Abstract
Objectives
To study the effect of mitral valve repair with or without concomitant tricuspid valve repair on functional tricuspid regurgitation and right ventricular function.
Methods
From 2001 to 2007, 1833 patients with degenerative mitral valve disease, a structurally normal tricuspid valve, and no coronary artery disease underwent mitral valve repair, and 67 underwent concomitant tricuspid valve repair. Right ventricular function (myocardial performance index and tricuspid annular plane systolic excursion) was measured before and after surgery using transthoracic echocardiography for randomly selected patients with tricuspid regurgitation grade 0, 1+, and 2+(100 patients for each grade) and 93 with grade 3+/4+, 393 patients in total.
Results
In patients with mild (<3+) preoperative tricuspid regurgitation, mitral valve repair alone was associated with reduced tricuspid regurgitation and mild worsening of right ventricular function. Tricuspid regurgitation of 2+or greater developed in fewer than 20%, and right ventricular function had improved, but not to preoperative levels, at 3 years. In patients with severe (3+/4+) preoperative tricuspid regurgitation, mitral valve repair alone reduced tricuspid regurgitation and improved right ventricular function; however, tricuspid regurgitation of 2+ or greater returned and right ventricular function worsened toward preoperative levels within 3 years. Concomitant tricuspid valve repair effectively eliminated severe tricuspid regurgitation and improved right ventricular function. Also, over time, tricuspid regurgitation did not return and right ventricular function continued to improve to levels comparable to that of patients with lower grades of preoperative tricuspid regurgitation.
Conclusions
In patients with mitral valve disease and severe tricuspid regurgitation, mitral valve repair alone was associated with improved tricuspid regurgitation and right ventricular function. However, the improvements were incomplete and temporary. In contrast, concomitant tricuspid valve repair effectively and durably eliminated severe tricuspid regurgitation and improved right ventricular function toward normal, supporting an aggressive approach to important functional tricuspid regurgitation.
The effect of surgery to relieve left-sided valve disease, with or without tricuspid valve repair (TVR), on right ventricular (RV) function in patients with functional tricuspid regurgitation (TR) is of great interest, but few studies have been published. In our companion study, we found that RV function was markedly abnormal in patients with severe (grade 3+/4+) TR.1 This was true for the myocardial performance index (MPI), which reflects global RV systolic and diastolic function, and tricuspid annular plane systolic excursion (TAPSE), which reflects longitudinal systolic function.2 Whether the TR was caused by RV dysfunction or vice versa remained unclear. The decreased function suggested by MPI and TAPSE, both being load-sensitive indexes, could reflect true RV dysfunction or altered pre- and afterload.2
All these patients underwent mitral valve repair (MVR) to correct their mitral regurgitation(MR).Most patients with severe TR also underwent concomitant TVR; patients with less severe TR underwent only MVR. It is well known that MVR reduces pulmonary pressure and RV afterload; however, correcting TR increases RV afterload. Correcting MR could also influence the right heart by changing the atrial and ventricular septal positions from the shifting volume and pressure loads.
Therefore, in the same quasi-experimental, enriched study cohort with no evidence of either organic tricuspid valve (TV) alteration or coronary artery disease, we attempted to answer the following questions about TR and RV function after correcting the left-sided valve disease with or without concomitant TVR:
What are the early, intermediate-, and long-term effects of MVR alone versus MVR with concomitant TVR on TR and RV function?
Do the early postoperative measures of RV function on predischarge transthoracic echocardiograms (TTEs) correlate with the preoperative measures of these same quantities, and what factors, including preoperative TR and the operation, are associated with their changes after MVR alone versus MVR with concomitant TVR?
Does the apparently diminished preoperative RV dysfunction associated with severe preoperative TR improve during follow-up after surgery?
What factors, including preoperative TR, RV function, and the operation (MVR alone vsMVR with concomitant TVR), are associated with the temporal pattern of RV function observed during follow-up?
PATIENTS AND METHODS
The patient details and study design have been reported in the companion study.1 In brief, for 2726 patients undergoing mitral valve surgery at Cleveland Clinic, a random sample of 100 patients was selected for each preoperative TR grade 0+, 1+, and 2+on TTE. All 93 patients with grade 3+or 4+TR were included, for a total of 393 patients. Patient characteristics and preoperative echocardiographic findings are presented in Tables E1 and E2. Characteristics of the patients included in the present study were similar to those of patients not included, as analyzed by TR grade (Tables E3–E5).
