Abstract
Introduction:
Although there is sufficient evidence that HMG CoA Reductase Inhibitors reduce stroke recurrence in patients with or ischemic heart disease, it remains unclear whether they also improve outcomes given before or after stroke onset and whether such an effect is more robust with pre-stroke or post-stroke use of statins.
Materials and Methods:
We carried out a retrospective analysis of a large University Health Consortium Database. Patients with statin use before or after stroke onset were included in the analysis. Twenty patients discontinued statins after stroke onset. The outcome measures were discharge home or long-term care facility and/or death within 45 days.
Results:
Patients with prior statin use were more likely to be discharged home (1.67, CI 1.12-2.49), as were post stroke statin patients who had a more robust effect OR 2.63, CI 1.61-4.53).
Conclusions:
Patients started on statins after stroke were more likely to be discharged home versus patients already on statins before stroke onset. However, both groups were also more likely to be discharged home than those patients not on statins.
Keywords: HMG CoA reductase inhibitors, ischemic stroke, outcome
Introduction
HMG CoA reductase inhibitors, commonly known as statins, are widely used lipid lowering agents. In addition to their effect on cholesterol levels statins appear to have additional independent effects such as antithrombotic and neuroprotective properties.(1,2,3) The beneficial effect of statins on stroke prevention have been well-documented in both patients at risk for cardiac events as well as in patient without prior-known coronary disease.(4) However, the effect of statins on acute stroke outcome have not been extensively studied. Limited observational studies suggest that pretreatment with statin improves functional outcome after ischemic stroke as measured by Modified Rankin Scale (mRS) and Barthel Index (BI).(5,6) Furthermore, pre-stroke statin use has been associated with improved survival following ischemic stoke.(7,8) Whether post-stroke treatment with statins is associated with improved outcome is unknown. In the present study we investigated whether the timing of statin use, prior to or following stroke onset, affected outcome after ischemic stroke as compared to no statin use as measured by the odds of discharge home versus need for long-term care (LTC) or death within 45 days.
Materials and Methods
A large nationwide database of stroke patients, the University Health Consortium (UHC) database 2003-2007 was used to identify patients retrospectively. Inclusion criteria were age >18 years and diagnosis of acute ischemic stroke. Patients who received thrombolytic treatment were included as thrombolytic use as one of the variables included in our analysis.
Demographic characteristics for each patient were recorded including age, gender, as well as information on prior use of antihypertensives, antiplatelet agents, and pre-admission statin use. Stroke risk factors were also recorded including presence of hypertension, diabetes, atrial fibrillation, previous transient ischemic attack (TIA) or ischemic stroke, and hyperlipidemia. Initial stroke severity was reported using the National Institutes of Health stroke scale (NIHSS). We stratified patients into those on statins before stroke onset versus started on statins after stroke onset (within 48 hours of admission) and compared these with those patients that had never been exposed to statins. Favorable outcome was defined as discharge home while unfavorable outcome was considered discharge to LTC or death within 45 days.
Statistical analysis
The dataset was analyzed using a univariate and multivariate analyses. χ2 test was utilized for all variables except continuous variables such age or initial mean arterial pressure (MAP), for which t test was performed. The following factors were included age, gender, stroke severity, vascular risk factors, medications including statins, angiotensin converting enzyme inhibitors and antiplatelet agents. Since initial stroke severity can influence these results, we included stroke severity as one of the variables in the analysis. Significant univariate predictors, P < 0.05, were included in the final multivariate step-wise binary logistic regression analysis.
Results
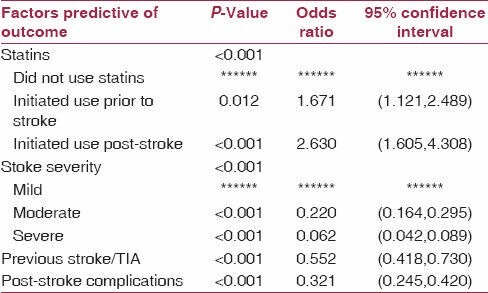
Baseline characteristics including age, gender, presence of hypertension, etc., are shown in Table 1. Stroke severity for the entire population is shown in Table 2. Two-hundred and thirty-two patients were on statins prior-to-stroke onset, 188 were initiated on statin post-stroke while 1198 patients did not take statins at any time. Univariate analysis yielded eight factors associated with significant outcomes [Table 3]. These included gender (P = 0.025), history of hyperlipidemia (P = 0.004), previous stroke or TIA (P < 0.001), post-stroke complications (P < 0.001), age (P = 0.02), initial MAP (P = 0.019) statin use, pre or post-stroke (P < 0.001), and stroke severity (P < 0.001). Final multivariate logistic regression analysis showed that both pre- and post-stroke stain used were significantly associated with discharge home. Pre-stroke statin use was associated with a 1.67 times greater chance of being discharged home compared to patients who were not treated with statins at any time. This outcome was maintained in patients initiated on statin therapy after stroke onset. Post-stroke statin use was in fact associated with a higher likelihood of discharge home, 2.63 times probability compared to untreated patients. Predictors of a less favorable outcome included stroke severity, previous stroke or TIA, and post-stroke complications. Moderate and severe stroke had a 4.55 and 16.13 probability, of discharge to LTC or death respectively. Previous stroke or TIA had a 1.81 and post-stroke complication a 3.12 probability of poor outcome [Tables 3 and 4].
