Abstract
Background
Water pipe (hookah) smoking has become a common activity in Germany, particularly among adolescents and young adults; in 2011, its lifetime prevalence was as high as 68.8%. Similar trends can be seen in other European countries. Water-pipe smokers are exposed to the same health-endangering substances as cigarette smokers, and the inhaled amount of carbon monoxide (CO) can be as much as ten times as high. In CO intoxication, carboxyhemoglobin is formed and causes direct injury at the cellular level, leading to hypoxia and nonspecific neurological manifestations. There have only been ten reported cases around the world of CO intoxication due to the use of a water pipe, and none of these were fatal. It should be recalled, however, that accidental CO intoxication is common and is associated with high morbidity and mortality.
Case presentation and course
We present a series of four young adults, aged 16 to 21, three of whom were hospitalized because of transient unconsciousness. The carboxyhemoglobin (CO-Hb) content of the blood in the symptomatic patients ranged from 20.1% to 29.6%, while the asymptomatic patient had a CO-Hb content of 16.7%. Water-pipe smoking was the cause of CO intoxication in all four cases. The CO-Hb values were successfully brought down by the administration of highly concentrated oxygen and all patients were discharged in asymptomatic condition.
Conclusion
This case series reveals that CO intoxication due to water-pipe smoking is probably more common than is generally realized. Emergency room staff should be aware of this problem and inquire specifically about water-pipe smoking in patients with nonspecific neurological manifestations.
Hookah smoking is becoming increasingly popular among adolescents and young adults, including in the West (1). For 2011 lifetime prevalence figures of up to 68.8% were recorded for young German adults (1).
There are many reasons for this increase, including migration (1), youth subculture (2), and the widespread misconception that hookah smoking is a healthier nicotine intake method than cigarettes (3).
Syncope often results in emergency hospital admission and has a broad spectrum of associated differential diagnoses (4, 5). Although the term "syncope” does have a precise definition (6), there is a great deal of uncertainty regarding its use in connection with intoxication in both clinical practice and the international literature. To avoid the confusion surrounding the definition of syncope, the term "transient loss of consciousness” is used in this case report.
The report describes a series of four cases in which patients suffered hookah-induced carbon monoxide poisoning (CO intoxication). In three of the four cases, poisoning manifested as transient loss of consciousness.
Following absorption via the lungs, carbon monoxide (CO) leads to the formation of carboxyhemoglobin and a left shift of the oxygen dissociation curve. This results in hypoxia, which is exacerbated by the interaction of carbon monoxide with cytochromes of the mitochondrial respiratory chain (7).
Although hookah smoking is widespread, the medical literature contains only a small number of case reports. A large hidden number of cases is therefore suspected.
The case series follows the CARE guidelines for medical case reports (8). It aims both to debunk the myth that hookah use is harmless and to raise the awareness of emergency doctors on the other hand, in order for carbon monoxide poisoning to be considered in young adults with recurrent transient loss of consciousness.
Case descriptions
Case 1:
A 16-year-old male patient was brought to the emergency room by paramedics following transient loss of consciousness. His medical history was normal. He stated that he had taken neither recreational drugs nor medication.
Two hours earlier, the patient had smoked a hookah with friends. He then became nauseous. He felt hot and began to breathe more rapidly. On his way home he collapsed and was unconscious for a short period.
Information from other individuals revealed no evidence of an epileptogenic event, clinical examination was normal, and there was no evidence of any focal neurological deficits. Laboratory tests showed no abnormalities. ECG revealed incomplete right bundle branch block.
Arterial blood gas analysis showed an FCOHb level of 20.1% (normal range 0 to 5%, maximum 10% in heavy smokers). The patient was administered high-dose oxygen (more than 10 L/min) via a non-rebreather mask. After two hours the patient’s FCOHb level was 4.8% and he was discharged home with no further manifestations.
Case 2:
An 18-year-old female patient was brought to the emergency room by paramedics following transient loss of consciousness. Her medical history was normal. She stated that she had taken neither recreational drugs nor medication.
Before this event the patient had been smoking a hookah with friends in a hookah lounge for approximately one hour. When she left the lounge she experienced a severe headache and paresthesia. Her vision was also blurred, and she finally collapsed and lost consciousness.
