Background: Vitamin K intestinal absorption is poorly understood.
Results: Modulating SR-BI and CD36 expression or function in cells and in mice led to control of vitamin K1 intestinal transport.
Conclusion: Intestinal scavenger receptors impact vitamin K1 transport through the enterocyte.
Significance: Understanding vitamin K1 intestinal absorption is crucial to maintain an optimal vitamin K status.
Keywords: Cell Culture, Intestine, Scavenger Receptor, Transgenic Mice, Vitamin K, Intestinal Absorption
Abstract
Vitamin K1 (phylloquinone) intestinal absorption is thought to be mediated by a carrier protein that still remains to be identified. Apical transport of vitamin K1 was examined using Caco-2 TC-7 cell monolayers as a model of human intestinal epithelium and in transfected HEK cells. Phylloquinone uptake was then measured ex vivo using mouse intestinal explants. Finally, vitamin K1 absorption was compared between wild-type mice and mice overexpressing scavenger receptor class B type I (SR-BI) in the intestine and mice deficient in cluster determinant 36 (CD36). Phylloquinone uptake by Caco-2 cells was saturable and was significantly impaired by co-incubation with α-tocopherol (and vice versa). Anti-human SR-BI antibodies and BLT1 (a chemical inhibitor of lipid transport via SR-BI) blocked up to 85% of vitamin K1 uptake. BLT1 also decreased phylloquinone apical efflux by ∼80%. Transfection of HEK cells with SR-BI and CD36 significantly enhanced vitamin K1 uptake, which was subsequently decreased by the addition of BLT1 or sulfo-N-succinimidyl oleate (CD36 inhibitor), respectively. Similar results were obtained in mouse intestinal explants. In vivo, the phylloquinone postprandial response was significantly higher, and the proximal intestine mucosa phylloquinone content 4 h after gavage was increased in mice overexpressing SR-BI compared with controls. Phylloquinone postprandial response was also significantly increased in CD36-deficient mice compared with wild-type mice, but their vitamin K1 intestinal content remained unchanged. Overall, the present data demonstrate for the first time that intestinal scavenger receptors participate in the absorption of dietary phylloquinone.
Introduction
The term “vitamin K” represents a group of fat-soluble molecules essential for the conversion of glutamic acid into γ-carboxyglutamic acid residues in specific substrate proteins. These proteins include active blood-clotting factors, osteocalcin and matrix γ-carboxyglutamic acid protein (1). Real deficiencies in vitamin K are rare. However, because it was recently shown to be involved in bone and artery calcification, optimal vitamin K status may prevent certain cardiovascular diseases and osteoporosis (1, 2). Moreover, patients with fat malabsorption disorders (biliary tract disease, pancreatic insufficiency, cystic fibrosis, etc.) present with reduced vitamin K status if they do not receive adequate supplementation. Vitamin K status in infants is also very precarious, and oral administration at birth and during the first few months of life is often recommended (3). Ensuring adequate vitamin K status at all ages is thus essential.
In the human diet, vitamin K is mainly consumed as vitamin K1 (phylloquinone), found in leafy green vegetables and in certain vegetable oils, including soybean and olive oil. Menaquinones are the other class of vitamin K found in the diet (vitamin K2 family). Mainly provided by liver and fermented products, such as cheese and natto, the vitamin K2 family only accounts for 10–25% of vitamin K in the Western diet (4).
To date, the mechanisms of vitamin K intestinal absorption remain largely unknown. Vitamin K1 has been proposed to be absorbed via an active transport protein in the small intestine (5), but this carrier protein has not yet been identified (6). Vitamin K transport and metabolism in the intestinal cell is also not clearly defined, but phylloquinone is believed to enter the blood circulation as a component of chylomicrons, which are subsequently taken up by the liver. Afterward, vitamin K is mainly found in triglyceride-rich lipoproteins (4, 7). Vitamin K is extensively catabolized. In the liver, it is found as menaquinone-7 to -13 (8), and in peripheral tissues, it is found as phylloquinone and/or menaquinone-4, believed to be formed in situ from menadione (9). This metabolic pathway was shown to occur in the intestine as well (10).
It is widely accepted that vitamin E interferes with vitamin K activity, sometimes inducing extensive bleeding in supplemented patients (11). Although it has been confirmed that excess of α-tocopherol could affect phylloquinone metabolism, the mechanisms of this phenomenon have not been fully elucidated (12). We suggest that a competition with vitamin E could also take place with uptake transporters in the intestine and would thus lead to decreased vitamin K absorption.
The objectives of this study were to investigate the mechanisms of vitamin K1 intestinal absorption, to evaluate the possibility of competition for absorption with vitamin E, and to specify the involvement of two transporters with broad specificity in this process: SR-BI2 and CD36.
MATERIALS AND METHODS
Chemicals
Phylloquinone (≥96% pure), 2-oleoyl-1-palmitoyl-sn-glycero-3-phosphocholine (phosphatidylcholine), 1-palmitoyl-sn-glycero-3-phosphocholine (lysophosphatidylcholine), monoolein, free cholesterol, oleic acid, sodium taurocholate, dicyclohexylcarbodiimide, hydroxysulfosuccinimide sodium salt, and dimethylsulfoxide (DMSO) were purchased from Sigma-Aldrich. Vitamin K1 2,3-epoxide was obtained from Santa Cruz Biotechnology, Inc. R,R,R-α-Tocopherol (vitamin E) and echinenone (≥95% pure) were a generous gift of DSM Ltd. (Basel, Switzerland).
Mouse monoclonal IgG raised against the external domain (amino acids 104–294) of human SR-BI, also known as CLA-1, was purchased from BD Transduction Laboratories (Lexington, KY). Anti-human CD13 antibody (used as a control antibody against another plasma membrane protein) was from Santa Cruz Biotechnology. Mouse monoclonal anti-human CD36 IgM was purchased from Sigma. BLT1 (blocks lipid transport 1; i.e. 2-hexyl-1-cyclopentanone thiosemicarbazone, a chemical inhibitor of lipid transport mediated by SR-BI) was purchased from Chembridge (San Diego, CA). Sulfo-N-succinimidyl oleate (SSO) was synthesized as described previously (13). Dulbecco's modified Eagle's medium (DMEM) containing 4.5 g/liter glucose and trypsin-EDTA (500 and 200 mg/liter, respectively), non-essential amino acids, penicillin/streptomycin, and PBS was purchased from Invitrogen, and fetal bovine serum (FBS) came from PAA (Vélizy-Villacoublay, France).
Human SR-BI cDNA cloned in pCDNA3.1 plasmid was a generous gift of Gerald Gaibelet (INSERM U1048, Toulouse, France), and empty pCDNA3.1 plasmid was a gift from Franck Peiretti (UMR NORT, Marseille, France). Human CD36 in pIRES plasmid and empty pIRES plasmid were provided by Jean-François Landrier (UMR NORT, Marseille, France). LC-MS grade ethanol (EtOH), methanol (MeOH), and 2-propanol (Merck) were used for liquid chromatography-mass spectrometry analysis. All other solvents used were HPLC grade from Carlo Erba (Val de Reuil, France). Formic acid (HCOOH) was purchased from Merck. Deionized water was purified by a Milli-Q water purification system (Millipore, Molsheim, France).
Preparation of Vitamin K1-enriched Vehicles for Cell and Mouse Experiments
Vitamin K1-rich Micelles
For delivery of phylloquinone to Caco-2 cells or to mouse intestinal explants, mixed micelles with lipid composition similar to those found in vivo (14) were prepared as described previously (15) to obtain the following final concentrations: 0.04 mm phosphatidylcholine, 0.16 mm lysophosphatidylcholine, 0.3 mm monoolein, 0.1 mm free cholesterol, 0.5 mm oleic acid, and 5 mm taurocholate (16). Phylloquinone was added into the micelles at a concentration of 0.25–5 μm, depending on the experiment. Concentration of vitamin K1 in the micellar solutions was confirmed before each experiment.
