Abstract
Venous thromboembolism (VTE) is the leading cause of morbidity and mortality among hospitalized patients. We searched the PubMed database and reviewed the articles published until June 2011. Articles related to the D-dimer and VTE were considered to write this paper. Many factors play a key role in changing the sensitivity and specificity of D-dimer testing, including the extent of thrombosis and fibrinolytic activity, duration of symptoms, anticoagulant therapy, comorbidity due to surgical or medical illnesses, inflammatory diseases, cancer, elderly age, pregnancy and the postpartum period, and previous VTE. Many previous studies have shown that the D-dimer test is highly sensitive (>95%) in acute deep venous thrombosis or pulmonary embolism, usually with a cut-off value of 500 μg FEU/l, which reasonably rules out acute VTE, particularly in patients with low clinical probability (LCP) or intermediate clinical probability. Patients with high D-dimer levels upon presentation may prompt a more intense diagnostic approach, irrespective of pretest probability. Studies performed after a negative D-dimer for 3 months proved the high negative predictive value (NPV) of D-dimer testing together with LCP in patients with suspected VTE. Among oncology patients, D-dimer testing has the highest sensitivity and NPV in excluding VTE. The new cutoff values of D-dimer testing were analyzed in a recent prospective study of pregnant women; they are 286 ng DDU/ml, 457 ng DDU/ml, and 644 ng DDU/ml for the first, second, and third trimesters, respectively.
Keywords: Clinical probability rule, D-dimer, Venous thromboembolism
Introduction
D-Dimer is used as an initial screening test in the emergency department to diagnose patients who have signs, or symptoms suggestive of venous thromboembolism (VTE). D-dimer is detectable in patients with deep venous thrombosis (DVT), as it is a marker of endogenous fibrinolysis.[1] The purpose of this test, which has a high negative predictive value (NPV), is to provide a fast and cost-effective way to triage patients with thromboembolic phenomenon. Although the D-dimer has a high NPV, patients with positive D-dimer should undergo further imaging to determine whether or not they have VTE. We searched the PubMed database and reviewed the articles published until June 2011. Articles related to the d-dimer and VTE was taken into consideration to write this paper. This article discusses the epidemiology of VTE, clinical probability rules (CPRs), D-dimer levels and types of D-dimer assays, factors influencing D-dimer testing, the value of D-dimer testing in specific populations (including the elderly, pregnant women, and oncology patients), and lastly, the role of D-dimer testing in evaluating patients with recurrent VTE.
Clinical Probability Rules
Before ordering the D-dimer test, it is essential to assess the patient's clinical probability for VTE. For suspected DVT, the Wells score outlined in Table 1 has been commonly used. In patients with a low clinical probability (LCP), intermediate clinical probability (ICP), and high clinical probability (HCP), the prevalence of DVT is <5%, 15%, and 70%, respectively.[2] For suspected pulmonary embolism (PE), Wells and revised Geneva scores [Table 1] have gained acceptance; among them, the revised Geneva score is entirely based on clinical variables and is independent of physician judgment.[3,4] The prevalence of PE was 8%, 28%, and 74% in patients with LCP, ICP, and HCP, respectively.[4]
Table 1.
Clinical probability rules
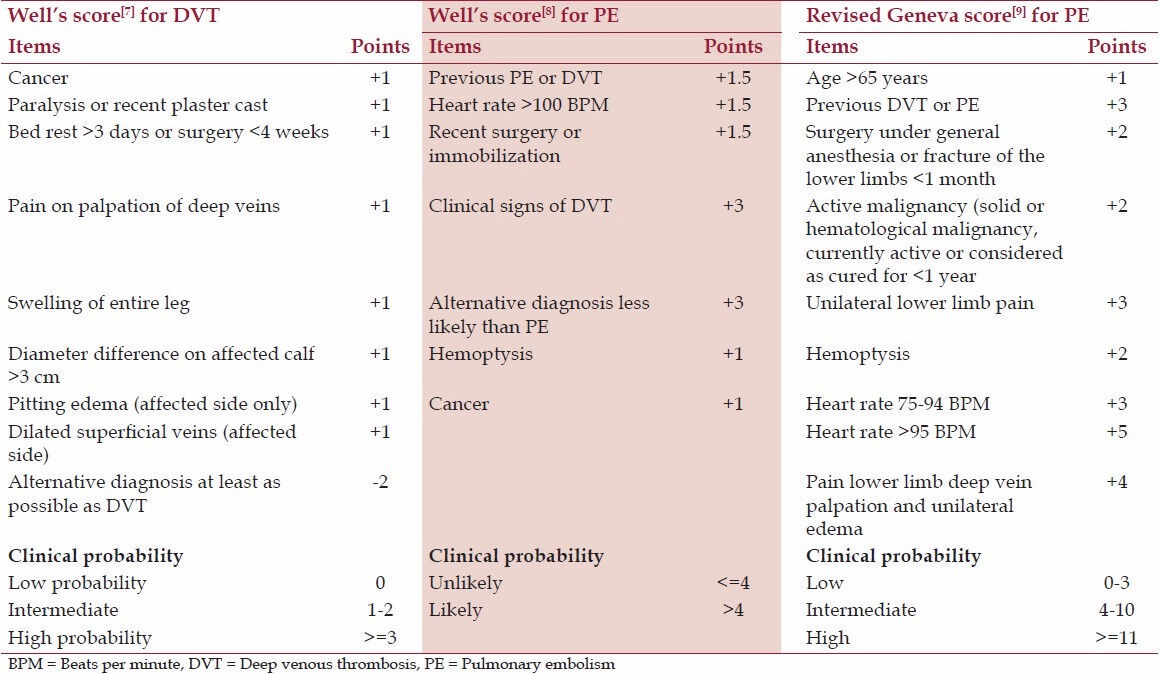
In the Wells' score, the presence of each clinical feature is given a positive score of +1. A score of –2 is given if an alternative diagnosis is highly likely, which mainly depends on individual physician judgment.[3] In a prospective cohort study of 807 patients, the authors concluded that four CPRs-Wells' rule, simplified Wells' rule, revised Geneva score, and simplified revised Geneva score-show similar performance with a normal D-dimer to exclude PE.[5] In a survey, 68% of respondents reported that they were familiar with at least 1 of 2 CPRs for PE.[6] In this study, physicians did not apply CPRs for suspected VTE due to medico-legal concerns, difficulty in memorizing and implementing the rules, the belief that clinical configuration is better, and the belief that none of the rules has been validated to their satisfaction.[6] Another study showed that 40% of inappropriate diagnostic strategies were attributable to the physician's failure to properly incorporate CPRs into their diagnostic decision.[7]
In their retrospective study of 1161 patients, Lee and Zierler[8] made a statement about the under usage of the diagnostic strategy with CPRs and D-dimer as initial screening followed for suspected VTE. Similarly, another retrospective study noted that there was no documentation of pretest probability (PTP) assessment for 62 of the 97 documented VTE suspected cases.[9] In this study, PTP assessment was not documented in the majority of emergency department cases of suspected VTE. Further, 25% of the documented decisions were in disagreement with established recommendations for a given test results, which were misinterpreted, applied incorrectly, or both.
