Abstract
To investigate the prevalence, correlates, attitude and treatment seeking behavior of erectile dysfunction (ED) in type 2 diabetes mellitus (T2DM) patients in the primary care setting, a multi-center cross-sectional survey using a structured anonymous self-administered questionnaire was performed in 10 general outpatient clinics. Of the 603 subjects (91% response rate), the prevalence of ED men, as defined by the International Index of Erectile Function, was 79.1%. Most subjects had mild ED (28.9%), followed by mild-to-moderate ED (27.9%), then moderate ED (13.4%) and severe ED (9%). Nearly 55% of those with ED did not consider themselves as having ED. Less than 10% of them had ever sought medical treatment, although 76.1% of them wished to receive management from doctor(s) should they be diagnosed with ED. They considered the most important management from doctors to be clinical assessment (41.7%), followed by management of potential underlying cause (37.8%), referral to specialist (27.5%), education (23.9%), prescription of phosphodiesterase type 5 inhibitors (16.9%) and referral to counseling service (6.7%). The prevalence of ED was strongly associated with subjects who thought they had ED (odds ratio (OR) = 90.49 (20.00–409.48, P< 0.001)) and were from the older age group (OR = 1.043 (1.011–1.076, P = 0.008)). In conclusion, ED is highly prevalent among T2DM men. The majority of them wanted management from doctors should they have ED, but only a minority would actually voice out the request. Screening of ED among T2DM men using structural questionnaire allowed the diagnosis of more than half of the ED cases, which otherwise would have gone undiagnosed.
Keywords: diabetes mellitus, erectile dysfunction, prevalence, risk factors
INTRODUCTION
Type 2 diabetes mellitus (T2DM) is common among the Chinese population. The prevalence of total diabetes (all types) in China is estimated to be 9.7%.1 In the Hong Kong Special Administrative Region (S.A.R.) alone, more than 160 000 T2DM patients were seen in public general outpatient clinics (GOPCs) in 2009, making it the second most common chronic illness.2 Erectile dysfunction (ED) is known to have a higher occurrence in T2DM patients when compared with the general population, yet this condition is often under-recognized. The prevalence of ED among T2DM patients is reported to be 75.2% in Beijing, China,3,4 63.6%–84.3% in Hong Kong5,6 and 83.9% in Taiwan, China,7 when compared to the general reported prevalence of 6.3%–25% in all men, with a higher rate of about 20%–45% in the older age group.8,9,10 ED in T2DM patients may be caused by vascular, neurogenic and/or endothelial dysfunction, oxidative processes and change in the nitric-oxide system.11 Not only is ED associated with increased cardiovascular risks;12 but it also has a negative impact on psychological well-being and leads to marital disharmony and impaired quality of life.13,14
Numerous researches revealed that men with ED find it difficult to report their conditions to doctors,15,16 although all men from a cross-national survey agreed that ED was a source of great dismal for themselves and their partners, and nearly all disagreed that they were too old for sex.17 To begin with, more than half of those who were screened ED positive did not in fact think that they had ED.18 For those who considered themselves having the condition, less than half sought treatment.19 T2DM men are generally reluctant to discuss the subject of ED with their doctors.20 Doctors also identified multiple barriers to managing ED in their practice,21,22 and it is uncommon for healthcare professionals to enquire about ED in diabetes mellitus (DM) clinics.23 Other known factors influencing ED treatment seeking behavior include severity of ED,24 level of bother,25 supportiveness of partner,26 and an increased awareness of the condition.27
Given that ED is a common, important yet difficult to diagnosis condition, especially among T2DM patients, different screening tools are available.28,29,30 Since 2003, Hong Kong has adopted recommendations from the American Diabetes Association31 and the National Institute for Health and Clinical Excellence.32 All public GOPCs arrange annual complication screening clinic for T2DM patients. For pragmatic consideration, nurses will pose a clinically validated “Yes–No” question33 to every T2DM man to screen for ED. GOPC doctors from these study centers suspected the validity of the single self-reported question on ED because of the observed higher occurrence of ED by doctors’ clinical assessment. This study aimed primarily at finding out the prevalence of ED by the use of structural questionnaires. We also aimed to verify if the answers for the single self-reported question on ED in our usual practice was indeed indicative of the true prevalence. Lastly, we aimed to find out the factors that correlated with T2DM patients’ attitude toward ED and their expectation for ED management in the primary care setting.
