Abstract
Aims
To explore the relationships between type 2 diabetes mellitus, area-based socioeconomic status (SES) and cardiovascular disease mortality in Scotland.
Methods
We used an area-based measure of SES, Scottish national diabetes register data linked to mortality records, and general population cause-specific mortality data to investigate the relationships between SES, type 2 diabetes and ischaemic heart disease (IHD) and cerebrovascular disease (CbVD) mortality, for 2001-2007. We used negative binomial regression to obtain age-adjusted relative risks (RRs) of mortality (by sex), comparing people with type 2 diabetes to the non-diabetic population.
Results
Among 216,652 people aged 40 years or older with type 2 diabetes (980,687 person-years), there were 10,554 IHD deaths and 4,378 CbVD deaths. Age-standardised mortality increased with increasing deprivation, and was higher among men. IHD mortality RRs were highest among the least deprived quintile and lowest in the most deprived quintile (Men, least deprived: RR 1.94 95% CI 1.61, 2.33; most deprived: RR 1.46 95% CI 1.23, 1.74) and were higher in women than men (Women, least deprived: RR 2.84 95% CI 2.12, 3.80; most deprived: RR 2.04 95% CI 1.55, 2.69). A similar, weaker, pattern was observed for cerebrovascular mortality.
Conclusions
Absolute risk of cardiovascular mortality is higher in people with diabetes than the non-diabetic population, and increases with increasing deprivation. The relative impact of diabetes on cardiovascular mortality differs by SES and further efforts to reduce cardiovascular risk both in deprived groups and people with diabetes are required. Prevention of diabetes may reduce socioeconomic health inequalities.
Keywords: Cerebrovascular disorders; Diabetes Mellitus, Type 2; Epidemiology; Myocardial Ischemia; Scotland; Socioeconomic factors
Introduction
The role of socioeconomic status (SES) in the morbidity and mortality from common chronic diseases has been widely investigated [1]. It is well documented that the prevalence of type 2 diabetes mellitus and risk factors associated with its development are higher among lower socioeconomic groups [2-5]. Long-term outcomes, such as all-cause mortality, among people with diabetes have also been shown to be associated with SES [6-10].
Few studies have examined the relationship between SES and cardiovascular disease mortality. Among those that have, results are mixed, with most studies reporting that cardiovascular mortality increases with decreasing SES[6, 7, 9, 11], and others reporting no association [12, 13]. Even fewer studies have determined whether the SES gradient for cardiovascular mortality differs by diabetes status[6, 9, 13]. Many studies have included small numbers of people with type 2 diabetes, limiting the power to detect relationships between SES and cardiovascular mortality.
A better understanding of the impact of SES on cardiovascular disease incidence and mortality among people with type 2 diabetes is needed to help develop and direct improved interventions for reducing complications and risk of death. Measures of SES may, for example, improve the predictive power of current cardiovascular risk models for people with diabetes [14, 15].
In Scotland, population-based data on almost all people with diagnosed diabetes are collected electronically from primary and secondary care where they are used for individual patient management. The database includes information on more than 200,000 people with diabetes, and is a valuable resource for research. Previous analyses of these data found an inverse relationship between SES and the relative risk of all-cause mortality [10]. This SES gradient for all-cause mortality differed between those with and without type 2 diabetes, with a lower relative risk among the most deprived SES group [10]. In this study, we sought to investigate whether a similar relationship is observed between SES and cardiovascular mortality among people with and without diabetes in Scotland between 2001 and 2007.
Methods
Scottish national electronic diabetes dataset
In Scotland, which has a population of 5.2 million, population-based data for people diagnosed with Type 1 or Type 2 diabetes mellitus are collected in the Scottish Care Information – Diabetes Collaboration (SCI-DC) dataset. National collation of demographic and diabetes clinical care data started in 2000. SCI-DC is populated through daily downloads from primary care databases, with data collated from all except five of the approximately 1000 general practices in Scotland, and from most hospital diabetes clinics.
Population of people with type 2 diabetes
In this study, we identified individuals included in the SCI-DC dataset between 2001 and 2007 who were diagnosed with type 2 diabetes and were aged 40 years or over during this period as both type 2 diabetes and cardiovascular disease mortality are rare in younger people. Presence of type 2 diabetes was defined by excluding people with type 1 diabetes (defined by applying an algorithm including diagnosis before 30 years of age, a prescribing history showing continuous insulin prescription from diagnosis of diabetes and no record of prescription of non-metformin oral diabetes drugs and clinically defined type of diabetes). We included individuals for whom data on year of birth, sex, SES and dead/alive status were available.
Our colleagues at the Information Services Division of the National Health Service National Services Scotland (NHS NSS) used the Scottish unique health record identifier, the Community Health Index, and probabilistic linkage methods to link the Scottish national diabetes register data to mortality records [16]. A research database containing no identifiable information was used for analysis. Approval for the generation and analysis of the linked dataset was obtained from the SCI-DC steering committee, the Scottish multi-centre research ethics committee, the Privacy Advisory Committee of NHS NSS and Caldicott guardians of all 14 Health Boards in Scotland.
