Abstract
Context:
When dealing with a patient with HIV that presents with an altered mental status, there are various infections and disease etiologies a physician has to rule out that may play a role in complicating the inherent complex nature of HIV. Toxoplasma gondii (T. gondii) and cytomegalovirus (CMV) affect a large part of the world's population and lead to a varied and broad symptomatology depending upon the severity of HIV, the CD4 count and how early the infection is diagnosed.
Case Report:
We report an HIV+ patient in his early 50s and with a low CD4 count that presented with severe lethargy and confusion. Imaging studies that were performed after stabilizing the patient revealed a ring-enhancing lesion in the brain and after further testing, a diagnosis of reactivated T. gondii with co-infection with CMV was made. Patients infected with T. gondii that are already immune-compromised deteriorate rapidly and the disease diagnosis poses several challenges.
Conclusion:
Clinicians have to be extremely careful about making a prompt diagnosis and initiate treatment without delay before the infection takes a deadly toll on the patient. Since our patient was not on the required prophylactic medication to prevent infection with T. gondii, it was imperative to start treatment in a timely manner and to monitor the patient for any further decline in functioning.
Keywords: Cytomegalovirus, Encephalitis, HIV, Toxoplasmosis
Introduction
Several opportunistic infections play a huge part in complicating the disease process in patients infected with HIV. One of the most common ones, Toxoplasma gondii, is an obligate intracellular parasitic protozoan that affects up to a third of the global population.
People with an intact immune response who get infected with T. gondii produce mild flu-like symptoms that resolve on their own with time. However, among patients with AIDS, more than 95% of toxoplasma encephalitis is due to recrudescence of a latent infection as a result of the progressive loss of cellular immune surveillance.[1] The primary manifestation in AIDS patients infected with toxoplasma is encephalitis. The infection usually arises when the CD4 count falls below 100/mm3. There is a tendency for the parasite to cause localized disease in the brain stem, basal ganglia, pituitary gland and corticomedullary junction.[2] The spontaneous and simultaneous development of multifocal lesions strongly suggest that although toxoplasma encephalitis arises because of reactivation of a latent infection, the multiple areas of the brain that are involved are likely a result of hematogenous spread of the parasite.[2] Clinical presentation of toxoplasma encephalitis varies greatly depending upon the severity of HIV determined by the CD4 count and a patient could present with acute onset of confusion with or without focal neurological deficits. Some of the focal signs include cranial nerve palsies, focal seizures, severe headaches, hemiplegia and hemiparesis. The focal neurological problems may be subtle and transient initially and with time evolve to persistent focal neurological deficits or may result in a rapidly fatal disease.[3] Non-focal symptoms include confusion, coma, lethargy and weakness.
On the other hand, cytomegalovirus (CMV) is a virus that primarily causes an infection of the central nervous system. A large majority of the adult population in the United States is infected with CMV and any pathology resulting in a suppressed immune system can lead to reactivation in an asymptomatic individual. Risk factors for reactivation include post tissue or bone marrow transplant and HIV/AIDS where the CD4 count is less than 100/mm3 or viral load is more than 1,000.[4] In an autopsy series of 47 patients with AIDS, 75% of those with CMV retinitis involving the peripapillary area also had encephalitis.[5] CMV encephalitis characterized by microglial nodules and focal parenchymal necrosis manifests with a more indolent change in mental status, very similar to AIDS dementia complex (ADC).[4] Some of the neurological findings vastly overlap with those of toxoplasmosis encephalitis and include ataxia, hemiparesis, aphasia and seizures.
Case Presentation
A 52-year-old male with a past medical history significant for hypertension and alcohol abuse was brought into the emergency room by a friend upon being at home sitting in his own excretions. He was non-responsive at the time of admission and slowly gained some consciousness and was able to verbalize a little but the speech was incoherent. The patient had a reported history of alcohol abuse. Upon physical examination, the patient had a temperature of 100˚F. He looked toxic and unkempt. Nails showed leukonychia with discoloration and were poorly kept with dirt. He had diffuse maculopapular rash on all extremities, including the trunk. Patient's laboratory tests revealed the following: White count, 17.4; with normal chemistry panel. Chest X-ray showed no acute infiltrates. Computed tomography (CT) scan of the head showed extensive low attenuation with mild mass effect predominantly affecting white matter bilaterally but also affecting the left basal ganglia. Possibilities include encephalitis, most likely viral. Toxic/metabolic or ischemic processes are considered less likely [Figure 1]. CT angiogram was performed as patient was also in respiratory distress, which showed a saddle embolus [Figure 2].