D-Dimer
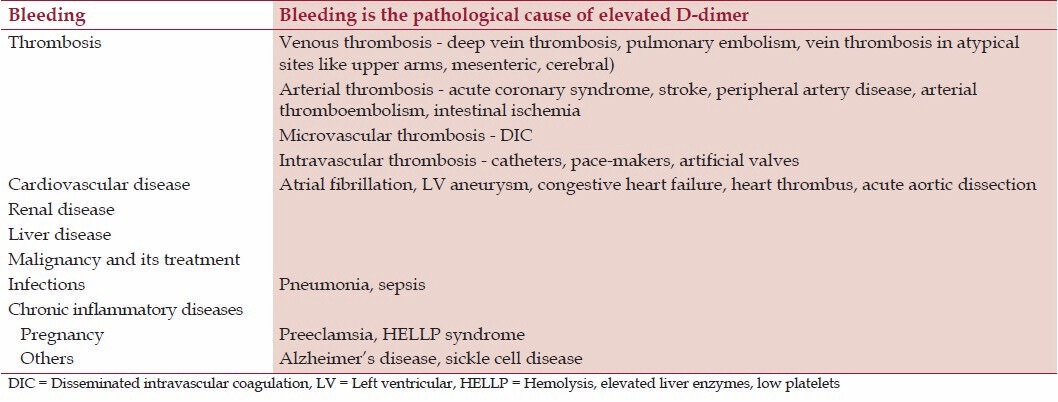
Clinicians must be aware that D-dimer is increased in many conditions. Physiologic causes of D-dimer elevation include pregnancy and puerperium, increasing age (>65 years), African American heritage, cigarette smoking, recent trauma, and the postoperative period.[10] Pathologic causes for D-dimer elevation are listed in Table 2.[10,11] Many strategies have been proposed for diagnosing VTE, including testing for D-dimer after a first negative imaging test to identify patients who require a new specific evaluation, initial D-dimer testing for the exclusion of VTE with further imaging tests only in patients with a positive test, and combined D-dimer testing with clinical probability and subsequent imaging tests.[10]
Table 2.
Pathological causes for elevated D-dimer levels
In the emergency department, apart from clinical assessment, testing for D-dimer levels is done in order to rule out a diagnosis of VTE in low-risk patients. In a meta-analysis performed by Stein et al.,[12] which included 31 studies to determine the accuracy of D-dimer testing in patients with suspected VTE, the prevalence of VTE ranged from 20% to 78% (average, 36%). In this study, patients with LCP or ICP had a probability for false-positive D-dimer levels ranging from 40% to 60%. A negative D-dimer test can effectively exclude VTE disease in a way comparable to a lung scan or duplex ultrasonography in LCP patients. In a meta-analysis by Brown et al.,[13] which assessed the use of D-dimer for excluding VTE, the prevalence was 17-58%. In the two aforementioned analyses, the sensitivity of D-dimer testing was 96% (95% confidence interval [CI], 0.90-1.00) and 94% (95% CI, 0.88-0.97), respectively.[12,13]
The D-dimer has been shown to be highly sensitive (>95%) in excluding acute VTE at the cutoff value of 500 μg FEU/l, at least in patients with LCP or ICP.[14] In a study by Taira et al.,[15] the authors concluded that LCP patients with D-dimer levels <500 ng DDU/ml may not require additional and costly imaging studies. In the prospective study of 270 patients with suspected VTE, the HCP, ICP, and LCP in patients with suspected PE was 25%, 64%, and 11%, respectively. The HCP, ICP, and LCP in patients with suspected DVT was 59%, 32%, and 9%, respectively.[16] In this study, the sensitivity of the D-dimer assay for ruling out VTE was 92% at a cut-off of <500 μg FEU/l, which did not reach the sensitivities observed in the other studies (>95%).
Vanfleteren and Wesseling[17] noted that, in the primary care setting, D-dimer is a useful test in suspected VTE patients. At their hospital in 2007 and 2008, the diagnostic yield of VTE in patients with positive D-dimer test results was 24% and 21%, respectively. The imaging tests performed was computed tomography (CT) pulmonary angiography or ventilation-perfusion scintigraphy and venous ultrasound. Another study evaluated D-dimer levels after 3-7 days among patients in the emergency department (n = 101) with LCP (<1.5) and negative D-dimer (<0.5 mg FEU/dl). Elevated D-dimer levels occurred in 13 out of 101 patients. Interestingly, none of the 13 patients was diagnosed with VTE, and all patients were observed for 3 months. The authors concluded that the normal D-dimer and LCP safely excluded VTE in emergency department patients, and follow-up D-dimer testing added no further information.[18] In a study of 197 out-patients and in-patients, many patients were not included in the HCP category as the Wells chart for PE has a high verge for allocating patients into this category.[19] D-dimer testing showed 100% sensitivity and 100% NPV, and a negative D-dimer together with a negative LCP or ICP score safely excluded VTE. However, the test lacked specificity and positive predictive value.[19] In another multicenter study of 747 patients with suspected VTE, the D-dimer assay proved to have 100% sensitivity and 100% NPV, and could be used to exclude VTE in patients with LCP.[20] In a prospective cohort study of 2206 patients with suspected PE who received follow-up for 3 months, the combination of negative D-dimer and PE was observed in 1057 patients (32.0%), of whom 1028 were not treated with anticoagulants; subsequent nonfatal VTE occurred in 5 patients (0.5%).[21]
D-Dimer in Patients with High Clinical Probability for Venous Thromboembolism
Patients with HCP should not be tested for D-dimer because a concentration below the diagnostic cutoff is rare in this population and the posttest probability for a D-dimer >500 μg FEU/l has a poor positive predictive value for VTE. The low specificity of the test prevents it from ruling in the disease.[22] Nevertheless, Bosson et al.[23] suggested in a retrospective study that a D-dimer level above 2000 μg FEU/l was predictive of the presence of PE, with an odds ratio of 6.9, irrespective of clinical probability. The main drawback of this study was the high prevalence of PE, which was 27%, 58%, and 85% in the LCP, ICP, and HCP categories, respectively. The authors noted that these results require clinical validation in a prospective study.