For the main analysis, we identified deaths among people with diabetes from ischaemic heart disease (IHD) (International Classification of Disease [ICD10] codes I20-25) and cerebrovascular disease (CbVD) (ICD10 I60-69, G45), where these codes were given as the underlying (primary) cause of death. Individuals were considered to be at risk between January 2001 (if aged at least 40 years during this year) until 31st December 2007 or date of death, whichever was earliest. People who reached 40 years of age during this period were considered at risk from that point onwards and people who were diagnosed with type 2 diabetes during the study period were considered at risk from the date of diagnosis.
Population without diabetes
We obtained data on the total population and numbers of ischaemic heart disease (ICD I20-I25) and CbVD (ICD I60-69, G45) deaths in the Scottish population by calendar year, age, sex and SIMD quintile from the Information Services Division of NHS NSS. We subtracted the number of deaths and person-years at risk among people with diabetes (types 1 and 2) from the total deaths and person-years at risk in the Scottish population to obtain a non-diabetic comparison population.
Socioeconomic status
We used the Scottish Index of Multiple Deprivation (SIMD), an area-based measure of socioeconomic status assigned on the basis of place of residence at datazone level (an area with a median population of 769 people) [17]. The 2006 version of the SIMD combines 31 indicators across 7 domains of income, employment, health, education, housing, geographic access and crime. The overall index is a weighted sum of these seven domain scores for each datazone and is assigned using postal codes. Quintiles of the index are defined at a national level, with quintile one used to identify the least deprived and quintile five used to identify the most deprived 20% of datazones.
Statistical analyses
We calculated IHD and CbVD mortality rates for the populations with type 2 diabetes and the non-diabetic population, age-standardised to the European Standard Population, from 40 years of age upwards, by sex and SES.
Since the data did not fit the Poisson distribution we used negative binomial regression, which takes account of over-dispersion [18], to obtain relative risks (RRs) with 95% confidence intervals (CIs) for the association between diabetes status and IHD mortality and CbVD mortality. We investigated whether there was effect modification of diabetes by SES by testing for both multiplicative interaction and by investigating the presence of supra-additive interaction between diabetes and the most deprived compared to the most affluent quintile using the methodology and resources described by Andersson et al [19]. A relative excess risk of interaction (RERI) of greater than zero and a synergy index greater than one derived from the latter method suggest that the combined effects of two exposures are greater than expected from adding the individual effects. Testing for multiplicative interactions is more conventional and is used to test the fit of statistical models but the investigation of additive interaction is more relevant to understanding population health [20].
Sensitivity analyses
Identifying IHD or CbVD deaths in our main analysis from the underlying cause of death may underestimate numbers of cardiovascular deaths among people with diabetes. Death certificate coding rules lead to the assignment of diabetes as the underlying cause of death in death records when both cardiovascular disease and diabetes are listed in part I of the death certificate. We therefore repeated our analyses using a broader definition of cardiovascular death, including deaths in which diabetes was recorded as underlying cause with IHD or CbVD mentioned elsewhere on the death record.
To investigate the effect of the incompleteness of the diabetes register between 2001 and 2004, prior to its widespread use in primary care which results in artificially low mortality in those years, we performed a further sensitivity analysis in which we restricted our analyses to only people included in the register between 2005 and 2007, when register coverage was almost universal.
Analyses were performed using STATA version 11 (College Station, Texas).
Results
Absolute mortality by diabetes status, sex and SES
After excluding people for whom SES data were unavailable (n = 1282), 216,652 people with type 2 diabetes of 40 years of age and above were included. Of these, 116,145 (54%) were men and 100,507 (46%) were women. During 525,077 person-years of follow-up in men, 22,033 died, 6,000 (27%) from IHD and 1,942 (9%) from CbVD. During 455,610 person-years of follow-up in women, 20,571 died, 4,554 (22%) from IHD and 2,436 (12%) from CbVD (Table 1).
Table 1. Deaths from ischaemic heart disease and cerebrovascular disease among people aged ≥40 years, between 2001 and 2007, by sex and socioeconomic status.
