Data collection and analysis
Surveys
Surveys were sent to 24 contacts at 17 sites in the six regions with a request to complete as ‘sender’ and as ‘receiver’ of the LCP data. The survey format was based on work from the IMPACT Project. For each LCP data, element respondents were asked the following:
- Do you personally RECEIVE this information with patient transfers?
- If No, does someone else at your site RECEIVE this information with patient transfers?
- Do you personally SEND this information with patient transfers?
- If No, does someone else at your site SEND this information with patient transfers?
For all information (sent or received), participants were asked to provide the format (paper or electronic). Descriptive statistics were used to summarize the survey data.
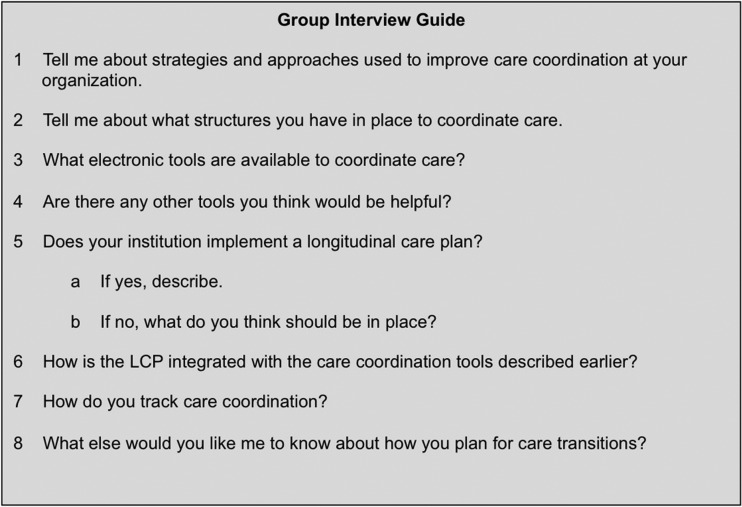
Group interviews
Twenty-nine interdisciplinary providers from 17 institutions participated in six group interviews. In all six group interviews, an interview guide based on a review of the literature on care plans (see figure 3) was used along with requests for clarification to increase response depth. We employed the AHRQ Broad Approaches and themes from the review of literature to frame the qualitative interview guide. Discussion focused on organizational readiness to support care coordination, communication, and reconciliation of the care plan across settings and levels of care. The moderator elicited answers from individual informants and promoted group discussion. Clarification was requested concerning information learned in earlier groups, such as their experiences and views about discipline-specific plans of care, plans of care developed within each level of care, the use (or lack) of IT for providing access to the care plan across settings and levels of care, and the process for care plan reconciliation.
Figure 3.
Group interview guide.
Raw data were transcribed into Microsoft Word, reviewed, and corrected for transcription accuracy and removal of identifying characteristics. The transcripts were uploaded into the NVivo37 software program, independently coded by two investigators (PCD, LS) using a priori codes. Codes were based on the elements included in the five Broad Approaches and the nine activities of the AHRQ Care Coordination Framework (see figure 1). A two-person consensus approach involving discussion and consultation was used to resolve coding discrepancies. A third investigator (ACH) adjudicated unresolved discrepancies. Basic content analysis methods38 were followed to analyze the descriptive data. Multiple methods including a process of debriefing among researchers, engagement with the raw data and codes, the use of field and reflective notes, and internal audits of coding were used to ensure credibility and dependability. Concepts were linked in order to discover new perspectives from the accounts of participants’ experiences.39 Demographic data from the 22 informants who returned the demographic form are included in table 2.
Table 2.
Summary of group interview participant characteristics (n=22)
| Mean age | 38 (range 24–69) |
| Female | 77% |
| Race | |
| White | 91% |
| Asian | 9% |
| Interdisciplinary provider type | |
| Nurse | 55% |
| Physician | 23% |
| Physical therapist | 5% |
| Other | 18% |
| Mean number of years working as a healthcare professional | 21 (range 2–50) |
| Years working at current institution | 22 (range 2–25) |
| Highest professional degree | |
| Diploma | 5% |
| BS/BA | 18% |
| MA/MS | 41% |
| Doctoral degree | 36% |
| Compared to your peers, how do you rate your computer skills? | |
| Above average | 41% |
| Average | 45% |
| Below average | 14% |
Results
Surveys
We received completed surveys from all 17 sites surveyed in the six regions: five ACH senders, four ACH receivers, three ‘Other’ senders (eg, SNF, HHA), and five ‘Other’ receivers. Responses (eg, total count of institutions responding ‘yes’ to receiving or sending each data element) by sender type are included in table 3.