Vitamin K1-rich Complete Medium
For delivery of phylloquinone to HEK cells, an appropriate volume of vitamin K1 stock solution in ethanol was added to a glass tube to obtain a final concentration of 2.5 μm unless otherwise indicated. Stock solution solvent was carefully evaporated under nitrogen. Dried residue was solubilized into FBS overnight, and DMEM was then added to reach a final FBS concentration of 10%. The concentration of phylloquinone in the medium was confirmed before each experiment.
Vitamin K1-rich Emulsions
For delivery of phylloquinone to mice, emulsions were prepared as follows. An appropriate volume of stock solution containing 500 μg of phylloquinone was transferred to an Eppendorf tube. Stock solution solvent was carefully evaporated under nitrogen. Dried residue was solubilized in 100 μl of peanut oil (Lesieur, Asnières-sur-Seine, France), and 200 μl of a NaCl 0.9% solution was added. The mixture was vigorously mixed in an ice-cold water bath during sonication (Branson 3510) for 15 min and used for force-feeding within 10 min of preparation.
Cell Culture
Caco-2 Cell Culture
Caco-2 clone TC-7 cells (17, 18) were cultured in the presence of DMEM supplemented with 20% heat-inactivated FBS, 1% non-essential amino acids, and 1% antibiotics (complete medium), as described previously (13, 19). For each experiment, cells were seeded and grown on transwell plates for 21 days to obtain confluent and highly differentiated cell monolayers. Twelve hours prior to each experiment, serum-free complete medium was used in the apical and basolateral chambers.
HEK Cell Culture and Transfection
HEK 293-T cells were purchased from the American Type Culture Collection (Manassas, VA). Cells were cultured in 10% FBS complete medium at 37 °C in a humidified atmosphere of air/carbon dioxide (90:10, v/v) and the medium was changed every 48 h. Monolayers were subcultured with a 4-day passage frequency when they reached a confluence of about 80% and were subsequently treated with 0.25% trypsin-EDTA. For each experiment, cells were seeded at a 1:10 dilution in 6-well plates and transfected 24 h afterward with 3 μg of DNA and 6 μl of Jet PeI per well in a 150 mm NaCl solution, according to the manufacturer's instructions. The medium was then changed 10–12 h after, and cells were grown for an additional 24 h. Transfection efficiency was verified by Western blotting as described previously (15). Briefly, proteins were determined using a bicinchoninic acid kit (Pierce), and 20 mg of protein was used for Western blot analysis. The blotting membrane was incubated with the anti-SR-BI or the anti-human CD36 antibody at a 1:1000 dilution. For visualization, monoclonal anti-mouse IgM or IgG conjugated to alkaline phosphatase (Sigma) was used as a secondary antibody at a 1:5000 dilution.
Characterization of Vitamin K1 Uptake in Cells
Uptake Measurement
At the beginning of each experiment, cell monolayers were washed with 0.5 ml of PBS. For uptake experiments, the apical side of the cell monolayers received the vitamin K1-enriched vehicles (whereas the other side received the serum-free complete medium if applicable). Cells were incubated for 60 min at 37 °C. At the end of each experiment, medium was harvested. Cells were washed twice in 0.5 ml of ice-cold PBS to eliminate adsorbed vitamin K1 and then scraped and collected in 0.5 ml of ice-cold PBS. Absorbed vitamin K1 was estimated as vitamin K1 found in scraped cells plus vitamin K1 found on the opposite side of the cell monolayer (if applicable).
Apical Efflux Measurement
For apical efflux experiments, the cells first received the vitamin K1-rich micelles at the apical side for 4 h. They were then washed three times with PBS and received apical medium containing vitamin K1-free mixed micelles (vitamin K1 acceptors). At the end of each experiment, the apical medium was collected. Cells were washed twice in 0.5 ml of ice-cold PBS to eliminate adsorbed vitamin K1 and then scraped and collected in 0.5 ml of PBS. Vitamin K1 effluxed by cells (i.e. phylloquinone recovered in the apical medium) was expressed as a percentage of vitamin K1 initially absorbed (determined as the total amount of vitamin K1 recovered in cells, apical medium, and basolateral medium together if applicable).
Competition with R,R,R-α-Tocopherol
Phylloquinone uptake was measured after incubation with phylloquinone-rich mixed micelles (2.5 μm) containing α-tocopherol at concentrations ranging from 0 to 50 μm. Similarly, α-tocopherol uptake was measured after incubation with tocopherol-rich micelles (5 μm) containing either no vitamin K1 or 2.5 μm vitamin K1.
Transport Inhibition by BLT1
For uptake experiments, BLT1 was used as described previously (13, 15, 21). Briefly, Caco-2 but not HEK cell monolayers were pretreated with either DMSO (control) or BLT1 at either 50 nm or 10 μm for 1 h. Both Caco-2 and HEK cells then received phylloquinone-enriched vehicles with either DMSO, 50 nm BLT1 or 10 μm BLT1, and uptake was measured as described above.
Uptake Inhibition by Anti-human SR-BI Antibody
For uptake experiments, cell monolayers were incubated for 5 min with 3.75 μg/ml anti-human SR-BI monoclonal antibody raised against the external domain before vitamin K1-rich micelles were added. Previous experiments have shown that this antibody concentration maximally inhibited absorption (15). Anti-human CD13 antibody was used as a control at 3.75 μg/ml.
Uptake Inhibition by SSO
SSO can be used in concentration ranges up to 1.25 mm, but it is classically used between 200 and 500 μm (13). Thus, during experiments, HEK cells received phylloquinone-enriched vehicles supplemented with 400 μm SSO, and uptake was measured as described above.
Efflux Inhibition by BLT1
The cells first received the phylloquinone-rich micelles at the apical side for 4 h. They were then washed two times with PBS and equilibrated in serum-free complete medium for 1 h. The cells then received apical medium containing vitamin K1 acceptors (i.e. vitamin K-free mixed micelles) supplemented with either DMSO or BLT1 at 10 μm for 3 h.
Characterization of Vitamin K1 Uptake in Mouse Intestine
Animals
Wild-type (WT) mice, mice deficient in CD36 (22, 23), and mice overexpressing SR-BI in the intestine (24, 25) were housed in a controlled environment (temperature = 22 ± 2 °C, humidity = 55 ± 10%, darkness from 6 p.m. to 6 a.m.). They were given a standard A04 chow diet (Safe, Augy, France) and water ad libitum. They were fasted overnight before each experiment. The protocol (number 24-25092012) was approved by the local animal research ethics committee (Comité National de Réflexion Ethique sur l'Expérimentation Animale de Marseille 14).
Vitamin K1 Uptake Inhibition in Mouse Intestinal Explants
Mice were fasted overnight, and intestinal explants were prepared as described previously (13). Briefly, on the day of the experiment, animals were euthanized by cervical dislocation, and the 4 cm distal to the first 3 cm of their small intestinal tract were immediately removed. The intestine samples were carefully rinsed with a sterile NaCl solution (0.9%), sliced into strips on ice as described previously (13), and homogeneously distributed in 12-well plates (Falcon Plates, BD Biosciences). Explants were incubated for 3 h in 500 μl of 2.5 μm vitamin K1-enriched mixed micelles supplemented with 10 μm BLT1 or 400 μm SSO or with no supplement. Each condition was performed in triplicate. After incubation, media were harvested, and the intestine explants were carefully rinsed twice in PBS. Samples were then suspended in 500 μl of PBS, homogenized with two 3-mm diameter stainless steel balls in 2-ml Eppendorf tubes using an MM301 ball mill (Retsch, Eragny sur Oise, France), and stored until analysis.
Postprandial Experiment with Vitamin K1
On the day of the experiment, the mice were force-fed with a phylloquinone-enriched emulsion.
To assess the phylloquinone postprandial response curve in WT mice, blood samples were taken by retroorbital puncture at 1.5, 3, 4.5, and 6 h after gavage. A final blood sample was taken at 7.5 h by intracardiac puncture before euthanasia by cervical dislocation.
