Abstract
Angiotensin-converting enzyme gene (ACE) insertion/deletion (I/D) polymorphism have long been linked to sporadic Alzheimer disease (SAD), but the established data remained controversial. To clarify this inconsistency, a comprehensive meta-analysis was conducted. Through searching of Pubmed, Embase, Alzgene, China National Knowledge Infrastructure (CNKI) and manually searching relevant references, 53 independent studies from 48 articles were included, involving a total of 8153 cases and 14932 controls. The strength of association was assessed by using odds ratios (ORs) with 95% confidence intervals (CIs). Further stratified analyses and heterogeneity analyses were tested, as was publication bias. Overall, significant associations were revealed between I/D polymorphism and SAD risk using allelic comparison (OR = 1.09, 95%CI = 1.01–1.17, p = 0.030), homozygote comparison (OR = 1.17, 95%CI = 1.01–1.34, p = 0.030) and the dominant model (OR = 1.16, 95%CI = 1.04–1.29, p = 0.008), but they were not sufficiently robust to withstand the false-positive report probability (FPRP) analyses. Otherwise, in subgroup analyses restricted to the high quality studies, the large sample size studies and studies with population-based controls, no significant association was observed in any genetic models. In summary, the current meta-analysis suggested that the ACE I/D polymorphism is unlikely to be a major determining factor in the development of SAD.
Introduction
Alzheimer's disease (AD) is the most common form of dementia in the elderly, and it is characterized by progressive memory loss and cognitive dysfunction [1]. Although some AD cases are familial, about 90% are sporadic [2]. Sporadic Alzheimer's disease (SAD) is considered to be a multifactorial disease with a complex interaction of both genetic and environmental factors [3]. One of the proposed mechanisms for SAD is the amyloid hypothesis, which suggests that deposition of beta-amyloid (Aβ) is a primary event in the pathological cascade for SAD [4]. The balance between the expression and the degradation of Aβ changes, and aggregate of Aβ would cause complex reactions, such as phosphorylation of protein Tau [5], loss of neurotransmitter [6] and finally formation of senile plaques (SP), as well as intracellular neurofibrillary tangles.
Recently, growing evidence has implicated angiotensin-converting enzyme (ACE), a zinc metalloprotease widely expressed in brain, as a possible modulator of Aβ metabolism [7]. The ACE gene is located on chromosome 17q23 and consists of 26 exons and 25 introns. The most common polymorphism of ACE gene is the insertion/deletion (I/D) variant of 287 base pairs in intron 16, which has been suggested to be associated with serum ACE protein levels [8], the specific activity of ACE protein domain [9], the transcriptional activity of ACE gene promoter region [10] and resulted in the susceptibility to SAD. A study published in 1999 first reported the association between the I/D polymorphism and SAD in a combined sample of three case-control samples from the United Kingdom [11]. Since then, a great number of studies have been performed on this polymorphism with SAD risk in different populations but have generated equivocal results. Therefore, in 2003–2005, three meta-analyses [12]–[14] have been published and implied possible association of the I/D polymorphism on AD risk. However, there were more and further single studies after 2005. Hence, an updated meta-analysis combining all available studies was performed to derive a more precise estimation of this relationship.
Materials and Methods
Literature search
This meta-analysis was performed according to the methodology advocated by the PRISMA statement [15]. All studies included in the meta-analysis were selected by searching the Pubmed, EMBASE, Alzgene and China National Knowledge Infrastructure (CNKI) databases up to May 2014 using the following keywords: “(Alzheimer or AD) and (angiotensin-converting enzyme gene or ACE) and (polymorphism or variant or genotype)”. In addition, the reference lists of reviews and retrieved articles were checked for potential studies. Articles that reported results from more than 1 population were considered as separate studies. Only studies published in English or Chinese were included.
Inclusion criteria
The studies included in the meta-analysis were required to meet the following criteria: (1) case-control or cohort design; (2) association between I/D polymorphism and SAD risk; (3) application of standardized clinical or pathologic criteria for the diagnosis of SAD; (4) sufficient genotype distributions for calculation of odds ratios (ORs) with 95% confidence intervals (CIs);
The following were excluded: (1) reports with incomplete data; (2) review articles, abstracts, case reports; (3) studies based on familiar Alzheimer's disease (FAD) or mild cognitive impairment (MCI); (4) studies about other ACE polymorphisms. When the articles contained duplicated data, the most recent or complete studies were selected.
Data extraction
Data were extracted from eligible articles independently by two of the authors, with any disagreement resolved by consensus. The following information was collected in a predefined data collection form: first author's name, publication year, country, geographical location of participants (North European, South Caucasian, Asian, etc), sample size, AD diagnosis criteria, genotyping methods, source of controls, risk allele frequency in controls, results of Hardy-Weinberg equilibrium (HWE) in controls and quality assessment of studies.
Quality score assessment
The quality of each study was independently assessed by two authors who used quality scoring criteria modified from previous studies [16], [17] (Table S1 in File S1). The modified criteria cover the representativeness of cases, the credibility of controls, genotyping examination, association assessment and total sample size. Quality scores ranged from 0 point (worst) to 12 points (best). Studies scoring higher than 9 points were classified as high quality.
Statistical analysis
First, deviance from HWE was assessed for the controls of each study using the chi-squared test. Second, genotype distributions of controls were used to estimate the frequency of the putative risk allele (I allele) in various geographic location using the inverse variance method [16]. Third, we mainly examined the overall effects for I/D polymorphism. Briefly, the pooled ORs along with their corresponding 95% CIs were estimated for allelic comparison (I vs D), additive model (homozygote comparison: II vs DD; heterozygote comparison: ID vs DD), the recessive model (II vs ID+DD) and the dominant model (II+ID vs DD).