The significance of D-dimer in patients with HCP of PE was reported in a prospective study by Söderberg et al.[24] D-dimer had a higher NPV than the Wells score, and the combination of both further improved the diagnostic algorithm. In the Christopher study, the false-negative rate of PE diagnosis by chest CT in patients with HCP was 5.3%.[25] Similarly, in the PIOPED II (Prospective Investigation of Pulmonary Embolism Diagnosis II) trial of 7284 patients, 6 of 15 patients with HCP for PE and a negative CT had PE.[26] In another retrospective study, there was a positive correlation between the prevalence of PE and the D-dimer level (7% at D-dimer levels of 0.5-1 μg FEU/ml and 90% at 9 μg FEU/ml).[27] In a separate study of 44 patients, similar results were obtained for distal versus proximal DVT, detected by ultrasonography of the lower limb.[27] In a study comparing the quantitative D-dimer levels to the presence of PE in symptomatic patients, PE prevalence was strongly related to the D-dimer level and increased 4 times with D-dimer levels >4000 ng FEU/ml compared with levels between 500 and 1000 ng FEU/ml.[28] In a study performed in an out-patient setting in 671 patients with clinically suspected PE, the specificity of a D-dimer test was 93% when D-dimer levels exceeded 4000 μg FEU/l. However, in the presence of ICP and HCP, this resulted in a limited positive predictive value because of the relatively low PE incidence (20%).[29] Thus, high D-dimer levels upon presentation may potentially prompt a more intense diagnostic approach, irrespective of PTP.
Types of D-Dimer Assays
D-dimers are detected by immunoassays using monoclonal antibodies specific for the cross-linked D-dimer domain in fibrinogen. Commercially available assays include latex agglutination, immunoturbidimetry, and enzyme-linked immunosorbent assay (ELISA).[10] Efforts made to standardize D-dimer results have not been successful thus far, because the D-dimer analyte is not uniform across the different assays. The NPV and sensitivity of established central laboratory ELISA D-dimer and rapid whole-blood quantitative D-dimer tests were 100%, but the rapid whole-blood test had greater specificity for VTE disease (73.3% vs. 67.9%), and the positive predictive value was poor for both tests.[30] The immunoturbidimetric monoclonal antibody method (Innovance D-dimer assay, Siemens Healthcare Diagnostics) has high enough sensitivity and NPV to be used as a standalone test in patients with a nonhigh PTP score, and the test provides quantitative and operator-independent results in individual samples in a very short time of 7-11 min, which is particularly useful in emergency situations.[31] The Innovance D-dimer assay is an extremely sensitive test, and nearly all patients with confirmed DVT and PE have positive results.[19] The sensitivity and NPV of the rapid ELISA D-dimer test are 100%. It can be used to rule out PE irrespective of clinical assessment, and it has been reviewed extensively in several prospective studies.[32,33] In the Christopher study, the Vitek Immuno-Diagnostic Assay System (VIDAS, bioMerieux) ELISA test had a sensitivity of 100% (500 μg/l) for ruling out the presence of PE. The 5 false-negative D-dimer test results (0.8%) occurred in the group tested with Tinaquant.[21] In a meta-analysis, Di Nisio et al.[34] analyzed the accuracy of different D-dimer assays from 113 individual studies and confirmed that the ELISA, the microplate ELISA, and the automated quantitative latex assays have a higher sensitivity but a lower specificity, resulting in a more confident exclusion of the disease at the cost of a potentially increased need for additional imaging. Studies performed after a negative D-dimer test for an interval of 3 months proved the high NPV of D-dimer testing together with LCP in patients with suspected VTE. In a study by Gibson et al.[35] involving all patients with a normal D-dimer (563), the VTE rate at a follow-up of 3 months was 2.3%. The VTE rate was 1.1% in patients with an unlikely probability of PE (477), and 9.3% among patients with LCP (86). Patients with negative D-dimer results and LCP for PE had an incidence of 0.7% (7/1028) at a follow-up of 3 months.[21] In a study of 1096 patients with suspected DVT, who had LCP and negative D-dimer, the incidence of VTE in the next 3 months was 0.4%.[1] In a multicenter study, the D-dimer test excluded PE in 561 patients (n = 1819) with LCP or ICP, and none of these patients had VTE in the 3-month follow-up, with a D-dimer below 500 μg FEU/l.[36]
Factors Influencing D-Dimer Levels
The diagnostic yield of D-dimer is affected not only by the choice of assay, but also by patient characteristics. Certain factors influence the sensitivity and specificity in D-dimer testing, such as the extent of thrombosis and fibrinolytic activity, duration of symptoms, age, surgical procedures, anticoagulants, and comorbid conditions such as inflammatory states, cancer, pregnancy and the postpartum period, and previous VTE.[37] D-dimer levels were positively correlated with thrombus extension, with high levels in the presence of larger thrombi. D-dimer levels had an inverse relation with duration between the onset of symptoms and testing, typically reaching 25% of the initial value after 1-2 weeks.[38] In a study of 197 patients with positive D-dimer, the authors concluded that the presence of acute VTE could not be excluded if the D-dimer test were done after 1 week following the clinical presentation.[39] Similar findings were noted by Speiser et al.[40] (n = 39) and Heit et al.[41] (n = 33) during their analyses. They concluded that the sensitivity of D-dimer was inversely correlated to the duration of symptoms.
In a study by Wada et al.,[42] 87 out of 754 patients had DVT, and the highest levels of D-dimer were seen on the 2nd day of clinical presentation. D-dimer concentration was also affected by anticoagulation therapy and decreased approximately 25% by 24 h, with a consequent decrease in sensitivity from 95.5% to 89.4%.[43] Individual factors, including patient age, renal function, and radiological chest abnormalities, were associated with false-positive D-dimer levels in 57%, 44%, and 70% of VTE-negative patients.[44] Interestingly, D-dimer testing was falsely positive in 94% of VTE-negative patients with advanced age (60 years or older), renal failure, and abnormal chest radiology. A careful clinical assessment may be a more useful option for deciding further appropriate investigations in these specific patients, in order to reduce unnecessary exposure to radiation, intravenous contrast, and economic burden.[44] D-dimer in renal failure reflects increased fibrin turnover apart from decreased elimination.[45,46] This group of patients has a relative risk of VTE of 2.1, which increases when the glomerular filtration rate reaches 75 ml/min/1.73 m2. D-dimer testing is of limited value in this group.