To compare phylloquinone postprandial response in WT and transgenic mice, a blood sample was taken after 4 h of digestion by intracardiac puncture before euthanasia by cervical dislocation. The intestine of each animal was then quickly harvested, carefully rinsed with PBS, and cut in 6-cm segments (duodenum, proximal jejunum, median jejunum, distal jejunum, and ileum). All of the fragments were suspended in 500 μl of PBS and homogenized as described above before storage and analysis.
All of the samples were sealed under nitrogen and stored at −80 °C until vitamin K1 analysis. Aliquots of cell samples were used to assess protein concentrations using a bicinchoninic acid kit (Pierce).
Sample Acid Hydrolysis
To analyze the potential metabolism of phylloquinone to menadione in enterocytes, 500 μl of cell or WT intestinal sample (cf. above) were deconjugated via acid hydrolysis, which also oxidized the released menadiol to menadione, as described previously (26).
Vitamin K1 Extraction
Phylloquinone was extracted from 500 μl of aqueous sample using the following method. Distilled water was added to sample volumes below 500 μl to reach a final volume of 500 μl. Echinenone was used as an internal standard and added to the samples in 500 μl of ethanol. The mixture was extracted once with 2 ml of hexane. The hexane phase obtained after centrifugation (500 × g, 10 min, 4 °C) was evaporated to dryness under nitrogen, and the dried residue was dissolved in 200 μl of mobile phase. A volume of 100–180 μl was used for HPLC analysis.
Vitamin K UPLC-MS Analysis
Analyses were performed by ultraperformance liquid chromatography using an ACQUITY system (Waters Corp., Milford, MA) linked simultaneously to a diode array detector (UPLC DAD, Waters Corp.) and interfaced with a Bruker Daltonics HCT Ultra Ion Trap mass spectrometer via an atmospheric pressure chemical ionization source operated in positive ion mode (UPLC DAD/APCI-MS). CompassTM software (Bruker Daltonics, Bremen, Germany) was used for mass spectrometric instrument control and data processing.
UPLC conditions were modified from Song et al. (27). Separation was carried out using an ACQUITY UPLC® BEH C18 column (50 mm × 2.1 mm, inner diameter 1.7 μm; Waters). The column temperature was 35 °C, the flow rate was 0.45 ml min−1, and 10 μl was injected. Analysis was achieved using a gradient of Milli-Q water/2-propanol (80:20, v/v) containing 0.1% HCOOH (v/v) (solvent A) and CH3OH containing 0.1% HCOOH (v/v) (solvent B). Gradient conditions of the mobile phase were as follows: A, 85%, 0–3 min; A, 85–5%, 3–8 min; A, 2%, 8–12 min; A, 2–0%, 12–14 min, followed by a return to the initial conditions (solvent A, 85%) and re-equilibration for 4 min. Peaks were detected at 270 nm.
The ion trap was operated in the Ultra Scan mode from m/z 120 to 800. The ICC target was set to 100,000 with a maximum accumulation time of 200 ms. Nitrogen (99.99% purity) was used as the desolvation gas. The source parameters were set as follows: dry temperature 350 °C, nebulizer pressure 50 p.s.i., dry gas flow 5 liters·min−1, vaporizer temperature of 350 °C, capillary voltage −2 kV, and corona current 4000 nA.
Vitamin K HPLC Analysis
Phylloquinone and R,R,R-α-tocopherol were separated using a 250 × 4.6-nm RP C18, 5-μm Zorbax column (Interchim, Montluçon, France) and a guard column.
The isocratic mobile phase consisted of 80% methanol, 19.45% ethanol, and 0.55% H2O containing 1 mm sodium acetate, 2 mm zinc chloride, and 2 mm acetic acid (flow rate = 1.2 ml·min−1), and the column was kept at a constant temperature (35 °C). The HPLC system was composed of a Dionex separation module (P680 HPLC pump and ASI-100 automated sample injector, Dionex, Aix-en-Provence, France), a Dionex UVD340U photodiode array detector, and a Jasco fluorimetric detector (Jasco, Nantes, France). Depending on the quantity of vitamin K present in the sample, phylloquinone was either measured at 248 nm using the photodiode array detector or at 430 nm after light emission at 244 nm using fluorimetric analysis (after postcolumn online reduction to the hydroquinone form in a 4.6 mm × 5-cm column freshly filled with 98% pure zinc dust) and identified by retention time coincident with authentic standard. Quantification was performed using Chromeleon software (version 6.50 SP4 Build 1000) comparing peak area with external calibration curves.
Statistical Analysis
Results are expressed as means ± S.E. Differences between more than two groups of unpaired data were analyzed using the non-parametric Kruskal-Wallis test. The non-parametric Mann-Whitney test was used as a post hoc test when the Kruskal-Wallis test showed significant differences between groups. Differences between only two groups of unpaired data were tested via Mann-Whitney U test. Values of p < 0.05 were considered significant. All statistical analyses were performed using Statview software, version 5.0 (SAS Institute, Cary, NC). Relationships between two variables were examined by regression analysis using KaleidaGraph version 3.6 software (Synergy Software, Reading, PA).
RESULTS
Metabolism of Vitamin K1 by Caco-2 Cells and Mouse Enterocyte
We first aimed to assess whether phylloquinone was metabolized in Caco-2 cells and mouse intestine.
Using the UPLC DAD/APCI-MS conditions described above, vitamin K1 was detected at 11.8 min (Fig. 1A, compound 2), producing a protonated ion [M + H]+ with m/z 451.2. After fragmentation, a daughter ion was detected at m/z 186.8 (Fig. 1B). The analyses of the cell samples incubated with vitamin K1 for either 1 or 24 h did not reveal local production of menadione (data not shown), regardless of whether or not the samples were acid-hydrolyzed. No other metabolites were detected after a 1-h incubation. However, vitamin K1 epoxide was detected after 24 h of incubation (Fig. 1A, compound 1) in the cellular compartment only of both acid hydrolyzed and non-hydrolyzed samples (retention time 10.8 min, m/z 467.2, identical to the standard molecule) (Fig. 1C). To avoid the metabolism of phylloquinone by the cells, cell experiments were conducted with incubation periods of 1 h. UPLC-MS analyses of WT mouse intestinal samples 4 h after force feeding demonstrated that vitamin K1 was the only form of vitamin K detectable in the intestinal mucosa in our experimental conditions (data not shown).
FIGURE 1.
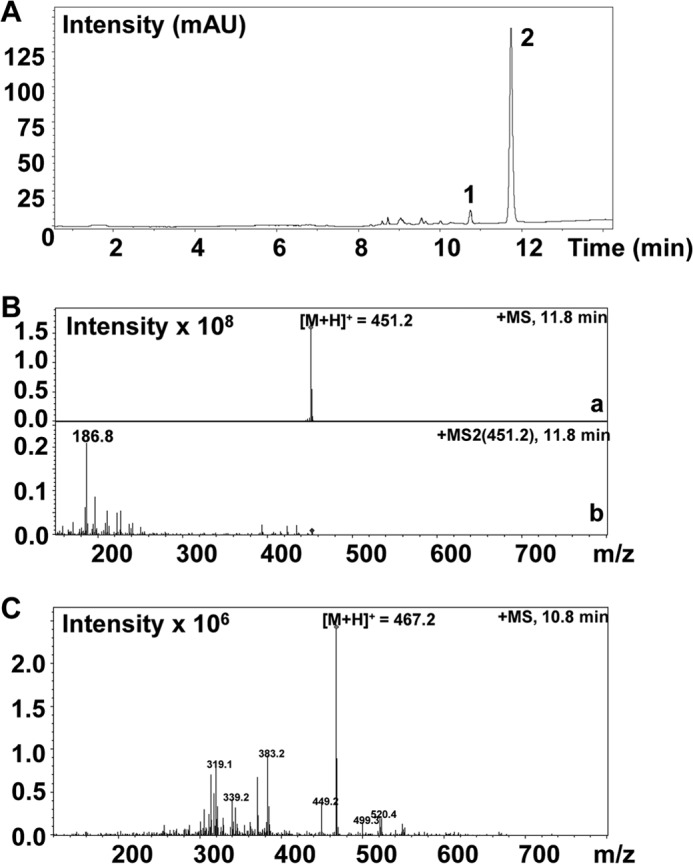
UPLC DAD/APCI-MS analysis of vitamin K1 and its epoxide detected in the Caco-2 cellular compartment extract after a 24-h incubation with 2.5 μm micellar vitamin K1. A, DAD chromatogram of the Caco-2 cellular compartment extract at 270 nm. mAU, milliabsorbance units. Compound 1, vitamin K1 epoxide (retention time = 10.8 min); compound 2, vitamin K1 (retention time = 11.8 min). B, MS (a) and MS2 spectra (b) of vitamin K1 (compound 2). C, MS spectrum of vitamin K1 epoxide (compound 1).