Cochran's Q statistic was used to test for heterogeneity, and the percentage variability of the heterogeneity between studies was quantified using the I2 statistic. Thus, I2 values around 25%, 50% and 75% would indicate low, medium and high heterogeneity respectively [18] . The random-effect model (DerSimonian-Laird) [19] was used to assess pooled ORs when I2 (%)>50% or P (Q)<0.10. Otherwise, the fixed-effect model (Mantel-Haenszel) [20] was used. Subgroup analyses were performed, when feasible, according to geographic location (ethnicity), sample size, quality appraisal score, genotyping methods, source of controls, and publication time. In addition, a meta-regression procedure was adopted to find potential sources of heterogeneity [21]. Further, Galbraith plots were used to visualize the impact of individual studies on the overall homogeneity, which identified the outliers as possible major sources of heterogeneity [22]. Cumulative meta-analyses of associations for I/D polymorphism were also performed to investigate the trend and the stability of risk effects as evidence accumulated over time (by publication year). In addition, sensitivity analyses were carried out to evaluate the stability of the results through sequential removal of each study or after excluding those studies that deviated from HWE. Moreover, sensitivity analyses limited to only the English-language studies were conducted to investigate the influence of Chinese-language studies on the overall meta-analysis. Publication bias was assessed graphically by funnel plots [23] and formally by Egger's tests [24] and Begg’s tests [25], given a significant value of 0.05. All of the above analyses were conducted using RevMan 5.2 (The Nordic Cochrane Centre, The Cochrane Collaboration) & STATA 12.0 (Stata, College, TX, USA).
For each statistically significant association, the false-positive report probability (FPRP) analyses were performed using the method reported by Wacholder et al [26]. The FPRP value is determined by the p value, the prior probability for the association, and statistical power. We calculated FPRP assuming a prior probability of 0.001 as previously proposed [27] for candidate gene analyses. Statistical power was based on the ability to detect an OR of 1.5, with α equal to the observed p value. An FPRP cutoff value of 0.2 was used [26] and only the results with FPRP value less than 0.2 were referred as noteworthy. Statistical power and FPRP analyses were computed using the Excel spreadsheet provided by Wacholder et al [26].
Result
Study characteristics
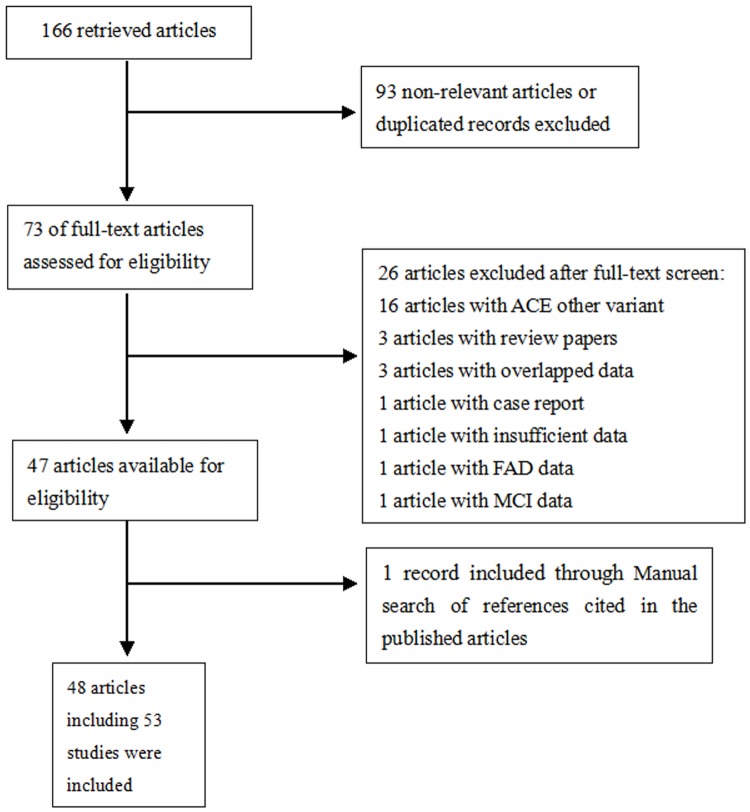
A total of 166 relevant articles were initially identified from Pubmed, EMBASE, Alzgene and CNKI databases. After titles and abstracts were screened, 93 articles were excluded because of irrelevant data. The full texts of the remaining 73 records were carefully reviewed (Fig. 1). Among these articles, 16 articles were about other ACE SNPs; two articles were excluded because of FAD [28] or MCI data [29]; four articles were excluded due to case reports [30] or review papers [31]–[33]; four articles were excluded owing to overlapped [34]–[36] or insufficient data [37]. Manual search of references cited in the published articles revealed one additional article [38]. Four of the eligible articles [11], [39]–[41] contained data from 9 independent studies. Therefore, 48 articles including 53 studies were included in the present meta-analysis [11], [12], [14], [38]–[82]. Among these studies, a total of 18 studies reported on North European populations; 14 studies on South Caucasians (defined here as from the Mediterranean or Jews); 15 studies on Asians and 6 studies on other ethnicities. Deviation of HWE was detected in the control subjects of eight studies [39], [40], [48], [50], [52], [64], [66], [71]. The flowchart for the process of including/excluding articles is shown in Figure 1, and the characteristics of all included studies are summarized in Table 1.
Figure 1. Flow chart of article selection in our meta-analysis.