Table 3.
LCP data element survey results by receiver/sender and data format
| LCP data elements | RECEIVE this information with patient transfers | SEND this information with patient transfers | ||||||
|---|---|---|---|---|---|---|---|---|
| Paper | Electronic | Paper | Electronic | |||||
| ACH | Non-ACH | ACH | Non-ACH | ACH | Non-ACH | ACH | Non-ACH | |
| Responsible clinician* | 2 | 1 | 0 | 3 | 1 | 1 | 4 | 0 |
| Patient problems* | 3 | 1 | 0 | 2 | 2 | 2 | 3 | 0 |
| Patient likes and dislikes | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Patient’s goals/expectations of care* | 0 | 0 | 0 | 1 | 1 | 1 | 0 | |
| Proposed interventions and procedures for patient after transfer/discharge related to patient goals | 1 | 1 | 0 | 2 | 2 | 1 | 1 | 0 |
| Patient self-management plan | 0 | 0 | 0 | 0 | 2 | 0 | 2 | 0 |
| Follow-up plans related to patient goals | 0 | 1 | 0 | 1 | 2 | 1 | 1 | 0 |
| Clinical instructions given to patient | 0 | 0 | 0 | 2 | 3 | 1 | 2 | 0 |
| Identified learner for education if patient is unable to receive education | 0 | 1 | 0 | 3 | 2 | 0 | 2 | 0 |
| Information for patient on tests pending at discharge/transfer | 0 | 1 | 0 | 1 | 3 | 0 | 2 | 0 |
| Who is responsible for following up? | 0 | 2 | 0 | 1 | 3 | 0 | 1 | 0 |
| Number(s) to call for results | 0 | 1 | 0 | 1 | 3 | 0 | 2 | 0 |
| Orders | 0 | 2 | 0 | 3 | 1 | 1 | 3 | 0 |
| Allergies | 4 | 0 | 0 | 5 | 0 | 3 | 4 | 0 |
| Pre-admission medication list (patient’s home medications prior to admission) | 2 | 1 | 0 | 2 | 1 | 1 | 3 | 0 |
| Discharge medications | 3 | 1 | 0 | 3 | 1 | 3 | 2 | 0 |
| Start date and duration | 3 | 1 | 0 | 3 | 1 | 3 | 2 | 0 |
| Route | 3 | 2 | 0 | 3 | 1 | 3 | 3 | 0 |
| Dose | 3 | 2 | 0 | 3 | 1 | 3 | 3 | 0 |
| Frequency | 3 | 2 | 0 | 3 | 1 | 3 | 3 | 0 |
| Date | 2 | 2 | 0 | 3 | 1 | 2 | 2 | 0 |
| Indication | 2 | 0 | 0 | 1 | 1 | 1 | 3 | 0 |
| Discharge medications unchanged from pre-admission medication list | 2 | 0 | 0 | 2 | 1 | 0 | 1 | 0 |
| Discharge medications on the pre-admission medication list but with change of dose or frequency | 2 | 1 | 0 | 2 | 1 | 0 | 1 | 0 |
| Explanation of change | 1 | 0 | 0 | 2 | 1 | 0 | 2 | 0 |
| New medications (not on pre-admission medication list) | 1 | 1 | 0 | 2 | 1 | 1 | 2 | 0 |
| Reason for addition | 1 | 1 | 0 | 2 | 1 | 0 | 1 | 0 |
| Medications removed from the pre-admission medication list | 1 | 0 | 0 | 2 | 1 | 0 | 2 | 0 |
| Reason for deletion | 1 | 0 | 0 | 2 | 1 | 0 | 1 | 0 |
| Pertinent medications administered during the course of this episode of care not on discharge medication list | 0 | 1 | 0 | 1 | 1 | 0 | 2 | 0 |
*Meaningful Use Requirements (ACH/Outpatient Provider only).
ACH, acute care hospital; LCP, longitudinal care plan.
Group interviews
During the six group interviews, informants’ experiences and views of the care plan in practice and as envisioned for the future emerged. In the sections that follow, we report the major findings as they relate to the use of an LCP within the five Broad Approaches and the degree to which use of the care plan in practice meets the definition of an LCP. Table 4 includes the five AHRQ Broad Approaches, the subthemes identified from a review of the literature and from the analysis, and quotes representing each subtheme.