METHODS
The project protocol, questionnaire and information to patient for consent were approved by the Research Ethics Committee of the Kowloon West Cluster, Hospital Authority of Hong Kong. This was a multi-center cross-sectional survey on T2DM men consecutively attending 10 primary care GOPCs in urban areas of Hong Kong S.A.R. using self-administered anonymous structured questionnaires.
Questionnaire
The first part of the questionnaire was designed to assess the prevalence of ED. We adopted the Chinese version of the 5-item version of the International Index of Erectile Function (IIEF-5).28 IIEF-5 is well acknowledged as one of the best screening tools and has been used widely in other studies.4,12 We also included the single self-reported question “Do you think you have ED?”.33 The second part of the questionnaire asked for information about the subjects’ age and marital status. Questions assessing treatment seeking behavior, and attitudes and concerns pertaining to ED were formulated based on the results of a qualitative structural interview of 1122 men with ED.34 The questions were first drafted in English, translated into Chinese by authors WHL and SNF, and then back-translated into English by another team doctor PS Lau. Discrepancies between the original and the back-translated English versions were discussed among authors and amended accordingly. A pilot study was conducted with 20 T2DM men. Feedbacks on the questionnaire (including font, font size, spacing, highlights, clarity, user-friendliness, attractiveness) were collected by individual face-to-face interviews. Revision was then made on the list of questions, wordings and length of the questionnaire.
Inclusion and exclusion criteria
All T2DM men, aged 18 and above, who were receiving treatment at the 10 GOPCs from March to May 2012 were invited to participate in the study. Their DM diagnosis was previously documented by doctors using the diagnostic criteria of the World Health Organization and the International Diabetes Federation Joint Consultation 2005.35 We excluded patients who were unable to understand Chinese sufficiently well, or had insufficient (corrected) vision to complete the questionnaires. Those with known secondary ED from genetic, endocrinological, neurological or surgical causes were also excluded from the study.
Survey process
Eligible T2DM patients were invited to complete the self-administered questionnaire in the waiting hall. All questionnaires were marked by chronological numbers to check for missing or no return cases. The number of patients approached, reason for exclusion, the number of refusals, and the number of questionnaires distributed and returned were recorded.
Data entry was done by the authors and designated research assistants using the same set of codes. Double entry was performed for each set of data by two different research assistants. Between-record checks and within-record checks were conducted to enhance accuracy and validity of data. All inconsistencies and out-of-range errors were individually verified against the original questionnaires by the author WHL.
Sample size
Based on the 65% ED prevalence found in an earlier local study,5 our sample size was calculated to ensure an error rate within 5% by a 95% confidence interval. Without accounting for the design effect due to clustering sampling by clinic, we needed to recruit 370 subjects. The median estimate of intra-class correlation was 0.01.36 Taking into account the homogeneity of patients attending the GOPCs, 60 subjects were required per clinic for 10 GOPCs, giving a total of 600 subjects.37
Statistical methods
Data collected was analyzed using the SPSS Windows 20.0 program (SPSS Inc., Chicago, IL, USA). Prevalence and severity of ED were reported according to the IIEF-5 score. Subjects’ attitudes and concerns pertaining to ED and treatment seeking behavior were presented as frequencies and percentages, stratified by severity of ED. Continuous IIEF-5 score and age were presented as mean and standard deviation, while the Kruskal-Wallis analysis of variance (ANOVA) test was used to assess the differences in age between severities of ED. Logistic regression models were performed to investigate the associations between age, marital status, subjects’ attitudes and concerns pertaining to ED and treatment seeking behavior. Association of each factor with the presence of ED was given by the respective odds ratio (OR).
