Introduction
Indoor air pollution is the degradation of indoor air quality by harmful chemicals and other materials; it can be up to 10 times worse than outdoor air pollution. This is because contained areas enable potential pollutants to build up more than open spaces. Statistics suggest that in developing countries, health impacts of indoor air pollution far outweigh those of outdoor air pollution. Indoor air pollution from solid fuels accounted for 3.5 million deaths and 4.5% global daily-adjusted life year (DALY) in 2010; it also accounted for 16% particulate matter pollution. Though there is a decrease in household air pollution from solid fuels in southeast Asia, still it ranked third among risk factors in the report of the Global Burden of Disease.(1) This paper provides an evidence-based insight into indoor air pollution, its effect on health, and suggested control measures.
Status of Indoor Air Pollution in India
The principal sources of indoor air pollution are: Combustion, building material, and bioaerosols.(2) While radon, asbestos, pesticides, heavy metals, volatile organic matter, and environmental tobacco smoke are considered major indoor pollutants in developed countries, the combustion products of biomass fuels contribute most to indoor air pollution in developing nations. In India, out of 0.2 billion people using fuel for cooking; 49% use firewood; 8.9% cow dung cake; 1.5% coal, lignite, or charcoal; 2.9% kerosene; 28.6% liquefied petroleum gas (LPG); 0.1% electricity; 0.4% biogas; and 0.5% any other means.(3)
The incomplete combustion products of biomass fuels include suspended particulate matter, carbon monoxide, polyaromatic hydrocarbons, polyorganic matter, formaldehyde, etc., which have adverse effects on health. The combustion of coal results in production of oxides of sulfur, arsenic, and fluorine. Pollutants such as aldehydes, volatile, and semivolatile organic compounds are produced from resins, waxes, polishing materials, cosmetics, and binders. Lastly; biological pollutants like dust mites, molds, pollen, and infectious agents produced in stagnant water, mattresses, carpets, and humidifiers too pollute indoor air.(4)
A study on quantifying exposures to respiratory particulate matter found concentrations of particulate matter ranging from 500 to 2,000 mg/m3 during cooking in biomass-using households. Average 24-h exposures ranged from 82 ± 39 mg/m3 for those using clean fuels, to 231 ± 109 mg/m3 for those who used biomass fuel for cooking.(5) In indoor air, carbon monoxide levels during cooking by dung, wood, coal, kerosene, and LPG were found to be 144, 156, 94, 108, and 14 mg/m3, respectively. The indoor levels of total polyaromatic hydrocarbons during use of dung, wood, coal, kerosene, and LPG were 3.56, 2.01, 0.55, 0.23, and 0.13 mg/m3 of air, respectively.(6) The formaldehyde mean levels were 670, 652, 109, 112, and 68 mg/m3, respectively, for dung, wood, coal, kerosene, and LPG.(7)
Effects of Indoor Air Pollution on Health
The ill-effects of indoor air pollution result in about 2 million premature deaths per year, wherein 44% are due to pneumonia, 54% from chronic obstructive pulmonary disease (COPD), and 2% from lung cancer.(8) The most affected groups are women and younger children, as they spend maximum time at home.(8) The morbidities associated with indoor air pollution are respiratory illnesses, viz., acute respiratory tract infection(9) and COPD,(10) poor perinatal outcomes like low birth weight(11) and still birth, cancer of nasopharynx, larynx, lung,(12) and leukemia. The harmful health effects of formaldehyde range from being an acute irritant, reducing vital capacity, causing bronchitis, to being a carcinogen causing leukemia and lung cancer.(13,14) There are few studies done so far to show the effect of wood smoke on cardiovascular health. A study from Guatemala reported that reduction in wood smoke exposure by use of improved chimney stove resulted in lowering of systolic blood pressure by 3.7 mmHg (95% confidence interval (CI): -8.1, 0.6) and diastolic blood pressure by 3.0 mmHg (95% CI: -5.7, -0.4).(15) Another study reported reduction in ST-segment depression (odds ratio (OR) 0.26, 95% CI: 0.08, 0.90) on electrocardiogram after stove intervention.(16)