Table 1. Characteristics of included studies in this meta-analysis evaluating the effects of I/D polymorphism on the risk of developing SAD.
| No. | First author (Year) | Country | Ethnicity | Sample size (Case/Control) | Criteria for SAD diagnosis | Genotyping method | Source of control | I allele frequency (%) | HWE (p) | Quality score |
| 1 | Scacchi 1998 [42] | Italy | South Caucasian | 80/153 | NINCDS/ADRDA | PCR (original primer) | P | 36.9 | Y (0.764) | 8 |
| 2 | Chapman 1998 [43] | Israel | South Caucasian | 49/40 | NINCDS/ADRDA and DSM-III-R | PCR (original primer) | P | 33.8 | Y (0.754) | 7 |
| 3 | Kehoe (London) 1999 [11] | UK | North European | 135/111 | NINCDS/ADRDA | PCR (insertion specific primer) | P | 41.4 | Y (0.251) | 9 |
| 4 | Kehoe (Belfast) 1999 [11] | UK | North European | 209/198 | NINCDS/ADRDA | PCR (insertion specific primer) | P | 51.5 | Y (0.485) | 10 |
| 5 | Kehoe (Cardiff) 1999 [11] | UK | North European | 198/77 | NINCDS/ADRDA | PCR (insertion specific primer) | P | 40.3 | Y (0.820) | 10 |
| 6 | Palumbo 1999 [44] | Italy | South Caucasian | 140/40 | NINCDS/ADRDA | PCR (insertion specific primer) | P | 37.5 | Y (0.109) | 9 |
| 7 | Hu 1999 [45] | Japan | Asian | 132/148 | NINCDS/ADRDA | PCR (original primer) | P | 61.8 | Y (0.618) | 10 |
| 8 | Alvarez 1999 [46] | Spain | South Caucasian | 350/517 | NINCDS/ADRDA | PCR (insertion specific primer) | P | 37.3 | Y (0.458) | 11 |
| 9 | Farrer (Moscow) 2000 [39] | Moscow | North European | 151/206 | NINCDS/ADRDA | PCR (original primer) | M | 47.6 | Y (0.221) | 11 |
| 10 | Farrer (Mixed) 2000 [39] | Mixed | North American | 235/162 | NINCDS/ADRDA | PCR (original primer) | P | 38.6 | N (0.022) | 10 |
| 11 | Mattila 2000 [47] | Finland | North European | 80/67 | NINCDS/ADRDA and CERAD | PCR (insertion specific primer) | P | 38.1 | Y (0.879) | 9 |
| 12 | Crawford 2000 [48] | USA | North American | 171/175 | NINCDS/ADRDA | PCR (insertion specific primer) | P | 38.3 | N (0.018) | 11 |
| 13 | Myllykangas 2000 [49] | Finland | North European | 121/75 | NINCDS/ADRDA and CERAD | PCR (original primer) | A | 57.3 | Y (0.166) | 9 |
| 14 | Yang 2000 [50] | China | Asian | 188/227 | NINCDS/ADRDA and DSM-IV | PCR (original primer) | H | 57.5 | N (<0.001) | 8 |
| 15 | Narain 2000 [52] | UK | North European | 239/342 | CERAD | PCR (insertion specific primer) | P | 47.2 | N (<0.001) | 10 |
| 16 | Isbir 2000 [51] | Turkey | South Caucasian | 35/29 | NINCDS/ADRDA | PCR (original primer) | P | 48.3 | Y (0.356) | 7 |
| 17 | Zuliani 2001 [53] | Italy | South Caucasian | 40/54 | NINCDS/ADRDA | PCR (original primer) | P | 42.6 | Y (0.317) | 9 |
| 18 | Perry 2001 [54] | USA | African American | 111/78 | NINCDS/ADRDA | PCR (original primer) | P | 32.1 | Y (0.302) | 9 |
| 19 | Richard (Cohort 1) 2001 [40] | France | South Caucasian | 433/475 | NINCDS/ADRDA and DSM-III-R | PCR (insertion specific primer) | P | 45.2 | Y (0.833) | 11 |
| 20 | Richard (Cohort 2) 2001 [40] | France | South Caucasian | 56/221 | NINCDS/ADRDA and DSM-III-R | PCR (insertion specific primer) | M | 50.7 | N (0.050) | 10 |
| 21 | Buss 2002 [55] | Europe | North European | 261/306 | NINCDS/ADRDA | PCR (insertion specific primer) | P | 46.7 | Y (0.618) | 10 |
| 22 | Wu 2002 [56] a | China | Asian | 96/96 | DSM-IV | PCR (original primer) | P | 49.5 | Y (0.839) | 9 |
| 23 | Lendon 2002 [57] | UK | North European | 214/99 | NINCDS/ADRDA and DSM-III-R | PCR (original primer) | P | 49.5 | Y (0.365) | 10 |
| 24 | Monastero 2002 [58] | Italy | South Caucasian | 149/149 | NINCDS/ADRDA | PCR (original primer) | P | 39.9 | Y (0.444) | 10 |
| 25 | Cheng 2002 [59] | China | Asian | 173/116 | NINCDS/ADRDA | PCR (insertion specific primer) | P | 64.7 | Y (0.545) | 11 |
| 26 | Panza 2003 [60] | Italy | South Caucasian | 141/268 | NINCDS/ADRDA | PCR (insertion specific primer) | P | 37.7 | Y (0.115) | 11 |
| 27 | Seripa (Italy) 2003 [41] | Italy | South Caucasian | 126/106 | NINCDS/ADRDA | PCR (insertion specific primer) | P | 37.7 | Y (0.708) | 10 |
| 28 | Seripa (USA) 2003 [41] | USA | North American | 124/97 | NINCDS/ADRDA and CERAD | PCR (insertion specific primer) | A | 45.4 | Y (0.098) | 10 |
| 29 | Kehoe 2003 [12] | UK | North European | 333/109 | CERAD | PCR (insertion specific primer) | A | 45.9 | Y (0.681) | 11 |
| 30 | Carbonell 2003 [61] | UK | North European | 80/65 | NINCDS/ADRDA | PCR (original primer) | M | 49.2 | Y (0.903) | 8 |
| 31 | Camelo 2004 [62] | Columbia | South American | 83/68 | NINCDS/ADRDA | PCR (original primer) | P | 47.8 | Y (0.456) | 7 |