RESULTS
Out of the 915 subjects approached, 191 were excluded (189 were unable to comprehend the self-administered questionnaire; two had known secondary ED from other underlying causes). Of the 724 subjects recruited, 10 did not wish to participate in the study and 57 failed to return the questionnaires. A total of 657 questionnaires were returned, giving a response rate of 91%, out of which 603 were considered as valid.
According to the responses, the overall prevalence of ED in T2DM men as defined by the IIEF-5 was 79.1% (Table 1). Among subjects with ED, the most prevalent was mild ED (28.9%), followed by mild-to-moderate (27.9%), moderate (13.4%), and severe (9%) ED. The severity of ED increased with age according to the Kruskal-Wallis ANOVA test (Table 2).
Table 1.
Demographics and prevalence of ED of subjects (n=603)
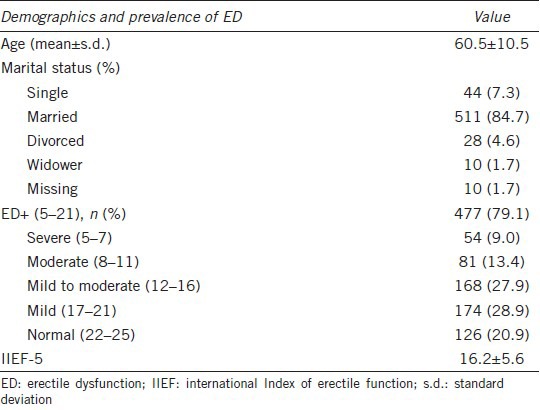
Table 2.
Characteristics by severity of ED
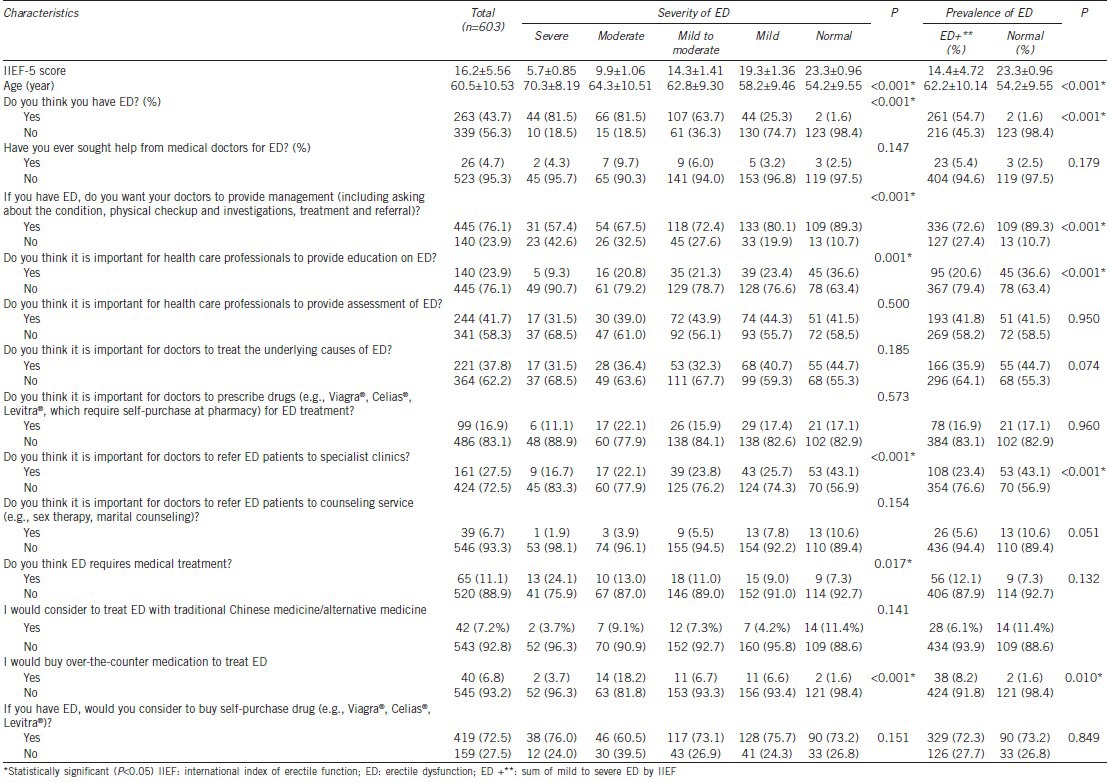
Among all subjects screened ED positive by IIEF-5, only 54.7% thought they had ED. For subjects with severe to moderate ED, 18.5% thought they had no ED. When we compared ED diagnosed by the single self-reported question on ED to IIEF-5 (Table 2), the single question was highly specific (specificity = 98.4%), but the sensitivity was only 54.7%. Hence, the use of the single self-reported question to screen for ED was shown to have missed more than half of the ED cases, including those with moderate to severe ED.