When paramedics arrived the patient’s circulation was stable and she was assigned a score of three on the Glasgow Coma Scale (GCS). The recorded loss of consciousness lasted approximately 15 minutes. On arrival at the emergency room she was given a GCS score of 15. Her circulation was stable and both clinical and neurological status seemed normal. There was no evidence of an epileptogenic event. ECG revealed no abnormalities. Cranial CT ruled out hemorrhage.
Arterial blood gas analysis showed an FCOHb level of 25.7% and she was administered high-dose (above 10 L/min) oxygen via a non-rebreather mask. When her FCOHb value reached 7% four hours later, the patient was discharged home with no further manifestations.
Case 3:
A 17-year-old female patient accompanied her friend (case 2) to the emergency room. She had also smoked a hookah in the hookah lounge. Although she had no manifest problems, on learning of her friend’s diagnosis she was afraid of also having carbon monoxide poisoning.
Arterial blood gas analysis was performed and showed an FCOHb level of 16.7%. Although she had no manifest problems, she was also administered high-dose (above 10 L/min) oxygen via a non-rebreather mask. Four hours later her FCOHb level was 5% and she was discharged home, still with no manifest problems.
Case 4:
A 21-year-old male patient was brought to the emergency room by paramedics following recurrent transient loss of consciousness. His medical history was normal. He stated that he had taken neither recreational drugs nor medication.
The patient had been smoking a hookah for several hours while visiting friends. Afterwards he complained of nausea and headaches. When he collapsed on his way home and subsequently lost consciousness three times, his friends contacted the emergency services.
In the emergency room he presented with stable circulation and was assigned a GCS score of 15. He reacted slowly and lethargically while his clinical history was being taken. His leading symptom was headache. Clinical and neurological examination revealed no abnormalities and his ECG was normal. There was no evidence of an epileptogenic event.
After arterial blood gas analysis showed an FCOHb level of 29.6%, he was administered high-dose (above 10 L/min) oxygen via a non-rebreather mask. Two hours later his FCOHb level was 8.4% and both his headache and his lethargy had resolved. The patient was therefore discharged home with no further manifestations.
The main findings are summarized in Table 1.
Table 1. Main findings of case series of carbon monoxide poisoning following hookah smoking.
| Patient | Age | Sex | Background of migration*1 | Leading symptom*2 | COHb (%) on admission | O2 therapy*3 | COHb (%) on discharge | Delayed effects*4 |
|---|---|---|---|---|---|---|---|---|
| 1 | 16 | M | No | Loss of consciousnes | 20.1 | Yes | 4.8 | No |
| 2 | 18 | F | Yes | Loss of consciousness | 25.7 | Yes | 7 | No |
| 3 | 17 | F | Yes | None | 16.7 | Yes | 5 | No |
| 4 | 21 | M | Yes | Loss of consciousness | 29.6 | Yes | 8.4 | No |
*1 All patients are of Caucasian ethnicity. In three of the four cases the patients’ parents were born in Southeastern Europe
*2 Information obtained from patients and others, e.g. paramedics’ records
*3 Oxygen at atmospheric pressure using high flow (>10 L) via a non-rebreather mask
*4 Information obtained during a telephone interview six to twelve months after hospital admission
Discussion
Carbon monoxide (CO) is a colorless, odorless gas produced during the incomplete combustion of hydrocarbons. Carbon monoxide poisoning is Germany’s leading cause of accidental poisoning, accounting for approximately 3700 hospital admissions and around 370 fatalities per year (9). Although it is most commonly caused by smoke inhalation from fires, accidental carbon monoxide poisoning has also been reported in connection with fireplaces, hot water boilers, and charcoal table barbecues (9).
Following inhalation, carbon monoxide diffuses rapidly across the alveolar membrane and binds reversibly—with 240 times the affinity of oxygen—to divalent heme iron, forming carboxyhemoglobin (COHb). Allosteric conformational change shifts the oxygen dissociation curve to the left. At the cellular level, the binding of CO to the cytochrome leads to dysfunction of the respiratory chain in the mitochondria. Formation of reactive oxygen species gives rise to neuronal and myocardial necrosis and apoptosis (10, 11).