Data Sources
All the data used for the present study were approved for use in research by the institutional review board, with patient consent waived. In addition to clinical and preoperative echocardiographic data described in the companion report,1 TR, TAPSE, and MPI were measured de novo, as previously described, on all postoperative TTEs available at Cleveland Clinic for these patients.2 Predischarge and follow-up TR was assessed on 707 TTEs for 388 patients (99% of total), and MPI and TAPSE on 643 TTEs for 355 patients (90%of total). The distribution of TTEs over time according to TR grade is shown in Table E6.
No fixed schedule for the postoperative surveillance TTEs was imposed. A total of 38% of patients had more than 1 TTE recorded, and 20% had more than 2. The number of TTEs per patient ranged from 1 to 10 (mean, 2). However, in 390 patients followed up at Cleveland Clinic, the pattern of intervals for the TTEs suggested a degree of regularity (Figure E1), and results (data not shown) in this group were entirely consistent with those presented for the group as a whole.
The intra- and interobserver variability of TAPSE andMPI was studied in 17 randomly selected patients. The intraobserver (R.D.) correlation was r = 0.97 for TAPSE (Figure E2, A) and r = 0.91 for MPI (Figure E2, B). The interobserver variability between investigator (R.D.) and sonographer was r = 0.61 for TAPSE (Figure E2, C) and r = .88 for MPI (Figure E2, D).
Statistical Analysis
Early response to surgery
Of the 393 patients, 3 (3.0%) of the 100 with grade 2+MR preoperatively underwent TVR (2 ring repair, 1 suture repair) concomitant with left-sided valve surgery, and 64 (69%) of the 93 with grade 3+/4+TR preoperatively underwent TVR (60 ring repair, 3 suture repair) or replacement (n = 1). Postoperatively, predischarge TTEs were retrievable and measurable for 96 of 100 patients with preoperative TR grade 0, 88 of 100 with TR grade 1+, 93 of 100 with grade TR 2+, and 85 of 93 (91%) with TR grade 3+/4+. TR grade could be measured on 362 predischarge TTEs, TAPSE on 349, and MPI on 348.
Analyses focused on the comparison of TR grade, TAPSE, and MPI from preoperative to predischarge levels. This included paired t-testing, correlation analyses, and multivariable ordinal logistic regression (TR grade) and linear regression analyses using the preoperative variables (TAPSE, MPI; Appendix E1). These analyses were performed overall, stratified according to whether a TV procedure had been performed and according to preoperative TR grade. For these multivariable analyses, we used “bagging” for variable selection.3 Automated stepwise regression was performed on 1000 bootstrap data sets with P = .05 used for the retention of variables. Thereafter, those present in 50%or more of the analyses were retained in the final model.
Course of postoperative TR and RV function
To assess the temporal trend of TR, TAPSE, and MPI after surgery, all postoperative and follow-up TTEs were analyzed longitudinally for pattern of change across time. A nonlinear mixed model4,5 was used to resolve the number of time phases to form a temporal decomposition model and to estimate the shaping parameters at each phase. Although each phase is defined across all time, each dominates the others in a different period from surgery (Figures E3–E5). We therefore used descriptive terms such as “early” and “late” to indicate the period of this dominance. Mixed-model regression6 for ordinal and continuous repeated measurements (SAS PROCNLMIXED, SAS Institute, Inc, Cary, NC) was used to implement the temporal decomposition model. The temporal pattern of prevalence of individual categories of the ordinal longitudinal data was obtained by averaging the patient-specific probability estimates. Because the underlying temporal patterns might be different for patients who underwent a TV procedure than in those who did not, we performed separate temporal pattern analyses for the 2 groups.
Missing values
We used a fivefold imputation7 with the Markov Chain Monte Carlo technique to impute the missing values for variables considered in multivariable analyses (PROC MI, SAS, version 9.1, SAS Institute, Inc), but not for outcomes. The missing information is indicated in each table. For variable selection, only the first imputed data set was used. Having established a model, we estimated the regression coefficients and their variance–covariance matrix for all 5 data sets. These were combined using PROC MIANALYZE (SAS Institute, Inc).