For the perceived causes of ED (Figure 1), 45.4% viewed ED as a natural consequence of aging; 29.5% perceived it as an illness which requires treatment; 12.6% regarded it as a secondary consequence of another disease; <10% did not regard it as a disease, or consider it a transient disturbance which requires no action.
Figure 1.
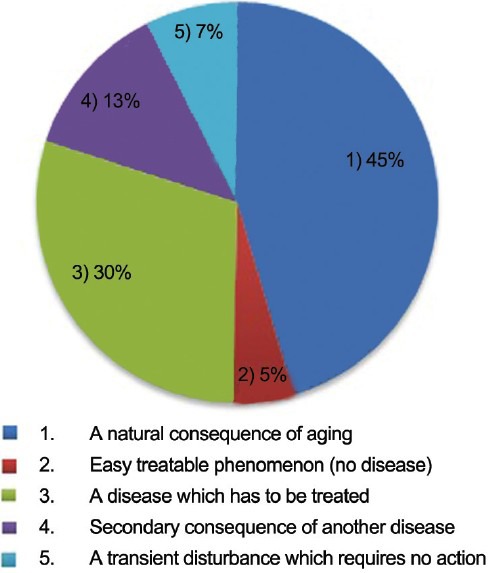
Perception of erectile dysfunction (n = 603).
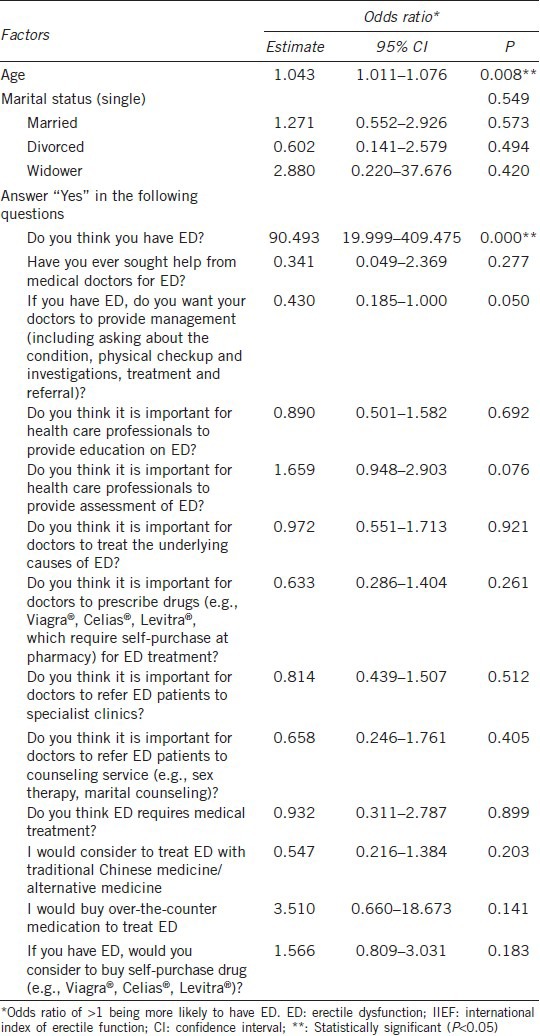
With regards to ED management, <10% of the subjects with ED had ever sought help from any doctor regardless of degree of severity. However, 76.1% of the subjects preferred receiving management from doctors should they be diagnosed with ED. For management options, 41.7% would like assessment by doctor, followed by management of potential underlying cause (37.8%), referral to specialist (27.5%), education and information on ED (23.9%), prescription of phosphodiesterase type 5 inhibitors (PDE-5) (16.9%) and referral to counseling service (6.7%) (Table 3). An overall decreasing trend of management desire with increasing ED severity, both in general and in the various modalities of management, was observed. Logistic regression analysis reported age, self-perception of ED and expectations on ED management to be significant factors associated with the presence of ED. Older subjects (OR: 1.043) or those with greater self-perception of ED (OR: 90.493) were associated with higher odds of having ED. Those with higher expectation of receiving management were associated with lower odds of having ED.