Elderly Patients
An analysis reported no clear advantage of measuring D-dimer after the age of 80, except when the risk of performing CT was too high due to impaired renal function.[47] In a study by Legnani et al., the authors highlighted the different age-specific, quantitative D-dimer cutoff values in patients aged 70 years or less and older than 70 years, respectively: VIDAS ELISA = 600 ng FEU/ml and 1200 ng FEU/ml, Innovance = 500 ng/ml and 900 ng/ml NP, Hemosil HS D-dimer (Instrumentation Laboratories) = 250 ng DDU/ml and 450 ng DDU/ml, and STA Liatest (Stago) = 700 ng FEU/ml and 1000 ng FEU/ml.[48] In a pooled analysis involving three prospective studies, normal D-dimer levels along with LCP effectively excluded DVT in elderly patients.[49]
Cancer
The validity of D-dimer in oncology patients is compromised as its levels may be elevated even in the absence of thrombosis. The risk factors for VTE in oncology patients include location of primary tumor, stage and initial period after diagnosis of tumor, and associated comorbidities.[45] Treatment modalities, including chemotherapy, antiangiogenic therapy, surgery, central venous catheters, and hospitalization, were other predisposing factors for thrombosis in these patients.[45] Laboratory biomarkers that predict VTE are thrombocytosis or leukocytosis, tissue factor, soluble P-selectin, and D-dimer.[50] In the prospective study involving 2263 consecutive patients with suspected DVT, independent poor prognostic factors were found for overall survival, including D-dimer levels >8000 ng FEU/ml and age >60 years. There were 247 patients (10.9%) with a known malignancy or who were diagnosed with malignancy during a follow-up period of 22 months.[51] The elevated D-dimer levels in these patients were not due to the presence of thrombus and may reflect the biology of the underlying tumor.
D-dimer levels >8000 ng FEU/ml were associated with an increased incidence of malignancy.[51] A retrospective study by Lee et al.[52] assessed D-dimer levels in 1068 patients with suspected DVT. The sensitivity of D-dimer was 86% and 83% in patients with and without cancer, respectively. However, the NPV was lower in oncology patients (79% vs. 96%). In contrast, in a study by ten Wolde et al.,[53] which evaluated 1739 patients with suspected DVT, the NPV for D-dimer testing was 97% in patients with and without cancer.
Similarly, the NPV and sensitivity of D-dimer testing was high for diagnosing PE among oncology patients.[54] Di Nisio et al.[55] analyzed 2066 patients and found that the NPV for the test was 100% and 97% among cancer patients with LCP and ICP, respectively. Another study reported a highest sensitivity (100%; 95% CI, 82-100%) and NPV (100%; 95% CI, 72-100%) in a sample of 72 cancer patients.[56] These data were confirmed in a second larger study, which involved a large cohort of 1721 outpatients. PE was ruled out by a negative D-dimer test in 494 out of 1554 (32%) patients without cancer, and in 18 out of 164 (11%) patients with a malignancy.
The sensitivity and NPV were 100% in both cancer and noncancer patients.[57] Regarding VTE recurrence in oncology patients, D-dimer and residual venous obstruction (RVO) are considered independent risk factors, and may help tailor anticoagulation treatment duration. Abnormal D-dimer levels observed during and after anticoagulation treatment may reflect the state of hypercoagulability not suppressed by anticoagulation treatment, while RVO may also be a marker of a prothrombotic condition. A practical approach might be to withdraw anticoagulation treatment in cases of normal D-dimer and absent RVO, measure D-dimer after 1 month, and resume anticoagulation treatment in cases of abnormal D-dimer.[58]
Pregnancy
The risk of VTE increases throughout pregnancy and is particularly high in the postpartum period, with an incidence of 1 per 1000 pregnancies.[59] The utility of a whole-blood agglutination D-dimer test to exclude DVT in pregnancy has been evaluated in a prospective study of 149 pregnant women. It showed 100% sensitivity, 100% NPV, and a specificity of 60%, and highlighted that D-dimer measurements were helpful in excluding VTE in the first and second trimester of pregnancy (although its value in the third trimester was limited).[60] In another study of 50 pregnant women, 50%, 22%, and 0% were in the reference range (0.5 mg FEU/l) during the first, second, and third trimesters, respectively.[61] In another prospective study of 89 pregnant women, D-dimer testing had 100% sensitivity at the new cutoff values for the first, second, and third trimesters (286 ng DDU/ml, 457 ng DDU/ml, and 644 ng DDU/ml, respectively).[62] In his study on 48 pregnant women, Morse[63] tried to establish a new reference range for D-dimer levels during pregnancy. The reference ranges were <465 ng DDU/ml and <640 ng DDU/ml for the second and third trimesters, respectively.