Table 4.
Group interview results organized by AHRQ Care Coordination Broad Approach and subthemes
| AHRQ Broad Approach | Subtheme | Quote representing subtheme |
|---|---|---|
| 1. Teamwork Focused on Coordination | Interdisciplinary involvement in care plan development current state | ‘The nurse practitioner and social worker start the plan in the web-based care management tracking system, and then they bring an initial [POC] to the team conference, where the patient is present and discussed, and then they fine tune and add to the drafted care plan. So at the team conference with the pharmacist, mental health [practitioner], and geriatrician, they all [provide] input at that point in time. Typically throughout the week, the geriatrician, mental health, and pharmacist do not access the POC. But the nurse practitioner and social worker then use that tool as an ongoing way to track implementation.’ |
| Patient involvement in care plan current state | ‘When we have our interdisciplinary team meeting we do invite patients and families to attend their particular rounding if they're able to do so and we are required to document patient family involvement in the plan, review it with them after the team meeting because the goals often will change [during the meeting], the discharge date or disposition often will change, so that patient involvement and engagement in that plan is absolutely a part of our work flow.’ | |
| Patient involvement in care plan ideal future state | ‘It could be great if we could somehow project it [the care plan] in the patient's room on the TV screen so they could actually see it and read it. A lot of adults learn better that way, visually, and kind of see what their goals were and have that opportunity to really engage and say no, I don't really think I can ambulate fifty feet by Friday, how about we start with thirty, or maybe, I think I can do a hundred feet can we push it up?’ | |
| Use of CCD to support team communication of care plan across setting | ‘Our care settings are outside of the incentive scope of Meaningful Use and HITECH, so we're not being paid to install systems that for example can handle a continuity of care document. But we recognize that that's important so we're working with our internally developed apps and with our purchased applications to have that capability and if the development plans hold up to have it by year end of this year, so that we will be able to receive a CCD when someone's admitted from an acute care setting, and to provide a CCD when they leave our organization and go on to the next care setting. Our expectation is that for starters this is going to be supplemental to the information that they're getting today, but as we learn both technically what we need to do and as we get feedback from upstream and downstream providers about what's necessary and what's technically doable, we expect that that data set will get richer over time.’ ‘We'll learn how good or not good that is and our intention is to work on it until we get it right. In some ways there's nothing that substitutes for a really good verbal communication and so it may be that, you know, two people at a distance looking at the same electronic [CCD] document and then talking about what's there and not there, and one having provided the care and the other one about to be providing the care with the patient. Hopefully that will be a robust and rich exchange that will really support a good handoff.’ |
|
| 2. Health Care Home (HCH) | Challenges related to lack of interoperability (emergency department to HCH) | ‘But the other piece that you were asking as far as communicating with the medical home, this is a big challenge for the emergency room with our current medical documentation in that when we discharge patients from the emergency room we don't routinely call their primary care providers and the office of the primary care provider receives a very rudimentary fax that basically just says your patient was here. Often they have little knowledge of what went on in the emergency room, what our thought process was, what we did for the patient, and it's a rare circumstance that they get a lot of information, and most providers don't have access to our medical records.’ |
| 3. Care Management | Siloed nature of care plans | ‘There is not one home for any unified care plan. There are many sub-care plans. There are many care plans with homes, but there is not one unified care plan across the system.’ |
| Potential benefits of care plan reconciliation and sharing | ‘For instance, let's say there was a diabetic and maybe they are able to do a percentage of their insulin, maybe they can draw it up but they can't inject or something of that nature… We may get a verbal communication about it. But it would be nice to know that they've met this goal and if [so], the next goal. And then we can say, “What's the teaching that we need to do on the home care side or maybe at the SNF level or whatever to then pick it up from there so they actually meet their ultimate goal.”’ | |
| Care plan current state best practice | ‘Current state is the family has a paper copy of their care plan; they are instructed to take it with them to any medical facility they visit. What future state would be is for them to identify ‘I have a care plan’ and that whoever, the pediatrician or the emergency room would be able to access that electronically.’ | |
| 4. Medication Management | Care plan reconciliation related to medication management | ‘So medication reconciliation is a huge part of the plan of care and coordination of care… So you have the tool to make sure the list is correct going in. It translates to the plan of care in patient-friendly language, and while that's not perfect yet, it's much better… So a lot of the use of electronic medical records to coordinate care, to make sure from the patient's perspective they have one list, and it's accurate, and they understand the changes.’ |