Table 3.
Factors associated with the presence of ED (by IIEF.5)
DISCUSSION
This survey on prevalence, attitude and treatment seeking behavior of ED among T2DM men attending primary care clinics obtained a response rate of 91%. The study showed a 79.1% prevalence of ED in T2DM Chinese men, and an increase in ED severity with age. Such findings correlate well with past literature.4,5 Most of the subjects had mild (28.9%) and mild to moderate (27.9%) ED, while a higher than expected proportion were having moderate to severe ED (22.4%). The severity of ED among our subjects were very similar to findings from a multi-clinic study in Mainland China,4 which revealed 9.1% as suffering from severe ED, 17.2% moderate, and 48.9% mild ED, as compared with 9.0%, 13.4%, and 56.8% respectively in our study. This high prevalence should caution both the public and health care professionals in view of the higher cardiovascular risk and psychological comorbidity associated with the condition. Regular screening of ED in T2DM men, and patient education to increase awareness and treatment seeking should be administered.
The seemingly highly specific single self-reporting question “Do you think you have ED?” was found to be an insensitive method for screening ED among T2DM patients. It is therefore important to choose a practical and more sensitive screening method for this highly prevalent group to enhance early detection and intervention. Asking T2DM patients to fill out self-administered questionnaires (e.g. IIEF-5) before the annual complication screening clinic appears to be a good option in our daily practice.
Only 30% of the respondents in this study regarded ED as a disease which requires treatment, and 45% thought it was simply a consequence of aging (Figure 1). Nearly 76.1% of the respondents wanted to receive management from doctors if they had ED, suggesting that though effective ED treatment was not much expected by our patients, they still wanted some form of management such as physical examination, investigation of possible cause, and referral to specialists. In particular, most subjects expected doctors to do an assessment and management of potential underlying causes, which include diabetic control and other cardiovascular risk factors. The results reflected the need for individualized evaluation of each T2DM patient with ED.38 This message should be clearly promulgated to all frontline doctors and nurses. Health care professionals should routinely screen all T2DM patients for ED and offer proper management should they be inflicted with the condition.
The low treatment seeking rate (<10%) for ED, despite the subjects’ desire for management verifies the existence of patient barriers as suggested in past literatures. This again points to the importance of the need of good screening for ED so that proper management of the overall condition may be given. Early detection is desirable as patients’ keenness for management decreases with increasing ED severity.
The acceptance of drug therapy for ED was relatively low in our subjects (16.9%), a finding comparable to previous studies.4,39 The cost of PDE-5 is likely a concern and yet the efficacy is not guaranteed. Apart from drug treatment, most subjects did not consider referral to counseling service or information and education sessions from health care professionals to be important.
Limited demographic and clinical data were collected due to the anonymous nature of our study. These would need to be taken into account in future studies. Further studies should be conducted to evaluate the different ED screening tools and investigate structural approaches to ED in correlation to different subgroups of T2DM men.
