Abstract
Objectives:
Low birth weight (LBW; <2500 g), which is often associated with preterm birth, is a common problem in India. Both are recognized risk factors for neonatal mortality. Kangaroo mother care (KMC) is a non-conventional, low-cost method for newborn care based upon intimate skin-to-skin contact between mother and baby. Our objective was to assess physiological state of LBW babies before and after KMC in a teaching hospital setting.
Materials and Methods:
Study cohort comprised in-born LBW babies and their mothers - 300 mother-baby pairs were selected through purposive sampling. Initially, KMC was started for 1 hour duration (at a stretch) on first day and then increased by 1 hour each day for next 2 days. Axillary temperature, respiration rate (RR/ min), heart rate (HR/ min), and oxygen saturation (SpO2) were assessed for 3 consecutive days, immediately before and after KMC.
Results:
Data from 265 mother-baby pairs were analyzed. Improvements occurred in all 4 recorded physiological parameters during the KMC sessions. Mean temperature rose by about 0.4°C, RR by 3 per minute, HR by 5 bpm, and SpO2 by 5% following KMC sessions. Although modest, these changes were statistically significant on all 3 days. Individual abnormalities (e.g. hypothermia, bradycardia, tachycardia, low SpO2) were often corrected during the KMC sessions.
Conclusions:
Babies receiving KMC showed modest but statistically significant improvement in vital physiological parameters on all 3 days. Thus, without using special equipment, the KMC strategy can offer improved care to LBW babies. These findings support wider implementation of this strategy.
Keywords: India, kangaroo mother care, low birth weight, newborn, physiological parameter, preterm
Introduction
Low birth weight (LBW; <2500 g regardless of gestational age), which is often associated with preterm birth, is an important predictor of infant death within 28 days of birth.(1) It is estimated that globally, out of 139 million live births, more than 20 million LBW babies are born each year-over 95% of them in developing countries, mainly of South Asia and sub-Saharan Africa.(2) It is also estimated that, in developing countries, LBW infants are approximately 13 times more likely to die than normal birth weight counterparts.(3) Medical cost is also significantly higher in caring for preterm and other LBW babies. LBW occurs in about 20-30% of all live births in India.(4)
A major problem with such babies is their inability to control body temperature – a preventable cause of their morbidity and mortality. A World Health Organization (WHO) supported study in Nepal showed that hypothermia was common in newborn infants soon after birth; increased mortality was noted across all grades of hypothermia, and the risk was 12 times higher among preterm babies.(5) A study from India(6) revealed that 2.9% intramural babies and 45% babies born at home developed mild to moderate hypothermia.
Kangaroo mother care (KMC) implies placing the newborn baby in intimate skin-to-skin contact with the mother's chest and abdomen coupled with frequent and preferably exclusive breast-feeding. This is similar to marsupial care-giving, where the premature baby is kept warm in the maternal pouch and close to the breasts for unlimited feeding. KMC has emerged as a non-conventional low cost method for newborn care that provides warmth, touch, and security to the newborn and is believed to confer significant survival benefit. An updated Cochrane review has reported that KMC benefits breastfeeding outcomes and cardio-respiratory stability in infants without negative effects.(7)
Indian data on outcome of KMC are limited, though it has been found to be an effective and feasible method of care of LBW babies in hospital setting.(8) With this background, the objective of our study was to assess the physiological state of LBW babies during KMC in a teaching hospital setting. The broader intention is to generate data to recommend wider implementation of the strategy.
Materials and Methods
The study design was quasi-experimental with subjects serving as their own control. The study cohort comprised LBW babies born at Institute of Postgraduate Medical Education & Research (IPGME&R), Kolkata and its associated SSKM Hospital, and mothers of these babies. This is a tertiary care teaching hospital with level III neonatal intensive care unit (NICU) facility. The study protocol was approved by the institutional ethics committee, and formal written informed consent of willing mothers was obtained. Babies with sick mothers or gross congenital malformations were not included.