Effect of Micellar Vitamin K1 Concentration on Vitamin K1 Uptake by Caco-2 Cells
We then aimed to characterize vitamin K1 uptake by differentiated Caco-2 cell monolayers.
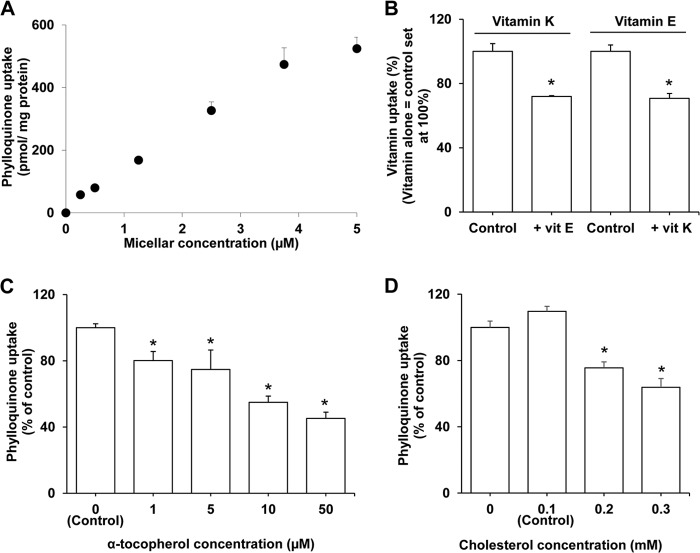
At concentrations ranging from 0.5 to 5 μm, absorption of vitamin K1 was not linear (Fig. 2A). The best fit was achieved using a hyperbolic curve y = ax/(x + b), R2 > 0.99. Apparent Qmax was 1.47 nmol of phylloquinone/mg of protein, and K was equal to 8.58 μm. Qmax represents the maximal amount of phylloquinone absorbed, and K represents the concentration of micellar phylloquinone required to reach Qmax/2.
FIGURE 2.
Characterization of vitamin K1 uptake in Caco-2 TC7 cells. A, effect of vitamin K1 micellar concentration on vitamin K1 uptake by differentiated Caco-2 TC-7 cell monolayers. The apical side received FBS-free medium containing phylloquinone-rich mixed micelles (0.25–5 μm), and the basolateral side received FBS-free medium. Incubation time was 60 min. Data are means ± S.E. (error bars) of three assays. B, competition for uptake by Caco-2 TC-7 cell monolayers between vitamin K1 and α-tocopherol. The apical side received FBS-free medium containing either phylloquinone-rich (2.5 μm) or α-tocopherol-rich (5 μm) mixed micelles alone or phylloquinone- or α-tocopherol-rich mixed micelles supplemented with α-tocopherol or phylloquinone at the same concentrations, respectively. The basolateral side received FBS-free medium. Incubation time was 60 min. Data are means ± S.E. of three assays. C, inhibition of vitamin K1 uptake with increasing concentrations of α-tocopherol in Caco-2 TC-7 cell monolayers. The apical side received FBS-free medium containing 2.5 μm micellar phylloquinone and increasing concentrations of micellar α-tocopherol (ranging from 0 to 50 μm). The basolateral side received FBS-free medium. Incubation time was 60 min. Data are means ± S.E. of three assays. D, inhibition of vitamin K1 uptake by increasing concentrations of cholesterol in Caco-2 TC-7 cell monolayers. The apical side received FBS-free medium containing 2.5 μm micellar phylloquinone and increasing concentrations of micellar cholesterol (ranging from 0 to 300 μm). The basolateral side received FBS-free medium. Incubation time was 60 min. Data are means ± S.E. of three assays.
Effect of Vitamin E Co-incubation on Vitamin K1 Uptake by Caco-2 Cells and Vice Versa
Next, we evaluated whether competition between vitamin K1 and E exists during nutrient uptake in differentiated Caco-2 cell monolayers.
As shown in Fig. 2B, co-incubation of 5 μm micellar α-tocopherol (vitamin E) with 2.5 μm micellar phylloquinone significantly decreased the uptake of phylloquinone by 28.0% (p < 0.05). Similarly, co-incubation of 2.5 μm micellar phylloquinone with 5 μm micellar α-tocopherol significantly decreased the uptake of α-tocopherol by 29.2% (p < 0.05). This effect was dose-dependent, as further shown in Fig. 2C, which suggests that these two vitamins share common uptake pathways.
Effect of the Amount of Cholesterol Incorporated in Micelles with Vitamin K1 on Vitamin K1 Uptake
Cholesterol is naturally present in micelles during digestion, but its concentration may vary depending on diet and biliary secretion. Fig. 2D shows that high micellar cholesterol concentrations significantly affected phylloquinone uptake. This suggests that cholesterol and phylloquinone may also display common uptake pathways.
Interestingly, vitamin E and cholesterol share common protein carriers at the apical side of the enterocyte. Among these transporters, the scavenger receptors SR-BI and CD36 are known to display broad substrate specificity. We thus investigated the involvement of SR-BI and CD36 in vitamin K1 intestinal apical uptake.
Involvement of SR-BI in Vitamin K1 Transport across the Apical Membrane of Caco-2 Cells
Uptake Experiment
The specific chemical inhibitor of SR-BI, BLT1, significantly decreased apical Caco-2 cell phylloquinone uptake by up to 38.5% when added at 50 nm (∼IC50 (28)). When added in excess (10 μm (13, 15, 21, 25, 29)), it led to an inhibition of 84.5% of phylloquinone uptake (Fig. 3A, p < 0.05). Moreover, Fig. 3B shows that the addition of anti-human SR-BI antibody raised against the external domain significantly decreased phylloquinone apical uptake by 15.6% compared with the control antibody (anti-CD13 antibody, p < 0.05). CD36 involvement in vitamin K1 uptake was not challenged in Caco-2 cells because this cell line does not express the protein.
FIGURE 3.
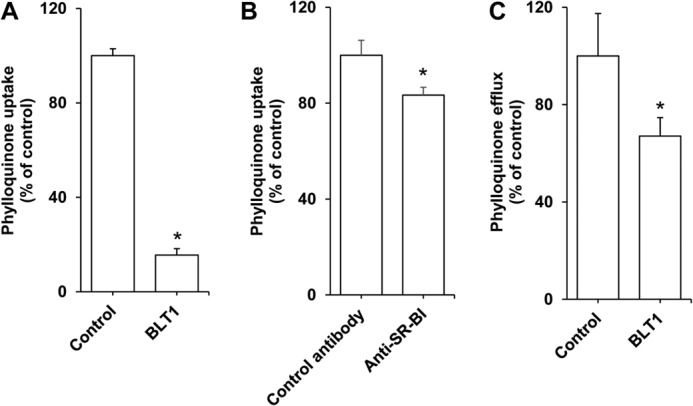
Effect of SR-BI inhibitors on vitamin K1 apical transport by differentiated Caco-2 TC-7 monolayers. A, effect of BLT1 on vitamin K1 uptake. The apical sides of the cell monolayers were preincubated for 60 min with either BLT1 at 10 μm or DMSO (control), before receiving FBS-free medium containing phylloquinone-enriched mixed micelles at a 2.5 μm concentration and supplemented with either BLT1 at 10 μm or DMSO. The basolateral sides received FBS-free medium. Incubation time was 60 min. Data are means ± S.E. (error bars) of three assays. *, significant difference with the control. B, effect of SR-BI-blocking antibody on vitamin K1 uptake. The apical side of the cell monolayers was pre-incubated for 5 min with either 3.75 μg/ml of anti-human SR-BI antibody or 3.75 μg/ml of anti-human CD13 antibody (control), before receiving FBS-free medium containing phylloquinone-enriched mixed micelles at a 2.5 μm concentration. The basolateral side received FBS-free medium. Incubation time was 60 min. Data are means ± S.E. of 3 assays. *, significant difference from the control. C, effect of BLT1 on vitamin K1 apical efflux. Cell monolayers were first enriched in phylloquinone during 4 h. The apical side of the monolayers was then carefully rinsed and received either FBS-free medium containing vitamin K1-free mixed micelles or the same mixture plus BLT1. The basolateral side received FBS-free medium. Efflux time was 60 min. Data are means ± S.E. of three assays. *, significant difference from the control (assay performed without BLT1).