Recurrent Venous Thromboembolism
Recurrence of unprovoked DVT occurs frequently after the discontinuation of anticoagulation in approximately half of patients within 10 years of an initial event, and is highest (10-15%) over the first 6-12 months.[64] Rathbun et al.[65] reported the results of a D-dimer test to exclude recurrent DVT in 300 patients with suspected DVT, who had a previous episode of DVT. The D-dimer test was normal in 45% of patients (n = 134), and 18% of patients (n = 54) had DVT. Recurrent VTE was diagnosed in only 1 patient (0.8%; 95% CI, 0.0-4%) during a 3-month follow-up. In another study, PE was ruled out by a negative D-dimer test in patients with previous VTE in 15.9% (49 out of 308) versus 32.7% (462 out of 1411) of patients without previous VTE. The recurrence risk was 0% during the next 3 months in patients with previous VTE and a negative D-dimer test who did not receive anticoagulation.[66] Surprisingly, the 2-fold lower chance of a negative D-dimer test result in patients with previous VTE was not influenced by older age, cancer, recent surgery, or acute inflammation or infection. Patients with normal D-dimer 1 month after stopping anticoagulation who did not resume anticoagulation had an annual recurrence rate of 4.4% in 1 study.[67] Patients with abnormal D-dimer were randomized to resume or not resume anticoagulation, with 2% and 10.2% annual recurrence rates, respectively.[67] In a study of 1818 patients, the risk of recurrent VTE was higher among patients with positive D-dimer levels than those with negative results during a follow-up period of 26.9 months after an unprovoked VTE. This was independent of patient age or timing of the postanticoagulation D-dimer testing.[68] In another prospective cohort study, 79 (13%) of 610 patients had recurrent VTE with a mean follow-up of 38 months, and they had significantly higher D-dimer levels. Patients with D-dimer levels <250 ng/ml had a recurrence rate of 3.7% at 2 years compared with 11.5% in patients with D-dimer levels >250 ng FEU/ml (P = 0.001). The relative risk of recurrence was 60% lower in patients with D-dimer levels <250 ng FEU/ml compared with patients with higher D-dimer levels.[60] In a prospective cohort study, 929 patients after first unprovoked VTE were followed for 43.3 months after discontinuation of anticoagulation, and a total of 176 patients (18.9%) had recurrent VTE. Gender, proximal versus distal DVT, PE versus distal thrombosis, and elevated levels of D-dimer per doubling were related to a higher recurrence risk.[70]
Discussion
Venous thromboembolism is a common condition that cannot be diagnosed solely on the basis of clinical presentation due to the lack of sensitivity and specificity of signs and symptoms. PE is a common yet potentially fatal disease, which results in >250,000 hospitalizations in the United States each year.[71] The prevalence of DVT and PE is 20% or less among clinically suspected individuals.[22] A missed diagnosis of VTE can lead to sudden death, chronic cardiopulmonary dysfunction, and impaired quality-of-life.[72] Among patients with suspected VTE, it is important to identify those who do not have the disease, in order to obviate the need for anticoagulation therapy and associated bleeding risk.[73] Simultaneously, over-testing patients for PE can be costly and expose them to harm from radiation, intravenous contrast, a false-positive diagnosis, and anticoagulation treatment. The risk factors for VTE are increasing age, cancer and its treatment, paralysis, prolonged immobility, long air travel, congestive heart failure, acute infection, pregnancy or puerperium, hormonal treatment, varicose veins, dehydration, previous VTE, inflammatory bowel disease, rheumatologic disease, nephrotic syndrome, persistent elevation of D-dimer, and atherosclerotic disease.[74]
Conclusion
Every effort should be made to implement the diagnostic strategies for VTE. The major limitation of D-dimer testing is its use in special clinical settings that result in low specificities, such as in oncology patients, elderly patients, and pregnant women. However, the test retains its high sensitivity and NPV in those situations.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Wells PS, Anderson DR, Rodger M, Forgie M, Kearon C, Dreyer J, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med. 2003;349:1227–35. doi: 10.1056/NEJMoa023153. [DOI] [PubMed] [Google Scholar]
- 2.Wells PS, Anderson DR, Bormanis J, Guy F, Mitchell M, Gray L, et al. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. Lancet. 1997;350:1795–8. doi: 10.1016/S0140-6736(97)08140-3. [DOI] [PubMed] [Google Scholar]
- 3.Wells PS, Anderson DR, Rodger M, Ginsberg JS, Kearon C, Gent M, et al. Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: Increasing the models utility with the SimpliRED D-dimer. Thromb Haemost. 2000;83:416–20. [PubMed] [Google Scholar]
- 4.Le Gal G, Righini M, Roy PM, Sanchez O, Aujesky D, Bounameaux H, et al. Prediction of pulmonary embolism in the emergency department: The revised Geneva score. Ann Intern Med. 2006;144:165–71. doi: 10.7326/0003-4819-144-3-200602070-00004. [DOI] [PubMed] [Google Scholar]
- 5.Douma RA, Mos IC, Erkens PM, Nizet TA, Durian MF, Hovens MM, et al. Performance of 4 clinical decision rules in the diagnostic management of acute pulmonary embolism: A prospective cohort study. Ann Intern Med. 2011;154:709–18. doi: 10.7326/0003-4819-154-11-201106070-00002. [DOI] [PubMed] [Google Scholar]
- 6.Runyon MS, Richman PB, Kline JA. Pulmonary Embolism Research Consortium Study Group. Emergency medicine practitioner knowledge and use of decision rules for the evaluation of patients with suspected pulmonary embolism: Variations by practice setting and training level. Acad Emerg Med. 2007;14:53–7. doi: 10.1197/j.aem.2006.07.032. [DOI] [PubMed] [Google Scholar]