Table 1.
Demographics
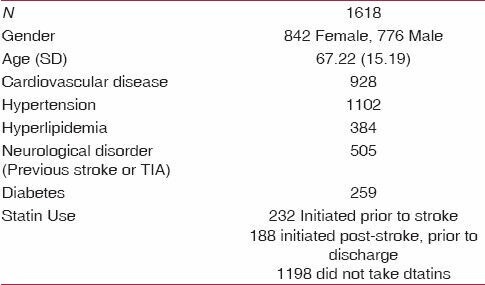
Table 2.
Stroke features
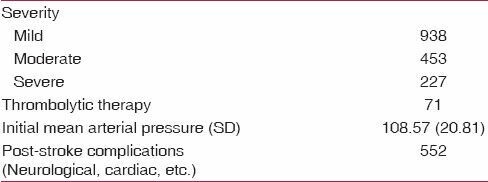
Table 3.
Univariate analysis of demographics and risk factors
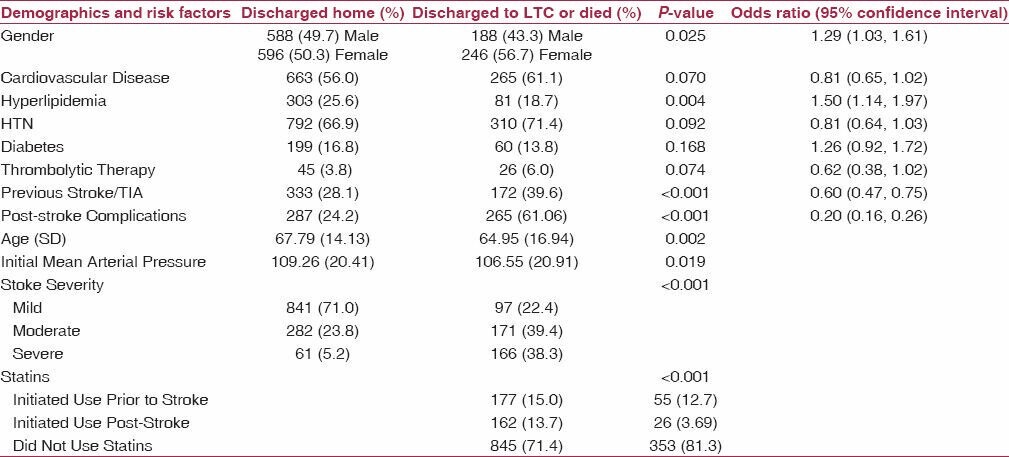
Table 4.
Multivariate analysis to determine the factors predictive of outcome
Discussion
The results of our analysis suggest that both pre- and post-stroke statin use are associated with a more favorable outcome, defined as likelihood of discharge home versus long-term care, after acute ischemic stroke. Pre-stroke statin use was associated with a 1.67 times greater chance of being discharged home compared to patients who were not treated with statins at any time. This benefit was also seen with post-stroke statin use, which was associated with 2.63 times greater probability of discharge home compared to untreated patients.