At first, the mothers were counseled regarding breastfeeding and KMC and their benefits. Then, breastfeeding and KMC were demonstrated with the help of volunteer mothers. After motivation, formal written informed consent of willing mothers was obtained for participation in the study. Three hundred mother-baby pairs were selected through purposive sampling over a period of 3 years. Babies requiring NICU admission were also included provided they became hemodynamically stable.
For implementing KMC, mothers were asked to use any front open light dress. Babies were dressed with cap, socks, and nappy and no other garments. After placing into a custom-made KMC bag, the baby was placed upright inside mother's clothing against bare skin of the chest and abdomen. Head was turned to one side and placed in a slightly extended position and eye to eye contact between mother and baby was encouraged. The hips were kept flexed and abducted in a ′frog′ position; the arms were also flexed. The baby was allowed to suck on the breast as often as it wanted. On the first day, KMC was provided for 1 hour at a time, second day 2 hours, third day 3 hours, and subsequently, the at-a-stretch duration was increased to as long as the mother felt comfortable. Counseling and demonstration were repeated for initially hesitant mothers till they were able to offer KMC confidently and correctly. Mothers who failed to execute KMC correctly despite repeated demonstrations were withdrawn from the study, although they were made conversant with the KMC technique ultimately.
Four vital physiological parameters of the baby, namely temperature, respiration rate, heart rate, and oxygen saturation, were assessed immediately before and after KMC for 3 consecutive days. Axillary temperature was measured (in °C) by digital thermometer. Respiration rate was assessed by observing chest movements for full one minute. Heart rate and oxygen saturation were recorded with the help of pulse-oximeter.
Statistical analysis
Data have been summarized by mean and standard deviation; 95% confidence interval (CI) values have been stated where deemed relevant. All 4 physiological variables were normally distributed. Boxplots have been used to depict the range of values encountered for individual parameters. Mean values before and after KMC were compared (two-tailed analysis) by Students' paired t test; P < 0.05 has been considered statistically significant. Statistica version 6 (Tulsa, Oklahoma: StatSoft Inc., 2001) software was used for analysis.
Results
Complete data was available for 265 cases out of the 300 mother-baby pairs recruited. Data from those 35 cases where the mother could not implement KMC correctly or for the scheduled duration on all 3 days were not included. The age of the mothers was 25.7 ± 5.19 years (mean ± standard deviation). The gestational age of the babies at birth was 33.2 ± 3.30 weeks and birth weight was 1450.9 ± 311.19 g. Table 1 depicts the physiological variables on the 3 successive days and [Table 2] summarizes the changes with their 95% CI and statistical significance. There were no deaths in these babies.
Table 1.
Range of values for the four physiological parameters recorded in the study
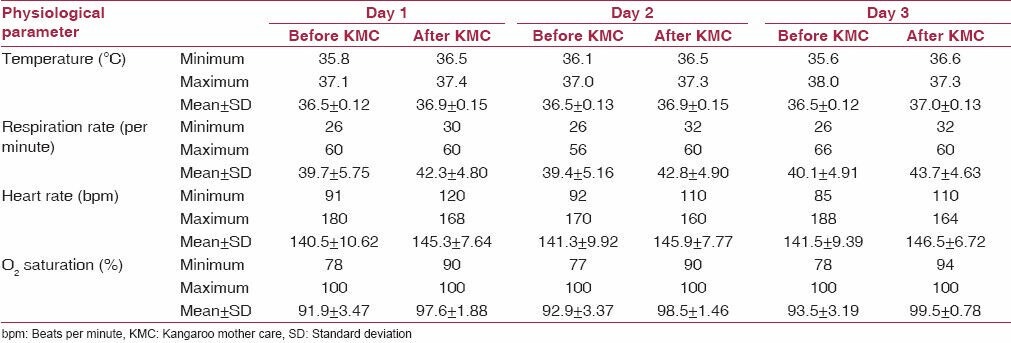
Table 2.