Figure 1.
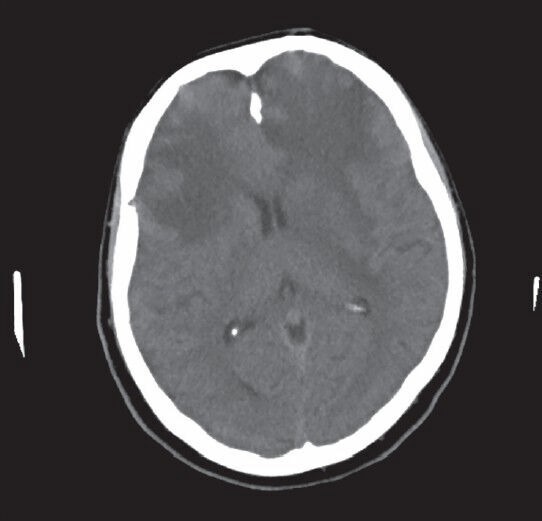
CT scan of the head showed extensive low attenuation with mild mass effect predominantly affecting white matter bilaterally
Figure 2.
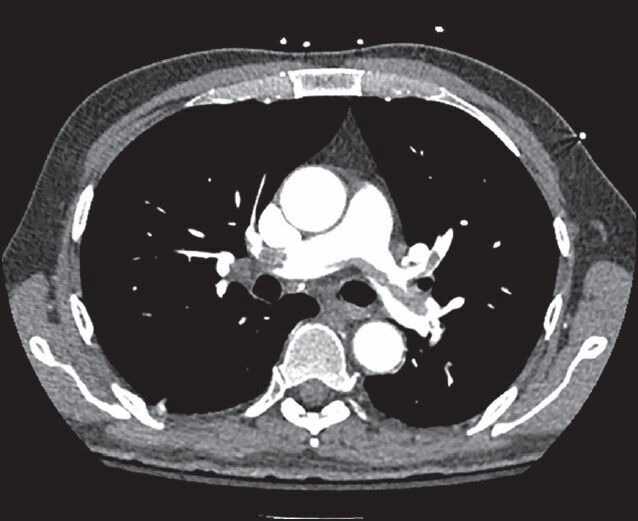
CT angiogram chest showing pulmonary embolus
Initially, the patient was treated with intravenous (IV) Vancomycin and Zosyn after being admitted to the intensive care unit. IV folic acid and thiamine were administered after considering the fact that the patient had been abusing alcohol for a long time and alcohol detox protocol was added to prevent delirium tremens and agitative behavior. Patient was also started on therapeutic dose of Lovenox for pulmonary embolism. Lumbar puncture was performed, which showed cerebrospinal fluid (CSF) protein 96 mg/dl, glucose 65 mg/dl, Mononuc 99% and PMN 1%. Acyclovir was started suspecting for herpes encephalitis. Rapid HIV test came out positive; viral load and Phenosense were ordered. Serology for HIV was found to be positive and CD4 count was noted to be 13. Magnetic resonance imaging (MRI) of the brain was done, which showed multiple bilateral supratentorial and infratentorial ring-enhancing lesions, measuring up to 3.4 × 1.9 cm in the left frontal lobe with extensive amount of vasogenic edema surrounding these lesions with a 4 mm rightward midline shift. These lesions exhibit peripheral ring-like low diffusivity, corresponding to the area of enhancement, without central low diffusivity, which is suspicious for toxoplasmosis [Figure 3]. Taking midline shift and saddle pulmonary embolism into consideration, the patient was transferred to a tertiary care center where he was found to be positive for CMV in CSF and T. gondii via PCR. He was treated with embolectomy for pulmonary embolism and CMV, and toxoplasmosis with resolution of his symptoms. He is currently being followed in our HIV clinic for HIV/AIDS management.
Figure 3.