Apical Efflux Experiment
Caco-2 cells were charged in phylloquinone before apical efflux of vitamin K1 was measured in the presence or the absence of BLT1 (Fig. 3C). Adding 10 μm BLT1 to the apical side of the cells in the presence of vitamin K-free mixed micelles significantly reduced the apical efflux of vitamin K1 by 80.5% (Fig. 2B, p < 0.05).
Effect of SR-BI and CD36 Transfection on Vitamin K1 Uptake in HEK Cells
To validate our previous and to extend then to CD36, we then used transfected HEK cells. Transfection with human SR-BI led to a significant 109.6% increase of phylloquinone uptake compared with control (cells transfected with an empty plasmid), and this increase was totally suppressed by 10 μm BLT1 (Fig. 4A). Fig. 4B shows that HEK cell transfection with human CD36 significantly increased phylloquinone uptake by 164.3% and that this increase was significantly impaired by the addition of a chemical inhibitor of CD36, SSO (400 μm). Because SR-BI and CD36 are not endogenously expressed in HEK cells (Fig. 3, insets), neither BLT1 nor SSO had an effect on phylloquinone uptake in untransfected HEK cells (data not shown).
FIGURE 4.
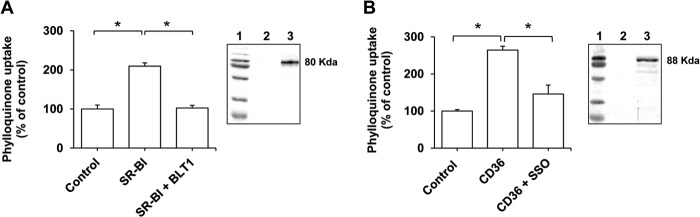
Effect of SR-BI and CD36 inhibitors on vitamin K1 uptake by HEK 293-T cells overexpressing scavenger receptors. A, effect of BLT1 on vitamin K1 uptake by HEK 293-T cells overexpressing SR-BI. Cells were transfected with either an empty pCDNA3.1 plasmid (control) or with a pCDNA3.1 plasmid containing SR-BI (SR-BI). The cell monolayers received then phylloquinone-enriched (2.5 μm) complete medium supplemented or not with BLT1 at 10 μm. Incubation time was 60 min. Data are means ± S.E. (error bars) of three assays. *, significant difference between groups. B, effect of SSO on vitamin K1 uptake by HEK 293-T cells overexpressing CD36. Cells were transfected with either an empty pIRES plasmid (control) or with a pIRES plasmid containing CD36 (CD36). The cell monolayers received then phylloquinone-enriched (2.5 μm) complete medium supplemented or not with SSO at 400 μm. Incubation time was 60 min. Data are means ± S.E. of three assays. *, significant difference between groups. Insets, Western blots of protein expression in HEK cells: size marker (1); control cells (2); HEK cells (3) overexpressing SR-BI (A) or CD36 (B).
Effect of BLT and SSO on Vitamin K1 Uptake by Mouse Intestinal Explants
To further confirm our data, we next performed ex vivo experiments. BLT1 and SSO significantly impaired phylloquinone uptake by mouse intestinal explants (−19.4 and −18.9%, respectively; Fig. 5).
FIGURE 5.
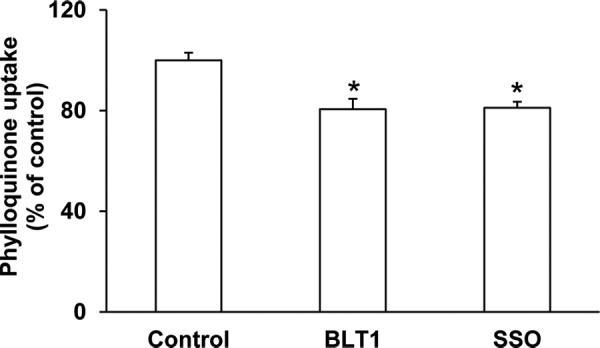
Effect of SR-BI and CD36 inhibitors on vitamin K1 uptake by ex vivo mouse intestinal explants. The mouse intestinal explants received FBS-free medium containing phylloquinone-enriched mixed micelles at 2.5 μm. supplemented with BLT1 at 10 μm concentration, SSO at a 400 μm concentration, or no supplementation. Incubation time was 3 h. Data are means ± S.E. (error bars) of three assays. *, significant difference between groups.
Vitamin K1 Postprandial Response in Mice
Finally, we assessed the phylloquinone postprandial response in mice after gavage (Fig. 6). Each mouse received 500 μg of phylloquinone in an oil-in-water emulsion. Our data show that phylloquinone peaked in plasma between 1.5 and 4.5 h after gavage.
FIGURE 6.
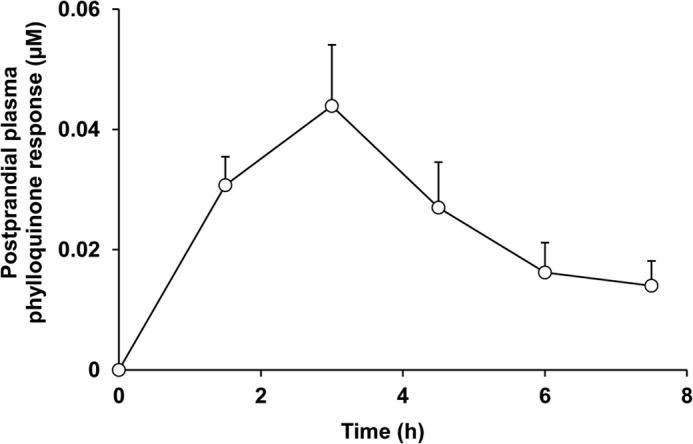
Plasma vitamin K1 response in wild-type mice. Mice were gavaged with a phylloquinone-enriched emulsion (500 μg), and multiple blood samples were taken over 7.5 h to assess plasma phylloquinone concentration. Data are mean ± S.E. (error bars) (n = 5).