Presentation
Continuous variables are summarized as the mean ± standard deviation and as equivalent 15th, 50th (median), and 85th percentiles when their distribution was skewed. Comparisons were made using the Wilcoxon rank-sum test. Categorical data are summarized by frequencies and percentages, with comparisons made using the χ2 test. All analyses were performed using SAS statistical software, version 9.1 (SAS Institute, Inc). Uncertainty is expressed by 68% confidence limits equivalent to ± 1 standard error.
RESULTS
Effects of MVR Alone on TR and RV Function
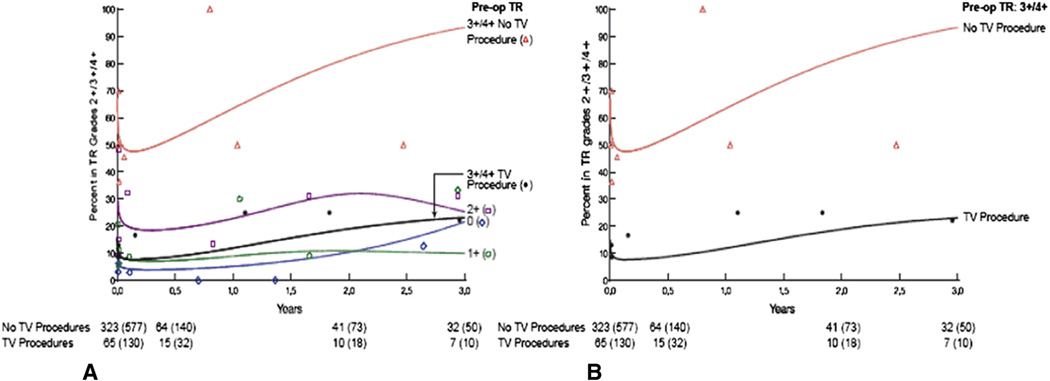
MVR alone (which reduced MR to grade 0 or 1+in 98% of patients) reduced TR, irrespective of the preoperative grade of TR, although patients with grade 2+or more TR were more likely to have the same higher grade of TR postoperatively. Over time, patients with lower grades of preoperative TR (0–2+) showed very little increase in TR, but those with severe TR preoperatively showed a return of grade 2+or more TR within 3 years (Figure 1).
FIGURE 1.
Percentage of patients with grade 2+/3+/4+tricuspid regurgitation (TR) grades postoperatively over time stratified by preoperative (pre-op) TR grades. Open diamonds and blue line indicate patients with preoperative TR grade 0; open circles and green line, those with preoperative grade 1+; open squares and purple line, those with preoperative grade 2+; closed circles and black line, those with preoperative grade 3+/4+and undergoing a tricuspid valve (TV) procedure; and open triangles and red line, those with preoperative grade 3+/4+and no TV procedure. A, TR grade 2+/3+/4+postoperatively according to preoperative TR grade and TV procedure; and (B) TR grade 2+/3+/4+postoperatively for patients with severe preoperative TR according to whether a TV procedure was performed.
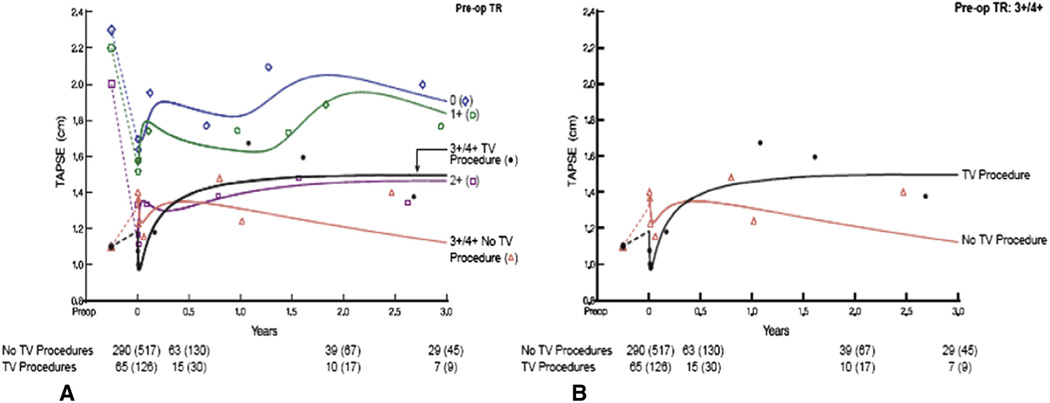
Parallel to the improvement in TR, a mild reduction of RV function was observed in patients with lower grade 0 to 2+ TR and normal RV function. For grade 0 and 1+TR, RV function was still normal, but for grade 2+TR, it was lower than normal (Figures 2 and 3). However, patients with severe TR and RV dysfunction preoperatively actually showed both reduced TR and improved RV function after MVR alone. RV function improvement was observed for both TAPSE and MPI. These improvements were, however, temporary, and, at 3 years, both TR and RV dysfunction had returned to the preoperative levels.