There is only a weak correlation between symptoms of acute carbon monoxide poisoning and COHb level; symptoms are better correlated with duration of exposure. In addition to nonspecific symptoms such as fatigue, nausea, and headaches, there is also a possibility of loss of consciousness, seizures, cardiac arrhythmia, myocardial ischemia, and death (7). In addition, the severity of toxicity is determined essentially by preexisting comorbidities (cardiovascular diseases, pulmonary diseases, anemia) and age. Age over 65 is associated with the highest mortality (12).
Carbon monoxide poisoning causes both immediate neurological symptoms and delayed neuropsychological effects. The latter can develop even after an asymptomatic latency phase lasting several weeks, and some can be long-term (13, 14). Symptoms that have been described range from mild cognitive effects (memory and concentration problems) via affective disorders (depression, anxiety disorders) through to gait and balance disorders, tremor, and loss of hearing in rare cases (15).
Approximately 100 million people smoke hookahs worldwide, particularly in North Africa and the Arab world (16). However, in Germany too, hookahs—also referred to as water pipes, narghiles, arghilas, shishas, and Hubble Bubble—are becoming increasingly popular among adolescents and young adults. This is because they are thought to provide "healthier” nicotine exposure than cigarettes (1, 3). Physicians face new challenges in the form of altered consumption behavior and a variety of new designer drugs, the manufacture of which exploits legal loopholes by processing existing substances (e.g. synthetic cannabinoids, known as "spice”) (17).
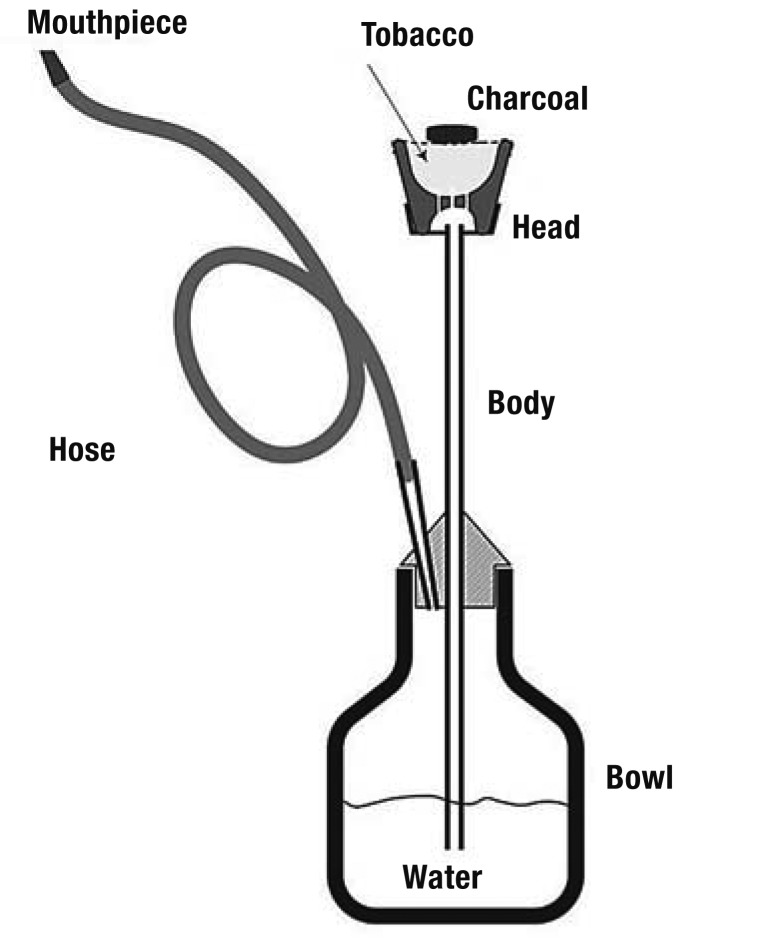
A hookah consists of a glass water container, a clay or metal tobacco bowl, a pipe stem, and a hose with a mouthpiece. A sheet of perforated aluminum foil is placed on the clay or metal tobacco bowl, and a piece of burning charcoal is placed on the foil. Inhaling through the hose draws smoke through the water container and into the mouth of the smoker (Figure).