| People with type 2 diabetes | People without diabetes | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| Men n=116,152 | Women n=100,507 | Men n=2,433,748 | Women n=2,630,482 | |||||||||
|
|
||||||||||||
| Socioeconomic status quintile | Person-years | IHD deaths N | CbVD deaths N | Person-years | IHD deaths N | CbVD deaths N | Person-years | IHD deaths N | CbVD deaths N | Person-years | IHD deaths N | CbVD deaths N |
| 1 (least deprived) | 84,067 | 746 | 278 | 59,773 | 505 | 349 | 1,839,545 | 4761 | 2021 | 2,101,479 | 4467 | 4035 |
| 2 | 101,110 | 1033 | 414 | 78,656 | 727 | 464 | 1,882,780 | 6246 | 2476 | 2,151,994 | 5811 | 4834 |
| 3 | 110,008 | 1278 | 371 | 93,603 | 930 | 527 | 1,832,739 | 7670 | 2850 | 2,135,428 | 6736 | 5067 |
| 4 | 116,010 | 1446 | 442 | 108,986 | 1108 | 545 | 1,698,901 | 8658 | 2823 | 2,077,940 | 7824 | 5029 |
| 5 (most deprived) | 113,882 | 1497 | 437 | 114,593 | 1284 | 551 | 1,561,147 | 9466 | 3021 | 1,931,388 | 7611 | 4667 |
| All | 525,077 | 6,000 | 1,942 | 455,610 | 4,554 | 2,436 | 8,815,112 | 36,801 | 13,191 | 10,398,229 | 32,449 | 23,632 |
IHD = ischaemic heart disease
CbVD = cerebrovascular disease
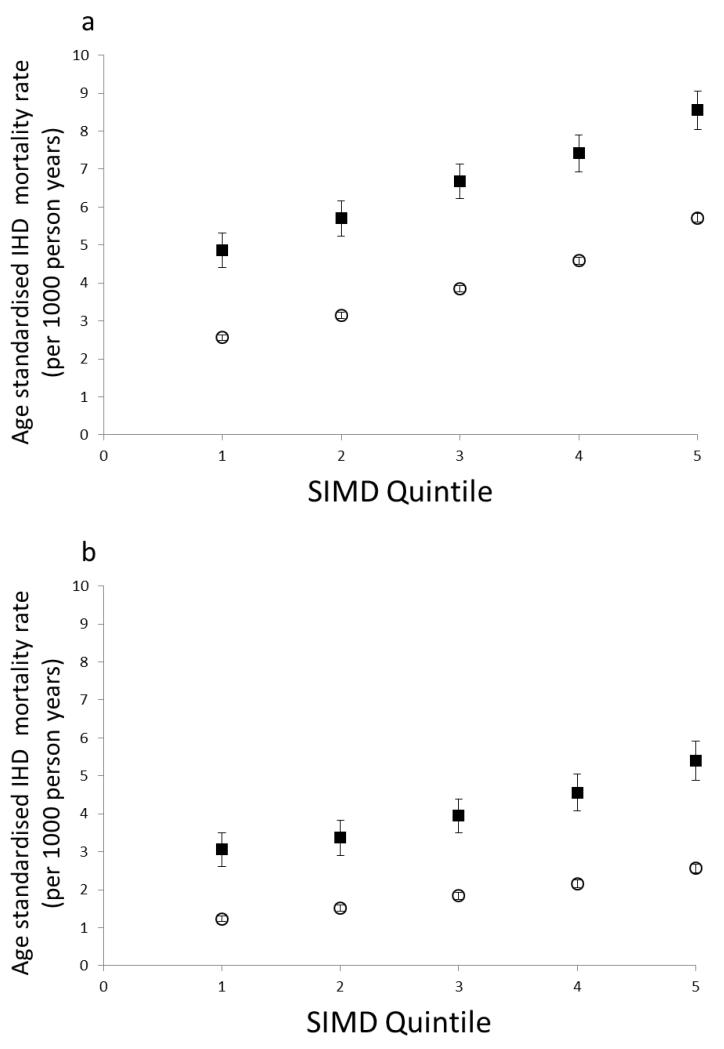
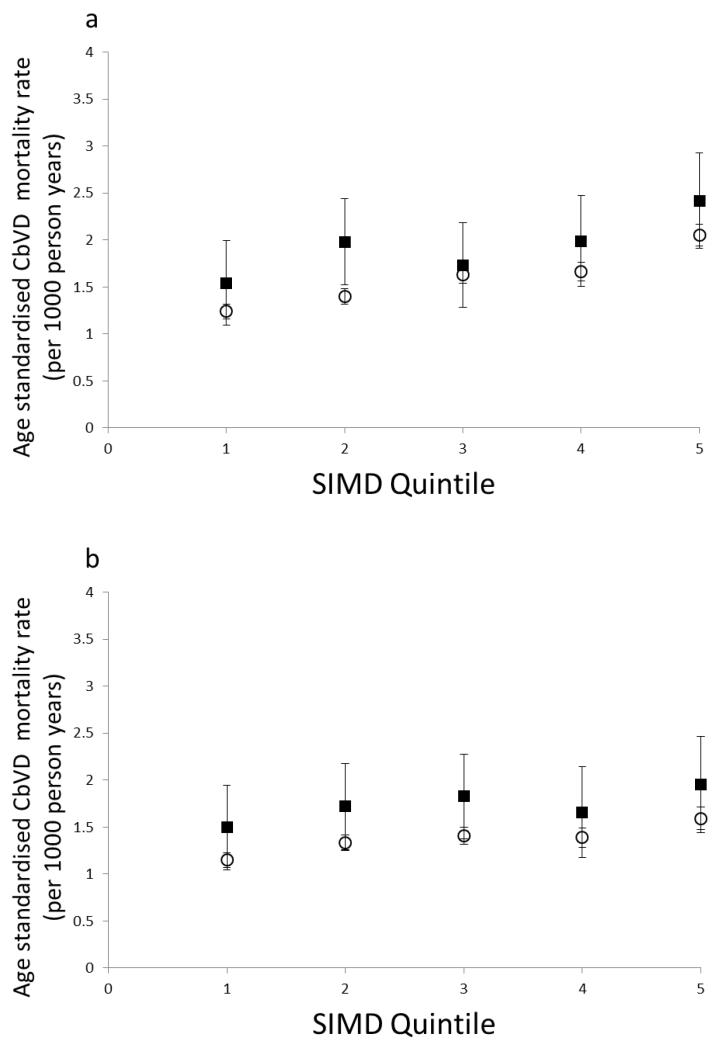
Age-standardised IHD and CbVD mortality rates increased with increasing deprivation, irrespective of diabetes status (Figures 1 and 2). In people with diabetes the IHD mortality rate was 80% higher in the most deprived than the least deprived quintile in both men and women (Figure 1). Among men with diabetes, the cerebrovascular mortality rate was about 50% higher in the most versus least deprived quintile, with a smaller difference among women (Figure 1). The IHD and CbVD mortality rates in people without diabetes also increased with increasing deprivation, although this relationship was less steep for CbVD than for IHD. As the slightly divergent lines of figure 1 demonstrate, the difference in absolute risks of cardiovascular disease mortality between people with diabetes and those without increases modestly across each deprivation category, although the combination of deprivation and diabetes appears to be particularly detrimental for women. The age-adjusted absolute risk difference in IHD mortality in women with diabetes and without was 1.77/1000 person years for the least deprived quintile and 2.82/1000 person years for the most deprived quintile.