FIGURE 2.
Tricuspid annular plane systolic excursion (TAPSE) over time stratified by preoperative tricuspid regurgitation (TR) grade. Depiction by preoperative TR grade and tricuspid valve (TV) procedure as in Figure 1. A, TAPSE for all preoperative TR grades and TV procedure. B, TAPSE for patients with severe preoperative TR according to whether a TV procedure was performed.
FIGURE 3.
Mean myocardial performance index (MPI) over time stratified by preoperative tricuspid regurgitation (TR) grades and tricuspid valve (TV) procedure. Depiction by preoperative TR grade and TV procedure as in Figure 1. A, MPI for all preoperative TR grades and TV procedure. B, MPI for patients with severe preoperative TR according to whether a TV procedure was performed.
Effects of MVR and Concomitant TVR on TR and RV Function
Of the patients with grade 2+TR and those with severe TR, 3 and 64 underwent a concomitant TV procedure (66 repair and 1 replacement) and 97 and 29 did not, respectively.
The TV procedure effectively reduced severe TR to 0 to 1+, and this improvement was stable over time, in contrast to when severe TR was not addressed (Table E7 and Figure 1). MVR with or without TVR reduced RV systolic pressure (Figure E6).
In patients with severe TR and impaired RV function preoperatively, RV function (both TAPSE and MPI) improved immediately after surgery, irrespective of whether the patients had undergone concomitant TVR (Figures 2 and 3). This immediate improvement was more pronounced if TVR had not been performed. After a brief decrease in TAPSE, both TAPSE and MPI improved for the first 6 months, irrespective of whether the patients had undergone a TV procedure. After TVR, this improvement continued for both measures, but without TVR, RV function started to progressively decline at 6 months in parallel with a return of TR to preoperative levels (Figures 2 and 3). At 3 years, both TAPSE and MPI were normal after TVR. However, without TVR, both TR and RV dysfunction had returned to preoperative levels.
Predictors of RV Function in Response to Surgery Immediate response
In general, the distribution of both TAPSE and MPI was toward worse RV function than preoperatively, except for patients with grade 3+/4+TR and poor RV function preoperatively. These trends were apparent in scattergrams of change for individual patients (Figure 4 and Figure E7). On the predischarge TTEs, TAPSE and MPI, although improved, were worse in patients with preoperative TR grade 2+or worse.
FIGURE 4.
Scattergram of preoperative (pre-op) versus postoperative (predischarge) myocardial performance index (MPI) according to preoperative grade of tricuspid regurgitation (TR). Each symbol represents 1 patient. Open circles indicate no tricuspid procedure was performed; filled circles indicate tricuspid procedure was performed. Dashed lines represent upper limit of normal. Corresponding data for tricuspid annular plane systolic excursion presented in Figure E7. A, n = 83; (B) n = 89; (C) n = 91; and (D) n = 86.
Temporal patterns
Preoperative factors associated with higher postoperative TR grade
Overall, a higher preoperative TR grade, female gender, and older age were associated with higher predischarge TR. In the early phase, which is the immediate effect of surgery, higher preoperative MPI and absence of a TV procedure were associated with a higher postoperative TR grade. In the late phase, lower ejection fraction, higher grade of MR, and absence of a TV procedure were associated with a higher postoperative TR grade (Table 1). No statistically significant association was found between preoperative TAPSE and postoperative TR in any phase (P>.2), nor was any interaction seen between preoperative MPI and preoperativeTAPSE on postoperative TR during either phase (P = .3).