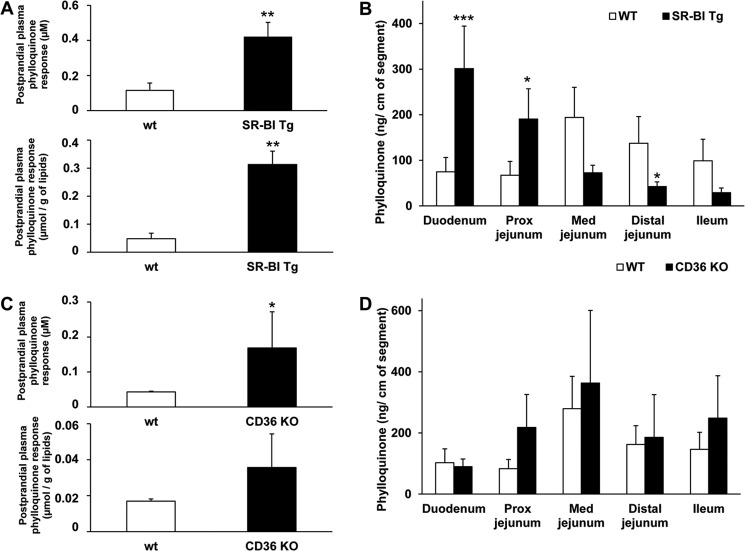
Effect of Intestinal SR-BI Overexpression on Vitamin K1 Absorption in Mice
4 h after gavage, the phylloquinone postprandial response was significantly increased in SR-BI transgenic mice compared with control mice (+162.4%, p = 0.0071; Fig. 6A). This difference was still significant after adjustment by plasma total lipids (+548.9%, p = 0.0011; Fig. 7A). Furthermore, the phylloquinone content of the first two fragments (duodenum and proximal jejunum) of SR-BI transgenic mice was significantly higher than the vitamin K1 content of the first two fragments of WT mice (+302.4%, p = 0.0008 and +183.1%, p = 0.0116; Fig. 7B). Conversely, the phylloquinone content of the last three fragments (median jejunum, distal jejunum, and ileum) of SR-BI transgenic mice was lower than the vitamin K1 content of the matched fragments of WT mice, although the difference was significant in the distal jejunum only (−69.1%, p = 0.0324; Fig. 5B).
FIGURE 7.
Vitamin K1 postprandial response and vitamin K1 content of mouse intestinal fragments in mice after force-feeding with a vitamin K1-enriched emulsion. A, effect of SR-BI overexpression at the intestinal level. Four hours after force feeding with an emulsion containing 500 μg of phylloquinone, a blood sample was taken (A), and mouse intestines were harvested and cut into five fragments (B). Data are means ± S.E. (error bars); n = 8 for control mice and 8 for SR-BI transgenic (Tg) mice). B, effect of CD36 deletion (CD36 KO). Four hours after force feeding with an emulsion containing 500 μg of phylloquinone, a blood sample was taken (C), and mouse intestines were harvested and cut into five fragments (D). Data are means ± S.E.; n = 4 for control mice and 5 for CD36-deficient mice. Prox, proximal; Med, median.
Effect of CD36 Deletion on Vitamin K1 Absorption in Mice
After gavage, the phylloquinone postprandial response was significantly increased in CD36-deficient mice compared with control mice (+290.2%, p = 0.014; Fig. 7C). This difference did not remain significant after adjustment by plasma total lipids. Additionally, the phylloquinone content in all intestinal fragments remained similar in the two groups of mice (Fig. 7D).
DISCUSSION
Phylloquinone intestinal absorption has been poorly investigated so far. To evaluate in detail the mechanism(s) involved in transport across the enterocyte, we used the popular Caco-2 TC-7 cell model, which has been extensively used to study fat-soluble vitamin intestinal absorption (13, 21, 30). There are no data on phylloquinone micellar concentration in the human gut. However, previous work has shown that lutein concentrations in the human duodenal lumen were 5–7 μm after a spinach-rich meal providing ∼10 mg lutein (31). Considering spinach phylloquinone content (32), such a meal would result in the production of micelles containing ∼0.03–0.05 μm phylloquinone. However, to allow an accurate quantification in cells, we used micellar concentrations ranging from 0.25 to 5 μm and principally 2.5 μm.
We first aimed to assess whether vitamin K1 was metabolized by intestinal cells under our experimental conditions. APCI is the most common method of ionization for lipophilic compounds in general, including vitamin K (27, 33, 34). The best detection was obtained in positive mode; thus, this was used for our analysis. The m/z 186.9 daughter ion corresponds to the loss of the side chain, as reported previously (34). A vitamin K1 epoxide was identified in the cytosol of Caco-2 cells after a 24-h incubation of vitamin K1-rich mixed micelles, whereas no metabolites were detected after a 1-h incubation. To avoid phylloquinone degradation and metabolism to accurately measure vitamin K1 transport, all experiments in Caco-2 cells were conducted after short incubation periods, and samples were analyzed by HPLC.
Our first results showed that vitamin K1 uptake is saturable, which supports a protein-mediated uptake hypothesis (35). Apparent Qmax for phylloquinone was in the same range as the apparent Qmax for tocopherol (21). The apparent K for phylloquinone was 10-fold smaller than that of tocopherol, suggesting a greater affinity of the cell brush-border membrane for vitamin K1 than for vitamin E, but these data should be considered cautiously because these values strongly depend on both micelle composition and experimental conditions (Caco-2 cells differentiated on filters, incubation period, etc.). The saturable uptake of vitamin K1 by Caco-2 cells is consistent with the previous findings of Hollander and colleagues, who showed that the use of a nitrogen atmosphere to inhibit mitochondrial respiration and the addition of 2,4-dinitrophenol to inhibit ATP synthesis together impaired phylloquinone intestinal absorption in rats. Although nonspecific experiments, these data suggested the involvement of a carrier protein in phylloquinone uptake (36).
We then explored the possibility of competition between dietary vitamin K1 and α-tocopherol for absorption. The fact that both vitamins could impair the uptake of each other suggests that the two molecules compete for entry into the intestinal cell and thus may share common absorption pathway(s). This situation could be particularly deleterious for vitamin K because its dietary intake is moderate (recommended daily allowance for an adult = 75 μg/day) compared with vitamin E (recommended daily allowance of 15 mg/day), with vitamin E supplementation increasing the imbalance further. This result could at least partially explain the excessive bleeding observed in patients supplemented with vitamin E (11). This result seems in disagreement with previous data obtained in rats and showing a non-significant decrease of phylloquinone serum concentration 6 h after gavage with 0.2 mg of phylloquinone and 10 mg of α-tocopherol (12). However, our data suggest that the phylloquinone absorption peak is probably earlier, around 3–4 h (Fig. 6), and a single measure of phylloquinone postprandial concentration at 6 h cannot exclude possible competition for absorption.
Vitamin E intestinal absorption was shown to involve cholesterol transporters, including scavenger receptors (21, 37). We thus aimed to evaluate the involvement of SR-BI and CD36 in phylloquinone transport across the brush border membrane. The finding that phylloquinone uptake in Caco-2 cells was specifically inhibited by both anti-human SR-BI antibody and BLT1 (a chemical inhibitor of SR-BI) (38, 39), is taken as primary evidence that SR-BI is involved in vitamin K1 uptake. BLT1 led to a 80% decrease in phylloquinone uptake, whereas the antibody led to a 15% decrease only. This difference, already observed previously with vitamin E (21), can be explained by the fact that BLT1 may be more efficient than the antibody to inhibit SR-BI activity. Moreover, the presence of proteases at the brush border membrane may hydrolyze the antibodies.
Interestingly, the role of SR-BI is not restricted to vitamin K1 uptake alone. The transporter was also able to mediate vitamin K1 efflux from the cell to the apical medium, as has been similarly shown for vitamin E (21) and D (13). CD36 involvement could not be evaluated in the Caco-2 monolayers because this cell model does not express the protein (15). Thus, in order to further examine the involvement of both scavenger receptors in phylloquinone transport, we studied phylloquinone uptake using HEK cells transfected with either SR-BI or CD36. HEK cells transfected with SR-BI displayed an increased BLT1-sensitive phylloquinone uptake, confirming SR-BI involvement in vitamin K1 absorption. Similarly, HEK cells transfected with CD36 exhibited SSO-sensitive uptake of phylloquinone, suggesting the involvement of CD36. We then performed an ex vivo experiment using mouse intestinal explants. We observed a significant 20% inhibition of vitamin K1 uptake by BLT1. This inhibition was less pronounced than the inhibition observed in Caco-2 cells treated with BLT1 (80%). This discrepancy is probably due to different transporter expression profiles in vivo and in vitro. We also confirmed the results obtained in HEK cells because SSO impaired phylloquinone uptake by mouse intestinal mucosa. However, the fact that we did not manage to fully inhibit phylloquinone uptake suggests that passive diffusion or other transporters are, at least partially, involved.