- 7.Roy PM, Meyer G, Vielle B, Le Gall C, Verschuren F, Carpentier F, et al. Appropriateness of diagnostic management and outcomes of suspected pulmonary embolism. Ann Intern Med. 2006;144:157–64. doi: 10.7326/0003-4819-144-3-200602070-00003. [DOI] [PubMed] [Google Scholar]
- 8.Lee JA, Zierler BK. The current state of practice in the diagnosis of venous thromboembolism at an academic medical center. Vasc Endovascular Surg. 2011;45:22–7. doi: 10.1177/1538574410385873. [DOI] [PubMed] [Google Scholar]
- 9.Smith C, Mensah A, Mal S, Worster A. Is pretest probability assessment on emergency department patients with suspected venous thromboembolism documented before SimpliRED D-dimer testing? CJEM. 2008;10:519–23. [PubMed] [Google Scholar]
- 10.Prisco D, Grifoni E. The role of D-dimer testing in patients with suspected venous thromboembolism. Semin Thromb Hemost. 2009;35:50–9. doi: 10.1055/s-0029-1214148. [DOI] [PubMed] [Google Scholar]
- 11.Lippi G, Franchini M, Targher G, Favaloro EJ. Help me, Doctor! My D-dimer is raised. Ann Med. 2008;40:594–605. doi: 10.1080/07853890802161015. [DOI] [PubMed] [Google Scholar]
- 12.Stein PD, Hull RD, Patel KC, Olson RE, Ghali WA, Brant R, et al. D-dimer for the exclusion of acute venous thrombosis and pulmonary embolism: A systematic review. Ann Intern Med. 2004;140:589–602. doi: 10.7326/0003-4819-140-8-200404200-00005. [DOI] [PubMed] [Google Scholar]
- 13.Brown MD, Rowe BH, Reeves MJ, Bermingham JM, Goldhaber SZ. The accuracy of the enzyme-linked immunosorbent assay D-dimer test in the diagnosis of pulmonary embolism: A meta-analysis. Ann Emerg Med. 2002;40:133–44. doi: 10.1067/mem.2002.124755. [DOI] [PubMed] [Google Scholar]
- 14.Righini M, Perrier A, De Moerloose P, Bounameaux H. D-dimer for venous thromboembolism diagnosis: 20 years later. J Thromb Haemost. 2008;6:1059–71. doi: 10.1111/j.1538-7836.2008.02981.x. [DOI] [PubMed] [Google Scholar]
- 15.Taira T, Taira BR, Carmen M, Chohan J, Singer AJ. Risk of venous thromboembolism in patients with borderline quantitative D-dimer levels. Am J Emerg Med. 2010;28:450–3. doi: 10.1016/j.ajem.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 16.Lukaschek J, Schmid HR, Vorburger C, Beer JH. Critical appraisal of the diagnostics of 270 consecutive cases of suspected venous thromboembolism and established consequences at a non-university center. Swiss Med Wkly. 2001;131:653–8. doi: 10.4414/smw.2001.09803. [DOI] [PubMed] [Google Scholar]
- 17.Vanfleteren L, Wesseling G. Evaluation of the diagnostic yield of D-dimer testing in suspected venous thromboembolism in primary care: A 2-year retrospective analysis. Prim Care Respir J. 2011;20:102–3. doi: 10.4104/pcrj.2010.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ljungqvist M, Söderberg M, Moritz P, Ahlgren A, Lärfars G. Evaluation of Wells score and repeated D-dimer in diagnosing venous thromboembolism. Eur J Intern Med. 2008;19:285–8. doi: 10.1016/j.ejim.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 19.Anoop P, Chappell P, Kulkarni S, Shirley JA. Evaluation of an immunoturbidimetric D-dimer assay and pretest probability score for suspected venous thromboembolism in a district hospital setting. Hematology. 2009;14:305–10. doi: 10.1179/102453309X446162. [DOI] [PubMed] [Google Scholar]
- 20.Legnani C, Cini M, Scarvelis D, Toulon P, Wu JR, Palareti G. Multicenter evaluation of a new quantitative highly sensitive D-dimer assay, the Hemosil D-dimer HS 500, in patients with clinically suspected venous thromboembolism. Thromb Res. 2010;125:398–401. doi: 10.1016/j.thromres.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 21.van Belle A, Büller HR, Huisman MV, Huisman PM, Kaasjager K, Kamphuisen PW, et al. Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, D-dimer testing, and computed tomography. JAMA. 2006;295:172–9. doi: 10.1001/jama.295.2.172. [DOI] [PubMed] [Google Scholar]
- 22.Bounameaux H, Perrier A, Righini M. Diagnosis of venous thromboembolism: An update. Vasc Med. 2010;15:399–406. doi: 10.1177/1358863X10378788. [DOI] [PubMed] [Google Scholar]
- 23.Bosson JL, Barro C, Satger B, Carpentier PH, Polack B, Pernod G. Quantitative high D-dimer value is predictive of pulmonary embolism occurrence independently of clinical score in a well-defined low risk factor population. J Thromb Haemost. 2005;3:93–9. doi: 10.1111/j.1538-7836.2004.01045.x. [DOI] [PubMed] [Google Scholar]
- 24.Söderberg M, Brohult J, Jorfeldt L, Lärfars G. The use of D-dimer testing and Wells score in patients with high probability for acute pulmonary embolism. J Eval Clin Pract. 2009;15:129–33. doi: 10.1111/j.1365-2753.2008.00967.x. [DOI] [PubMed] [Google Scholar]
- 25.Douma RA, Kamphuisen PW, Huisman MV, Büller HR. Christopher Study Investigators. False normal results on multidetector-row spiral computed tomography in patients with high clinical probability of pulmonary embolism. J Thromb Haemost. 2008;6:1978–9. doi: 10.1111/j.1538-7836.2008.03154.x. [DOI] [PubMed] [Google Scholar]
- 26.Stein PD, Fowler SE, Goodman LR, Gottschalk A, Hales CA, Hull RD, et al. Multidetector computed tomography for acute pulmonary embolism. N Engl J Med. 2006;354:2317–27. doi: 10.1056/NEJMoa052367. [DOI] [PubMed] [Google Scholar]
- 27.Hochuli M, Duewell S, Frauchiger B. Quantitative d-dimer levels and the extent of venous thromboembolism in CT angiography and lower limb ultrasonography. Vasa. 2007;36:267–74. doi: 10.1024/0301-1526.36.4.267. [DOI] [PubMed] [Google Scholar]
- 28.Tick LW, Nijkeuter M, Kramer MH, Hovens MM, Büller HR, Leebeek FW, et al. High D-dimer levels increase the likelihood of pulmonary embolism. J Intern Med. 2008;264:195–200. doi: 10.1111/j.1365-2796.2008.01972.x. [DOI] [PubMed] [Google Scholar]
- 29.Perrier A, Desmarais S, Goehring C, de Moerloose P, Morabia A, Unger PF, et al. D-dimer testing for suspected pulmonary embolism in outpatients. Am J Respir Crit Care Med. 1997;156:492–6. doi: 10.1164/ajrccm.156.2.9702032. [DOI] [PubMed] [Google Scholar]