TABLE 1.
Risk factors associated with higher grade of postoperative tricuspid regurgitation
| Factor | Estimate ± SE |
P value |
Reliability (%)* |
|---|---|---|---|
| Overall | |||
| Older age† | 1.1 ± 0.23 | <.0001 | 77 |
| Women | 1.02 ± 0.26 | .0001 | 52 |
| Higher grade of preoperative TR‡ | −1.7 ± 0.53 | .001 | 71 |
| Early phase | |||
| Higher preoperative MPI§ | 4.1 ± 1.8 | .02 | 61 |
| Absence of TV procedure | −4.2 ± 1.1 | .0001 | |
| Late phase | |||
| Lower LVejection fraction‖ | 3.9 ± 1.3 | .003 | 61 |
| Higher MR grade | 1.4 ± 0.56 | .02 | 78 |
| Absence of TV procedure | −2.3 ± 0.58 | <.0001 |
LV, Left ventricular; MPI, myocardial performance index; MR, mitral regurgitation; SE, standard error; TR, tricuspid regurgitation; TV, tricuspid valve.
Percentage of times variable appeared in 500 bootstrap models.
(Age/50)2, squared transformation.
(1/[TR grade+1]), inverse transformation.
MPI2, squared transformation.
(50/ejection fraction), inverse transformation.
Preoperative factors associated with lower (worse) TAPSE
Overall, a higher grade of preoperative TR, higher heart rate, larger left atrial systolic area, lower left ventricular ejection fraction, and higher blood urea nitrogen were associated with lower postoperative TAPSE (Table 2). In the early phase, only a TV procedure was associated with lower postoperative TAPSE. In the late phase, absence of a TV procedure, higher bilirubin level, and lower TV fractional area shortening were associated with lower postoperative TAPSE.
TABLE 2.
Preoperative risk factors associated with lower (worse) postoperative TAPSE
| Factor | Estimate ± SE |
P value |
Reliability (%)* |
|---|---|---|---|
| Overall | |||
| Higher preoperative TR | 100 | ||
| 1+vs 0 | 0.13 ± 0.047 | .006 | |
| 2+vs 0 | 0.45 ± 0.047 | <.0001 | |
| 3+/4+vs 0 | 0.50 ± 0.051 | <.0001 | |
| Higher heart rate† | −0.16 ± 0.079 | .05 | 60 |
| Larger LA area in systole‡ | −4.9 ± 1.8 | .005 | 99 |
| Lower LVejection fraction§ | 0.22 ± 0.087 | .01 | 65 |
| Higher BUN‖ | 0.052 ± 0.019 | .005 | 77 |
| Early phase | |||
| Shorter RV base to apex length¶ | −0.76 ± 0.41 | .06 | 85 |
| TV procedure | 1.04 ± 0.52 | .03 | |
| Late phase | |||
| Lower TV fractional shortening# | −7.04 ± 4.02 | .07 | 88 |
| Higher bilirubin** | 0.72 ± 0.24 | .006 | 83 |
| No TV procedure | −0.72 ± 0.26 | .006 |
BUN, Blood urea nitrogen; LA, left atrial; LV, left ventricular; RV, right ventricular; SE, standard error; TAPSE, tricuspid annular plane systolic excursion; TR, tricuspid regurgitation; TV, tricuspid valve.
Percentage of times factor appeared in 500 bootstrap models.
(75/heart rate), inverse transformation.
(1/LA area in systole), inverse transformation.
(50/LV ejection fraction), inverse transformation.
(BUN/20)2, squared transformation.
(RV base to apex length/7)2, squared transformation.
(TV fractional shortening)2, squared transformation.
Ln(bilirubin), natural logarithmic transformation.
Preoperative factors associated with higher (worse) MPI
Overall, a higher grade of preoperative TR, higher heart rate, larger left atrial volume index, lower MR grade, a history of chronic obstructive pulmonary disease, and older age were associated with higher postoperative MPI (Table 3). In the early phase, a history of hypertension, higher mean systemic arterial pressure, and higher preoperative MPI were associated with higher postoperative MPI. No factors were associated with postoperative MPI in the late phase.