| 5. Health IT-Enabled Coordination | Limitations of current state health IT tools | ‘We're also doing chronic care management training with our clinicians. [This includes] a lot of things like telephone triaging, really looking at the patient and determining their specific goals. One of their goals may be to stay out of the hospital. There's a lot of those things, however none of it is really software driven, meaning the software doesn't have the logic to help with the decision making to help the clinician with any specific care plan or interventions or anything like that.’ |
| Use of patient portal | [Using the patient portal] The patient can say ‘These are my concerns coming in for my next visit,’ the provider can put some information in there, so it really is the beginning of this ongoing plan of care that hopefully will become seamless and be able to be integrated at some point in time into the inpatient record, if the patient is admitted due to whatever their concerns are, but it also allows us to have a seamless transition back, to have follow-up conversation on the portal.; | |
| Innovative solutions | ‘We've identified the need [for an LCP] we have a lot of innovation going on; for example—we'll use the problem list as a potential LCP. The problem is diabetes and it would list the goals of care. In addition there is some functionality in [the vendor-based EHR system], it says, “What are the patient's goals of care and background” and you can enter it into a field that is automatically pulled in.’ |
AHRQ, Agency for Healthcare Research and Quality; CCD, Continuity of Care Document; EHR, electronic health record; IT, information technology; LCP, longitudinal care plan; POC, plan of care; SNF, skilled nursing facility.
Teamwork focused on coordination
We defined teamwork as the degree to which interdisciplinary team members (including patients) were involved in forming and updating the care plan. At some sites, the care plan was used to document teamwork focused on care coordination targeting the patient's and the care team's goals. This was particularly true as part of research efforts within clinical organizations and where teams were focused on management of a specific population or disease process (eg, geriatrics, pediatrics, diabetes, and heart failure). There was universal recognition that both the patient and family caregivers should be included as fundamental members of the interdisciplinary team in the process of care plan generation and updating. However, we found that, in practice, patient/family involvement was often peripheral, and when present, often occurred as an additional step after the care plan had been already developed by the interdisciplinary team.
While the particular template used to document the care plan was generally site specific, one organization (interview #2) was implementing the Continuity of Care Document (CCD)40 for this purpose. Team members believed that use of this standard in conjunction with a verbal handoff would support communication of the care plan across settings.
Health care home
AHRQ defines the health care home (HCH) as a model of the organization of primary healthcare that is patient-centered, comprehensive, coordinated, accessible, and committed to quality.41 We found that communication of the care plan to the HCH as patients transitioned out of an inpatient facility was a challenge. Several organizations had policies in place that required a phone call to the HCH, but the degree to which this was executed was variable. Follow-up phone calls to patients to ensure recommended aftercare were a common strategy for connecting patients with their HCH. Participants from all sites talked about the communication challenges related to health IT and the lack of interoperability with HCHs.
Care management
AHRQ defines care management as processes, including case management and disease management, to assist patients in managing their conditions efficiently and effectively.42 Most participants reported that a care plan to support care management was generated at each site and that while the plan from the previous setting may serve as a reference, little or no care plan reconciliation occurred as a patient transitioned across settings. There was widespread recognition of the potential benefit of sharing and reconciling plans of care for patients with chronic illness. One site (interview #5) reported that a best practice for a small percentage of pediatric patients in a research setting included a paper-based care plan used across settings to improve coordination.
Medication management
We found that electronic and paper tools and interdisciplinary processes existed within many settings to support planning related to medication management. Providers from all settings described processes and tools in place to support medication reconciliation and some emphasized patient and family involvement in this process. One site was using a visit summary form that noted any medication changes (initiated/discontinued medications, dosing changes). High-risk patients were contacted at regular intervals after discharge to verify that they had their medications, that they were taking them, and to answer any questions. Another organization instituted calls for high risk patients at 1, 3, 5 and then again 30 days post discharge. This organization developed a new metric to track patient compliance that includes patients getting the medication from the pharmacy and completing the first 30-day supply. Another organization is using an avatar to reinforce medication teaching at discharge.