Changes in physiological parameters before and after KMC in the study cohort
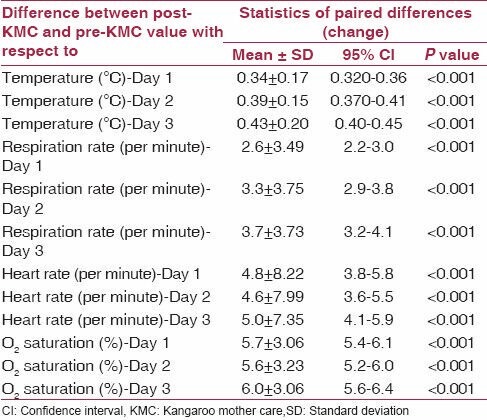
Temperature showed a small rise during KMC, and the changes were statistically significant on all 3 days. During initiation of the KMC session, some babies had mild hypothermia. During KMC, most babies showed steady rise in temperature and none developed hypothermia.
No baby had respiratory distress at baseline. The mean change in respiration rate during KMC was 2.6 ± 3.49 (P < 0.001) on day 1, 3.3 ± 3.75 (P < 0.001) on day 2, and 3.7 ± 3.73 (P < 0.001) on day 3. During KMC sessions, the babies showed regular respiration and often fell asleep. No baby developed apnea during KMC. From the standard deviation figures in Table 2, it is evident that the variability in respiration rate was also brought down by KMC.
Heart rate showed a rise during KMC, and the mean changes were modest but statistically significant on all 3 days - 4.8 ± 8.22 on day 1 (P < 0.001), 4.6 ± 7.99 on day 2 (P < 0.001), and 5 ± 7.35 on day 3 (P < 0.001). Few babies had bradycardia (< 100 bpm) at baseline - 2 babies on day 1, and 1 each on day 2 and 3 - but during KMC session, all babies achieved normal (between 100-170 bpm) and stable heart rates.
Mean oxygen saturation also improved by about 5% on all 3 days, the change being statistically significant along with distinct reduction in the dispersion of this parameter. Below 90% saturation at start of the KMC session was present in 64, 47, and 32 babies respectively on the 3 days, but all recovered following the session. Even babies on oxygen had their oxygen requirement reduced within 15 minutes of starting KMC.
Figures 1 and 2 depict the range of values encountered for body temperature and oxygen saturation in the study cohort over the 3 successive study days.
Figure 1.
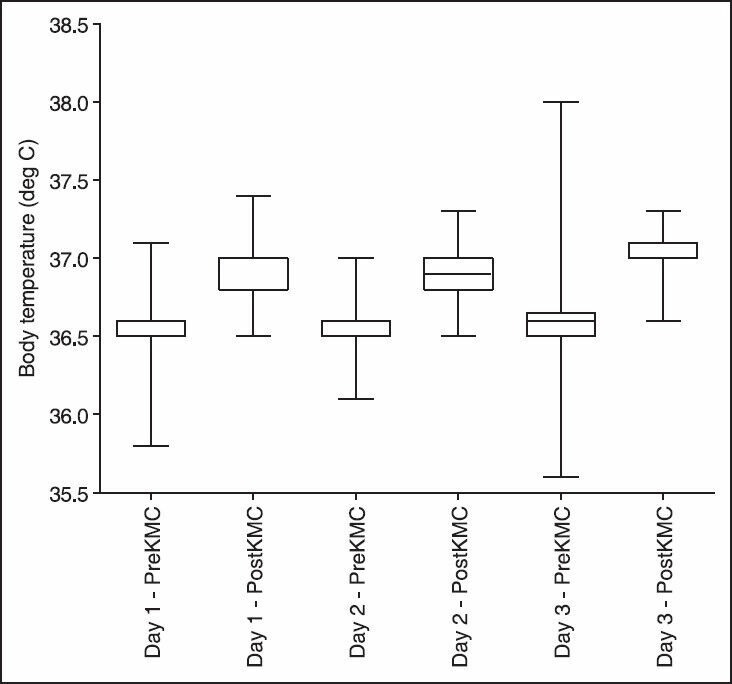
Temperature changes induced by kangaroo mother care sessions on the three successive study days
Figure 2.