TABLE 3.
Preoperative risk factors associated with greater (worse) postoperative MPI
| Factor | Estimate ± SE |
P value |
Reliability (%)* |
|---|---|---|---|
| Overall | |||
| Greater preoperative TR | 100 | ||
| 1+vs 0 | 0.098 ± 0.022 | <.0001 | |
| 2+vs 0 | 0.16 ± 0.024 | <.0001 | |
| 3+/4+vs 0 | 0.12 ± 0.036 | .0009 | |
| History of COPD | 0.12 ± 0.027 | <.0001 | 95 |
| Higher heart rate† | 0.034 ± 0.019 | .07 | 50 |
| Older age‡ | 0.038 ± 0.015 | .01 | 88 |
| Larger LA volume index§ | 0.039 ± 0.018 | .03 | 85 |
| Lower MR | −0.059 ± 0.028 | .03 | 42 |
| TV procedure | 0.036 ± 0.032 | .3 | |
| Early phase | |||
| History of hypertension | 0.033 ± 0.016 | .04 | 42 |
| Greater mean systemic arterial pressure‖ | −6.7 ± 4.02 | .09 | 58 |
| Greater preoperative MPI¶ | 0.055 ± 0.028 | .05 | 58 |
| Late phase | |||
| None |
COPD, Chronic obstructive pulmonary disease; LA, left atrial; MPI, myocardial performance index; MR, mitral regurgitation; SE, standard error; TR, tricuspid regurgitation; TV, tricuspid valve.
Percentage of times factor appeared in 500 bootstrap models.
(75/heart rate), inverse transformation.
(Age/50)2, squared transformation.
Ln(LA volume index), natural logarithmic transformation.
(1/mean arterial pressure), inverse transformation.
MPI2, squared transformation.
DISCUSSION
Functional TR secondary to left-sided heart disease has been thought to be caused by changes in RV geometry, the size and shape of the TV annulus, and the relative displacement of papillary muscles.8–10 In accordance with this theory, eliminating MR should initiate reverse RV remodeling and reduce TR. Our findings confirmed that MVR alone reduced RV systolic pressure and improved TR of every severity grade.
In our companion report, however, RV dysfunction stood out as having a more consistent association with severe functional TR than any other measure of RV remodeling. Other than the efficiency and durability of TVR in reducing TR, little information is available on the effect of these procedures on RV reverse remodeling and RV dysfunction. In patients with grade 0 to 2+TR, MVR induced a mild early reduction of RV function; however, the function remained at low normal, and a few experienced worsening of TR, as observed by Yilmaz and colleagues.11 We do not have a good explanation for this mild RV dysfunction, but speculate that it could be nonspecific effects related to suboptimal myocardial protection of the right ventricle during surgery, perioperative management of volume (preload) and drugs, or just a general effect of surgery. RV function quickly recovered, but not to preoperative levels. Although this suggests a possible disconnect between TR and RV function, these patients did not have much TR preoperatively. In fact, in patients with severe TR, MVR alone improved RV function in parallel with improvement in TR; however, these improvements did not last.
The effectiveness of TVR was impressive, because it both eliminated severe TR and improved RV function. Immediate improvement of RV function, by both TAPSE and MPI, was less after concomitant TVR than after MVR alone. However, the effect of TVR was durable over time, with a minimal return of TR, such as was observed by Chan and colleagues,12 and continued improvement of RV function, which eventually reached low normal levels for both TAPSE and MPI.13 It is certainly good news that in this setting of severe functional TR secondary to mitral valve disease, RV dysfunction was reversible, returning to close to normal after TVR and remaining stable. This occurred even though the patients who had undergone concomitant TVR were sicker than those with severe TR undergoing MVR alone, although the RV dysfunction was the same (Table E8). In contrast, the early improvements of TR and RV function after MVR alone were eliminated within 3 years.
The interaction between TR and RV function appears to be in both directions; not only does RV dysfunction affect the severity of TR, but reduced TR is also associated with improved RV function. Functional TR is secondary to RV dysfunction and vice versa.