Our results are in agreement with previous observational studies that have shown improvement in both functional outcome and mortality in stroke patients pretreated with statins. Marti-Fabregas' et al. found improved functional outcome, defined as Barthel Index greater than 95, at 3 months in patients using statins at time of ischemic stroke onset.(5) Elkind et al. similarly found a lower ninety day mortality in patients taking lipid lowering agents in a large population based study in northern Manhattan.(7)
In agreement with more recent studies using databases and population-based interventions(9,10) the present study also included patients in whom statins were initiated within 48 hours of the onset of stroke. The benefits of statins were not only maintained in this group, the effect was more robust than that seen in the pre-stroke statin use group. Similar results were seen in a previous observational study showing favorable outcome (mRS less than or equal to 2) at 12 weeks in patients treated with statins after stroke onset.(11) A trend toward improved outcome in patients treated with statins at admission was also seen in the observational study alluded to earlier by Marti-Fabregas et al.(5) However, that study had only a small number of patients; 19 that began statins after stroke onset and the study was not designed to explore this question.(9,10)
Possible explanations for the immediate benefits may be related to enhancement of endothelial nitric oxide synthesis. Endothelial nitric oxide inhibits platelet aggregation and leukocyte activation and regulates region blood flow and blood pressure. These effects may result in reduced infarct volume, which may translate into favorable outcome.(12) Statins have also been shown to reduce severity of acute stroke which again may translate into increased likelihood of discharge to home.(13) Improved outcome may also be related to enhancement of collateralization. This mechanism has been demonstrated angiographically in patients treated with stains.(14)
Mechanisms of delayed benefit may include effects of statins on promoting angiogenesis, synaptogenesis, and neurogenesis when initiated after stroke onset. This mechanism has been demonstrated in animal models where statins have been shown to induce endothelial vascular growth factor and cerebral cGMP which promote angiogenesis and neurogenesis when started 1 day after stroke onset.(15) It is also possible that the pre-stroke-treated patients exhibited a saturation effect on these potential enhancers of post-stroke recovery. Our study did not account for patients in whom statins were stopped at hospital admission and this may have confounded the results.
The present study has several strengths. It included a diverse patient population from a nationwide database. By using discharge to home as our primary outcome measure we were able to assess the potential short-term benefits of statins in acute stroke. In contrast, previous studies have mainly looked at potential long-term benefits of statin use such as secondary prevention of stroke and long-term functional outcome.(4,5,16,17,18,19)
This study is limited by its retrospective design. As mentioned previously, there was some data that was not available to us for review such as percentage of patients on statins prior to stroke onset in which statins were held at admission and this may have confounded our results. In addition we did not have data on stroke subtype available to us including cardioembolic, lacunar, or atherosclerotic. It is possible that patients with presumed stroke of atherosclerotic origin may have benefited more from statins as they have been shown to have effects on plaque stabilization.
In conclusion, we have found that both pre-stroke and post-stroke statin use in the may be associated with improved outcome after acute ischemic stroke. Post-stroke statin use seems to have a more robust effect on outcome. These findings may have treatment implications. However, further studies including prospective studies are required to confirm these findings before treatment recommendations can be made.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Gertz K, Laufs U, Lindauer U, Nickenig G, Bohm M, Dirnagl U, et al. Withdrawal of statin treatment abrogates stroke protection in mice. Stroke. 2003;34:551–7. doi: 10.1161/01.str.0000054055.28435.bf. [DOI] [PubMed] [Google Scholar]