Figure 1. Age-standardised ischaemic heart disease mortality rates by socioeconomic status, for men and women with and without type 2 diabetes.
White circles, people without diabetes; Black squares, people with type 2 diabetes mellitus
SIMD = Scottish index of multiple deprivation; IHD = ischaemic heart disease; T2DM= type 2 diabetes mellitus
Figure 2. Age-standardised cerebrovascular disease mortality rates by socioeconomic status, for men and women with and without type 2 diabetes.
White circles, people without diabetes; Black squares, people with type 2 diabetes mellitus
SIMD = Scottish index of multiple deprivation; CbVD = cerebrovascular disease; T2DM= type 2 diabetes mellitus
Relative mortality risk, comparing people with and without diabetes
Cardiovascular mortality risk was significantly greater among people with diabetes compared to the non-diabetic population, both before and after adjusting for SES, with inclusion of SES improving the fit of the models for men and women. In analyses adjusted for age alone, IHD mortality risk among men with diabetes was 73% greater than those without diabetes (RR 1.73 95% CI 1.51, 1.98), and was attenuated slightly upon further adjustment for SES (RR 1.71 95% CI 1.57, 1.86). The RR for type 2 diabetes and IHD mortality was higher in women (age adjusted RR: 2.40 95% CI 2.01, 2.87; age and SES adjusted RR: 2.34 95% CI 2.05, 2.67). As expected, the age and SES adjusted RRs were higher when the broader definition of IHD mortality including any mention on a death certificate was applied in a sensitivity analysis (men: RR 2.06 95% CI 1.89, 2.24; women: 2.97 95% CI 2.60, 3.40).
The presence of type 2 diabetes also conferred an increased risk of CbVD, although the RR were lower than for IHD, with little difference between men and women (men: age adjusted RR 1.25 95% CI 1.10, 1.42, age and SES adjusted RR 1.24 95% CI 1.13, 1.36; women: age adjusted RR 1.33 95% CI 1.18, 1.51, age and SES adjusted RR 1.31 95% CI 1.18, 1.45). Again, the RRs were higher when the broader definition of CbVD mortality was applied (men: 1.49 95% CI 1.36, 1.63; women: 1.59 95% CI 1.43, 1.77). Relative risks of IHD and CbVD associated with diabetes stratified by SES are shown in table 2. There were no statistically significant multiplicative interactions between deprivation and type 2 diabetes but there were lower relative risks associated with type 2 diabetes in more deprived than among less deprived quintiles (see Table 2)).
Table 2. Age-adjusted mortality risk ratios for ischaemic heart disease and cerebrovascular disease mortality, by sex and socioeconomic status, comparing people with and without type 2 diabetes, estimated from negative binomial regression models.
| Socioeconomic status quintile | Ischaemic heart disease | Cerebrovascular disease | ||
|---|---|---|---|---|
|
| ||||
| Men | Women | Men | Women | |
| 1 (least deprived) | 1.94 (1.61, 2.33) | 2.84 (2.12, 3.80) | 1.38 (1.12, 1.70) | 1.64 (1.32, 2.05) |
| 2 | 1.86 (1.55, 2.23) | 2.50 (1.89, 3.32) | 1.45 (1.19, 1.76) | 1.40 (1.13, 1.74) |
| 3 | 1.75 (1.46, 2.09) | 2.20 (1.67, 2.91) | 1.13 (0.93, 1.37) | 1.36 (1.10, 1.68) |
| 4 | 1.61 (1.35, 1.92) | 2.20 (1.67, 2.91) | 1.22 (1.00, 1.47) | 1.16 (0.94, 1.43) |
| 5 (most deprived) | 1.46 (1.23, 1.74) | 2.04 (1.55, 2.69) | 1.07 (0.89, 1.30) | 1.07 (0.87, 1.32) |
| P-value for interaction* (Likelihood ratio test) | 0.192 | 0.527 | 0.154 | 0.055 |
Interaction between socioeconomic status and diabetes status on mortality
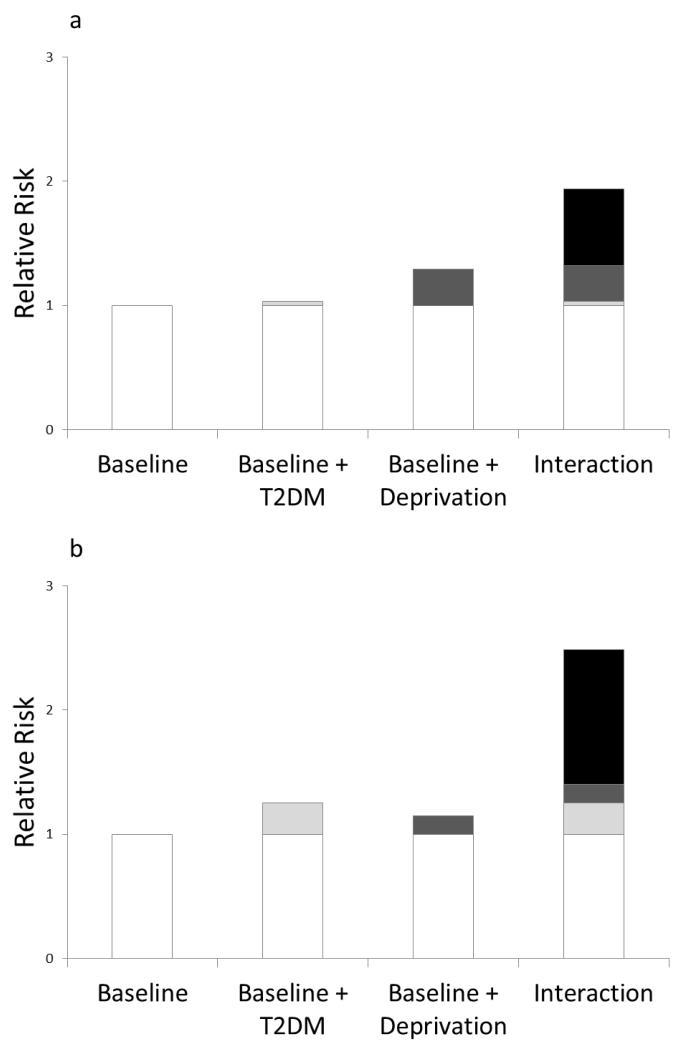
In addition there was evidence of a non-statistically significant supra-additive interaction between diabetes and SES for IHD mortality (RERI 0.63 and synergy index=2.98 for men; RERI 1.09 and synergy index=3.70 for women, see table 1 in supplementary web data for more information). The excess risks due to diabetes and being in the most compared to the least deprived quintile and their interaction after adjusting for age are shown by sex in figure 3. For CbVD, estimates of the synergy index and relative excess risk due to interaction had wide confidence intervals and are therefore difficult to interpret (data available from authors).
Figure 3. Contribution to age-adjusted relative risk of ischaemic heart disease from type 2 diabetes, SES and effect modification of diabetes by SES, comparing quintile 5 to quintile 1 for men and women.