Figure.
Schematic representation of a hookah
(from: Cobb CO, et al.: Acute toxicant exposure and cardiac autonomic dysfunction from smoking a single narghile waterpipe with tobacco and with a "healthy” tobacco-free alternative. Toxicol Lett 2012; 215: 70–5. Reproduced with the kind permission of Elsevier, Oxford)
In actual fact, hookah smoking gives rise to the same harmful substances as cigarette smoking (in particular tar, nicotine, and carbon monoxide) (19). In addition to the type of tobacco used and the different temperatures at the combustion area, there are qualitative and quantitative differences in inhaled toxins, caused in particular by the differing duration of inhalation (approximately five minutes for cigarettes and 50 for hookahs). It should be stressed that both conventional tobacco blends and alternative, nicotine-free herb blends differ only in their nicotine content, not in the quantities of other toxic substances (carbon monoxide, tar, polycyclic hydrocarbons) inhaled (18, 20). As a result of the combustion of charcoal, a hookah smoker inhales more than 10 times more carbon monoxide than a cigarette smoker (19).
Table 2 provides an overview of all case reports of carbon monoxide poisoning associated with hookah use published in PubMed up to July 2014.
Table 2. Published case reports of carbon monoxide poisoning following hookah smoking.
| Author | Year | Country | No. of cases | Patient age | Leading symptoms | COHb (%) | Treatment |
|---|---|---|---|---|---|---|---|
| Lim et al. (21) | 2009 | Singapore | 1 | 19 | Dizziness | 27.8 | Oxygen at atmospheric pressure |
| Uyanýk et al. (22) | 2009 | Turkey | 1 | 25 | Headache, vomiting, dizziness | 28.7 | Oxygen at atmospheric pressure |
| Cavus et al. (23) | 2010 | Turkey | 1 | 25 | Loss of consciousness | 31.1 | Oxygen at atmospheric pressure |
| Arziman et al. (24) | 2011 | Turkey | 5 | 17 to 27 | 3 × nausea, dizziness, 1 × loss of consciousness | 11.4 to 24.3 | Oxygen at atmospheric pressure |
| La Fauci et al. (25) | 2011 | Italy | 1 | 16 | Confusion | 24 | Hyperbaric oxygen |
| Clarke et al. (26) | 2012 | UK | 11 | 17 to 34 | Headache, dizziness | 7.3 to 21 | Oxygen at atmospheric pressure |
| Ashurst et al. (27) | 2012 | USA | 1 | 21 | Vomiting, loss of consciousness | 15.3 | Oxygen at atmospheric pressure |
| Karaca et al. (28) | 2013 | Turkey | 1 | 20 | Loss of consciousness | 31.1 | Oxygen at atmospheric pressure |
| Ozkan et al. (29) | 2013 | Turkey | 1 | 19 | Loss of consciousness | 32.7 | Oxygen at atmospheric pressure |
| Bens et al. (30) | 2013 | The Netherlands | 3 | * | Dizziness, headache | 5.7 to 22 | Oxygen at atmospheric pressure |
Search terms: narghile, waterpipe, shisha, carboxyhemoglobin, carbon monoxide, poisoning, syncope
Database: Medline as of July 2014
*Not apparent from abstract. Article in Dutch
The dates and geographical distribution of the case reports (no cases before 2009, two in 2009, one in 2010, two in 2011, two in 2012, three in 2013; six case reports in the Middle East/Southeast Asia, four in Europe/the USA) may reflect the prevalence and increasing incidence of hookah smoking, as well as increasing awareness among physicians. The symptoms most frequently described are nonspecific and include headache, dizziness, nausea, and vomiting; five cases of transient loss of consciousness have also been recorded in connection with hookah smoking. With one exception, all patients were treated with oxygen at atmospheric pressure via a non-rebreather mask.
No follow-up was performed in any of the cases described. However, in one case prolonged neurological complaints such as dizziness and headaches were reported over a period of several weeks (30).
Although there have not yet been any recorded cases of fatal carbon monoxide poisoning following hookah use, carbon monoxide poisoning is one of the leading causes of fatal accidental poisoning worldwide (31). Because its spectrum of clinical symptoms is broad and nonspecific, diagnosis is often subject to substantial delay.