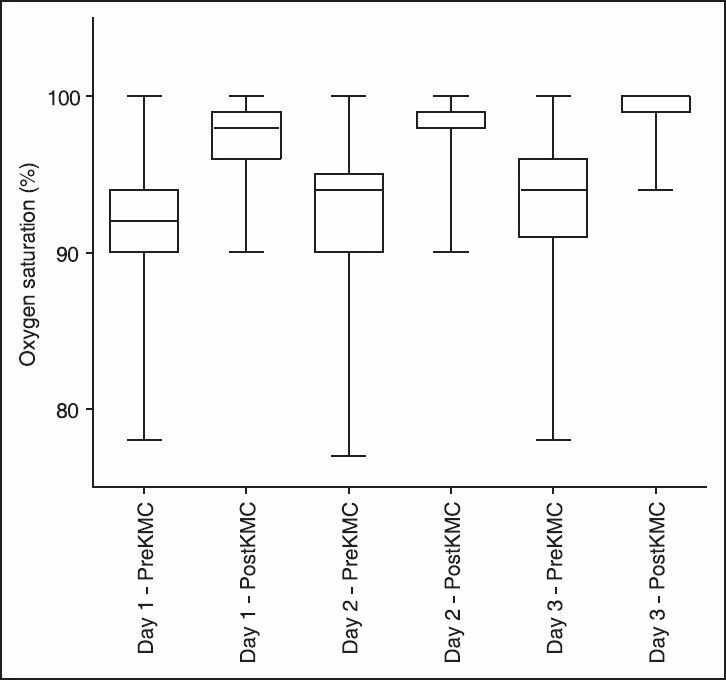
Changes in O2 saturation brought about by kangaroo mother care sessions on the three successive study days
Overall, it can be said that babies receiving KMC showed statistically significant improvement in all the 4 vital physiological parameters, of which the extent of rise in respiration rate and oxygen saturation were also clinically significant. This was seen on all 3 days.
Discussion
KMC is a simple and low-cost intervention for the care of LBW infants. It enhances both infant and maternal well-being and can be practiced in any situation without needing special equipment (e.g. special cots, heaters, incubators). Although initially conceived for use in developing countries with limited resources, its use has expanded worldwide as caregivers, parents, and administrators become increasingly familiar with the physiological, psychological, and cost benefits associated with the practice.(9,10,11)
Our study results are broadly in agreement with earlier studies. Although not a marked rise, the smooth upward trend in temperature during KMC sessions should protect the newborn against temperature fluctuations and cold stress. Jothipriya J has reported that mean axillary temperature and mean heart rate were higher during KMC than during routine care.(12) If nothing else, KMC achieves the goal of ′keeping baby warm,′ which is one of the most cost-effective interventions to protect babies during the critical neonatal period.(13) Ludington-Hoe et al. have reported that kangaroo care promotes stability of physiological function.(14) In their study,(15) heart rate remained stable (mean 143.9), respiratory rate ranged from 20 to 72 (mean 41.2), and apnea episodes did not occur during KMC. After placing babies in KMC position, their temperature never fell below 36.8°C and remained at a mean of 37.1°C.
There was distinct improvement in oxygen saturation during the KMC sessions. This is relevant for sick newborns, particularly those requiring oxygen supports. Earlier studies also report decrease in apnea and improvement in oxygen saturation in mechanically ventilated babies able to tolerate transfer and position changes.(16,17)
A meta-analysis of 23 studies of 190 term and 326 preterm infants (gestational age 26 to 36 weeks) concluded that there was an increase in body temperature of 0.22°C, no change in heart rate, and a statistically but not clinically significant decrease in oxygen saturation of 0.60% during periods of skin-to-skin contact.(18) Prematurity did not affect the stability of these parameters. Our study found a similar rise of temperature, a small but statistically significant rise in heart rate, and a definite improvement in oxygen saturation. These improvements are unlikely to have been due to chance alone since similar improvements were noted on all 3 days, even with as little as 1 hour of kangaroo care on the first day.