White block, baseline relative risk; Light grey block, relative risk due to type 2 diabetes; Dark grey block, relative risk due to deprivation; Black block, relative risk due to interaction between deprivation and type 2 diabetes
IHD = ischaemic heart disease; T2DM= type 2 diabetes mellitus
When we restricted our analyses to patients included in the diabetes register between 2005 and 2007 we found similar results, albeit with less precision, given the smaller sample size (data available from authors).
Discussion
Using a national diabetes register with near-complete population coverage we found that absolute rates of cardiovascular mortality increased with increasing deprivation and were higher among people with type 2 diabetes than those without diabetes. There was no evidence of both multiplicative and additive interaction between diabetes and SES.
The relationship between cardiovascular mortality and SES may be mediated partly by an increased prevalence of cardiovascular risk factors among lower socioeconomic groups [21]. However, a previous study of diabetes register data from two areas of Scotland found little difference by SES in control of blood pressure, cholesterol levels or diabetes suggesting that there is equitable treatment of these risk factors [5]. In contrast, other risk factors that require behaviour change including smoking and obesity were more common in lower compared with higher socioeconomic groups [5]. Although the Scottish Health Survey contains data on risk factor prevalence on a survey sample, similar data for the whole non-diabetic population included in our analyses were not available. Consequently we were unable to investigate to what extent differences in risk factor patterns contribute to the observed differences in cardiovascular mortality between people with and without diabetes at a population level.
Current predictive models for coronary heart disease in people with diabetes include factors such as age, sex, smoking status, glycaemic control, cholesterol and blood pressure [14, 15], but do not include SES. Inclusion of social deprivation improves cardiovascular risk prediction in the ASSIGN score, a cardiovascular risk score, when compared to the Framingham score in a Scottish population and allow targeting preventive treatment for the most socially deprived groups [22]. Similarly, QRISK2, which also includes a deprivation measure (the Townsend score) performs better than Framingham in identifying high risk populations for cardiovascular disease [23]. Further work is required to investigate whether the inclusion of SES improves the predictive capabilities of cardiovascular disease prediction models for people with diabetes.
Comparisons with previous studies
The observed increase in cardiovascular disease mortality associated with diabetes is in keeping with results of previous studies, which report an increased risk of around two- to three-fold [24-32]. The overall RR we obtained for diabetes are slightly lower than in studies from other parts of the UK [30, 31], and from some other countries [24, 25, 27, 29]. We found that presentation of an overall RR for diabetes and cardiovascular disease mortality masks differences by SES in the Scottish population. Differences in distribution of SES may contribute to differences in the effect of diabetes on mortality between populations. Some of the variability in the findings of previous studies is due to differences in cardiovascular death coding, particularly whether underlying cause of death only or secondary causes of death are counted. The former method, which we used in our main analysis, is likely to result in conservative RR estimates as demonstrated by the higher relative risks reported from our sensitivity analyses using mention of cardiovascular disease anywhere on the death certificate when the underlying cause of death was reported as diabetes. This broader definition may overestimate cardiovascular death rates among people with diabetes because it will include cardiovascular disease reported in part II of the death certificate (i.e. as a condition that has contributed to death but is not part of the main causal sequence leading to death) when comparable information is not available for the non-diabetic population. Lower relative risks in our study might also partly reflect the decreasing relative mortality associated with diabetes over time that has been observed in studies of time trends [29,33].