| 32 | Chalmers 2004 [63] | UK | North European | 83/58 | CERAD | PCR (insertion specific primer) | A | 43.1 | Y (0.904) | 9 |
| 33 | Feng 2004 [64] a | China | Asian | 26/68 | DSM-IV | PCR (insertion specific primer) | P | 60.3 | N (<0.001) | 7 |
| 34 | Lehmann 2005 [14] | UK | North European | 203/248 | NINCDS/ADRDA | PCR (original primer) | M | 46.2 | Y (0.713) | 10 |
| 35 | Kolsch 2005 [65] | Germany | North European | 351/348 | DSM-IV | PCR (insertion specific primer) | P | 45.3 | Y (0.174) | 12 |
| 36 | Zhang 2005 [66] | China | Asian | 192/195 | NINCDS/ADRDA and DSM-IV | PCR (original primer) | P | 65.4 | N (0.006) | 8 |
| 37 | Sleeger 2005 [67] | Netherland | North European | 250/6403 | DSM-III-R | PCR (insertion specific primer) | P | 47.1 | Y (0.428) | 12 |
| 38 | Keikhaee 2006 [68] | Iran | Asian | 117/125 | NINCDS/ADRDA | PCR (original primer) | P | 43.2 | Y (0.806) | 8 |
| 39 | Meng 2006 [69] | Israel | South Caucasian | 92/166 | NINCDS/ADRDA | PCR (original primer) | P | 31.0 | Y (0.993) | 8 |
| 40 | Wehr 2006 [70] | Poland | North European | 100/144 | NINCDS/ADRDA | PCR (insertion specific primer) | P | 48.6 | Y (0.492) | 9 |
| 41 | Wang B 2006 [71] | China | Asian | 104/128 | DSM-III-R | PCR (original primer) | P | 62.1 | N (0.013) | 7 |
| 42 | Wang HK 2006 [72] | China | Asian | 151/161 | NINCDS/ADRDA and DSM-IV | PCR (insertion specific primer) | P | 76.1 | Y (0.929) | 11 |
| 43 | Nacimas 2007 [73] | Italy | South Caucasian | 235/303 | DSM-IV | PCR (insertion specific primer) | P | 33.7 | Y (0.145) | 12 |
| 44 | Liu 2007 [74] a | China | Asian | 39/50 | NINCDS/ADRDA and DSM-IV | PCR (original primer) | P | 57.0 | Y (0.311) | 7 |
| 45 | Han 2008 [75] a | China | Asian | 55/59 | NINCDS/ADRDA | PCR (original primer) | P | 61.1 | Y (0.441) | 7 |
| 46 | Vardy 2009 [38] | UK | North European | 94/188 | NINCDS/ADRDA | PCR (insertion specific primer) | H | 47.9 | Y (0.980) | 10 |
| 47 | Miners 2009 [76] | UK | North European | 86/49 | CERAD | PCR (insertion specific primer) | A | 34.7 | Y (0.487) | 8 |
| 48 | Ning 2010 [77] | China | Asian | 138/469 | NINCDS/ADRDA and DSM-III-R | PCR (original primer) | P | 61.3 | Y (0.528) | 11 |
| 49 | Nirmal 2011 [78] | India | Asian | 95/130 | DSM-IV | PCR (insertion specific primer) | P | 45.4 | Y (0.937) | 10 |
| 50 | Cousin 2011 [79] | France | South Caucasian | 421/460 | NINCDS/ADRDA | PCR (original primer) | P | 44.5 | Y (0.582) | 10 |
| 51 | Lucatelli 2011 [80] | Brazil | South American | 35/67 | NINCDS/ADRDA and DSM-IV | PCR (original primer) | P | 53.7 | Y (0.072) | 8 |
| 52 | Yang 2011 [81] | China | Asian | 257/137 | NINCDS/ADRDA | PCR (insertion specific primer) | P | 74.1 | Y (0.213) | 12 |
| 53 | Zhang 2014 [82] a | China | Asian | 96/102 | NINCDS/ADRDA and DSM-IV | PCR (original primer) | H | 49.5 | Y (0.999) | 8 |
NINCDA/ADRDA: The National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer’s Disease and Related Disorders Association; DSM: Diagnostic and Statistical Manual of Mental Disorders; CERAD: Consortium to Establish a Registry for Alzheimer’s Disease; P: population-based controls; M: Mixed; A: autopsy controls; H: Hospital-based controls; HWE: Hardy-Weinberg equilibrium; Y: Yes; N: No.
Chinese-language studies.
Pooled prevalence of I/D polymorphism in controls
Overall, the eligible studies included 8153 cases and 14932 controls, and all these samples were genotyped. The pooled frequencies of the ACE I allele in control populations demonstrated variation among geographic location/ethnicity groups. Frequencies of the I allele were highest among Asians (59.3%, 95%CI = 54.5–63.9%, using random-effect model), followed by North Europeans (46.9%, 95%CI = 46.2–47.7%, using fixed-effect model) and South Caucasians (39.7%, 95%CI = 36.6–42.8%, using random-effect model). Sensitivity analyses excluding the HWE-deviated studies showed similar results.
Meta-analysis results
Summaries of the odds ratios for different comparisons were provided in Table 2. In brief, the associations between I/D polymorphism and SAD risk were revealed using allelic comparison (OR = 1.09. 95%CI = 1.01–1.17), homozygote comparison (OR = 1.17, 95%CI = 1.01–1.34) and the dominant model (OR = 1.16, 95%CI = 1.04–1.29). However, FPRP values at the pre-specified prior probability of 0.001were all higher than 0.2 (Table 3), indicating that the associations were not noteworthy. Otherwise, the recessive model showed no significant association in the overall comparisons and all subgroup analyses.