- 30.Lee-Lewandrowski E, Nichols J, Van Cott E, Grisson R, Louissaint A, Benzer T, et al. Implementation of a rapid whole blood D-dimer test in the emergency department of an urban academic medical center: Impact on ED length of stay and ancillary test utilization. Am J Clin Pathol. 2009;132:326–31. doi: 10.1309/AJCP6US3ILGEAREE. [DOI] [PubMed] [Google Scholar]
- 31.de Moerloose P, Palareti G, Aguilar C, Legnani C, Reber G, Peetz D. A multicenter evaluation of a new quantitative highly sensitive D-dimer assay for exclusion of venous thromboembolism. Thromb Haemost. 2008;100:505–12. doi: 10.1160/th08-04-0202. [DOI] [PubMed] [Google Scholar]
- 32.Kucher N, Kohler HP, Dornhöfer T, Wallmann D, Lämmle B. Accuracy of D-dimer/fibrinogen ratio to predict pulmonary embolism: A prospective diagnostic study. J Thromb Haemost. 2003;1:708–13. doi: 10.1046/j.1538-7836.2003.00145.x. [DOI] [PubMed] [Google Scholar]
- 33.Perrier A, Roy PM, Sanchez O, Le Gal G, Meyer G, Gourdier AL, et al. Multidetector-row computed tomography in suspected pulmonary embolism. N Engl J Med. 2005;352:1760–8. doi: 10.1056/NEJMoa042905. [DOI] [PubMed] [Google Scholar]
- 34.Di Nisio M, Squizzato A, Rutjes AW, Büller HR, Zwinderman AH, Bossuyt PM. Diagnostic accuracy of D-dimer test for exclusion of venous thromboembolism: A systematic review. J Thromb Haemost. 2007;5:296–304. doi: 10.1111/j.1538-7836.2007.02328.x. [DOI] [PubMed] [Google Scholar]
- 35.Gibson NS, Sohne M, Gerdes VE, Nijkeuter M, Buller HR. The importance of clinical probability assessment in interpreting a normal d-dimer in patients with suspected pulmonary embolism. Chest. 2008;134:789–93. doi: 10.1378/chest.08-0344. [DOI] [PubMed] [Google Scholar]
- 36.Righini M, Le Gal G, Aujesky D, Roy PM, Sanchez O, Verschuren F, et al. Diagnosis of pulmonary embolism by multidetector CT alone or combined with venous ultrasonography of the leg: A randomised non-inferiority trial. Lancet. 2008;371:1343–52. doi: 10.1016/S0140-6736(08)60594-2. [DOI] [PubMed] [Google Scholar]
- 37.Siragusa S, Terulla V, Pirrelli S, Porta C, Falaschi F, Anastasio R, et al. A rapid D-dimer assay in patients presenting at the emergency room with suspected acute venous thrombosis: Accuracy and relation to clinical variables. Haematologica. 2001;86:856–61. [PubMed] [Google Scholar]
- 38.D'Angelo A, D'Alessandro G, Tomassini L, Pittet JL, Dupuy G, Crippa L. Evaluation of a new rapid quantitative D-dimer assay in patients with clinically suspected deep vein thrombosis. Thromb Haemost. 1996;75:412–6. [PubMed] [Google Scholar]
- 39.Goldin Y, Pasvolsky O, Rogowski O, Shapira I, Steinvil A, Halpern P, et al. The diagnostic yield of D-Dimer in relation to time from symptom onset in patients evaluated for venous thromboembolism in the emergency medicine department. J Thromb Thrombolysis. 2011;31:1–5. doi: 10.1007/s11239-010-0480-6. [DOI] [PubMed] [Google Scholar]
- 40.Speiser W, Mallek R, Koppensteiner R, Stümpflen A, Kapiotis S, Minar E, et al. D-dimer and TAT measurement in patients with deep venous thrombosis: Utility in diagnosis and judgement of anticoagulant treatment effectiveness. Thromb Haemost. 1990;64:196–201. [PubMed] [Google Scholar]
- 41.Heit JA, Minor TA, Andrews JC, Larson DR, Li H, Nichols WL. Determinants of plasma fibrin D-dimer sensitivity for acute pulmonary embolism as defined by pulmonary angiography. Arch Pathol Lab Med. 1999;123:235–40. doi: 10.5858/1999-123-0235-DOPFDD. [DOI] [PubMed] [Google Scholar]
- 42.Wada H, Kobayashi T, Abe Y, Hatada T, Yamada N, Sudo A, et al. Elevated levels of soluble fibrin or D-dimer indicate high risk of thrombosis. J Thromb Haemost. 2006;4:1253–8. doi: 10.1111/j.1538-7836.2006.01942.x. [DOI] [PubMed] [Google Scholar]
- 43.Couturaud F, Kearon C, Bates SM, Ginsberg JS. Decrease in sensitivity of D-dimer for acute venous thromboembolism after starting anticoagulant therapy. Blood Coagul Fibrinolysis. 2002;13:241–6. doi: 10.1097/00001721-200204000-00010. [DOI] [PubMed] [Google Scholar]
- 44.Qasim A, Duggan M, O'Connell N, O'Driscoll A. Clinical conditions and patient factors significantly influence diagnostic utility of D-dimer in venous thromboembolism. Blood Coagul Fibrinolysis. 2009;20:244–7. doi: 10.1097/MBC.0b013e328325600f. [DOI] [PubMed] [Google Scholar]
- 45.Gordge MP, Faint RW, Rylance PB, Ireland H, Lane DA, Neild GH. Plasma D dimer: A useful marker of fibrin breakdown in renal failure. Thromb Haemost. 1989;61:522–5. [PubMed] [Google Scholar]
- 46.Wattanakit K, Cushman M, Stehman-Breen C, Heckbert SR, Folsom AR. Chronic kidney disease increases risk for venous thromboembolism. J Am Soc Nephrol. 2008;19:135–40. doi: 10.1681/ASN.2007030308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Righini M, Nendaz M, Le Gal G, Bounameaux H, Perrier A. Influence of age on the cost-effectiveness of diagnostic strategies for suspected pulmonary embolism. J Thromb Haemost. 2007;5:1869–77. doi: 10.1111/j.1538-7836.2007.02667.x. [DOI] [PubMed] [Google Scholar]
- 48.Legnani C, Palareti G, Cosmi B, Cini M, Tosetto A, Tripodi A, et al. Different cut-off values of quantitative D-dimer methods to predict the risk of venous thromboembolism recurrence: A post-hoc analysis of the PROLONG study. Haematologica. 2008;93:900–7. doi: 10.3324/haematol.12320. [DOI] [PubMed] [Google Scholar]
- 49.Carrier M, Le Gal G, Bates SM, Anderson DR, Wells PS. D-dimer testing is useful to exclude deep vein thrombosis in elderly outpatients. J Thromb Haemost. 2008;6:1072–6. doi: 10.1111/j.1538-7836.2008.03007.x. [DOI] [PubMed] [Google Scholar]
- 50.Khorana AA, Connolly GC. Assessing risk of venous thromboembolism in the patient with cancer. J Clin Oncol. 2009;27:4839–47. doi: 10.1200/JCO.2009.22.3271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Knowlson L, Bacchu S, Paneesha S, McManus A, Randall K, Rose P. Elevated D-dimers are also a marker of underlying malignancy and increased mortality in the absence of venous thromboembolism. J Clin Pathol. 2010;63:818–22. doi: 10.1136/jcp.2010.076349. [DOI] [PubMed] [Google Scholar]