Our finding that the relative risk of cardiovascular mortality associated with diabetes is higher in women than men also concurs with the findings of previous studies [25, 34]. Recent evidence suggests that this gender difference might be due to women with diabetes having greater relative differences when compared to women without diabetes in cardiovascular risk factors including abdominal adiposity, insulin resistance and inflammation, than similar comparisons for men [35].
Results from previous studies that examined the effect of SES on cardiovascular mortality in people with diabetes have been mixed. In the UK, a study using the South Tees district Diabetes Register found increasing cardiovascular mortality with increasing area-based deprivation [9]. Other studies have examined the effect of individual SES measures on cardiovascular mortality, including the Whitehall Study, which found increasing cardiovascular mortality with decreasing occupational social class [6]. An analysis of US health survey data showed increasing cardiovascular mortality with decreasing education level in people with type 2 diabetes [7]. In contrast, an Italian diabetes register found no association between individual educational level and cardiovascular mortality [13]. Comparisons of Finnish data over time found widening socioeconomic disparities in cardiovascular mortality by social class in people with type 2 diabetes [11, 12]. The findings of the different studies suggest that both individual and area-based SES influence the effect of diabetes on cardiovascular mortality. These studies also reported that the RR for diabetes and IHD mortality were higher than those for CbVD mortality, similar to our findings.
We are not aware of any other studies that have compared area-based SES gradients in cardiovascular mortality between people with and without diabetes. However, two studies have compared individual-based SES gradients in cardiovascular mortality. One study found that the social class gradients in cardiovascular or IHD mortality did not differ by diabetic status [6]. However, this study included only men and very few cases of diabetes and may have therefore been underpowered to detect differences in SES mortality gradients. A second study found that the relative difference in cardiovascular mortality risk was greater in the highest than the lowest educated group, similar to the pattern we report [13]. The South Tees study reported that relative differences in all-cause mortality were highest in the most deprived groups and decreased with increasing affluence but did not report RR for cardiovascular disease mortality stratified by SES [9]. The differences between our study and the latter study might reflect secular trends and better management of cardiovascular risk factors, particularly in people with diabetes, since the latter study was performed in 1994-1999 [33, 36].
Study strengths
Our study includes data on over 99% of people diagnosed with type 2 diabetes in Scotland in recent years, and is therefore at minimal risk of selection bias. With data on over 200,000 people with type 2 diabetes and almost 15,000 cardiovascular deaths, this is the largest study to date to have examined the relationship between cardiovascular disease mortality and SES, with sufficient power to stratify by sex and SES, and to examine IHD and CbVD mortality separately. We were also able to make comparisons using routinely collected national data on cardiovascular mortality, removing all deaths and follow-up time for people with diabetes from this comparison group to generate a non-diabetic comparison group.
Study limitations
Our study has some limitations
Although the diabetes register includes data on cardiovascular risk factors such as blood pressure and body mass index, these data were not available for the general population comparison group and we were therefore unable to investigate the effect of such variables. Type of diabetes was determined from a combination of clinical record, age at onset and prescription records and there may be some misclassification. We were also unable to examine whether individual-based measures of SES, such as education and occupational social class, followed the same pattern of association with diabetes status and cardiovascular disease mortality as the area-based measure of SES. There are some limitations to using routinely collected data in that errors (e.g. in the coding of cause of death) will have occurred. Death coding errors are unlikely to have varied systematically by SES but it is possible that accuracy of recording of cause of death varies by diabetes status. A final potential limitation is that the diabetes register does not include all people who had diabetes who died prior to 2004/5. Therefore, people included in the early period of the register might be unrepresentative in that they reflect a healthier sub-group. However, when we restricted our analyses to only people included in the register between 2005 and 2007, we obtained very similar results suggesting that this limitation does not introduce serious bias.
Conclusions and implications
There is a marked socio-economic gradient in cardiovascular disease mortality for both people with diabetes and the non-diabetic population and the absolute increase in risk associated with diabetes increased modestly with increasing deprivation. These findings demonstrate the potential impact of type 2 diabetes prevention on cardiovascular mortality and highlight the need for sustained efforts to prevent and reduce cardiovascular risk in populations living in more deprived areas, irrespective of diabetes status. The role of SES as an independent predictor of cardiovascular disease in models of vascular outcomes for people with diabetes should be explored further. Prevention of diabetes may contribute to reducing socio-economic health inequalities.
Acknowledgements
These data were available for analysis by members of the Scottish Diabetes Research Network (SDRN) thanks to the hard work and dedication of NHS staff across Scotland who enter the data and people and organisations (the Scottish Care Information -Diabetes Collaboration [SCI-DC] Steering Group, the Scottish Diabetes Group, the Scottish Diabetes Survey Group, the managed clinical network managers and staff in each Health Board) involved in setting up, maintaining and overseeing SCI-DC. The SDRN receives core support from the Chief Scientist Office at the Scottish Government Health Department. The costs of data linkage were covered by the Scottish Government Health Department. This work was funded by the Wellcome Trust through the Scottish Health Informatics Programme (SHIP) Grant (Ref WT086113). SHIP is a collaboration between the Universities of Aberdeen, Dundee, Edinburgh, Glasgow and St Andrews and the Information Services Division of NHS Scotland. We thank Carole Hart for supplying the Excel spreadsheet needed to estimate relative excess risk of interaction. Caroline Jackson was funded by the Chief Scientist Office and the Medical Research Council. We thank David McAllister for his helpful comments on the draft manuscript.