- 2.Koh KK. Effects of statins on vascular wall: vasomotor function, inflammation, and plaque stability. Cardiovasc Res. 2000;47:648–57. doi: 10.1016/s0008-6363(00)00146-2. [DOI] [PubMed] [Google Scholar]
- 3.Vaughan CJ. Prevention of stroke and dementia with statins: Effects beyond lipid lowering. Am J Cardiol. 2003;91:23B–9B. doi: 10.1016/s0002-9149(02)03270-8. [DOI] [PubMed] [Google Scholar]
- 4.Amarenco P, Bogousslavsky J, Callahan A, 3rd, Goldstein LB, Hennerici M, Rudolph AE, et al. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355:549–59. doi: 10.1056/NEJMoa061894. [DOI] [PubMed] [Google Scholar]
- 5.Marti-Fabregas J, Gomis M, Arboix A, Aleu A, Pagonabarraga J, Belvis R, et al. Favorable outcome of ischemic stroke in patients pretreated with statins. Stroke. 2004;35:1117–21. doi: 10.1161/01.STR.0000125863.93921.3f. [DOI] [PubMed] [Google Scholar]
- 6.Yoon SS, Dambrosia J, Chalela J, Ezzeddine M, Warach S, Haymore J, et al. Rising statin use and effect on ischemic stroke outcome. BMC Med. 2004;2:4. doi: 10.1186/1741-7015-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elkind MS, Flint AC, Sciacca RR, Sacco RL. Lipid-lowering agent use at ischemic stroke onset is associated with decreased mortality. Neurology. 2005;65:253–8. doi: 10.1212/01.wnl.0000171746.63844.6a. [DOI] [PubMed] [Google Scholar]
- 8.Aslanyan S, Weir CJ, McInnes GT, Reid JL, Walters MR, Lees KR. Statin administration prior to ischaemic stroke onset and survival: Exploratory evidence from matched treatment-control study. Eur J Neurol. 2005;12:493–8. doi: 10.1111/j.1468-1331.2005.01049.x. [DOI] [PubMed] [Google Scholar]
- 9.Ni Chroinin D, Callaly EL, Duggan J, Merwick A, Hannon N, Sheehan O, et al. Association between acute statin therapy, survival, and improved functional outcome after ischemic stroke: the North Dublin Population Stroke Study. Stroke. 2011;42:1021–9. doi: 10.1161/STROKEAHA.110.596734. [DOI] [PubMed] [Google Scholar]
- 10.Flint AC, Kamel H, Navi BB, Rao VA, Faigeles BS, Conell C, et al. Statin use during ischemic stroke hospitalization is strongly associated with improved poststroke survival. Stroke. 2012;43:147–54. doi: 10.1161/STROKEAHA.111.627729. [DOI] [PubMed] [Google Scholar]
- 11.Moonis M, Kane K, Schwiderski U, Sandage BW, Fisher M. HMG-CoA reductase inhibitors improve acute ischemic stroke outcome. Stroke. 2005;36:1298–300. doi: 10.1161/01.STR.0000165920.67784.58. [DOI] [PubMed] [Google Scholar]
- 12.Laufs U, Gertz K, Dirnagl U, Bohm M, Nickenig G, Endres M. Rosuvastatin, a new HMG-CoA reductase inhibitor, upregulates endothelial nitric oxide synthase and protects from ischemic stroke in mice. Brain Res. 2002;942:23–30. doi: 10.1016/s0006-8993(02)02649-5. [DOI] [PubMed] [Google Scholar]
- 13.Greisenegger S, Mullner M, Tentschert S, Lang W, Lalouschek W. Effect of pretreatment with statins on the severity of acute ischemic cerebrovascular events. J Neurol Sci. 2004;221:5–10. doi: 10.1016/j.jns.2004.01.015. [DOI] [PubMed] [Google Scholar]
- 14.Ovbiagele B, Saver JL, Starkman S, Kim D, Ali LK, Jahan R, et al. Statin enhancement of collateralization in acute stroke. Neurology. 2007;68:2129–31. doi: 10.1212/01.wnl.0000264931.34941.f0. [DOI] [PubMed] [Google Scholar]
- 15.Chen J, Zhang ZG, Li Y, Wang Y, Wang L, Jiang H, et al. Statins induce angiogenesis, neurogenesis, and synaptogenesis after stroke. Ann Neurol. 2003;53:743–51. doi: 10.1002/ana.10555. [DOI] [PubMed] [Google Scholar]
- 16.Pedersen TR, Kjekshus J, Pyorala K, Olsson AG, Cook TJ, Musliner TA, et al. Effect of simvastatin on ischemic signs and symptoms in the Scandinavian simvastatin survival study (4S) Am J Cardiol. 1998;81:333–5. doi: 10.1016/s0002-9149(97)00904-1. [DOI] [PubMed] [Google Scholar]
- 17.Plehn JF, Davis BR, Sacks FM, Rouleau JL, Pfeffer MA, Bernstein V, et al. Reduction of stroke incidence after myocardial infarction with pravastatin: the Cholesterol and Recurrent Events (CARE) study. The Care Investigators. Circulation. 1999;99:216–23. doi: 10.1161/01.cir.99.2.216. [DOI] [PubMed] [Google Scholar]
- 18.MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebocontrolled trial. Lancet. 2002;360:7–22. doi: 10.1016/S0140-6736(02)09327-3. [DOI] [PubMed] [Google Scholar]
- 19.Waters DD, Schwartz GG, Olsson AG, Zeiher A, Oliver MF, Ganz P, et al. Effects of atorvastatin on stroke in patients with unstable angina or non-Q-wave myocardial infarction: a Myocardial Ischemia Reduction with Aggressive Cholesterol Lowering (MIRACL) substudy. Circulation. 2002;106:1690–5. doi: 10.1161/01.cir.0000031568.40630.1c. [DOI] [PubMed] [Google Scholar]