An additional important question relates to how well TAPSE and MPI reflect RV function and changes in RV function after surgery. TAPSE measures longitudinal systolic function and has been shown to correlate highly with MRI-derived volumes14 and radionuclide ejection fraction.15 The MPI primarily measures contractility, and its calculation involves consideration of energy-dependent periods of contraction, ejection, and diastolic relaxation.16 The use of TAPSE and MPI as measures of postoperative RV function has not been validated.2 The temporal pattern of TAPSE and MPI was very similar, with a significant positive relationship between the pre- and postoperative values. Our findings are similar to a recent MRI study in which RV volumes and ejection fraction were measured in patients undergoing surgical repair of severe TR.13 This indicates that TAPSE and MPI are equally useful measures of RV function postoperatively as preoperatively in our group of patients, and this seemed to also be true after concomitant TVR. The factors associated with worse RV function postoperatively (Tables 2 and 3) make sense because these factors are all indicators of more advanced disease and right heart failure, with expected effects on the right heart.
Study Limitations
The study population was patients with degenerative mitral valve disease and secondary “functional” TR. Therefore, the results might not be applicable to other patient categories with TR and RV dysfunction. Although our findings make sense and fit into an understandable pattern, validation of the selected measures of RV function, TAPSE and MPI, against other qualitative and quantitative measures of RV function needs additional study. In particular, validation of RV function measures after cardiac surgery is important, because the surgery and perioperative management include so many manipulations that could affect these measures. Nevertheless, we were impressed by the consistency of our results, causing us to believe TAPSE and MPI are relatively good measures of intrinsic RV function.
All echocardiographic measures are subject to intra- and interobserver variability. To this is added the variability across time because equipment has changed. For the present study, intraobserver variability was excellent, with little evidence of bias. Thus, for all measurements reported, which were made by 1 investigator, we believe the results are reproducible. The agreement between investigator and sonographer was more variable, particularly for TAPSE. This surprised us because of the ease with which TAPSE can be measured.
This was a single-institution, observational study; thus, echocardiographic follow-up was, to an unknown extent, opportunistic rather than systematic. However, a large number of postoperative echocardiograms were available to enable powerful longitudinal data analysis of multiple measurements over time instead of independent time points.17
Study Implications
In patients with degenerative mitral valve disease and functional TR, MVR alone was associated with mild impairment of RV function in patients with lower grades of TR. In patients with severe TR, both TR and RV function improved. However, these improvements were incomplete and temporary, with both TR and RV dysfunction returning to preoperative levels within 3 years. In contrast, concomitant TVR durably eliminated severe TR and was associated with improved RV function toward normal, supporting an aggressive approach to important functional TR.
Supplementary Material
Acknowledgment
This study was supported in part by the Kenneth Gee and Paula Shaw, PhD, Chair in Heart Research (to Dr Blackstone), and the Peter and Elizabeth C. Tower and Family Endowed Chair in Cardiothoracic Research, James and Sharon Kennedy, the Slosburg Family Charitable Trust, Stephen and Saundra Spencer, and Martin Nielsen (to Dr Pettersson).
Abbreviations and Acronyms
- MPI
myocardial performance index
- MR
mitral regurgitation
- MVR
mitral valve repair
- RV
right ventricular
- TAPSE
tricuspid annular plane systolic excursion
- TR
tricuspid regurgitation
- TTE
transthoracic echocardiogram
- TV
tricuspid valve
- TVR
tricuspid valve repair
Footnotes
Supplemental material is available online.
Disclosures: Authors have nothing to disclose with regard to commercial support.