Abbreviations
- CbVD
Cerebrovascular disease
- IHD
Ischaemic heart disease
- NHS NSS
National Health Service National Services Scotland
- RERI
Relative excess risk due to interaction
- SCI-DC
Scottish Care Information – Diabetes Collaboration
- SES
Socioeconomic status
- SIMD
Scottish Index of Multiple Deprivation
Footnotes
The authors declare that there is no duality of interest associated with this manuscript
References
- 1.Dalstra JAA, Kunst AE, Borrell C, et al. Socioeconomic differences in the prevalence of common chronic diseases: an overview of eight European countries. Int J Epidemiol. 2005;34:316–326. doi: 10.1093/ije/dyh386. [DOI] [PubMed] [Google Scholar]
- 2.Connolly V, Unwin N, Sherriff P, Bilous R, Kelly W. Diabetes prevalence and socioeconomic status: a population based study showing increased prevalence of type 2 diabetes mellitus in deprived areas. J Epidemiol Community Health. 2000;54:173–177. doi: 10.1136/jech.54.3.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Evans JM, Newton RW, Ruta DA, MacDonald TM, Morris AD. Socioeconomic status, obesity and prevalence of Type 1 and Type 2 diabetes mellitus. Diabet Med. 2000;17:478–480. [PubMed] [Google Scholar]
- 4.Ismail AA, Beeching NJ, Gill GV, Bellis MA. Capture-recapture-adjusted prevalence rates of Type 2 diabetes are related to social deprivation. QJM. 2011;92:707–710. doi: 10.1093/qjmed/92.12.707. [DOI] [PubMed] [Google Scholar]
- 5.Wild S, MacLeod F, McKnight J, et al. Impact of deprivation on cardiovascular risk factors in people with diabetes: an observational study. Diabet Med. 2008;25:194–195. doi: 10.1111/j.1464-5491.2008.02382.x. [DOI] [PubMed] [Google Scholar]
- 6.Chaturvedi N, Jarrett J, Shipley MJ, Fuller JH. Socioeconomic gradient in morbidity and mortality in people with diabetes: cohort study findings from the Whitehall study and the WHO multinational study of vascular disease in diabetes. BMJ. 1998;316:100–106. doi: 10.1136/bmj.316.7125.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dray-Spira R, Gary-Webb TL, Brancati FL. Educational disparities in mortality among adults with diabetes in th U.S. Diabetes Care. 2010;33(6):1200–1205. doi: 10.2337/dc09-2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robinson N, Lloyd CE, Stevens LK. Social deprivation and mortality in adults with diabetes mellitus. Diabet Med. 1998;15:205–212. doi: 10.1002/(SICI)1096-9136(199803)15:3<205::AID-DIA519>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 9.Roper NA, Bilous RW, Kelly WF, Unwin NC, Connolly VM. Excess mortality in a population with diabetes and the impact of material deprivation: longitudinal, population based study. BMJ. 2001;322:1389–1393. doi: 10.1136/bmj.322.7299.1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Walker J, Livingstone S, Colhoun HM, et al. The effect of socioeconomic status on mortality among people with type 2 diabetes: a study from the Scottish Diabetes Research Network epidemiology group. Diabetes Care. 2011;34:1127–1132. doi: 10.2337/dc10-1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koskinen SVP, Martelin TP, Valkonen T. Socioeconomic differences in mortality among diabetic people in Finland: five year follow up. BMJ. 1996;313:975. doi: 10.1136/bmj.313.7063.975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Forssas E, Keskimaki I, Reunanen A, Koskinen S. Widening socioeconomic mortality disparity among diabetic people in Finland. Eur J Public Health. 2003;13:38–43. doi: 10.1093/eurpub/13.1.38. [DOI] [PubMed] [Google Scholar]
- 13.Gnavi R, Petrelli A, Demaria M, Spadea T, Carta Q, Costa G. Mortality and educational level among diabetic and non-diabetic population in the Turin Longitudinal Study: a 9-year follow-up. Int J Epidemiol. 2004;33:864–871. doi: 10.1093/ije/dyh089. [DOI] [PubMed] [Google Scholar]
- 14.Cederholm J, Eeg-Olofsson K, Eliasson B, Zethelius B, Nilsson P, Gudbjornsdottir S, on behalf of the Swedish National Diabetes Register Risk prediction of cardiovascular disease in type 2 diabetes. A risk equation from the Swedish National Diabetes Register. Diabetes Care. 2008;31:2038–2043. doi: 10.2337/dc08-0662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stevens RJ, Kothari V, Adler AI, Stratton M, Holman R, United Kingdom Prospective Diabetes Study (UKPDS) Group The UKPDS risk engine: a model for the risk of coronary heart disease in Type II diabetes (UKPDS 56) Clin Sci. 2001;101:671–679. [PubMed] [Google Scholar]
- 16.Kendrick SW, Clarke JA. The Scottish Record Linkage system. Health Bull. 1993;51:72–79. [PubMed] [Google Scholar]
- 17.The Scottish Government [accessed on 12th March 2012];Scottish Index of Multiple Deprivation. 2011 http://www.scotland.gov.uk/Topics/Statistics/SIMD.