As the photometric absorption of COHb is similar to that of oxyhemoglobin, COHb cannot be detected using standard pulsoximetry. Carbon monoxide poisoning can therefore only be confirmed by venous or arterial blood gas analysis.
Treatment options include high-concentration oxygen via a non-rebreather mask and hyperbaric oxygen therapy in a pressure chamber. The former allows administration of 90% FiO2 using high flow (10 to 15 L/min), provided the fit of the mask is airtight (32). The half-life of COHb can be reduced from three to four hours in ambient air (21% O2) to 40 to 80 minutes using a non-rebreather mask, or 15 to 30 minutes in hyperbaric conditions (2.5 bar) (33).
As mentioned above, initial COHb level is only weakly correlated with both the severity of symptoms and delayed neurological/neuropsychiatric effects. In addition, different studies have different inclusion and exclusion criteria. The studies currently available therefore provide a heterogeneous range of opinions concerning the best treatment (34, 35). As high-concentration oxygen is safe, universally available, and cost-effective, while hyperbaric therapy can cause complications (barotrauma, perforated eardrum, seizure, air embolism), the latter should be reserved for patients with severe symptoms and for carbon monoxide poisoning during pregnancy (13, 35).
Conclusion
As hookah smoking is widespread, and the observation period in this case report was short (four cases in six months), it is suspected that many cases of carbon monoxide poisoning following hookah use remain hidden. The majority of those affected are probably not admitted to a hospital because their symptoms are nonspecific. In addition, the fact that high COHb levels can be found even in completely asymptomatic patients (see case 3) demonstrates the dangerous and unpredictable nature of carbon monoxide poisoning.
In this case series 75% of patients had a background of migration. A possible association has already been described in the literature (1, 36) and may be due to differing smoking habits in different cultures.
All patients were asked about any delayed effects during a telephone interview conducted in July 2014. In particular, they were asked about neurological/neuropsychological symptoms such as headache, dizziness, vision problems, concentration problems, forgetfulness, and depression. With the exception of patient two, who had suffered respiratory difficulties for several weeks, all the patients reported that they had had absolutely no symptoms following their event.
Although this case series did not provide any evidence of delayed neurological consequences, swift diagnosis and treatment is extremely important in cases of carbon monoxide poisoning.
Oxygen therapy at atmospheric pressure seems to be a cost-effective, safe, effective treatment in emergency care.
This case series provides evidence that the number of cases of carbon monoxide poisoning in connection with hookah smoking is underestimated. This should prompt emergency admission staff to ask targeted questions regarding hookah smoking for patients with nonspecific neurological symptoms.
Key Messages.
Hookah smoking gives rise to the same harmful substances as cigarette smoking. The inhaled quantity of carbon monoxide (CO) can actually be up to 10 times greater.
Hookah smoking can lead to significant carbon monoxide poisoning. Clinically, it can be associated with transient loss of consciousness.
Because the photometric absorption spectrum of carboxyhemoglobin is similar to that of oxyhemoglobin, carbon monoxide poisoning can only be confirmed using a special pulsoximeter or by venous or arterial blood gas analysis.
Swift administration of high-dose (>10 L/min) oxygen via a non-rebreather mask is a cost-effective, safe, effective treatment. In patients with severe symptoms and for carbon monoxide poisoning during pregnancy, therapy in hyperbaric conditions should be considered as a treatment option.