References
- 1.Vargas Abello LM, Klein AL, Marwick TH, Nowicki ER, Rajeswaran J, Puwanant S, et al. Understanding right ventricular dysfunction and functional tricuspid regurgitation accompanying mitral valve disease. J Thorac Cardiovasc Surg. doi: 10.1016/j.jtcvs.2012.01.088. Epub 2012 May 22. [DOI] [PubMed] [Google Scholar]
- 2.Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713. doi: 10.1016/j.echo.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 3.Breiman L. Bagging predictors. Machine Learning. 1996;24:123–140. [Google Scholar]
- 4.Diggle PJ, Heagerty PJ, Liang KY, Zeger SL. Analysis of longitudinal data. 2nd ed. New York: Oxford University Press; 2002. [Google Scholar]
- 5.Mason DP, Rajeswaran J, Murthy SC,McNeill AM, Budev MM, Mehta AC, et al. Spirometry after transplantation: how much better are two lungs than one? Ann Thorac Surg. 2008;85:1193–1201. e1–e2. doi: 10.1016/j.athoracsur.2007.12.023. [DOI] [PubMed] [Google Scholar]
- 6.Blackstone EH. Breaking down barriers: helpful breakthrough statistical methods you need to understand better. J Thorac Cardiovasc Surg. 2001;122:430–439. doi: 10.1067/mtc.2001.117536. [DOI] [PubMed] [Google Scholar]
- 7.Rubin DB. Multiple imputation for non-response in surveys. New York: Wiley; 1997. [Google Scholar]
- 8.Tei C, Pilgrim JP, Shah PM, Ormiston JA, Wong M. The tricuspid valve annulus: study of size and motion in normal subjects and in patients with tricuspid regurgitation. Circulation. 1982;66:665–671. doi: 10.1161/01.cir.66.3.665. [DOI] [PubMed] [Google Scholar]
- 9.Ubago JL, Figueroa A, Ochoteco A, Colman T, Duran RM, Duran CG. Analysis of the amount of tricuspid valve annular dilatation required to produce functional tricuspid regurgitation. Am J Cardiol. 1983;52:155–158. doi: 10.1016/0002-9149(83)90087-5. [DOI] [PubMed] [Google Scholar]
- 10.Sagie A, Schwammenthal E, Padial LR, Vazquez de Prada JA, Weyman AE, Levine RA. Determinants of functional tricuspid regurgitation in incomplete tricuspid valve closure: Doppler color flow study of 109 patients. JAm Coll Cardiol. 1994;24:446–453. doi: 10.1016/0735-1097(94)90302-6. [DOI] [PubMed] [Google Scholar]
- 11.Yilmaz O, Suri RM, Dearani JA, Sundt TM, III, Daly RC, Burkhart HM, et al. Functional tricuspid regurgitation at the time of mitral valve repair for degenerative leaflet prolapse: the case for a selective approach. J Thorac Cardiovasc Surg. 2011;142:608–613. doi: 10.1016/j.jtcvs.2010.10.042. [DOI] [PubMed] [Google Scholar]
- 12.Chan V, Burwash IG, Lam BK, Auyeung T, Tran A, Mesana TG, et al. Clinical and echocardiographic impact of functional tricuspid regurgitation repair at the time of mitral valve replacement. Ann Thorac Surg. 2009;88:1209–1215. doi: 10.1016/j.athoracsur.2009.06.034. [DOI] [PubMed] [Google Scholar]
- 13.Kim HK, Kim YJ, Park EA, Bae JS, Lee W, Kim KH, et al. Assessment of haemodynamic effects of surgical correction for severe functional tricuspid regurgitation: cardiac magnetic resonance imaging study. Eur Heart J. 2010;31:1520–1528. doi: 10.1093/eurheartj/ehq063. [DOI] [PubMed] [Google Scholar]
- 14.Endo Y, Maddukuri PV, Vieira ML, Pandian NG, Patel AR. Quantification of right ventricular volumes and function by real time three-dimensional echocardiographic longitudinal axial plane method: validation in the clinical setting. Echocardiography. 2006;23:853–859. doi: 10.1111/j.1540-8175.2006.00327.x. [DOI] [PubMed] [Google Scholar]
- 15.Ueti OM, Camargo EE, Ueti Ade A, de Lima-Filho EC, Nogueira EA. Assessment of right ventricular function with Doppler echocardiographic indices derived from tricuspid annular motion: comparison with radionuclide angiography. Heart. 2002;88:244–248. doi: 10.1136/heart.88.3.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burgess MI, Bright-Thomas RJ, Ray SG. Echocardiographic evaluation of right ventricular function. Eur J Echocardiogr. 2002;3:252–262. [PubMed] [Google Scholar]
- 17.Mehta RH, Bruckman D, Das S, Tsai T, Russman P, Karavite D, et al. Implications of increased left ventricular mass index on in-hospital outcomes in patients undergoing aortic valve surgery. J Thorac Cardiovasc Surg. 2001;122:919–928. doi: 10.1067/mtc.2001.116558. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.