Abstract
Context:
Post-thyroidectomy hypoparathyroidism presenting with Parkinsonian features and seizures with extensive intracranial calcifications is uncommon. Acquired intracranial calcification that affects structures other than the basal ganglia is rare.
Case Report:
We report a case of a 45-year-old woman with a history of total thyroidectomy who presented with Parkinsonian features, cerebellar signs, and seizures. Brain imaging revealed extensive intracranial calcifications secondary to long-standing hypoparathyroidism. The patient was treated with intravenous (IV) calcium gluconate therapy and shifted to oral calcium and calcitriol therapy. Her symptoms improved markedly. At four months of follow up, the patient had not suffered another episode of seizure and was being gradually weaned off anti-Parkinsonian therapy.
Conclusion:
This case describes the rare finding of extensive intracranial calcifications in a case of iatrogenic hypoparathyroidism secondary to thyroidectomy with its wide array of features and its remarkable response to restoration of calcium levels to normal limits.
Keywords: Cerebellar and parkinsonian features after thyroidectomy, Hypoparathyroidism leading to seizures, Parkinsonism secondary to thyroidectomy
Introduction
Iatrogenic hypoparathyroidism presenting with Parkinsonian features and seizures with extensive intracranial calcifications is uncommon. Acquired Intracranial calcification that affects structures other than the basal ganglia is rare. However, we report a case of iatrogenic hypoparathyroidism after total thyroidectomy in a patient who presented with severe hypocalcemia and extensive calcifications of paraventricular, cerebellar, and basal ganglia regions, and recovered after calcium supplementation.
Case Presentation
A 45-year-old woman presented to the Medicine Emergency Room with new onset Generalized Tonic Clonic convulsions, tongue bite, and urinary incontinence for 48 hours before admission. The patient had been diagnosed as a case of Parkinson's syndrome two years back and put on anti-Parkinsonian therapy on the basis of clinical suspicion. Thereafter, her Parkinsonian features had improved.
She had a medical history of “Goiter” for which she had undergone total thyroidectomy 10 years back. She had been put on calcium supplements and levothyroxine therapy since her surgery, but she had been irregular with her treatment, with no follow-ups for last one and a half years. No family history of similar illness was present. The patient's parents were alive and healthy with no significant medical problems.
After initial stabilization of the patient with anticonvulsant therapy, the patient was evaluated better. There was painful spasm of hand on inflating sphygmomanometer cuff above systolic blood pressure (i.e., Trousseau's sign was positive). Chvostek sign was also positive. Intention tremors were present. Examination of neck revealed a scar of past thyroid surgery. The patient had cerebellar signs in the form of truncal ataxia, dysdiadochokinesia, dyssynergia, and past pointing. Tandem walking was impaired. Limbs were hypotonic with diminished tendon reflexes.
Investigations revealed: Hemoglobin-11.5 gm%, Total Leukocyte count-10,500/cu.mm (N64, L26, M05, E04, B01), Na-134.5 mEq/L, K-3.54 mEq/L, Fasting blood sugar-92 mg/dL, Urea-24 mg/dL, Creatinine-0.9 mg/dL, serum calcium-6.1 mg/dL, serum albumin-4.1 mg/dL. Serum LDH, Liver function tests, Magnesium, Chest X-ray, and abdominal USG revealed no abnormalities. Serum parathormone levels were inappropriately low for the level of hypocalcemia. ECG revealed a prolonged QT interval (QTc-0.58 s).
Brain CT revealed extensive intracranial calcifications. Dense calcium deposits were observed in the paraventricular, cerebellar, and basal ganglia regions [Figures 1 and 2].
Figure 1.
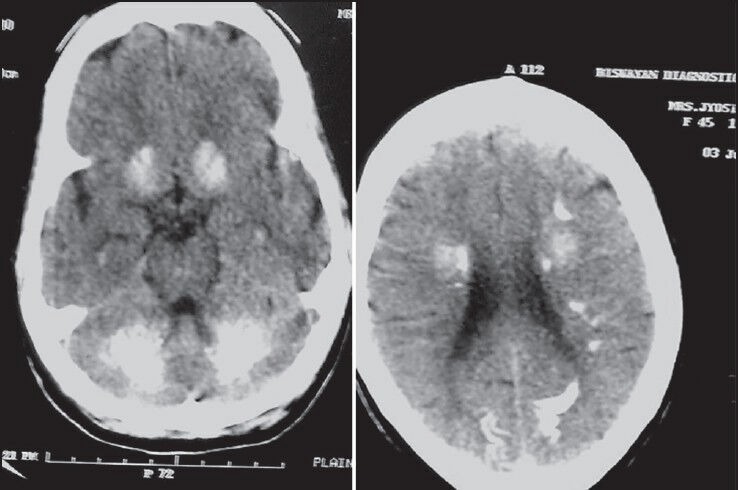
CT scan of brain shows extensive calcifications extending to paraventricular, cerebellar and basal ganglia regions
Figure 2.