Table 2. Summary odds ratio and heterogeneity of the I/D polymorphism on SAD risk.
| Variables | N | Allelic comparison (I vs D) | Additive model (II vs DD) | Additive model (ID vs DD) | Recessive model (II vs ID+DD) | Dominant model (II+ID vs DD) | ||||||||||
| OR (95%CI)a | I2 (%) | P (Q) | OR (95%CI)a | I2 (%) | P (Q) | OR (95%CI)a | I2 (%) | P (Q) | OR (95%CI)a | I2 (%) | P (Q) | OR (95%CI)a | I2 (%) | P (Q) | ||
| Overall | 53 | 1.09 (1.01, 1.17) | 60 | <10−3 | 1.17 (1.01, 1.34) | 52 | <10−3 | 1.11 (0.98, 1.25) | 60 | <10−3 | 1.08 (0.96, 1.21) | 53 | <10−3 | 1.16 (1.04, 1.29) | 51 | <10−3 |
| All in HWE | 45 | 1.11 (1.03, 1.20) | 56 | <10 −3 | 1.19 (1.02, 1.38) | 49 | <10 −3 | 1.08 (0.95, 1.24) | 58 | <10−3 | 1.10 (0.97, 1.25) | 52 | <10−3 | 1.17 (1.05, 1.31) | 45 | 0.001 |
| English-language articles | 48 | 1.07 (0.99, 1.15) | 56 | <10−3 | 1.13 (0.98, 1.29) | 48 | <10−3 | 1.09 (0.96, 1.24) | 62 | <10−3 | 1.05 (0.94, 1.17) | 48 | <10−3 | 1.14 (1.02, 1.27) | 50 | <10 −3 |
| Geographic location | ||||||||||||||||
| North European | 18 | 1.11 (1.01, 1.21) | 36 | 0.067 | 1.24 (1.05, 1.48) | 24 | 0.176 | 1.16 (0.91, 1.48) | 34 | 0.100 | 1.12 (0.97, 1.29) | 25 | 0.165 | 1.22 (1.03, 1.45) | 25 | 0.125 |
| South Caucasian | 14 | 0.99 (0.91, 1.09) | 15 | 0.292 | 0.96 (0.80, 1.16) | 9 | 0.356 | 0.98 (0.83, 1.15) | 32 | 0.118 | 0.92 (0.78, 1.10) | 13 | 0.307 | 1.04 (0.93, 1.17) | 0 | 0.525 |
| Asian | 15 | 1.19 (0.96, 1.49) | 80 | <10−3 | 1.38 (0.94, 2.04) | 75 | <10−3 | 1.16 (0.86, 1.57) | 56 | 0.004 | 1.27 (0.96, 1.67) | 76 | <10−3 | 1.26 (0.91, 1.75) | 68 | <10−3 |
| Other ethnicities | 6 | 1.04 (0.82, 1.31) | 25 | 0.150 | 1.02 (0.69, 1.52) | 39 | 0.148 | 1.24 (0.90, 1.73) | 41 | 0.131 | 0.90 (0.69, 1.18) | 0 | 0.421 | 1.15 (0.82, 1.63) | 54 | 0.053 |
| Study quality | ||||||||||||||||
| High (>9) | 28 | 1.05 (0.97, 1.15) | 63 | <10−3 | 1.10 (0.94, 1.30) | 54 | <10−3 | 1.02 (0.88, 1.25) | 65 | <10−3 | 1.05 (0.91, 1.21) | 63 | <10−3 | 1.10 (0.98, 1.23) | 45 | 0.005 |
| Low (≤9) | 25 | 1.14 (0.99, 1.30) | 57 | <10−3 | 1.27 (0.99, 1.63) | 50 | 0.003 | 1.25 (1.02, 1.54) | 46 | 0.007 | 1.13 (0.94, 1.36) | 35 | 0.046 | 1.25 (1.01, 1.55) | 56 | <10 −3 |
| Sample size | ||||||||||||||||
| Large (≥250) | 28 | 1.04 (0.95, 1.14) | 66 | <10−3 | 1.09 (0.92, 1.29) | 59 | <10−3 | 1.01 (0.87, 1.18) | 67 | <10−3 | 1.04 (0.90, 1.20) | 63 | <10−3 | 1.08 (0.96, 1.23) | 54 | <10−3 |
| Small (<250) | 25 | 1.17 (1.03, 1.32) | 49 | <10 −3 | 1.32 (1.04, 1.66) | 39 | 0.024 | 1.28 (1.06, 1.55) | 35 | 0.042 | 1.16 (0.96, 1.40) | 34 | 0.048 | 1.29 (1.06, 1.56) | 45 | 0.009 |
| Source of control | ||||||||||||||||
| PB | 40 | 1.08 (0.99, 1.18) | 63 | <10−3 | 1.15 (0.96, 1.37) | 60 | <10−3 | 0.98 (0.90, 1.06) | 65 | <10−3 | 1.08 (0.94, 1.24) | 58 | <10−3 | 1.13 (0.99, 1.28) | 55 | <10−3 |
| Non PB | 13 | 1.11 (0.95, 1.28) | 52 | 0.015 | 1.18 (0.98, 1.43) | 5 | 0.400 | 1.29 (1.11, 1.50) | 0 | 0.624 | 1.04 (0.86, 1.25) | 27 | 0.175 | 1.24 (1.01, 1.52) | 35 | 0.102 |
| Date of publication time | ||||||||||||||||
| After or during 2003 | 28 | 1.06 (0.95, 1.18) | 65 | <10−3 | 1.10 (0.91, 1.33) | 53 | 0.001 | 0.94 (0.80, 1.10) | 52 | 0.001 | 1.10 (0.93, 1.30) | 61 | <10−3 | 1.05 (0.92, 1.20) | 38 | 0.023 |
| Before 2003 | 25 | 1.12 (1.01, 1.24) | 56 | <10 −3 | 1.24 (1.01, 1.53) | 52 | 0.001 | 1.30 (1.10, 1.54) | 54 | 0.001 | 1.06 (0.91, 1.23) | 41 | 0.017 | 1.28 (1.09, 1.52) | 58 | <10 −3 |
| Genotyping method | ||||||||||||||||
| PCR (insertion-specific) | 27 | 1.06 (0.96, 1.17) | 63 | <10−3 | 1.14 (0.94, 1.38) | 58 | <10−3 | 1.11 (0.92, 1.34) | 72 | <10−3 | 1.03 (0.88, 1.19) | 54 | 0.001 | 1.17 (1.01, 1.35) | 58 | <10 −3 |
| PCR (original primer) | 26 | 1.11 (0.99, 1.25) | 59 | <10−3 | 1.20 (0.98, 1.47) | 47 | 0.005 | 1.10 (0.94, 1.28) | 33 | 0.054 | 1.14 (0.96, 1.36) | 51 | 0.001 | 1.14 (0.97, 1.33) | 44 | 0.008 |
N: number of studies; OR: odd ratio; CI: confidence interval; I2: value of I2 for heterogeneity test; P (Q): p value of the Cochran’s Q test for heterogeneity.