Health IT-enabled coordination
In general, participants described the limitations of health IT tools to support generation, update, and reconciliation of the care plan across transitions. While some electronic tools were in place, they were optimized for use within a single setting. There was a lack of interoperability of systems across settings. Coordination across settings required specially trained nurses or other providers to ensure that the appropriate information followed the patient. Some organizations used nurse liaisons to manually enter information from the inpatient record into the electronic referral system. We also heard about the limitations of the health IT tools in place with respect to clinical decision support and reflecting patient preferences. As a result, there is heavy use of telephone, email, and fax to maximize communication across settings.
Most regions had patient portals in place with varying degrees of functionality. The intent for these portals was to provide information and tools to promote patient activation related to maintaining and updating the care plan, to engage in visit planning, and to enhance communication with providers across settings. However, existing functionality was limited to prescription renewals, laboratory results, educational content, and basic communication with outpatient providers. Other approaches needed to activate the patient based on their care plan, such as texting, engagement with social media, and integration of personal devices to populate progress towards the individual’s health and wellness goals, were not reported.
Discussion
We investigated the current state of the use of LCPs and the degree to which use of the care plan in practice meets the definition of an LCP in healthcare settings in six US regions. While we did find evidence of care plan elements corresponding to each of the AHRQ Broad Approaches, the degree to which current state care plans support care coordination was limited. We found that the LCP is a commonly envisioned tool to support care coordination, but it was not used in practice. Overall, there was little consistency regarding how the care plan was defined across organizations and in general it was described as a set of processes conducted (often independently) by each discipline within a single setting to document patient and care team goals rather than as a dynamic set of workflows reconciled across settings for the purposes of identifying and achieving health and wellness goals along the spectrum of care. The organizations that participated in this evaluation are many of those that are viewed as high performing institutions with respect to health IT deployment, and even in these settings there is limited electronic exchange of care plan data elements. The limited data sent electronically outside acute care settings is not surprising, given that MU incentives for electronic data exchange are available only to ACH and ambulatory providers.27 28 While the standards for MU may lead to universal adoption of a set of care plan data elements, they represent a subset of the data required for an LCP and few incentives exist for adoption outside of acute care and ambulatory settings. The addition of data elements to represent patient preferences, follow-up plans related to patient goals, and the patient self-care management plan should be included in future stages of MU. As noted in table 3, acute hospital sites are sending some care plan data electronically with at least one hospital routinely sending one or more of the care plan data elements. The majority of ACHs reported that they routinely sent information related to the responsible clinician, patient problems, orders, allergies, and medications electronically. The additional data needed to support sharing and reconciliation of an LCP were less likely to be available electronically. No sites reported sending data related to patient likes and dislikes electronically, and the acute hospitals in our sample received none of the care plan data electronically from non-acute care sites. We noted from the group interviews was that while many ACHs were sending some care plan information electronically, these data were not typically standardized. Data were often exchanged in free text formats.
While an interdisciplinary care plan within a given healthcare facility is an essential foundation for a meaningful LCP that can transcend individual facilities, we found that interdisciplinary plans were not the norm. The tools (paper-based and electronic) developed for communication and documentation of the care plan were generally used independently by each discipline. Interdisciplinary care team members have access to care plan information documented by other disciplines, but coordinated views were rare and separate care plans, with distinct patient goals (sometimes overlapping, occasionally conflicting) existed within a single patient record.
The care plan tools were optimized for use within a single setting and there was limited functionality to support care plan reconciliation across settings. Care plan information was often transferred via paper and faxed documents and was generally not reconciled as patients transitioned from one setting to the next; rather, a new care plan was developed as part of the transition process. The degree to which the new plan was informed by the plan developed in the previous setting was variable. The overarching care plan structure as proposed by the S&I Framework, could potentially be leveraged in future stages of MU to provide a means to reconcile multiple provider-specific treatment plans and discipline-specific plans of care into one overarching, patient-centric care plan (eg, an LCP).
Occasionally in some settings, the care plan was available electronically but not universally. When electronic data were available, its primary purpose related to planning within a single setting and not for the purpose of care coordination across settings. When transferred as part of an electronic discharge summary, care plan data were often in a free text format and there was limited consistency as to which data elements were included. Interoperability was limited between electronic systems in use in different settings even within the same healthcare system. Specially trained staffs were often required to manually transfer data and information from one electronic system to another so that providers in the next level of care would have access to the information that they needed to care for a patient. This lack of interoperability has implications associated with the manual processes including the potential for inaccurate information transfer and possibility that the selective transfer of information may create new patient safety risks. Moreover, the resource intensiveness of manual abstraction is not likely to be sustainable or scalable to limited resource environments.