In cases of non-specific neurological symptoms, targeted questions should be asked regarding hookah smoking, and carbon monoxide poisoning should be ruled out using blood gas analysis.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Bundeszentrale für gesundheitliche Aufklärung. Die Drogenaffinität Jugendlicher in Deutschland 2011. Bundeszentrale für gesundheitliche Aufklärung. 2012:40–58. [Google Scholar]
- 2.Chaouachi K. Hookah (Shisha, Narghile) smoking and environmental tobacco smoke (ETS) A critical review of the relevant literature and the public health consequences. Int J Environ Res Public Health. 2009;6:798–843. doi: 10.3390/ijerph6020798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith-Simone S, Maziak W, Ward KD, Eissenberg T. Waterpipe tobacco smoking: knowledge, attitudes, beliefs, and behavior in two US. samples. Nicotine Tob Res. 2008;10:393–398. doi: 10.1080/14622200701825023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Güldner S, Langada V, Popp S, Heppner HJ, Mang H, Christ M. Patients with syncope in a German emergency department: Description of patients and processes. Dtsch Arztebl Int. 2012;109:58–65. doi: 10.3238/arztebl.2012.0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Greve Y, Geier F, Popp S, et al. The prevalence and prognostic significance of near syncope and syncope—a prospective study of 395 cases in an emergency department (the SPEED Study) Dtsch Arztebl Int. 2014;111:197–204. doi: 10.3238/arztebl.2014.0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kapoor WN. Syncope. N Engl J Med. 2000;343:1856–1862. doi: 10.1056/NEJM200012213432507. [DOI] [PubMed] [Google Scholar]
- 7.Weaver LK. Clinical practice Carbon monoxide poisoning. N Engl J Med. 2009;360:1217–1225. doi: 10.1056/NEJMcp0808891. [DOI] [PubMed] [Google Scholar]
- 8.Gagnier JJ, Riley D, Altman DG, Moher D, Sox H, Kienle GS for the CARE group. The CARE guidelines: Consensus-based clinical case reporting guideline development. Dtsch Arztebl Int. 2013;110:603–608. doi: 10.3238/arztebl.2013.0603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaiser G, Schaper A. Akute Kohlenmonoxidvergiftung. Notfall + Rettungsmedizin. 2012;15:429–435. [Google Scholar]
- 10.Jaffe FA. Pathogenicity of carbon monoxide. Am J forensic Med Pathol Off Publ Natl Assoc Med Exam. 1997;18:406–410. doi: 10.1097/00000433-199712000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Henry CR, Satran D, Lindgren B, Adkinson C, Nicholson CI, Henry TD. Myocardial injury and long-term mortality following moderate to severe carbon monoxide poisoning. JAMA. 2006;295:398–402. doi: 10.1001/jama.295.4.398. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC) Unintentional Non-Fire-related carbon monoxide exposures—United States, 2001-2003. Morb Mortal Wkly Rep. 2005;54:36–39. [PubMed] [Google Scholar]
- 13.Dries DJ, Endorf FW. Inhalation injury: epidemiology, pathology, treatment strategies. Scand J Trauma Resusc Emerg Med. 2013;21 doi: 10.1186/1757-7241-21-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lader M. Neuro-psychiatric complications of carbon monoxide poisoning. Curr Med Lit - Psychiatry. 2009;20:1–7. [Google Scholar]
- 15.Pepe G, Castelli M, Nazerian P, et al. Delayed neuropsychological sequelae after carbon monoxide poisoning: predictive risk factors in the Emergency Department A retrospective study. Scand J Trauma Resusc Emerg Med. 2011;19 doi: 10.1186/1757-7241-19-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Asfar T, Ward KD, Eissenberg T, Maziak W. Comparison of patterns of use, beliefs, and attitudes related to waterpipe between beginning and established smokers. BMC Public Health. 2005;5 doi: 10.1186/1471-2458-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weilemann LS. Droge ist nicht gleich Droge. Med Klin Intensivmed Notfmed. 2013;108:484–490. doi: 10.1007/s00063-013-0219-1. [DOI] [PubMed] [Google Scholar]