Finally, we performed in vivo absorption experiments. Preliminary tests showed that vitamin K1 was not detectable in fasting plasma samples of mice bred in house, and no vitamin K metabolites were detected in mouse intestinal mucosa 4 h after force feeding. The results obtained in mice overexpressing SR-BI in the intestine provide further evidence that SR-BI is directly involved in phylloquinone absorption. Indeed, the phylloquinone postprandial response was significantly increased in transgenic mice compared with wild-type animals. Furthermore, phylloquinone content of the intestinal mucosa of the transgenic mice was very different from the controls. Phylloquinone significantly accumulated in the first fragments of mouse intestine, where SR-BI overexpression is the strongest (24). Conversely, less phylloquinone uptake was recovered in the last intestinal sections, probably because it was largely absorbed in the proximal part of the intestine.
The results obtained in CD36-deficient mice revealed an indirect involvement of this transporter in phylloquinone transport. Indeed, CD36-deficient mice had a higher phylloquinone postprandial response than wild-type mice, contrary to what might be expected if CD36 is mainly implicated in phylloquinone uptake. Deficient mice also had a significantly increased postprandial triglyceride response (data not shown). This result is in agreement with our previous work on γ-tocopherol (37). This result is also in agreement with previous data demonstrating that in the presence of lipids, CD36 induces large chylomicron formation via an induction of both apolipoprotein B48 and microsomal triglyceride transfer protein, probably through ERK1/2 modulation. By contrast, CD36 deletion results in an impaired secretion of chylomicrons that are smaller in size and thus resistant to lipoprotein lipase activity (20, 23, 40), which leads to triacylglycerol and phylloquinone accumulation. The fact that phylloquinone content was similar in WT and CD36-deficient mouse intestinal fragments indicates that CD36 involvement in vitamin K1 uptake may be balanced by the activity of other transporters. Another possibility is that CD36 also impacts chylomicron secretion from the enterocyte to the lymph. A delay in secretion would then result in a temporary accumulation of the chylomicrons in the intestinal cells that would mask a reduced uptake. Because our cell models (CD36-transfected HEK cells) cannot mimic this secretion step, this could also explain the discrepancy between our in vitro and in vivo data. Further studies are required to validate this last assumption.
The physiological consequences of these novel findings remain to be evaluated. We suggest that interindividual variation in intestinal scavenger receptor expression and/or function may be linked to variations in intestinal phylloquinone absorption efficiency. Ultimately, these variations could impact health status in subgroups of population at risk of developing cardiovascular diseases or osteoporosis.
Acknowledgment
We are very grateful to Dr. Rachel Kopec for helpful comments on the manuscript.
This work was supported by a grant from the Société Française de Nutrition (Lu/SFN grant).
- SR-BI
- scavenger receptor class B type I
- CD36
- cluster determinant 36
- SR-BI transgenic mice
- mice overexpressing SR-BI in the intestine
- APCI
- atmospheric pressure chemical ionization
- SSO
- sulfo-N-succinimidyl oleate
- UPLC
- ultraperformance liquid chromatography
- HEK
- human embryonic kidney.
REFERENCES
- 1. Willems B. A., Vermeer C., Reutelingsperger C. P., Schurgers L. J. (2014) The realm of vitamin K dependent proteins: shifting from coagulation toward calcification. Mol. Nutr. Food Res. 58, 1620–1635 [DOI] [PubMed] [Google Scholar]
- 2. Adams J., Pepping J. (2005) Vitamin K in the treatment and prevention of osteoporosis and arterial calcification. Am. J. Health Syst. Pharm. 62, 1574–1581 [DOI] [PubMed] [Google Scholar]
- 3. Martin A. (2001) Apports Nutritionnels Conseillés pour la Population Française, 3rd Ed., pp. 244–248, Lavoisier, Paris [Google Scholar]
- 4. Shearer M. J., Newman P. (2014) Recent trends in the metabolism and cell biology of vitamin K with special reference to vitamin K cycling and MK-4 biosynthesis. J. Lipid Res. 55, 345–362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hollander D., Rim E., Muralidhara K. S. (1977) Vitamin K1 intestinal absorption in vivo: influence of luminal contents on transport. Am. J. Physiol. 232, E69–E74 [DOI] [PubMed] [Google Scholar]
- 6. Reboul E., Borel P. (2011) Proteins involved in uptake, intracellular transport and basolateral secretion of fat-soluble vitamins and carotenoids by mammalian enterocytes. Prog. Lipid Res. 50, 388–402 [DOI] [PubMed] [Google Scholar]
- 7. Saupe J., Shearer M. J., Kohlmeier M. (1993) Phylloquinone transport and its influence on γ-carboxyglutamate residues of osteocalcin in patients on maintenance hemodialysis. Am. J. Clin. Nutr. 58, 204–208 [DOI] [PubMed] [Google Scholar]
- 8. Thijssen H. H., Drittij-Reijnders M. J. (1996) Vitamin K status in human tissues: tissue-specific accumulation of phylloquinone and menaquinone-4. Br. J. Nutr. 75, 121–127 [DOI] [PubMed] [Google Scholar]
- 9. Okano T., Shimomura Y., Yamane M., Suhara Y., Kamao M., Sugiura M., Nakagawa K. (2008) Conversion of phylloquinone (vitamin K1) into menaquinone-4 (vitamin K2) in mice: two possible routes for menaquinone-4 accumulation in cerebra of mice. J. Biol. Chem. 283, 11270–11279 [DOI] [PubMed] [Google Scholar]
- 10. Hirota Y., Tsugawa N., Nakagawa K., Suhara Y., Tanaka K., Uchino Y., Takeuchi A., Sawada N., Kamao M., Wada A., Okitsu T., Okano T. (2013) Menadione (vitamin K3) is a catabolic product of oral phylloquinone (vitamin K1) in the intestine and a circulating precursor of tissue menaquinone-4 (vitamin K2) in rats. J. Biol. Chem. 288, 33071–33080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Traber M. G. (2008) Vitamin E and K interactions: a 50-year-old problem. Nutr. Rev. 66, 624–629 [DOI] [PubMed] [Google Scholar]
- 12. Hanzawa F., Sakuma E., Nomura S., Uchida T., Oda H., Ikeda S. (2014) Excess α-tocopherol decreases extrahepatic phylloquinone in phylloquinone-fed rats but not menaquinone-4 in menaquinone-4-fed rats. Mol. Nutr. Food Res. 58, 1601–1609 [DOI] [PubMed] [Google Scholar]
- 13. Reboul E., Goncalves A., Comera C., Bott R., Nowicki M., Landrier J. F., Jourdheuil-Rahmani D., Dufour C., Collet X., Borel P. (2011) Vitamin D intestinal absorption is not a simple passive diffusion: evidences for involvement of cholesterol transporters. Mol. Nutr. Food Res. 55, 691–702 [DOI] [PubMed] [Google Scholar]
- 14. Staggers J. E., Hernell O., Stafford R. J., Carey M. C. (1990) Physical-chemical behavior of dietary and biliary lipids during intestinal digestion and absorption: 1. phase behavior and aggregation states of model lipid systems patterned after aqueous duodenal contents of healthy adult human beings. Biochemistry 29, 2028–2040 [DOI] [PubMed] [Google Scholar]
- 15. Reboul E., Abou L., Mikail C., Ghiringhelli O., André M., Portugal H., Jourdheuil-Rahmani D., Amiot M. J., Lairon D., Borel P. (2005) Lutein transport by Caco-2 TC-7 cells occurs partly by a facilitated process involving the scavenger receptor class B type I (SR-BI). Biochem. J. 387, 455–461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Borel P., Pasquier B., Armand M., Tyssandier V., Grolier P., Alexandre-Gouabau M. C., Andre M., Senft M., Peyrot J., Jaussan V., Lairon D., Azais-Braesco V. (2001) Processing of vitamin A and E in the human gastrointestinal tract. Am. J. Physiol. Gastrointest. Liver Physiol. 280, G95–G103 [DOI] [PubMed] [Google Scholar]