The indoor air pollutants have potential health effects.(17) The particulates cause respiratory infections, chronic bronchitis, COPD, and also lead to exacerbation of COPD. Sulfur dioxide and nitrogen dioxide cause wheezing and exacerbation of asthma. In addition to this, nitrogen dioxide causes respiratory infections and deteriorates lung functions. Sulfur dioxide has an additional etiological role in exacerbation of COPD and cardiovascular disease. The risk of poor perinatal outcomes, viz., low birth weight and perinatal death increases from exposure to carbon monoxide. Biomass smoke, especially metal ions and polycyclic aromatics, leads to development of cataract. Polycyclic aromatic hydrocarbons lead to development of cancers of lungs, mouth, nasopharynx, and larynx. As a consequence of poverty, factors such as living conditions, sanitation, and access to water are associated with solid fuel use, and should be considered while measuring impact of solid fuel on child survival.(17)
Various studies in India have reported harmful effects of indoor air pollution. In a large case-control study, after adjustment for demographic factors and living conditions, solid-fuel use significantly increased child deaths at ages 1-4 years (prevalence ratio boys: 1.30, 95% CI: 1.08-1.56; girls: 1.33, 95% CI: 1.12-1.58). More girls than boys died from exposure to solid fuels. Solid fuel use was also associated with nonfatal pneumonia (boys: Prevalence ratio 1.54; 95% CI: 1.01-2.35; girls: Prevalence ratio 1.94; 95% CI: 1.13-3.33).(18)
The use of fuel other than LPG was significantly associated with acute lower respiratory tract infection even after adjusting for other risk factors (adjusted OR = 4·73, 95% CI: 1.67-13.45). In children with acute lower respiratory infection, 24.8% had pneumonia, 45.5% had severe pneumonia, and 29.7% had very severe disease.(19) In Ladakh, due to severe cold, and ventilation kept to a minimum, the inmates are exposed to high concentration of soot, resulting in morbidities which resemble pneumoconiosis.(20,21) The use of biomass fuel was associated with significantly prolonged nasal mucociliary clearance time (765.8 ± 378.16 s) in comparison to clean fuel users (545.4 ± 215.55 s), and reduced peak expiratory flow rate (319.3 l/min) as compared to clean fuel users (371.7 l/min).(22)
The use of biomass as a cooking fuel was found to be significantly associated with a high prevalence of active tuberculosis (OR = 3.56, 95% CI: 2.82-4.50). The prevalence remained large and significant even after analyzing separately for men (OR = 2.46) and women (OR = 2.74) and for urban (OR = 2.29) and rural areas (OR = 2.65). Fifty-one percent of prevalence of active tuberculosis is attributable to cooking smoke in the age group 20 years and above.(23)