Based on our interviews, the patient’s current role in the care plan development and update process was found to be limited, and when present, was generally peripheral to the interdisciplinary generation and update processes. We did note two examples of best practices. In the first example, the Consolidated CCD (C-CCD) was being implemented to support care coordination and care plan reconciliation across settings (interview #2). Processes existed within this organization to involve patients and family in the generation and update of the care plan and the organization planned to provide patients with a consumer version of the C-CCD. Once fully implemented, the C-CCD will include an LCP and may provide a model that can be adopted by other organizations. In a second example, a paper care plan used in a pediatric research setting was developed with the patient and family (interview #5). The family was instructed to take it with them any time they visit a provider or medical facility. While their ideal future state is to have the care plan available electronically, the paper version does support care coordination across settings and provides a ‘low tech’ solution that can be used as organizations transition from paper-based to electronic systems.
This work has several limitations. The participating sites represent a small sample of healthcare settings across the USA. The sites included are known to be technologically advanced and may not be representative of the majority of US healthcare settings. In addition, there are limitations associated with the qualitative approach used. A single interview was completed in each region, so we were unable to verify our assessment of each institution. The perspectives gained may selectively describe the experience of distinct provider types or certain patient types that require ACH, HHA, or SNF services. In addition, the use of a priori codes for the qualitative interviews raises the possibility that important unanticipated themes, raised during the group interviews, were missed.
Conclusions
We evaluated leading healthcare delivery organizations and found little to no current use of LCPs and numerous hurdles precluding the use of health IT to enable the idealized vision of the LCP. We found that while a care plan was frequently used in conjunction with the AHRQ Broad Approaches, that the degree to which its use in practice functions as an LCP to support transitions and achievement of an individual's health and wellness goals across settings is limited. A care plan that is used by all disciplines within individual settings was often lacking and this is a fundamental barrier to achieving an LCP that can transcend individual facilities. The ultimate value of the LCP will be demonstrated with improved patient experience (quality, satisfaction), cost, and population outcomes,43 but this requires an LCP that leverages electronic systems to dynamically pull together the various elements to create appropriate and actionable views for providers and/or patients. However, we found that even in these technologically advanced organizations, that the lack of interoperability of the care plan data elements translates into very low ‘organizational readiness’ for the LCP. Until standardized, structured, electronic LCP data elements and value sets are routinely captured within individual settings and exchanged across all settings, it is not possible to realize potential benefits. Strategies are needed to transform the LCP from an idealized tool into a reality. Future studies across integrated care delivery networks using LCP messaging tools (such as the C-CCD) to exchange standardized LCP elements are needed to evaluate impact. Widespread adoption of the LCP may require a rebranding and marketing with a toolset that will make it easy for all care team members (including patients) to integrate the LCP into existing workflows. A common set of LCP standards for adoption across settings and interoperability between systems are essential. The definitions and use cases developed by the S&I Framework provide a starting point. Tools, practices, and processes to enable care plan reconciliation all still need to be further developed. In addition, studies are needed to obtain the patient and family perspectives on the LCP and their role in achieving this vision. Once in place, the LCP can be used across the Broad Approaches as a tool to improve coordination, to support patient and family engagement in the process, and to ultimately accomplish the Triple Aim.43
Footnotes
Contributors: PCD, LS, ACH, and DWB developed the interview guide; PCD, LS, and LAV conducted the group interviews; and PCD, LS, and ACH conducted the qualitative analysis. All authors contributed to drafting or revising the article.
Funding: This work is based on material that was prepared under, and paid for by, the Centers for Medicare & Medicaid Services (CMS) under Contract #HHSM-500-2009-00010C.
Competing interests: None.