The reasons for the beneficial effects of KMC are yet to be fully explored. Heat transfer from mother to baby is obvious. The intimate and early skin-to-skin contact between mother and baby, with repeated nutritive and non-nutritive suckling, possibly also evokes neuropsychological responses that program physiology and behavior. Further, during KMC, the infant experiences maternal heart sounds, rhythmic maternal breathing, warmth and prone positioning, all of which offer gentle stimulation across auditory, tactile, vestibular, and thermal sensory systems, which may in sum total have a tranquilizing effect on the baby, allowing physiological parameters to stabilize.(19)
This study had its share of limitations. It was observational in nature rather than a randomized controlled trial. Despite being motivated, several mothers failed to provide KMC correctly, even after repeated demonstrations, and their data had to be excluded. This emphasizes the need for perseverance for both mothers and nursing staff towards proper KMC technique.(20) The study was conducted in the postnatal ward and NICU setting where healthcare providers are strongly motivated and maintain close supervision. Similar close supervision may not be possible in general ward and domiciliary settings. Therefore, we cannot claim that improvement of physiological parameters, with its attendant clinical implications, would be obtainable in any setting. Indeed, implementation of KMC requires organized planning and effort, and lack of these are barriers towards extending the benefits to all babies in need of such care.(21,22)
Notwithstanding these limitations, it can be stated that low birth weight babies receiving KMC show modest but statistically significant rise in temperature, respiration rate, heart rate, and oxygen saturation through kangaroo care, without the need for any special equipment. This can help to avoid complications and the need for more elaborate interventions. There is a case for making KMC the standard of care for the LBW newborn in our setting. However, adequate planning and manpower would be needed to motivate and train mothers to undertake KMC and to monitor that they do so satisfactorily.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Born Too Soon: The global action report on preterm birth. Geneva: World Health Organization; 2012. March of Dimes, The Partnership for Maternal Newborn and Child-Health, Save the Children, World Health Organization. [Google Scholar]
- 2.Sachdev HP. Low birth weight in south Asia. Int J Diab Dev Countries. 2001;21:13–31. [Google Scholar]
- 3.Yasmin S, Osrin D, Paul E, Costello A. Neonatal mortality of low-birth-weight infants in Bangladesh. Bull World Health Organ. 2001;79:608–14. [PMC free article] [PubMed] [Google Scholar]
- 4.Bharati P, Pal M, Bandyopadhyay M, Bhakta A, Chakraborty S, Bharati P. Prevalence and causes of low birth weight in India. Malays J Nutr. 2011;17:301–13. [PubMed] [Google Scholar]
- 5.Mullany LC, Katz J, Khatry SK, LeClerq SC, Darmstadt GL, Tielsch JM. Risk of mortality associated with neonatal hypothermia in southern Nepal. Arch Pediatr Adolesc Med. 2010;164:650–6. doi: 10.1001/archpediatrics.2010.103. [DOI] [PubMed] [Google Scholar]
- 6.Kumar V, Shearer JC, Kumar A, Darmstadt GL. Neonatal hypothermia in low resource settings: A review. J Perinatol. 2009;29:401–12. doi: 10.1038/jp.2008.233. [DOI] [PubMed] [Google Scholar]