A random-effect model was used when P (Q) <0.10 or I2>50%; otherwise, a fixed-effect model was used.
Bold values are significant associations before the FPRP analyses.
Table 3. False-positive report probability values for associations between SAD risk and I/D polymorphism.
| Significant association | OR (95%CI) | P a | Statistical powerb | Prior probability | ||||
| 0.25 | 0.1 | 0.01 | 0.001 | 0.0001 | ||||
| Overall analyses | ||||||||
| Allelic comparison (I vs D) | 1.09 (1.01, 1.17) | 0.030 | 1 | 0.049 | 0.133 | 0.628 | 0.945 | 0.994 |
| Additive model (II vs DD) | 1.17 (1.01, 1.34) | 0.030 | 1 | 0.065 | 0.173 | 0.698 | 0.959 | 0.996 |
| Dominant model (II+ID vs DD) | 1.16 (1.04, 1.29) | 0.008 | 1 | 0.018 | 0.053 | 0.379 | 0.860 | 0.984 |
| All in HWE | ||||||||
| Allelic comparison (I vs D) | 1.11 (1.03, 1.20) | 0.009 | 1 | 0.025 | 0.073 | 0.463 | 0.897 | 0.989 |
| Additive model (II vs DD) | 1.19 (1.02, 1.38) | 0.027 | 0.999 | 0.060 | 0.161 | 0.679 | 0.955 | 0.995 |
| Dominant model (II+ID vs DD) | 1.17 (1.05, 1.31) | 0.005 | 1 | 0.019 | 0.055 | 0.391 | 0.866 | 0.985 |
| English language article | ||||||||
| Dominant model (II+ID vs DD) | 1.14 (1.02, 1.27) | 0.018 | 1 | 0.050 | 0.135 | 0.633 | 0.946 | 0.994 |
| North European subgroup | ||||||||
| Allelic comparison (I vs D) | 1.11 (1.01, 1.21) | 0.033 | 1 | 0.050 | 0.138 | 0.637 | 0.947 | 0.994 |
| Additive model (II vs DD) | 1.24 (1.05, 1.48) | 0.012 | 0.983 | 0.050 | 0.136 | 0.634 | 0.946 | 0.994 |
| Dominant model (II+ID vs DD) | 1.22 (1.03, 1.45) | 0.022 | 0.990 | 0.068 | 0.179 | 0.706 | 0.960 | 0.996 |
| Low study quality subgroup | ||||||||
| Additive model (ID vs DD) | 1.25 (1.02, 1.54) | 0.034 | 0.957 | 0.102 | 0.253 | 0.789 | 0.974 | 0.997 |
| Dominant model (II+ID vs DD) | 1.25 (1.01, 1.55) | 0.038 | 0.952 | 0.117 | 0.284 | 0.814 | 0.978 | 0.998 |
| Small sample size subgroup | ||||||||
| Allelic comparison (I vs D) | 1.17 (1.03, 1.32) | 0.018 | 1 | 0.031 | 0.088 | 0.515 | 0.915 | 0.991 |
| Additive model (II vs DD) | 1.32 (1.04, 1.66) | 0.021 | 0.863 | 0.058 | 0.155 | 0.669 | 0.953 | 0.995 |
| Additive model (ID vs DD) | 1.28 (1.06, 1.55) | 0.011 | 0.948 | 0.035 | 0.098 | 0.545 | 0.924 | 0.992 |
| Dominant model (II+ID vs DD) | 1.29 (1.06, 1.56) | 0.010 | 0.940 | 0.027 | 0.076 | 0.476 | 0.902 | 0.989 |
| Non PB subgroup | ||||||||
| Additive model (ID vs DD) | 1.29 (1.11, 1.50) | 0.001 | 0.975 | 0.003 | 0.009 | 0.087 | 0.489 | 0.906 |
| Dominant model (II+ID vs DD) | 1.24 (1.01, 1.52) | 0.037 | 0.967 | 0.106 | 0.263 | 0.797 | 0.975 | 0.997 |
| Before 2003 subgroup | ||||||||
| Allelic comparison (I vs D) | 1.12 (1.01, 1.24) | 0.035 | 1 | 0.080 | 0.207 | 0.742 | 0.967 | 0.997 |
| Additive model (II vs DD) | 1.24 (1.01, 1.53) | 0.037 | 0.962 | 0.123 | 0.295 | 0.822 | 0.979 | 0.998 |
| Additive model (ID vs DD) | 1.30 (1.10, 1.54) | 0.002 | 0.951 | 0.008 | 0.022 | 0.200 | 0.716 | 0.962 |
| Dominant model (II+ID vs DD) | 1.28 (1.09, 1.52) | 0.003 | 0.965 | 0.015 | 0.043 | 0.333 | 0.835 | 0.981 |
| PCR (insertion-specific) subgroup | ||||||||
| Dominant model (II+ID vs DD) | 1.17 (1.01, 1.35) | 0.035 | 1 | 0.086 | 0.221 | 0.757 | 0.969 | 0.997 |
OR: odd ratio; CI: confidence interval.
p value for significant test; b Statistical power was calculated using the number of observations in the meta-analysis and the OR and p value in this table.
Bold values indicated that the prior probability <0.2.