- 52.Lee AY, Julian JA, Levine MN, Weitz JI, Kearon C, Wells PS, et al. Clinical utility of a rapid whole-blood D-dimer assay in patients with cancer who present with suspected acute deep venous thrombosis. Ann Intern Med. 1999;131:417–23. doi: 10.7326/0003-4819-131-6-199909210-00004. [DOI] [PubMed] [Google Scholar]
- 53.ten Wolde M, Kraaijenhagen RA, Prins MH, Büller HR. The clinical usefulness of D-dimer testing in cancer patients with suspected deep venous thrombosis. Arch Intern Med. 2002;162:1880–4. doi: 10.1001/archinte.162.16.1880. [DOI] [PubMed] [Google Scholar]
- 54.King V, Vaze AA, Moskowitz CS, Smith LJ, Ginsberg MS. D-dimer assay to exclude pulmonary embolism in high-risk oncologic population: Correlation with CT pulmonary angiography in an urgent care setting. Radiology. 2008;247:854–61. doi: 10.1148/radiol.2473070939. [DOI] [PubMed] [Google Scholar]
- 55.Di Nisio M, Rutjes AW, Büller HR. Combined use of clinical pretest probability and D-dimer test in cancer patients with clinically suspected deep venous thrombosis. J Thromb Haemost. 2006;4:52–7. doi: 10.1111/j.1538-7836.2005.01671.x. [DOI] [PubMed] [Google Scholar]
- 56.Di Nisio M, Sohne M, Kamphuisen PW, Büller HR. D-Dimer test in cancer patients with suspected acute pulmonary embolism. J Thromb Haemost. 2005;3:1239–42. doi: 10.1111/j.1538-7836.2005.01323.x. [DOI] [PubMed] [Google Scholar]
- 57.Righini M, Le Gal G, De Lucia S, Roy PM, Meyer G, Aujesky D, et al. Clinical usefulness of D-dimer testing in cancer patients with suspected pulmonary embolism. Thromb Haemost. 2006;95:715–9. [PubMed] [Google Scholar]
- 58.Cosmi B, Legnani C, Cini M, Guazzaloca G, Palareti G. The role of D-dimer and residual venous obstruction in recurrence of venous thromboembolism after anticoagulation withdrawal in cancer patients. Haematologica. 2005;90:713–5. [PubMed] [Google Scholar]
- 59.Ginsberg JS, Brill-Edwards P, Burrows RF, Bona R, Prandoni P, Büller HR, et al. Venous thrombosis during pregnancy: Leg and trimester of presentation. Thromb Haemost. 1992;67:519–20. [PubMed] [Google Scholar]
- 60.Chan WS, Chunilal S, Lee A, Crowther M, Rodger M, Ginsberg JS. A red blood cell agglutination D-dimer test to exclude deep venous thrombosis in pregnancy. Ann Intern Med. 2007;147:165–70. doi: 10.7326/0003-4819-147-3-200708070-00005. [DOI] [PubMed] [Google Scholar]
- 61.Kline JA, Williams GW, Hernandez-Nino J. D-dimer concentrations in normal pregnancy: New diagnostic thresholds are needed. Clin Chem. 2005;51:825–9. doi: 10.1373/clinchem.2004.044883. [DOI] [PubMed] [Google Scholar]
- 62.Kovac M, Mikovic Z, Rakicevic L, Srzentic S, Mandic V, Djordjevic V, et al. The use of D-dimer with new cutoff can be useful in diagnosis of venous thromboembolism in pregnancy. Eur J Obstet Gynecol Reprod Biol. 2010;148:27–30. doi: 10.1016/j.ejogrb.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 63.Morse M. Establishing a normal range for D-dimer levels through pregnancy to aid in the diagnosis of pulmonary embolism and deep vein thrombosis. J Thromb Haemost. 2004;2:1202–4. doi: 10.1111/j.1538-7836.2004.00776.x. [DOI] [PubMed] [Google Scholar]
- 64.Prandoni P, Noventa F, Ghirarduzzi A, Pengo V, Bernardi E, Pesavento R, et al. The risk of recurrent venous thromboembolism after discontinuing anticoagulation in patients with acute proximal deep vein thrombosis or pulmonary embolism. A prospective cohort study in 1,626 patients. Haematologica. 2007;92:199–205. doi: 10.3324/haematol.10516. [DOI] [PubMed] [Google Scholar]
- 65.Rathbun SW, Whitsett TL, Raskob GE. Negative D-dimer result to exclude recurrent deep venous thrombosis: A management trial. Ann Intern Med. 2004;141:839–45. doi: 10.7326/0003-4819-141-11-200412070-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Le Gal G, Righini M, Roy PM, Sanchez O, Aujesky D, Perrier A, et al. Value of D-dimer testing for the exclusion of pulmonary embolism in patients with previous venous thromboembolism. Arch Intern Med. 2006;166:176–80. doi: 10.1001/archinte.166.2.176. [DOI] [PubMed] [Google Scholar]
- 67.Cosmi B, Palareti G. Update on the predictive value of D-dimer in patients with idiopathic venous thromboembolism. Thromb Res. 2010;125(Suppl 2):S62–5. doi: 10.1016/S0049-3848(10)70016-5. [DOI] [PubMed] [Google Scholar]
- 68.Douketis J, Tosetto A, Marcucci M, Baglin T, Cushman M, Eichinger S, et al. Patient-level meta-analysis: Effect of measurement timing, threshold, and patient age on ability of D-dimer testing to assess recurrence risk after unprovoked venous thromboembolism. Ann Intern Med. 2010;153:523–31. doi: 10.7326/0003-4819-153-8-201010190-00009. [DOI] [PubMed] [Google Scholar]
- 69.Eichinger S, Minar E, Bialonczyk C, Hirschl M, Quehenberger P, Schneider B, et al. D-dimer levels and risk of recurrent venous thromboembolism. JAMA. 2003;290:1071–4. doi: 10.1001/jama.290.8.1071. [DOI] [PubMed] [Google Scholar]
- 70.Eichinger S, Heinze G, Jandeck LM, Kyrle PA. Risk assessment of recurrence in patients with unprovoked deep vein thrombosis or pulmonary embolism: The Vienna prediction model. Circulation. 2010;121:1630–6. doi: 10.1161/CIRCULATIONAHA.109.925214. [DOI] [PubMed] [Google Scholar]
- 71.Goldhaber SZ. Pulmonary embolism. N Engl J Med. 1998;339:93–104. doi: 10.1056/NEJM199807093390207. [DOI] [PubMed] [Google Scholar]
- 72.Kline JA, Courtney DM, Than MP, Hogg K, Miller CD, Johnson CL, et al. Accuracy of very low pretest probability estimates for pulmonary embolism using the method of attribute matching compared with the Wells score. Acad Emerg Med. 2010;17:133–41. doi: 10.1111/j.1553-2712.2009.00648.x. [DOI] [PubMed] [Google Scholar]
- 73.Büller HR, Agnelli G, Hull RD, Hyers TM, Prins MH, Raskob GE. Antithrombotic therapy for venous thromboembolic disease: The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(3 Suppl):401S–28. doi: 10.1378/chest.126.3_suppl.401S. [DOI] [PubMed] [Google Scholar]
- 74.Prandoni P. Acquired risk factors for venous thromboembolism in medical patients. Hematology Am Soc Hematol Educ Program. 2005;1:458–61. doi: 10.1182/asheducation-2005.1.458. [DOI] [PubMed] [Google Scholar]