- 18.Cameron AC, Trivedi PK. Regression Analysis of Count Data. Cambridge University Press; Cambridge: 1998. [Google Scholar]
- 19.Andersson T, Alfredsson L, Kallberg H, Zdravkovic S, Ahlbom A. Calculating measures of biological interaction. Eur J Epidemiol. 2005;20(7):575–579. doi: 10.1007/s10654-005-7835-x. [DOI] [PubMed] [Google Scholar]
- 20.Ahlbom A, Alfredsson L. Interaction: a word with two meanings creates confusion. Eur J Epidemiol. 2005;20:563–564. doi: 10.1007/s10654-005-4410-4. [DOI] [PubMed] [Google Scholar]
- 21.Hotchkiss JW, Davies C, Gray L, Bromley C, Capewell S, Leyland A. Trends in adult cardiovascular disease risk factors and their socio-economic patterning in the Scottish population 1995-2008: cross-sectional surveys. BMJ Open. 2011 doi: 10.1136/bmjopen-2011-000176. doi:10.1136/cmjopen-2011-000176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Woodward M, Brindle P, Tunstall-Pedoe H. Adding social deprivation and family history to cardiovascular risk assessment: the ASSIGN score from the Scottish Heart Health Extended Cohort (SHHEC) Heart. 2007;93:172–176. doi: 10.1136/hrt.2006.108167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Collins G, Altman D. An independent and external validation of QRISK2 cardiovascular disease risk score: a prospective open cohort study. BMJ. 2010;330:c2442. doi: 10.1136/bmj.c2442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Asia Pacific Cohort Studies Collaboration The effects of diabetes on the risks of major cardiovascular diseases and death in the Asia-Pacific region. Diabetes Care. 2003;26:360–366. doi: 10.2337/diacare.26.2.360. [DOI] [PubMed] [Google Scholar]
- 25.Dale AC, Nilsen TI, Vatten L, Midthjell K, Wiseth R. Diabetes mellitus and risk of fatal ischaemic heart disease by gender: 18 years follow-up of 74 914 individuals in the HUNT 1 study. Eur Heart J. 2007;28:2924–2929. doi: 10.1093/eurheartj/ehm447. [DOI] [PubMed] [Google Scholar]
- 26.De Marco R, Locatelli F, Zoppini G, Verlato G, Bonora E, Muggeo M. Cause-specific mortality in type 2 diabetes. The Verona Diabetes Study. Diabetes Care. 1999;22:756–761. doi: 10.2337/diacare.22.5.756. [DOI] [PubMed] [Google Scholar]
- 27.Gu K, Cowie CC, Harris MI. Mortality in adults with and without diabetes in a national cohort of the US population, 1971-1993. Diabetes Care. 1998;21:1138–1145. doi: 10.2337/diacare.21.7.1138. [DOI] [PubMed] [Google Scholar]
- 28.Mulnier HE, Seaman HF, Raleigh VS, et al. Risk of stroke in people with type 2 diabetes in the UK: a study using the General Practice Research Database. Diabetologia. 2006;49:2859–2865. doi: 10.1007/s00125-006-0493-z. [DOI] [PubMed] [Google Scholar]
- 29.Preis SR, Hwang SJ, Coady S, et al. Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the Framingham Heart Study, 1950-2005. Circulation. 2009;119:1728–1735. doi: 10.1161/CIRCULATIONAHA.108.829176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roper NA, Bilous RW, Kelly WF, Unwin NC, Connolly VM. Cause-specific mortality in a population with diabetes. Diabetes Care. 2002;25:43–48. doi: 10.2337/diacare.25.1.43. [DOI] [PubMed] [Google Scholar]
- 31.Swerdlow AJ, Jones ME. Mortality during 25 years of follow-up of a cohort with diabetes. Int J Epidemiol. 1996;25:1250–1261. doi: 10.1093/ije/25.6.1250. [DOI] [PubMed] [Google Scholar]
- 32.The Emerging Risk Factors Collaboration Diabetes mellitus, fasting glucose, and risk of cause-specific death. NEJM. 2011;364:829–841. doi: 10.1056/NEJMoa1008862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gulliford MC, Charlton J. Is relative mortality of type 2 diabetes mellitus decreasing? Am J Epidemiol. 2008;169:455–461. doi: 10.1093/aje/kwn342. [DOI] [PubMed] [Google Scholar]
- 34.Huxley R, Barzi F, Woodward M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ. 2006;332:73–78. doi: 10.1136/bmj.38678.389583.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wannamethee SG, Papacosta O, Lawlor DA, et al. Do women exhibit greater differences in established and novel risk factors between diabetes and non-diabetes than men? The British Regional Heart Study and British Women’s Heart Health Study. Diabetologia. 2012;50:80–87. doi: 10.1007/s00125-011-2284-4. [DOI] [PubMed] [Google Scholar]
- 36.Charlton J, Latinovic R, Gulliford MC. Explaining the decline in early mortality in men and women with type 2 diabetes. Diabetes Care. 2008;31:1761–1766. doi: 10.2337/dc08-0137. [DOI] [PMC free article] [PubMed] [Google Scholar]