When studies were stratified by sample size (Figure 2) and quality appraisal score (Figure 3), the significant associations were especially found in studies with small sample size and the low quality subgroup (Table 2). However, FPRP analyses suggested that the positive results were weak evidence of true associations (Table 3). Otherwise, it was noted that the significant associations between I/D variant and SAD risk disappeared when we restricted to the large sample size studies and the high quality studies (Table 2).
Figure 2. Meta-analysis for the association of SAD risk with ACE I/D polymorphism: subgroup analysis by sample size (allelic comparison: I vs D).
Figure 3. Meta-analysis for the association of SAD risk with ACE I/D polymorphism: subgroup analysis by quality appraisal score (dominant model: II+ID vs DD).
We also investigated potential influence arising from the use of different genotyping method (genotyping with insertion-specific primers prevents mistyping of ID to DD and is thus considered to be more accurate compared with the original method [83]) (Table 2). No statistically significant finding was observed in either the PCR with original primers subgroup or the PCR with insertion-specific primers counterpart, with one exception: a fragile significant finding was seen in the latter subgroup for the dominant model (OR = 1.17, 95%CI = 1.01−1.35), while it was not sufficient robust to withstand the FPRP analysis (Table 3).
When studies were stratified by source of controls (Table 2), significant elevated SAD risks were associated with the I/D polymorphism in the non population-based control subgroup for heterozygote comparison (OR = 1.29, 95%CI = 1.11−1.50) and the dominant model (OR = 1.24, 95%CI = 1.01−1.52), but not among the population-based control subgroup. However, FPRP values of two comparisons were 0.489, 0.975 respectively, indicating the associations were not reliable (Table 3).
The data were additionally stratified by publication time (Table 2). Significant increase associations were found before 2003 using allelic comparison (OR = 1.12, 95%CI = 1.01−1.24), additive model (for II vs DD, OR = 1.24, 95%CI = 1.01−1.53; for ID vs DD, OR = 1.30, 95%CI = 1.10−1.54) and the dominant model (OR = 1.28, 9%CI = 1.09−1.52). However, these associations were not observed between 2004–2014 in all genetic models. The cumulative meta-analysis also illustrated that the exaggerated effect was observed in the earliest study and the accumulated evidence hovered around the conventional 5% significance level until 2002 (Figure S1).
In the subgroup analysis by geographic location (Table 2), significantly increased risks were found among the North Europeans for allelic comparison (OR = 1.11, 95%CI = 1.01−1.21), homozygote comparison (OR = 1.24, 95%CI = 1.05−1.48) and the dominant model (OR = 1.22, 95%CI = 1.03−1.45). However, the associations did not pass the FPRP analyses (Table 3). Otherwise, no associations were detected in South Caucasians, Asians and mixed population groups in any genetic models.
Sensitivity analyses
Sensitivity analyses showed that no single study notably changed the pooled ORs, indicating that the results of this meta-analysis were stable. Furthermore, after exclusion of HWE-deviated studies, the corresponding pooled ORs did not change significantly (Table 2). However, when we restricted to the English-language studies, only the dominant model between I/D variant and SAD risk remained significant (Table 2), suggesting that a potential language bias was possible. This significant association did not pass the FPRP analysis either (Table 3).
Heterogeneity analyses
Moderate heterogeneity existed in the overall comparisons (Table 2). When we analyzed data by subgroups, heterogeneity was decreased only in several groups, including North European and South Caucasian populations, studies with other ethnicities, studies with non population-based controls. However, heterogeneity was remained in other subgroups (Table 2). Among all the covariates investigated by meta-regression analyses, sample size (P = 0.023) and publication time (P = 0.009) were factors that contributed to the observed heterogeneity across all studies under the heterozygote comparison (Table S2 in File S1). However, combining with these two factors could only explained 40.48% of the τ2 value in heterozygote comparison, indicating that sample size and publication time could explain part of the heterogeneity, but notable heterogeneity still existed. Otherwise, HWE, language, geographic location, quality of studies, sample size, publication time, source of controls and genotyping methods did not contribute the heterogeneity across the overall studies under other genetic comparisons (P>0.05) (Table S2 in File S1). Galbraith plots spotted at least fourteen studies (studies were spotted as the outliers in at least two genetic models) [11], [45], [47], [50], [56], [64], [65], [71], [72], [77], [80]–[82] as the outliers and the possible major sources of heterogeneity in the analyses of total studies (Figure S2a–e). It was noted that 9 [45], [50], [56], [64], [71], [72], [77], [81], [82] of these 14 studies belonged to Asian subgroup. However, we did not try to reduce the obvious heterogeneity by excluding these fourteen studies because it might be unacceptable and could cause some biases by excluding too many studies [84].
Publication bias
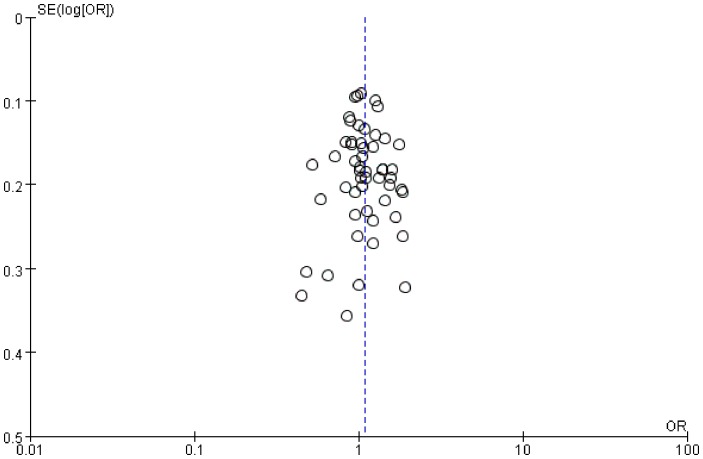
Funnel plots, Begg's and Egger's tests were performed to assess the publication bias. Funnel plots did not reveal obvious evidence of asymmetry (Figure 4), and all the p values of Begg's tests and Egger's tests were greater than 0.05 (Table S3 in File S1), providing statistical evidence of the funnel plot's symmetry. Ultimately, the results did not suggest any evidence of publication bias.