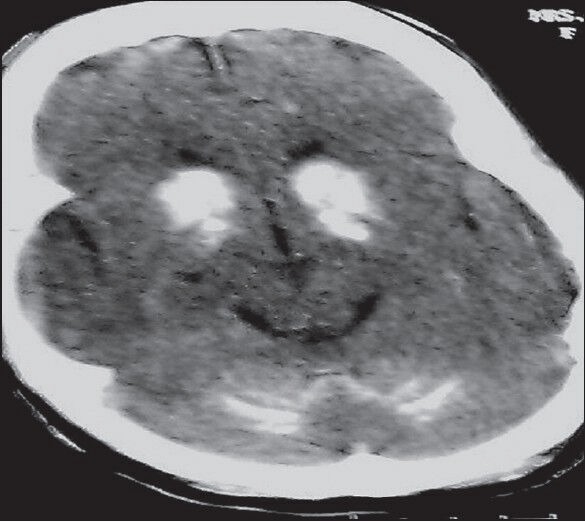
CT brain shows extensive basal ganglia and cerebellar calcifications
The patient was treated with intravenous (IV) calcium gluconate therapy and shifted to oral calcium and calcitriol therapy. Her symptoms improved markedly. By day 7 of hospital admission, the patient could walk back home. At four months of follow up, the patient had not suffered another episode of seizure and was being gradually weaned off anti-Parkinsonian therapy. Her serum calcium levels were well within normal limits at that time.
Discussion
Hypoparathyroidism is an endocrine disorder caused because of congenital disorders, iatrogenic causes, infiltration of the parathyroid glands, suppression of parathyroid function, or idiopathic mechanisms.[1] Acquired hypoparathyroidism is usually due to inadvertent removal of parathyroid gland during neck surgeries for hyperthyroidism, or it can occur due to removal of too much parathyroid gland during surgery for hyperparathyroidism.[2] Other rare causes of acquired hypoparathyroidism include radiation-induced damage subsequent to radioiodine therapy, sarcoidosis, hemochromatosis, hemosiderosis, Wilson's disease, and metastatic infiltration of the parathyroid gland.[2]
Postoperative hypoparathyroidism is the most common complication of complete or near-complete extirpation of thyroid gland by destruction or vascular compromise of parathyroid tissue.[3] Grave's disease, thyrotoxicosis caused by hyperactive thyroid adenomas, recurrent goiter, and thyroid carcinoma have a greater risk of resulting in permanent postoperative hypoparathyroidism after surgery.[4]
Brain calcinosis syndrome (BCS) is usually defined as bilateral calcium accumulation in the brain parenchyma, most often within the basal ganglia. The pathogenic mechanism of brain calcinosis in postoperative hypoparathyroidism is not yet defined.
Radiologically, hypoparathyroidism causes calcification most often in bilateral basal ganglia.[5] Thalami and cerebellum can be rarely involved. In our patient, calcinosis exceeds the common brain locations. A review of the literature reveals only few case reports of such excessive calcification of brain matter in postoperative hyperparathyroidism.[6,7,8] Armelisasso et al. also described occurrence of tonic clonic seizure in a 36-year-old male with hypoparathyroidism.[9] Garg et al. reported tonic clonic seizures in a female patient with hypoparathyroidism.[10] However, hardly any such case reports describe such extensive brain calcification acquired due to iatrogenic injury.
Our case report highlights a potentially treatable cause of Parkinsonian features and seizure disorder. It describes the rare finding of extensive intracranial calcifications in a case of iatrogenic hypoparathyroidism secondary to thyroidectomy. It also highlights how simple and effective treatment with oral calcium and calcitriol therapy can lead to rapid and miraculous resolution of symptoms in these cases.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Girija AS. Idiopathic hypoparathyroidism with extensive intracranial calcification associated with kinesogenicchoreoathetosis. J Assoc Physicians India. 2000;48:938–9. [PubMed] [Google Scholar]
- 2.Potts JT. Diseases of the parathyroid gland and other hyper and hypocalcemic disorders. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, et al., editors. Harrison's Principles of Internal Medicine. 17th ed. Vol. 2. New York: McGraw Hills; 2008. pp. 2377–96. [Google Scholar]
- 3.Wysolmerski, John J, Insogna LK. The parathyroid glans, hypercalcemia, and hypocalcemia. In: Cecil LR, Goldman L, Schafer IA, editors. Goldman's Cecil Medicine. 24th ed. Vol 2. Philadelphia: Elsevier/Saunders; 2011. p. 1597. [Google Scholar]
- 4.Thomusch O, Machens A, Sekulla C, Ukkat J, Brauckhoff M, Dralle H. The impact of surgical technique on postoperative hypoparathyroidism in bilateral thyroid surgery: A multivariate analysis of 5846 consecutive patients. Surgery. 2003;133:180–5. doi: 10.1067/msy.2003.61. [DOI] [PubMed] [Google Scholar]
- 5.Fulop M, Zeifer B. Case report: Extensive brain calcification in hypoparathyroidism. Am J Med Sci. 1991;302:292–5. doi: 10.1097/00000441-199111000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Lang C, Huk W, Pichl J. Comparison of extensive brain calcification in postoperative hypoparathyrodism on CT and NMR scan. Neuroradiology. 1989;31:29–32. doi: 10.1007/BF00342026. [DOI] [PubMed] [Google Scholar]
- 7.Rizvi I, Ansari NA, Beg M, Shamim MD. Widespread intracranial calcifications, seizures and extra-pyramidal manifestations in a case of hypoparathyroidism. N Am J Med Sci. 2012;4:369–72. doi: 10.4103/1947-2714.99523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Basak RC. A case report of basal ganglia calcification- a rare finding of hypoparathyroidism. Oman Med J. 2009;24:220–2. doi: 10.5001/omj.2009.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Armelisasso C, Vaccario ML, Pontecorvi A, Mazza S. Tonic-clonic seizures in a patient with primary hypoparathyroidism: A case report. Clin EEG Neurosci. 2004;35:97–9. doi: 10.1177/155005940403500209. [DOI] [PubMed] [Google Scholar]
- 10.Garg RK, Garg N, Tandon N, Khurana ML, Ammini AC. Idiopathic hypoparathyroidism presenting as epilepsy in a 40 years female. Neurol India. 1999;47:244–5. [PubMed] [Google Scholar]