CONCLUSIONS
ED is highly prevalent in T2DM Chinese men in the primary care setting. In our study, more than one-fifth of them suffered from moderate to severe ED. T2DM men with ED wanted management from doctors, but they seldom seek help actively. Most of them expected doctors to offer assessment and management of potential underlying causes, while desire for counseling and education services and drug therapy was low.
AUTHOR CONTRIBUTIONS
All authors designed the study protocols and the study questionnaire. WHL and SNF coordinated and supervised data collections in research sites. CKHW designed and performed statistical analysis and drafted all result tables. WHL and ESC drafted the manuscript. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declare no competing interests.
ACKNOWLEDGMENTS
This study would not have been possible without the support of the Department of Family Medicine and Primary Care of the University of Hong Kong, the Kowloon West Cluster Family Medicine and Primary Healthcare Department and the 10 participating GOPCs. Our special gratitude goes to Professor Cindy Lam, Professor William CW Wong, Dr. WY Chin, Dr. YK Yiu, Dr. KL Cheung, Dr. PS Lau, Dr. Susanna Hung, Dr. TY Lo and the doctors, nurses and staffs of the 10 GOPCs.
REFERENCES
- 1.Yang W, Lu J, Weng J, Jia W, Ji L, et al. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362:1090–101. doi: 10.1056/NEJMoa0908292. [DOI] [PubMed] [Google Scholar]
- 2.Wong KW, Ho SY, Chao DV. Quality of diabetes care in public primary care clinics in Hong Kong. Fam Pract. 2012;29:196–202. doi: 10.1093/fampra/cmr060. [DOI] [PubMed] [Google Scholar]
- 3.Tamler R. Diabetes, obesity, and erectile dysfunction. Gend Med. 2009;6(Suppl 1):4–16. doi: 10.1016/j.genm.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 4.Yang G, Pan C, Lu J. Prevalence of erectile dysfunction among Chinese men with type 2 diabetes mellitus. Int J Impot Res. 2010;22:310–7. doi: 10.1038/ijir.2010.21. [DOI] [PubMed] [Google Scholar]
- 5.Siu SC, Lo SK, Wong KW, Ip KM, Wong YS. Prevalence of and risk factors for erectile dysfunction in Hong Kong diabetic patients. Diabet Med. 2001;18:732–8. doi: 10.1046/j.0742-3071.2001.00557.x. [DOI] [PubMed] [Google Scholar]
- 6.Yu LW, Kong AP, Tong PC, Tam C, Ko GT, et al. Evaluation of erectile dysfunction and associated cardiovascular risk using structured questionnaires in Chinese type 2 diabetic men. Int J Androl. 2010;33:853–60. doi: 10.1111/j.1365-2605.2009.01026.x. [DOI] [PubMed] [Google Scholar]
- 7.Jiann BP, Lu CC, Lam HC, Chu CH, Sun CC, et al. Patterns and their correlates of seeking treatment for erectile dysfunction in type 2 diabetic patients. J Sex Med. 2009;6:2008–16. doi: 10.1111/j.1743-6109.2009.01264.x. [DOI] [PubMed] [Google Scholar]
- 8.Dean J. Characterisation, prevalence, and consultation rates of erectile dysfunction. Clin Cornerstone. 2005;7:5–11. doi: 10.1016/s1098-3597(05)80043-2. [DOI] [PubMed] [Google Scholar]
- 9.Tan HM, Low WY, Ng CJ, Chen KK, Sugita M, et al. Prevalence and correlates of erectile dysfunction (ED) and treatment seeking for ED in Asian Men: the Asian Men's Attitudes to Life Events and Sexuality (MALES) study. J Sex Med. 2007;4:1582–92. doi: 10.1111/j.1743-6109.2007.00602.x. [DOI] [PubMed] [Google Scholar]
- 10.Cheng JY, Ng EM, Chen RY, Ko JS. Prevalence of erectile dysfunction in Asian populations: a meta-analysis. Int J Impot Res. 2007;19:229–44. doi: 10.1038/sj.ijir.3901517. [DOI] [PubMed] [Google Scholar]