- 18.Cobb CO, Sahmarani K, Eissenberg T, Shihadeh A. Acute toxicant exposure and cardiac autonomic dysfunction from smoking a single narghile waterpipe with tobacco and with a "healthy” tobacco-free alternative. Toxicol Lett. 2012;215:70–75. doi: 10.1016/j.toxlet.2012.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shihadeh A, Saleh R. Polycyclic aromatic hydrocarbons, carbon monoxide, "tar”, and nicotine in the mainstream smoke aerosol of the narghile water pipe. Food Chem Toxicol. 2005;43:655–661. doi: 10.1016/j.fct.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 20.Shihadeh A, Salman R, Jaroudi E, et al. Does switching to a tobacco-free waterpipe product reduce toxicant intake? A crossover study comparing CO, NO, PAH, volatile aldehydes, "tar” and nicotine yields. Food Chem Toxicol. 2012;50:1494–1498. doi: 10.1016/j.fct.2012.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lim L, Lim GH, Seow E. Case of carbon monoxide poisoning after smoking shisha. Int J Emerg Med. 2009;2:121–122. doi: 10.1007/s12245-009-0097-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Uyanýk B, Arslan ED, Akay H, Erçelik E, Tez M. Narghile (hookah) smoking and carboxyhemoglobin levels. J Emerg Med. 2011;40 doi: 10.1016/j.jemermed.2009.05.032. [DOI] [PubMed] [Google Scholar]
- 23.Cavus UY, Rehber ZH, Ozeke O, Ilkay E. Carbon monoxide poisoning associated with narghile use. Emerg Med J. 2010;27 doi: 10.1136/emj.2009.077214. [DOI] [PubMed] [Google Scholar]
- 24.Arziman I, Acar YA, Yildirim AO, et al. Five cases of carbon monoxide poisoning due to narghile (shisha) Hong Kong J Emerg Med. 2011;18:255–257. [Google Scholar]
- 25.La Fauci G, Weiser G, Steiner IP, Shavit I. Carbon monoxide poisoning in narghile (water pipe) tobacco smokers. CJEM. 2012;14:57–59. doi: 10.2310/8000.2011.110431. [DOI] [PubMed] [Google Scholar]
- 26.Clarke SFJ, Stephens C, Farhan M, et al. Multiple patients with carbon monoxide toxicity from water-pipe smoking. Prehosp Disaster Med. 2012;27:612–614. doi: 10.1017/S1049023X12001227. [DOI] [PubMed] [Google Scholar]
- 27.Ashurst J V, Urquhart M, Cook MD. Carbon monoxide poisoning secondary to hookah smoking. J Am Osteopath Assoc. 2012;112:686–688. [PubMed] [Google Scholar]
- 28.Karaca Y, Eryigit U, Aksut N, Turkmen S. Syncope associated with water pipe smoking. BMJ Case Rep. 2013 doi: 10.1136/bcr-2013-009526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ozkan S, Ozturk T, Ozmen Y, Durukan P. Case report syncope associated with carbon monoxide poisoning due to narghile smoking. Case Reports in Emergency Medicine. 2013;2013:2–4. doi: 10.1155/2013/796857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bens BWJ, ter Maaten JC, Ligtenberg JJM. [Carbon monoxide poisoning after smoking from a water pipe] Ned Tijdschr Geneeskd. 2013;157 [PubMed] [Google Scholar]
- 31.Raub JA, Mathieu-Nolf M, Hampson NB, Thom SR. Carbon monoxide poisoning-a public health perspective. Toxicology. 2000;145:1–14. doi: 10.1016/s0300-483x(99)00217-6. [DOI] [PubMed] [Google Scholar]
- 32.British Thoracic Society Standards of Care Committee. Non-invasive ventilation in acute respiratory failure. Thorax. 2002;57:192–211. doi: 10.1136/thorax.57.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weaver LK, Howe S, Hopkins R, Chan KJ. Carboxyhemoglobin half-life in carbon monoxide-poisoned patients treated with 100% oxygen at atmospheric pressure. Chest. 2000;117:801–808. doi: 10.1378/chest.117.3.801. [DOI] [PubMed] [Google Scholar]
- 34.Shawna Silver, Camala Smith, Andrew Worster. Should hyperbaric oxygen be used for carbon monoxide poisoning? Can J Emerg Med. 2006;8:43–46. [Google Scholar]
- 35.Buckley Nick A, Juurlink David N, Isbister G, Bennett Michael H, Lavonas Eric J. Hyperbaric oxygen for carbon monoxide poisoning. Cochrane Database Syst Rev. 2011 doi: 10.1002/14651858.CD002041.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jackson D, Aveyard P. Waterpipe smoking in students: prevalence, risk factors, symptoms of addiction, and smoke intake Evidence from one British university. BMC Public Health. 2008;8 doi: 10.1186/1471-2458-8-174. [DOI] [PMC free article] [PubMed] [Google Scholar]