Results from a study among elderly men and women (age ≥ 60 years) showed higher prevalence of asthma in households using biomass fuels than those using cleaner fuels (OR = 1.59; 95% CI: 1.30-1.94). As compared to men (OR = 1.83; 95% CI: 1.32-2.53), the effect of cooking smoke on asthma was greater among women after adjustment.(24) The results from a study conducted in southern India reported a higher prevalence of COPD among biomass fuel user than clean fuel users (OR: 1.24; 95% CI: 0.36-6.64). It also found that the prevalence was two times higher in women spending more than 2 h a day in cooking.(25) Biomass fuels contain carcinogens like polyaromatic hydrocarbons, formaldehyde, etc. A case-control study among women diagnosed with lung cancer reported that in addition to tobacco, exposure to biomass fuels also leads to development of lung cancer. In nonsmoker women, exposure to biomass fuel was associated with higher risk of developing lung cancer (OR 3.04, 95% CI: 1.1-8.38). The exposure to biomass fuel remained significantly associated with lung cancer despite adjusting for other factors like smoking and passive smoking.(26)
As compared to the use of cow dung and wood smoke, LPG use was found to be associated with cortical, nuclear, and mixed cataract with an odds ratio of 0.69 (95% CI: 0.4-0.9),(27) whereas biomass fuel use resulted in partial or complete blindness with odds of 1.32 (95% CI: 1.2-1.5), as compared to other fuels.(28) Similar studies in western India reported use of wood to be an important cause of age-dependent cataract (OR = 2.12, 95% CI: 1.03-4.34). Coal and cattle dung use resulted in eye irritation (OR = 2.04, 95% CI: 1.13-3.68) and (OR = 1.83, 95% CI: 1.35-2.47), respectively.(29)
The higher levels of carbon monoxide due to biomass fuels in houses, resulted in higher carboxyhemoglobin levels, which were comparable to smokers.(30) A study among users of biomass fuels during pregnancy found a 50% excess risk of stillbirths.(31) The exposure to biomass fuel was associated with 49% increased risk of low birth weight babies.(32) Mothers from households using high pollution fuels were 1.4 (OR 1.41, 95% CI: 1.27, 1.55) times more likely to give birth to a low birth weight baby as compared to those using cleaner fuels. The use of biomass fuel during pregnancy was found to be associated with size at birth. As compared to newborns born in households using low pollution fuels (electricity, LPG, biogas, and natural gas), those born in households using high pollution fuels (wood, straw, animal dung, crop residue, coal, and charcoal) were 73 g lighter (mean birth weight 2,883.8 g versus 2,810.7 g, P < 0.001).(33)
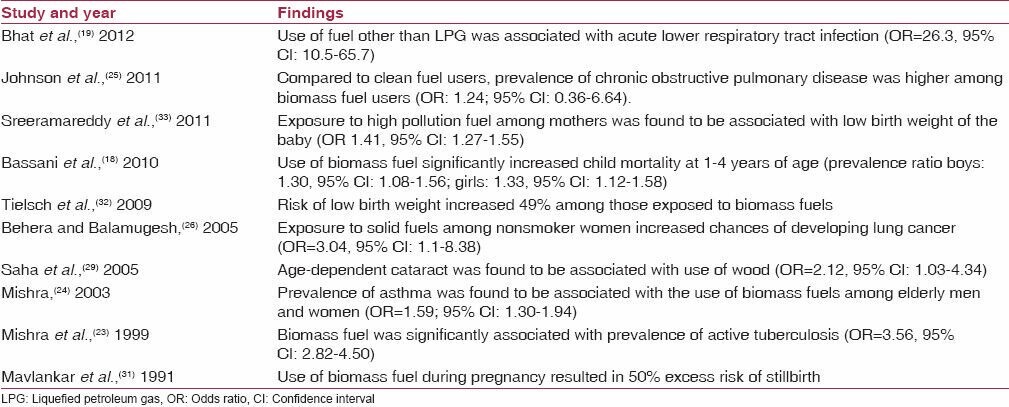
The effects of indoor air pollution in India on health are depicted in Table 1.
Table 1.
Effects of indoor air pollution in India on health
Control Measures
Studies done so far in India provide us enough evidence that indoor air pollution is a cause of increasing morbidities and mortalities, and there is a need for an urgent intervention. There are social, cultural, and financial factors that influence the decision of people about energy and cooking.(34) Other factors include the availability and flexibility of traditional fuels, the type of dishes prepared, the taste of food, the problems with smoke, the aesthetic appeal of stoves, and users' perception about other alternatives. Following is a list of suggested measures which should be adopted to curb the menace of indoor air pollution:
Public awareness: One of the most important steps in prevention of indoor air pollution is education, viz., spreading awareness among people about the issue and the serious threat it poses to their health and wellbeing. The education should help people in finding different ways of reducing exposures with better kitchen management and protection of children at home. People should also be educated about the use of alternative cleaner sources of energy to replace direct combustion of biomass fuel. The stakeholders must include not only public, but also politicians and administrators to ensure their commitment and increase their awareness about health effects of indoor air pollution.