- 11.Phé V, Rouprêt M. Erectile dysfunction and diabetes: a review of the current evidence-based medicine and a synthesis of the main available therapies. Diabetes Metab. 2012;38:1–13. doi: 10.1016/j.diabet.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 12.Rosen RC, Wing RR, Schneider S, Wadden TA, Foster GD, et al. Erectile dysfunction in type 2 diabetic men: relationship to exercise fitness and cardiovascular risk factors in the Look AHEAD trial. J Sex Med. 2009;6:1414–22. doi: 10.1111/j.1743-6109.2008.01209.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.El-Sakka AI. Erectile dysfunction, depression, and ischemic heart disease: does the existence of one component of this triad necessitate inquiring the other two? J Sex Med. 2011;8:937–40. doi: 10.1111/j.1743-6109.2011.02231.x. [DOI] [PubMed] [Google Scholar]
- 14.Low WY, Tong SF, Tan HM. Erectile dysfunction, premature ejaculation and hypogonadism and men's quality of life: an Asian perspective. J Men's Health. 2008;5:282–8. [Google Scholar]
- 15.Baldwin K, Ginsberg P, Harkaway RC. Under-reporting of erectile dysfunction among men with unrelated urologic conditions. Int J Impot Res. 2003;15:87–9. doi: 10.1038/sj.ijir.3900948. [DOI] [PubMed] [Google Scholar]
- 16.Salonia A, Ferrari M, Saccà A, Pellucchi F, Castagna G, et al. Delay in seeking medical help in patients with new-onset erectile dysfunction remained high over and despite the PDE5 era – an ecological study. J Sex Med. 2012;9:3239–46. doi: 10.1111/j.1743-6109.2012.02953.x. [DOI] [PubMed] [Google Scholar]
- 17.Perelman M, Shabsigh R, Seftel A, Althof S, Lockhart D. Attitudes of men with erectile dysfunction: a cross-national survey. J Sex Med. 2005;2:397–406. doi: 10.1111/j.1743-6109.2005.20355.x. [DOI] [PubMed] [Google Scholar]
- 18.Shabsigh R, Kaufman J, Magee M, Creanga D, Russell D, et al. Lack of awareness of erectile dysfunction in many men with risk factors for erectile dysfunction. BMC Urol. 2010;10:18. doi: 10.1186/1471-2490-10-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shabsigh R, Perelman MA, Laumann EO, Lockhart DC. Drivers and barriers to seeking treatment for erectile dysfunction: a comparison of six countries. BJU Int. 2004;94:1055–65. doi: 10.1111/j.1464-410X.2004.05104.x. [DOI] [PubMed] [Google Scholar]
- 20.Thomas CM, Marron B, Parr JH, Stewart A, Wahid ST, et al. Erectile dysfunction: “they don’t talk and we may not ask”. Diabet Med. 2010;27(Suppl 1):129. [Google Scholar]
- 21.Low WY, Ng CJ, Tan NC, Choo WY, Tan HM. Management of erectile dysfunction: barriers faced by general practitioners. Asian J Androl. 2004;6:99–104. [PubMed] [Google Scholar]
- 22.Hackett G, Kember LE. Barriers to knowledge, awareness, and diagnosis of erectile dysfunction and low testosterone in men: survey of 1,019 men and 222 general practitioners in the UK. J Sex Med. 2011;8:433. [Google Scholar]
- 23.Grant PS, Lipscomb D. How often do we ask about erectile dysfunction in the diabetes review clinic. Development of a neuropathy screening tool? Acta Diabetol. 2009;46:285–90. doi: 10.1007/s00592-008-0084-1. [DOI] [PubMed] [Google Scholar]
- 24.McCabe M, Matic H. Severity of ED: relationship to treatment-seeking and satisfaction with treatment using PDE5 inhibitors. J Sex Med. 2007;4:145–51. doi: 10.1111/j.1743-6109.2006.00401.x. [DOI] [PubMed] [Google Scholar]