- 7.Moore ER, Anderson GC, Bergman N, Dowswell T. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. 2012;5:CD003519. doi: 10.1002/14651858.CD003519.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parmar VR, Kumar A, Kaur R, Parmar S, Kaur D, Basu S, et al. Experience with kangaroo mother care in a neonatal intensive care unit (NICU) in Chandigarh, India. Indian J Pediatr. 2009;76:25–8. doi: 10.1007/s12098-009-0024-2. [DOI] [PubMed] [Google Scholar]
- 9.Thukral A, Chawla D, Agarwal R, Deorari AK, Paul VK. Kangaroo mother care - an alternative to conventional care. Indian J Pediatr. 2008;75:497–503. doi: 10.1007/s12098-008-0077-7. [DOI] [PubMed] [Google Scholar]
- 10.Hendricks-Muñoz KD, Li Y, Kim YS, Prendergast CC, Mayers R, Louie M. Maternal and neonatal nurse perceived value of kangaroo mother care and maternal care partnership in the neonatal intensive care unit. Am J Perinatol. 2013;30:875–80. doi: 10.1055/s-0033-1333675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pallás-Alonso CR, Losacco V, Maraschini A, Greisen G, Pierrat V, Warren I, et al. European Science Foundation Network. Parental involvement and kangaroo care in European neonatal intensive care units: A policy survey in eight countries. Pediatr Crit Care Med. 2012;13:568–77. doi: 10.1097/PCC.0b013e3182417959. [DOI] [PubMed] [Google Scholar]
- 12.Priya JJ. Kangaroo care for low birth weight babies. Nurs J India. 2004;95:209–12. [PubMed] [Google Scholar]
- 13.Singh A, Yadav A, Singh A. Utilization of postnatal care for newborns and its association with neonatal mortality in India: An analytical appraisal. BMC Pregnancy Childbirth. 2012;12:33. doi: 10.1186/1471-2393-12-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ludington-Hoe SM. Evidence-based review of physiologic effects of kangaroo care. Curr Womens Health Rev. 2011;7:243–53. [Google Scholar]
- 15.Ludington-Hoe SM, Anderson GC, Simpson S, Hollingsead A, Argote LA, Rey H. Birth related fatigue in 34-36-week preterm neonates: Rapid recovery with very early kangaroo (skin-to-skin) care. J Obstet Gynecol Neonatal Nurs. 1999;28:94–102. doi: 10.1111/j.1552-6909.1999.tb01970.x. [DOI] [PubMed] [Google Scholar]
- 16.Cleary GM, Spinner SS, Gibson E, Greenspan JS. Skin-to-skin parental contact with fragile preterm infants. J Am Osteopath Assoc. 1997;97:457–460. doi: 10.7556/jaoa.1997.97.8.457. [DOI] [PubMed] [Google Scholar]
- 17.Hunt F. The importance of kangaroo care on infant oxygen saturation levels and bonding. J Neonatal Nurs. 2008;14:47–51. [Google Scholar]
- 18.Mori R, Khanna R, Pledge D, Nakayama T. Meta-analysis of physiological effects of skin-to-skin contact for newborns and mothers. Pediatr Int. 2010;52:161–70. doi: 10.1111/j.1442-200X.2009.02909.x. [DOI] [PubMed] [Google Scholar]
- 19.Jefferies AL. Canadian Paediatric Society, Fetus and Newborn Committee. Kangaroo care for the preterm infant and family. Paediatr Child Health. 2012;17:141–6. doi: 10.1093/pch/17.3.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blomqvist YT, Frölund L, Rubertsson C, Nyqvist KH. Provision of kangaroo mother care: Supportive factors and barriers perceived by parents. Scand J Caring Sci. 2013;27:345–53. doi: 10.1111/j.1471-6712.2012.01040.x. [DOI] [PubMed] [Google Scholar]
- 21.Bergh AM, Rogers-Bloch Q, Pratomo H, Uhudiyah U, Sidi IP, Rustina Y, et al. Progress in the implementation of kangaroo mother care in 10 hospitals in Indonesia. J Trop Pediatr. 2012;58:402–5. doi: 10.1093/tropej/fmr114. [DOI] [PubMed] [Google Scholar]
- 22.Maulik PK, Darmstadt GL. Community-based interventions to optimize early childhood development in low resource settings. J Perinatol. 2009;29:531–42. doi: 10.1038/jp.2009.42. [DOI] [PubMed] [Google Scholar]