Change in pattern of fuel use: Fuel use depends on ones' habit, its availability, and most importantly, its affordability. At present, majority of low income families rely solely on direct combustion of biomass fuels for their cooking needs as this is the cheapest and easiest option available to them; however, this could be rectified by promoting the use of cleaner energy sources such as gobar gas which utilizes cow dung to produce gas for cooking.
Modification of design of cooking stove: The stoves should be modified from traditional smoky and leaky cooking stoves to the ones which are fuel efficient, smokeless and have an exit (e.g., chimney) for indoor pollutants. A good example is the one designed by the National Biomass Cookstoves Initiative, of the Ministry of New and Renewable Energy under a Special Project on Cookstove during 2009-2010, with the primary aim of enhancing the availability of clean and efficient energy for the energy deficient and poorer sections of the country.(35)
Improvement in ventilation: During construction of a house, importance should be given to adequate ventilation; for poorly ventilated houses, measures such as a window above the cooking stove and cross ventilation though doors should be instituted.
Intersectoral coordination and global initiative: Indoor air pollution can only be controlled with coordinated and committed efforts between different sectors concerned with health, energy, environment, housing, and rural development.
Tackling indoor air pollution and providing universal access to clean household energy is a great opportunity to improve health, reduce poverty, and protect our environment; thus, contributing significantly to achieving the Millennium Development Goals (MDGs) which are listed below:
Improved household energy practices will provide opportunities for income generation-MDG 1 (eradicate extreme poverty and hunger).
With less time spent on fuel collection and lost due to ill health, children will have more time for school attendance and homework-MDG 2 (achieve universal primary education).
Freeing women's time for income generation will help in eradicating poverty and hunger (MDG 1) and achieving gender equality (MDG 3).
Better respiratory health: MDG 4 ( reduce child mortality), MDG 5 (improve maternal health), and MDG 6 (combat HIV/AIDS, malaria and other diseases like tuberculosis).
Use of clean household energy will ensure environmental sustainability; the World Health Organization is the agency responsible for reporting the “proportion of the population using solid fuels” as an indicator for reporting progress towards MDG 7 to ensure environmental sustainability (MDG 7).
An intersectoral approach for use of clean household energy practices will lead to economic and social development-MDG 8 (develop a global partnership for development).
Conclusion
Though evidence exists for increase in indoor air pollution in India, and its association with both increased morbidity and mortality, there is still a need of further studies to assess the exposure levels of indoor pollutants and to further strengthen the evidence for their association with outcomes like tuberculosis, cataract, asthma, cardiovascular health, and cancers. At the same time, effective interventions, starting from education, change in fuel patterns, proper designing of stoves and houses, to a committed and determined intersectoral coordination towards promotion of public health is the need of the hour.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Indoor air pollution in India — a major environmental and public health concern. [Last accessed on 2013 Mar 10];ICMR Bulletin. 2001 31:1–9. Available from: http://www.icmr.nic.in/bumay01.pdf . [Google Scholar]
- 3.Houselisting and Housing Census Data Highlights — 2011. [Last accessed on 2013 Mar 16]. Available from: http://www.censusindia.gov.in/2011census/hlo/hlo_highlights.html .
- 4.Zhang J, Smith KR. Indoor air pollution: A global health concern. Br Med Bull. 2003;68:209–25. doi: 10.1093/bmb/ldg029. [DOI] [PubMed] [Google Scholar]
- 5.Balakrishnan K, Sankar S, Parikh J, Padmavathi R, Srividya K, Venugopal V, et al. Daily average exposures to respirable particulate matter from combustion of biomass fuels in rural households of southern India. Environ Health Perspect. 2002;110:1069–75. doi: 10.1289/ehp.021101069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel TS, Aryan CV. Indoor air quality: Problems and perspectives. In: Shukla PR, editor. Energy Strategies and Greenhouse Gas Mitigation. 1st ed. New Delhi: Allied Publishers Limited; 1997. p. 72. [Google Scholar]
- 7.Raiyani CV, Jana JP, Desai NM, Shah SH, Shah PG, Kashyap SK. Assessment of indoor exposure to polycyclic aromatic hydrocarbons for urban poor using various types of cooking fuels. Bull Environ Contam Toxicol. 1993;50:757–63. doi: 10.1007/BF00194673. [DOI] [PubMed] [Google Scholar]
- 8.Indoor air pollution and health. [Last accessed on 2013 Mar 20]. Available from: http://www.who.int/mediacentre/factsheets/fs292/en .