- 25.Evangelia N, Kirana PS, Chiu G, Link C, Rosen R, et al. Level of bother and treatment-seeking predictors among male and female in-patients with sexual problems: a hospital-based study. J Sex Med. 2010;7:700–11. doi: 10.1111/j.1743-6109.2009.01605.x. [DOI] [PubMed] [Google Scholar]
- 26.Gerster S, Günzler C, Roesler C, Leiber C, Berner MM. Treatment motivation of men with ED: what motivates men with ED to seek professional help and how can women support their partners? Int J Impot Res. 2013;25:56–62. doi: 10.1038/ijir.2012.37. [DOI] [PubMed] [Google Scholar]
- 27.Günzler C, Kriston L, Stodden V, Leiber C, Berner MM. Can written information material help to increase treatment motivation in patients with erectile dysfunction? A survey of 1188 men. Int J Impot Res. 2007;19:330–5. doi: 10.1038/sj.ijir.3901531. [DOI] [PubMed] [Google Scholar]
- 28.Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–26. doi: 10.1038/sj.ijir.3900472. [DOI] [PubMed] [Google Scholar]
- 29.Kleinman KP, Feldman HA, Johannes CB, Derby CA, McKinlay JB. A new surrogate variable for erectile dysfunction status in the Massachusetts male aging study. J Clin Epidemiol. 2000;53:71–8. doi: 10.1016/s0895-4356(99)00150-x. [DOI] [PubMed] [Google Scholar]
- 30.O’Leary MP, Fowler FJ, Lenderking WR, Barber B, Sagnier PP, et al. A brief male sexual function inventory for urology. Urology. 1995;46:697–706. doi: 10.1016/S0090-4295(99)80304-5. [DOI] [PubMed] [Google Scholar]
- 31.American Diabetes Association. Standards of medical care in diabetes – 2013. Diabetes Care. 2013;36(Suppl 1):S11–66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Institute for Health and Clinical Excellence. CG66 type 2 diabetes: full guideline. [Last updated on 2011 Jun 14; Last accessed on 2013 Sep 22]. Available from: http://www.nice.org.uk/guidance/index.jsp?action=download and o=40803 .
- 33.O’Donnell AB, Araujo AB, Goldstein I, McKinlay JB. The validity of a single-question self-report of erectile dysfunction. Results from the Massachusetts Male Aging Study. J Gen Intern Med. 2005;20:515–9. doi: 10.1111/j.1525-1497.2005.0076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berner MM, Plöger W, Burkart M. A typology of men's sexual attitudes, erectile dysfunction treatment expectations and barriers. Int J Impot Res. 2007;19:568–76. doi: 10.1038/sj.ijir.3901571. [DOI] [PubMed] [Google Scholar]
- 35.Colagiuri S. WHO/IDF guidelines on the diagnostic criteria for diabetes and impaired glycaemic regulation: 570. Diabetic Med. 2006;23(Suppl 4):202. [Google Scholar]
- 36.Adams G, Gulliford MC, Ukoumunne OC, Eldridge S, Chinn S, et al. Patterns of intra-cluster correlation from primary care research to inform study design and analysis. J Clin Epidemiol. 2004;57:785–94. doi: 10.1016/j.jclinepi.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 37.Machin D, Campbell M, Fayers P, Pinol A. Oxford: Blackwell Science Ltd; 1997. Sample Size Tables for Clinical Studies. [Google Scholar]
- 38.Hatzichristou D. Understanding individuals’ response to erectile dysfunction. Int J Impot Res. 2008;20(Suppl 2):S15–20. doi: 10.1038/ijir.2008.48. [DOI] [PubMed] [Google Scholar]
- 39.Behrend L, Vibe-Petersen J, Perrild H. Sildenafil in the treatment of erectile dysfunction in men with diabetes: demand, efficacy and patient satisfaction. Int J Impot Res. 2005;17:264–9. doi: 10.1038/sj.ijir.3901302. [DOI] [PubMed] [Google Scholar]