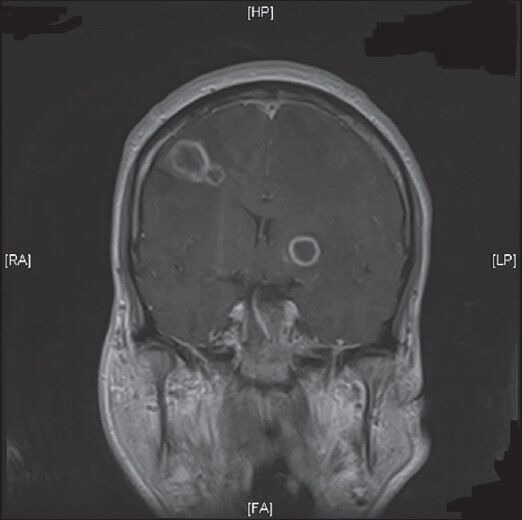
MRI of the brain showing ring-enhancing lesions, largest measuring up to 3.4 × 1.9 cm in the left superior frontal lobe
Discussion
As observed in our patient, this is not a very unusual presentation in patients infected with HIV, which is at a far enough stage to cause central nervous system dysfunction, thus causing lethargy and apathy. Clinical presentation of T. gondii vastly depends upon the age and immune status of the patient. As stated earlier, the infection is usually benign in immunocompetent people of all age groups and resolves on its own with time. In contrast, patients who are immunocompromised with T. gondii can have devastating effects. Some of the varied clinical presentations include an acute confusional state with or without focal neurological deficits, chorioretinitis, pneumonitis or multi-organ failure.[6] An HIV+ patient who presents with fever, confusion, ataxia and a ring enhancing lesion of brain MRI should raise a suspicion for reactivation toxoplasmosis and such a patient is also prone to seizures and other focal neurological deficits due to the mass effect of the intracerebral lesion. A number of methods have been employed to correctly diagnose T. Gondii of which the main the most common and effective ones include polymerase chain reaction and serology. Direct diagnosis can be made with tissue sections or body fluid smears that demonstrate tachyzoites.[7] Patients that are severely immunocompromised can be tested by subjecting body fluids and tissues to PCR amplification of T gondii genes which offers a sensitivity of 50% but a very high specificity.[7] Because cerebral toxoplasmosis in AIDS patients most commonly results from reactivation of a prior primary infection, patients should be screened for antibodies against T. gondii at the time of diagnosis with HIV. Some of the most common medications used to treat active toxoplasmic infection include pyrimethamine, sulfadiazine and folinic acid. The duration of treatment is usually 2-4 months and can be altered based on resolution of exacerbation of the symptoms. Maintenance therapy can be started after the acute phase has resolved and should consist of the same regimen as in the acute phase but at half dose[8] and later discontinued if patients have sustained (for at least 6 months) CD4 counts of >200 cells/μL on HAART. Patients who test positive for antibodies at the time of screening should be treated prophylactically with trimethoprim/sulfamethoxazole. Primary prophylaxis for toxoplasma encephalitis can be discontinued in patients who have responded to effective HAART with sustained CD4 counts of >200 cells/μL for at least 3 months.
Our patient was also found to be positive for CMV infection. Clinical presentation can be markedly different and some of the most common manifestations include ventriculo-encephalitis with abrupt onset of confusion and lethargy, polyradiculopathy, transverse myelitis, non-specific gastrointestinal symptoms, including bloody diarrhea and CMV pneumonitis, which presents as cough, fever and sputum production. CMV causing lesions are not just limited to the brain as the infection has been found to infect peripheral nerves and spinal cords too. The diagnosis of CMV is extremely difficult to make and often poses a huge challenge to physicians. Even when investigations are performed early in the course of the disease, results may be misleadingly negative: Cerebrospinal fluid cell count is normal in 5-10% of patients, particularly in children; CT results are normal in the first week of illness in up to a third of patients; MRI images are normal in 10%; and detection of viral DNA by PCR can be negative initially.[9] Good history taking still remains of utmost importance and if the patient is extremely disoriented to provide details, every effort should be made to reach out to friends and family to seek information about recent travel, exposure to animals or occupation hazards that might have predisposed him to any possible risk factors. Brain imaging and CSF analysis still remain two of the best modalities to diagnose the infection. An MRI would show ventriculitis, meningitis, infarcts, hydrocephalus and cerebral atrophy.[10] CSF findings would show normal glucose, elevated protein count and mononuclear leukocytosis. PCR of the CSF can help make a definitive diagnosis, which has a high sensitivity and specificity. For CMV encephalitis, particularly prominent in HIV infection, combination therapy with intravenous gancylovir plus or minus foscarnet has been recommended.[11] Current guidelines recommend discontinuation of secondary prophylaxis in HAART recipients with a sustained (>6 mo) increase in CD4+ T cells to greater than 100-150 cells/μL.[12] CMV prophylaxis with oral ganciclovir should be considered for patients with CD4 lymphocyte counts below 50 cells/μL who may be at increased risk for retinitis.