- 17. Salvini S., Charbonnier M., Defoort C., Alquier C., Lairon D. (2002) Functional characterization of three clones of the human intestinal Caco-2 cell line for dietary lipid processing. Br. J. Nutr. 87, 211–217 [DOI] [PubMed] [Google Scholar]
- 18. Chantret I., Rodolosse A., Barbat A., Dussaulx E., Brot-Laroche E., Zweibaum A., Rousset M. (1994) Differential expression of sucrase-isomaltase in clones isolated from early and late passages of the cell line Caco-2: evidence for glucose-dependent negative regulation. J. Cell Sci. 107, 213–225 [DOI] [PubMed] [Google Scholar]
- 19. Goncalves A., Gleize B., Roi S., Nowicki M., Dhaussy A., Huertas A., Amiot M. J., Reboul E. (2013) Fatty acids affect micellar properties and modulate vitamin D uptake and basolateral efflux in Caco-2 cells. J. Nutr. Biochem. 24, 1751–1757 [DOI] [PubMed] [Google Scholar]
- 20. Drover V. A., Ajmal M., Nassir F., Davidson N. O., Nauli A. M., Sahoo D., Tso P., Abumrad N. A. (2005) CD36 deficiency impairs intestinal lipid secretion and clearance of chylomicrons from the blood. J. Clin. Invest. 115, 1290–1297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Reboul E., Klein A., Bietrix F., Gleize B., Malezet-Desmoulins C., Schneider M., Margotat A., Lagrost L., Collet X., Borel P. (2006) Scavenger receptor class B type I (SR-BI) is involved in vitamin E transport across the enterocyte. J. Biol. Chem. 281, 4739–4745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Febbraio M., Abumrad N. A., Hajjar D. P., Sharma K., Cheng W., Pearce S. F., Silverstein R. L. (1999) A null mutation in murine CD36 reveals an important role in fatty acid and lipoprotein metabolism. J. Biol. Chem. 274, 19055–19062 [DOI] [PubMed] [Google Scholar]
- 23. Tran T. T., Poirier H., Clément L., Nassir F., Pelsers M. M., Petit V., Degrace P., Monnot M. C., Glatz J. F., Abumrad N. A., Besnard P., Niot I. (2011) Luminal lipid regulates CD36 levels and downstream signaling to stimulate chylomicron synthesis. J. Biol. Chem. 286, 25201–25210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bietrix F., Yan D., Nauze M., Rolland C., Bertrand-Michel J., Coméra C., Schaak S., Barbaras R., Groen A. K., Perret B., Tercé F., Collet X. (2006) Accelerated lipid absorption in mice overexpressing intestinal SR-BI. J. Biol. Chem. 281, 7214–7219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Reboul E., Soayfane Z., Goncalves A., Cantiello M., Bott R., Nauze M., Tercé F., Collet X., Coméra C. (2012) Respective contributions of intestinal Niemann-Pick C1-like 1 and scavenger receptor class B type I to cholesterol and tocopherol uptake: in vivo v. in vitro studies. Br. J. Nutr. 107, 1296–1304 [DOI] [PubMed] [Google Scholar]
- 26. Thijssen H. H., Vervoort L. M., Schurgers L. J., Shearer M. J. (2006) Menadione is a metabolite of oral vitamin K. Br. J. Nutr. 95, 260–266 [DOI] [PubMed] [Google Scholar]
- 27. Song Q., Wen A., Ding L., Dai L., Yang L., Qi X. (2008) HPLC-APCI-MS for the determination of vitamin K(1) in human plasma: method and clinical application. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 875, 541–545 [DOI] [PubMed] [Google Scholar]
- 28. Yu M., Romer K. A., Nieland T. J., Xu S., Saenz-Vash V., Penman M., Yesilaltay A., Carr S. A., Krieger M. (2011) Exoplasmic cysteine Cys384 of the HDL receptor SR-BI is critical for its sensitivity to a small-molecule inhibitor and normal lipid transport activity. Proc. Natl. Acad. Sci. U.S.A. 108, 12243–12248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Borel P., Lietz G., Goncalves A., Szabo de Edelenyi F., Lecompte S., Curtis P., Goumidi L., Caslake M. J., Miles E. A., Packard C., Calder P. C., Mathers J. C., Minihane A. M., Tourniaire F., Kesse-Guyot E., Galan P., Hercberg S., Breidenassel C., González Gross M., Moussa M., Meirhaeghe A., Reboul E. (2013) CD36 and SR-BI are involved in cellular uptake of provitamin A carotenoids by Caco-2 and HEK cells, and some of their genetic variants are associated with plasma concentrations of these micronutrients in humans. J. Nutr. 143, 448–456 [DOI] [PubMed] [Google Scholar]
- 30. Reboul E., Trompier D., Moussa M., Klein A., Landrier J. F., Chimini G., Borel P. (2009) ATP-binding cassette transporter A1 is significantly involved in the intestinal absorption of α- and γ-tocopherol but not in that of retinyl palmitate in mice. Am. J. Clin. Nutr. 89, 177–184 [DOI] [PubMed] [Google Scholar]
- 31. Tyssandier V., Reboul E., Dumas J. F., Bouteloup-Demange C., Armand M., Marcand J., Sallas M., Borel P. (2003) Processing of vegetable-borne carotenoids in the human stomach and duodenum. Am. J. Physiol. Gastrointest. Liver Physiol. 284, G913–G923 [DOI] [PubMed] [Google Scholar]
- 32. Bolton-Smith C., Price R. J., Fenton S. T., Harrington D. J., Shearer M. J. (2000) Compilation of a provisional UK database for the phylloquinone (vitamin K1) content of foods. Br. J. Nutr. 83, 389–399 [PubMed] [Google Scholar]
- 33. Kamao M., Suhara Y., Tsugawa N., Okano T. (2005) Determination of plasma vitamin K by high-performance liquid chromatography with fluorescence detection using vitamin K analogs as internal standards. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 816, 41–48 [DOI] [PubMed] [Google Scholar]
- 34. Kopec R. E., Schweiggert R. M., Riedl K. M., Carle R., Schwartz S. J. (2013) Comparison of high-performance liquid chromatography/tandem mass spectrometry and high-performance liquid chromatography/photo-diode array detection for the quantitation of carotenoids, retinyl esters, α-tocopherol and phylloquinone in chylomicron-rich fractions of human plasma. Rapid Commun. Mass Spectrom. 27, 1393–1402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Artursson P., Karlsson J., Ocklind G., Schipper N. (1995) Epithelia Cell Culture: A Practical Approach, pp. 111–133, IRL Press at Oxford University Press, Oxford [Google Scholar]
- 36. Hollander D. (1973) Vitamin K1 absorption by everted intestinal sacs of the rat. Am. J. Physiol. 225, 360–364 [DOI] [PubMed] [Google Scholar]
- 37. Goncalves A., Roi S., Nowicki M., Niot I., Reboul E. (2014) Cluster-determinant 36 impacts on vitamin E postprandial response. Mol. Nutr. Food Res. 10.1002/mnfr.201400339 [DOI] [PubMed] [Google Scholar]
- 38. Nieland T. J., Penman M., Dori L., Krieger M., Kirchhausen T. (2002) Discovery of chemical inhibitors of the selective transfer of lipids mediated by the HDL receptor SR-BI. Proc. Natl. Acad. Sci. U.S.A. 99, 15422–15427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Nieland T. J., Chroni A., Fitzgerald M. L., Maliga Z., Zannis V. I., Kirchhausen T., Krieger M. (2004) Cross-inhibition of SR-BI- and ABCA1-mediated cholesterol transport by the small molecules BLT-4 and glyburide. J. Lipid Res. 45, 1256–1265 [DOI] [PubMed] [Google Scholar]
- 40. Goudriaan J. R., den Boer M. A., Rensen P. C., Febbraio M., Kuipers F., Romijn J. A., Havekes L. M., Voshol P. J. (2005) CD36 deficiency in mice impairs lipoprotein lipase-mediated triglyceride clearance. J. Lipid Res. 46, 2175–2181 [DOI] [PubMed] [Google Scholar]