- 9.Dherani M, Pope D, Mascarenhas M, Smith KR, Weber M, Bruce N. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under five years: A systematic review and meta-analysis. Bull World Health Organ. 2008;86:390–8C. doi: 10.2471/BLT.07.044529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kurmi OP, Semple S, Simkhada P, Smith WC, Ayres JG. COPD and chronic bronchitis risk of indoor air pollution from solid fuel: A systematic review and meta-analysis. Thorax. 2010;65:221–8. doi: 10.1136/thx.2009.124644. [DOI] [PubMed] [Google Scholar]
- 11.Pope DP, Mishra V, Thompson L, Siddiqui AR, Rehfuess EA, Weber M, et al. Risk of low birth weight and stillbirth associated with indoor air pollution from solid fuel use in developing countries. Epidemiol Rev. 2010;32:70–81. doi: 10.1093/epirev/mxq005. [DOI] [PubMed] [Google Scholar]
- 12.Sapkota A, Gajalakshmi V, Jetly DH, Roychowdhury S, Dikshit RP, Brennan P, et al. Indoor air pollution from solid fuels and risk of hypopharyngeal/laryngeal and lung cancers: A multicentric case control study from India. Int J Epidemiol. 2008;37:321–8. doi: 10.1093/ije/dym261. [DOI] [PubMed] [Google Scholar]
- 13.Blair A, Saracci R, Stewart PA, Hayes RB, Shy C. Epidemiologic evidence of the relationship between formaldehyde exposure and cancer. Scand J Work Environ Health. 1990;16:381–93. doi: 10.5271/sjweh.1767. [DOI] [PubMed] [Google Scholar]
- 14.Acheson ED, Barnes HR, Gardner MJ, Osmond C, Pannet B, Taylor CP. Formaldehyde process workers and lung cancer. Lancet. 1984;1:1066–7. doi: 10.1016/s0140-6736(84)91466-1. [DOI] [PubMed] [Google Scholar]
- 15.McCracken JP, Smith KR, Díaz A, Mittleman MA, Schwartz J. Chimney stove intervention to reduce long-term wood smoke exposure lowers blood pressure among Guatemalan women. Environ Health Perspect. 2007;115:996–1001. doi: 10.1289/ehp.9888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCracken JP, Smith KR, Stone P, Díaz A, Arana B, Schwartz J. Intervention to lower household wood smoke exposure in Guatemala reduces ST-segment depression on electrocardiograms. Environ Health Perspect. 2011;119:1562–8. doi: 10.1289/ehp.1002834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bruce N, Perez-Padilla R, Albalak R. Indoor air pollution in developing countries: A major environmental and public health challenge. Bull World Health Organ. 2000;78:1078–92. [PMC free article] [PubMed] [Google Scholar]
- 18.Bassani DG, Jha P, Dhingra N, Kumar R. Child mortality from solid-fuel use in India: A nationally-representative case-control study. BMC Public Health. 2010;10:491. doi: 10.1186/1471-2458-10-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramesh Bhat Y, Manjunath N, Sanjay D, Dhanya Y. Association of indoor air pollution with acute lower respiratory tract infections in children under 5 years of age. Paediatr Int Child Health. 2012;32:132–5. doi: 10.1179/2046905512Y.0000000027. [DOI] [PubMed] [Google Scholar]
- 20.Norboo T, Yahya M, Bruce NG, Heady JA, Ball KP. Domestic pollution and respiratory illness in a Himalayan village. Int J Epidemiol. 1991;20:749–57. doi: 10.1093/ije/20.3.749. [DOI] [PubMed] [Google Scholar]