For a patient like ours who is HIV+ and who was brought to the hospital in an extremely confused state, it becomes imperative to rule out any opportunistic infection as soon as possible or to initiate treatment if the disease is suspected based on clinical presentation.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Luft BJ, Remington JS. AIDS commentary Toxoplasmic encephalitis. J Infect Dis. 1988;157:1–6. doi: 10.1093/infdis/157.1.1. [DOI] [PubMed] [Google Scholar]
- 2.Dannemann BR, McCutchan JA, Israelski DM, Antoniskis D, Leport C, Luft B, et al. Treatment of toxoplasmic encephalitis in patients with AIDS. A randomized trial comparing pyrimethamine plus clindamycin to pyrimethamine plus sulfonamides. The California Collaborative Treatment Group. Ann Intern Med. 1992;116:33–43. doi: 10.7326/0003-4819-116-1-33. [DOI] [PubMed] [Google Scholar]
- 3.Post MJ, Chan JC, Hensley GT, Hoffman TA, Moskowitz LB, Lippmann S. Toxoplasma encephalitis in Haitian adults with acquired immunodeficiency syndrome: A clinical-pathologic-CT correlation. AJR Am J Roentgenol. 1983;140:861–8. doi: 10.2214/ajr.140.5.861. [DOI] [PubMed] [Google Scholar]
- 4.Robinson-Papp J, Simpson DM. Neuromuscular diseases associated with HIV-1 infection. Muscle Nerve. 2009;40:1043–53. doi: 10.1002/mus.21465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bylsma SS, Achim CL, Wiley CA, Gonzalez C, Kuppermann BD, Berry C, et al. The predictive value of cytomegalovirus retinitis for cytomegalovirus encephalitis in acquired immunodeficiency syndrome. Arch Ophthalmol. 1995;113:89–95. doi: 10.1001/archopht.1995.01100010091026. [DOI] [PubMed] [Google Scholar]
- 6.Coelho RA, Kobayashi M, Carvalho LB., Jr Prevalence of IgG antibodies specific to Toxoplasma gondii among blood donors in Recife, Northeast Brazil. Rev Inst Med Trop Sao Paulo. 2003;45:229–31. doi: 10.1590/s0036-46652003000400011. [DOI] [PubMed] [Google Scholar]
- 7.Jones JL, Kruszon-Moran D, Sanders-Lewis K, Wilson M. Toxoplasma gondii infection in the United States, 1999 2004, decline from the prior decade. Am J Trop Med Hyg. 2007;77:405–10. [PubMed] [Google Scholar]
- 8.Liesenfeld O, Montoya JG, Kinney S, Press C, Remington JS. Effect of testing for IgG avidity in the diagnosis of Toxoplasma gondii infection in pregnant women: Experience in a US reference laboratory. J Infect Dis. 2001;183:1248–53. doi: 10.1086/319672. [DOI] [PubMed] [Google Scholar]
- 9.Chaudhuri A, Kennedy PG. Diagnosis and treatment of viral encephalitis. Postgrad Med J. 2002;78:575–83. doi: 10.1136/pmj.78.924.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cinque P, Cleator GM, Weber T, Monteyne P, Sindic C, Gerna G, et al. Diagnosis and clinical management of neurological disorders caused by cytomegalovirus in AIDS patients. European Union Concerted Action on Virus Meningitis and Encephalitis. J Neurovirol. 1998;4:120–32. doi: 10.3109/13550289809113490. [DOI] [PubMed] [Google Scholar]
- 11.Springer KL, Weinberg A. Cytomegalovirus infection in the era of HAART: Fewer reactivations and more immunity. J Antimicrob Chemother. 2004;54:582–6. doi: 10.1093/jac/dkh396. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan JE, Benson C, Holmes KK, Brooks JT, Pau A, Masur H. Centers for Disease Control and Prevention (CDC); National Institutes of Health; HIV Medicine Association of the Infectious Diseases Society of America. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: Recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep. 2009;58:1–207. [PubMed] [Google Scholar]