Ethics approval: The Partners HealthCare IRB approved this study.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Durbin J, Barnsley J, Finlayson B, et al. Quality of communication between primary health care and mental health care: an examination of referral and discharge letters. J Behav Health Serv Res 2012;39:445–61 [DOI] [PubMed] [Google Scholar]
- 2.Davis MM, Devoe M, Kansagara D, et al. “Did I do as best as the system would let me?” Healthcare professional views on hospital to home care transitions. J Gen Intern Med 2012;27:1649–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.King BJ, Gilmore-Bykovskyi AL, Roiland RA, et al. The consequences of poor communication during transitions from hospital to skilled nursing facility: a qualitative study. J Am Geriatr Soc 2013;61:1095–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hesselink G, Schoonhoven L, Plas M, et al. Quality and safety of hospital discharge: a study on experiences and perceptions of patients, relatives and care providers. Int J Qual Health Care 2013;25:66–74 [DOI] [PubMed] [Google Scholar]
- 5.Jeffs L, Kitto S, Merkley J, et al. Safety threats and opportunities to improve interfacility care transitions: insights from patients and family members. Patient Prefer Adherence 2012;6:711–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cortelyou-Ward K, Swain A, Yeung T. Mitigating error vulnerability at the transition of care through the use of health IT applications. J Med Syst 2012;36:3825–31 [DOI] [PubMed] [Google Scholar]
- 7.Callen J, Paoloni R, Li J, et al. Perceptions of the effect of information and communication technology on the quality of care delivered in emergency departments: a cross-site qualitative study. Ann Emerg Med 2013;61:131–44 [DOI] [PubMed] [Google Scholar]
- 8.Moy NY, Lee SJ, Chan T, et al. Development and sustainability of an inpatient-to-outpatient discharge handoff tool: a quality improvement project. Jt Comm J Qual Patient Saf 2014;40:219–27 [DOI] [PubMed] [Google Scholar]
- 9.Cherescavich G. A shared nursing care plan. Am J Nurs 1959;59:202. [PubMed] [Google Scholar]
- 10.Elsom KO. Elements of the medical process. Their place in medical care planning. JAMA 1971;217:1226–32 [PubMed] [Google Scholar]
- 11.Knox E, Acheson R, Anderson D, et al. Epidemiology in health care planning: a guide to the uses of a scientific method. Oxford, UK: Oxford University Press, 1979 [Google Scholar]
- 12.Bronow RS, Beltran RA, Cohen SC, et al. The Physicians Who Care plan. Preserving quality and equitability in American medicine. JAMA 1991;265:2511–15 [PubMed] [Google Scholar]
- 13.Wood MM. Guide to better care …a nursing plan. Am J Nurs 1961;61:61–2 [PubMed] [Google Scholar]
- 14.Blinder VS, Norris VW, Peacock NW, et al. Patient perspectives on breast cancer treatment plan and summary documents in community oncology care: a pilot program. Cancer 2013;119:164–72 [DOI] [PubMed] [Google Scholar]
- 15.Parry C, Kent EE, Forsythe LP, et al. Can't see the forest for the care plan: a call to revisit the context of care planning. J Clin Oncol 2013;31:2651–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paterson JM, Allega RL. Improving communication between hospital and community physicians. Feasibility study of a handwritten, faxed hospital discharge summary. Discharge Summary Study Group. Can Fam Physician 1999;45:2893–9 [PMC free article] [PubMed] [Google Scholar]
- 17.Gore DC, Powell JM, Baer JG, et al. Crew resource management improved perception of patient safety in the operating room. Am J Med Qual 2010;25:60–3 [DOI] [PubMed] [Google Scholar]
- 18.Sullivan F, Wilson P. The completeness and accuracy of patient record transfer between practices. Health Bull 1997;55:16–19 [PubMed] [Google Scholar]
- 19.Terrell KM, Miller DK. Strategies to improve care transitions between nursing homes and emergency departments. J Am Med Dir Assoc 2011;12:602–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zamora Z, McCall B, Patel L, et al. Implementation of a web-based system to improve the transitional care of older adults. J Nurs Care Qual 2012;27:182–9 [DOI] [PubMed] [Google Scholar]
- 21.Lamson L, Carver F. Nursing care plan not dead yet. Am J Nurs 1991;91:211897586 [Google Scholar]
- 22.Motamedi SM, Posadas-Calleja J, Straus S, et al. The efficacy of computer-enabled discharge communication interventions: a systematic review. BMJ Qual Saf 2011;20:403–15 [DOI] [PubMed] [Google Scholar]
- 23.Balaban RB, Weissman JS, Samuel PA, et al. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med 2008;23:1228–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.LaMantia MA, Scheunemann LP, Viera AJ, et al. Interventions to improve transitional care between nursing homes and hospitals: a systematic review. J Am Geriatr Soc 2010;58:777–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.CMS. Medicare and Medicaid programs; electronic health record incentive program—stage 2 proposed rule. Washington, DC: Centers for Medicare & Medicaid Services, 2012 [Google Scholar]
- 26.S&I Framework. Longitudinal Coordination of Care Interoperable Care Plan Exchange Use Case v2.0. 2013. http://wiki.siframework.org/file/view/LCC%20Care%20Plan%20Exchange%20Use%20Case%20Finalv2.pdf/451850044/LCC%20Care%20Plan%20Exchange%20Use%20Case%20Finalv2.pdf (accessed 19 Oct 2013).