- 21.Norboo T, Angchuk PT, Yahya M, Kamat SR, Pooley FD, Corrin B, et al. Silicosis in a Himalayan village population: Role of environmental dust. Thorax. 1991;46:341–3. doi: 10.1136/thx.46.5.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Priscilla J, Padmavathi R, Ghosh S, Paul P, Ramadoss S, Balakrishnan K, et al. Evaluation of mucociliary clearance among women using biomass and clean fuel in a periurban area of Chennai: A preliminary study. Lung India. 2011;28:30–3. doi: 10.4103/0970-2113.76298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mishra VK, Retherford RD, Smith KR. Biomass cooking fuels and prevalence of tuberculosis in India. Int J Infect Dis. 1999;3:119–29. doi: 10.1016/s1201-9712(99)90032-2. [DOI] [PubMed] [Google Scholar]
- 24.Mishra V. Effect of indoor air pollution from biomass combustion on prevalence of asthma in the elderly. Environ Health Perspect. 2003;111:71–8. doi: 10.1289/ehp.5559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson P, Balakrishnan K, Ramaswamy P, Ghosh S, Sadhasivam M, Abirami O, et al. Prevalence of chronic obstructive pulmonary disease in rural women of Tamilnadu: Implications for refining disease burden assessments attributable to household biomass combustion. Global Health Action. 2011;4:7226. doi: 10.3402/gha.v4i0.7226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Behera D, Balamugesh T. Indoor air pollution as a risk factor for lung cancer in women. J Assoc Physicians India. 2005;53:190–2. [PubMed] [Google Scholar]
- 27.Mohan M, Sperduto RD, Angra SK, Milton RC, Mathur RL, Underwood BA, et al. India-US case control study of age-related cataracts. India-US Case-Control Study Group. Arch Ophthalmol. 1989;107:670–6. doi: 10.1001/archopht.1989.01070010688028. [DOI] [PubMed] [Google Scholar]
- 28.Mishra VK, Retherford R, Smith KR. Biomass cooking fuels and prevalence of blindness in Indian. J Environ Med. 1999;1:189–99. doi: 10.1016/s1201-9712(99)90032-2. [DOI] [PubMed] [Google Scholar]
- 29.Saha A, Kulkarni PK, Shah A, Patel M, Saiyed HN. Ocular morbidity and fuel use: An experience from India. Occup Environ Med. 2005;62:66–9. doi: 10.1136/oem.2004.015636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Behera D, Dash S, Malik SK. Blood carboxyhaemoglobin levels following acute exposure to smoke of biomass fuels. Indian J Med Res. 1998;88:522–4. [PubMed] [Google Scholar]
- 31.Mavlankar DV, Trivedi CR, Gray RH. Levels and risk factors for perinatal mortality in Ahmedabad, India. Bull World Health Organ. 1991;69:435–42. [PMC free article] [PubMed] [Google Scholar]
- 32.Tielsch JM, Katz J, Thulasiraj RD, Coles CL, Sheeladevi S, Yanik EL, et al. Exposure to indoor biomass fuel and tobacco smoke and risk of adverse reproductive outcomes, mortality, respiratory morbidity and growth among newborn infants in south India. Int J Epidemiol. 2009;38:1351–63. doi: 10.1093/ije/dyp286. [DOI] [PubMed] [Google Scholar]
- 33.Sreeramareddy CT, Shidhaye RR, Sathiakumar N. Association between biomass fuel use and maternal report of child size at birth – an analysis of 2005-06 India Demographic Health Survey data. BMC Public Health. 2011;11:403. doi: 10.1186/1471-2458-11-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Global Alliance for Clean Cookstoves. [Last accessed on 2013 Apr 11]. Available from: http://www.cleancookstoves.org/resources/reports-andresearch/?country=IN .
- 35.National Biomass Cookstoves Programme (NBCP) Ministry of New and Renewable Energy. [Last accessed on 2013 Apr 11]. Available from: http://mnre.gov.in/schemes/decentralizedsystems/national-biomass-cookstovesinitiative/