- 27.HHS.gov. Medicare and medicaid programs; electronic health record incentive program—stage 2. Fed Regist 2012;77:53967–4162 [PubMed] [Google Scholar]
- 28.CMS. HITPC stage 3 request for comment. Washington, DC: Department of Health and Human Services, 2013 [Google Scholar]
- 29.Darmer MR, Ankersen L, Nielsen BG, et al. Nursing documentation audit—the effect of a VIPS implementation programme in Denmark. J Clin Nurs 2006;15:525–34 [DOI] [PubMed] [Google Scholar]
- 30.Dellefield ME. Interdisciplinary care planning and the written care plan in nursing homes: a critical review. Gerontologist 2006;46:128–33 [DOI] [PubMed] [Google Scholar]
- 31.Hayrinen K, Lammintakanen J, Saranto K. Evaluation of electronic nursing documentation-Nursing process model and standardized terminologies as keys to visible and transparent nursing. Int J Med Inform 2010;79:554–64 [DOI] [PubMed] [Google Scholar]
- 32.Keenan G, Yakel E, Tschannen D, et al. Documentation and the nurse care planning process. In: AHRQ, ed. Patient safety and quality an evidence-based handbook for nurses. Rockville, MD: Agency for Healthcare Research and Quality, 2008:1–40 [PubMed] [Google Scholar]
- 33.McDonald KM, Schultz E, Chapman T, et al. Prospects for care coordination measurement using electronic data sources (Prepared by Stanford University under subcontract to Battelle on Contract No. 290-04-0020—AHRQ SQI-II.). Rockville, MD: Agency for Healthcare Research and Quality, 2012 [Google Scholar]
- 34.TJC. The Joint Commission E-dition. Hospital 2010 2010. http://www.jointcommission.org/assets/1/6/hospital_pre-pubs_for_cop_changes_20110110.pdf (accessed 1 May 2012).
- 34a. McDonald KM, Schultz E, Albin L, et al. Care Coordination Atlas Version 3 (Prepared by Stanford University under subcontract to Battelle on Contract No. 290-04-0020). AHRQ Publication No. 11-0023-EF. Rockville, MD: Agency for Healthcare Research and Quality. November 2010.
- 35.S&I Framework. Long Term Care Post Acute Care. 2013. http://wiki.siframework.org/LCC+Long-Term+Post-Acute+Care+(LTPAC)+Transition+SWG (accessed 4 Mar 2013).
- 36.HHS. Health information technology: standards, implementation specifications, and certification criteria for electronic health record technology, 2014 edition; revisions to the permanent certification program for health information technology; proposed rule. Fed Regist 2012;p 77. http://www.gpo.gov/fdsys/pkg/FR-2012-09-04/pdf/2012-20982.pdf [PubMed] [Google Scholar]
- 37.NVivo qualitative data analysis software [computer program]. Version 10: QSR International Pty Ltd; 2012
- 38.Miles M, Huberman A. Qualitative data analysis: an expanded sourcebook. 2nd edn. Thousand Oaks: Sage, 1994 [Google Scholar]
- 39.Kearney MH. Levels and applications of qualitative research evidence. Res Nurs Health 2001;24:145–53 [DOI] [PubMed] [Google Scholar]
- 40.Framework SI. Companion Guide to Consolidated CDA for MU2. 2013. http://wiki.siframework.org/Companion+Guide+to+Consolidated+CDA+for+MU2 (accessed 30 Jul 2013).
- 41.AHRQ. Patient Centered Medical Home Resource Center. 2011. http://pcmh.ahrq.gov/portal/server.pt/community/pcmh__home/1483/what_is_pcmh_ (accessed 14 Sep 2013).
- 42.McDonald K, Schultz E, Albin L, et al. Care coordination atlas version 3. Rockville, MD: Agency for Healthcare Research and Quality, 2010. AHRQ Publication No.11-0023-EF [Google Scholar]
- 43.Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff 2008;27:759–69 [DOI] [PubMed] [Google Scholar]