Figure 4. Funnel plot for the association of SAD risk with ACE I/D polymorphism (allelic comparison: I vs D).
Discussion
Previous studies investigating the association between I/D polymorphism and SAD risk have provided controversial results, and most of these studies involved relatively small samples, which were difficult to assess any genetic effects reliably. Meta-analysis has been recognized as an important tool to more precisely define the effect of selected genetic polymorphism on the risk for complex disease [85]. A meta-analysis in 2005 showed that D homozygote was at reduced of AD risk [14]. However, the previous meta-analyses did not cover any studies published in Chinese, which could lead to selection bias and might bias the effect estimate of a meta-analysis. Furthermore, since 2005, sixteen new articles have been published. Hence, to provided the most comprehensive assessment of the association between I/D polymorphism and SAD risk, an updated meta-analysis of all available studies was performed. And our meta-analysis indicated that the ACE I/D polymorphism is unlikely to be a major determining factor in the development of SAD. We believed that our results have made much more powerful and detailed analyses to support our results. First, more studies were included in our meta-analysis. Second, more comprehensive subgroup analyses were conducted, and no significant associations were found when we restricted to the high quality subgroup, the large sample size subgroup and the population-based controls subgroup. Finally, to avoid false positive findings, the FPRP analyses were performed for all significant findings observed in our analyses. And none of these significant associations passed the FPRP analyses, indicating that these associations were weak.
Too many reports of associations between genetic variants and complex diseases were false positive [86]. Many false-positive results were likely to be published due to the widely used significance threshold of p<0.05. Therefore, this meta-analysis adopted FPRP analyses, which is based not only on the observed p value but also on both the statistical power and prior probability of the hypothesis, making our results more reliable [26].
Moderate heterogeneity between studies was identified for all genetic models in the overall comparisons. Common reasons of heterogeneity may include differences in the studied populations (e.g., geographic location), or in sample selection (e.g., source of controls, HWE), or in methods (e.g., genotyping methods), or it may be due to interaction with other risk factors (e.g., sample size, study quality and publication time). The meta-regression analyses indicated that the potential sources of heterogeneity for heterozygote comparison were sample size and publication time. However, the sources of heterogeneity for the other models were not found, suggesting that heterogeneity might also be explained by other confounding factors. Nevertheless, when studies were stratified by geographic location, the heterogeneity was higher in the Asian subgroup while it was decreased in other populations. It was the same with the results of Galbraith plot analyses, which spotted at least 14 studies as the outliers and 9 of these 14 studies belonged to the Asian subgroup. These two analyses provided evidence that a combination of heterogeneous studies from the Asian subgroup contributed to the moderate heterogeneity of overall analyses. However, in the Asian subgroup, meta-regression did not find any sources of heterogeneity (data not shown), suggesting that the heterogeneity in the Asian subgroup might be explained by other confounding factors. In general, more rigorous and uniform studies were required.
In the present study, results from populations with different genetic backgrounds were not the same. The combinations of the South Caucasians studies and the Asian studies showed no significant results. However, results from the North European subgroup were distinct and the pooled ACE I allele frequency of the controls showed a modest difference across ethnicities (North European studies: 46.9%; South Caucasian studies: 39.7%; Asian studies: 59.3%). These inconsistent data may be explained by the different genetic background across ethnicities. Nevertheless, owing to the greater FPRP values of significant associations in the North European subgroup, the observed ethnic difference in this meta-analysis was also likely to be caused by chance because continued reliance on the standard p value criterion of 0.05 to define statistical significance without consideration of power or prior probability may generated a fluctuated risk estimate [26]. Thus, large and carefully designed studies on ethnicity difference were also needed to provide the best evidence for these possible associations.
When studies were stratified by sample size, significant elevated SAD risks were associated with the I/D polymorphism in the small sample size subgroup. However, small sample with limited participants was often accompanied with selection biases, and lacked sufficient power to support or deny an association [87]. It was therefore speculated that the small sample size subgroup might overestimate the magnitude of association between I/D variant and SAD risk. Moreover, these significant associations in the small sample size subgroup were weak as they did not pass the FPRP analyses. Finally, when we restricted to the large sample size subgroup, no statistically significant finding was observed in any genetic models.
In the stratification analysis by source of controls, significant associations were observed using heterozygote comparison and the dominant model in the non populations-based subgroup. However, the genotype distributions in the non population-based studies may not be representative of the general population. Given the fact that these associations were not noteworthy (did not pass the FPRP analyses) and no significant association was found in the population-based studies, we thought that this significant association for the I/D variant might be a spurious finding. More and larger population-based studies were required to further clarify the association between I/D variant and SAD risk.
Despite our efforts in performing a deeper analysis, some limitations also exist in our meta-analysis. First, in most overall and subgroup analyses, moderate heterogeneity was detected and might have potential impact in the pooled results. Due to the limited information, subgroup analyses and meta regression according to other confounding factors were not performed. Second, sensitivity analysis limited to English-language studies suggested that a potential language bias was possible. However, we only included studies published in Chinese and English, more studies published in other languages should be concerned. Finally, lack of individual participants' data has restricted further adjustments by other covariables, such as APOE ε4 status, gender, etc.
In conclusion, given that all significant associations could not pass the FPRP analyses and no significant association was detected in the high quality studies, the large sample size studies and the population-based studies, we suggest that the ACE I/D polymorphism is unlikely to be a major determining factor in the development of SAD.
Supporting Information
Cumulative meta-analysis of the relation between ACE I/D polymorphism and risk of SAD (I vs D). Each study was used as an information step. The vertical dotted line is the summary odds ratio. Bars represent 95% confidence interval (CIs)
(TIF)
Galbraith plots of association between I/D polymorphism and SAD risk. Each number represents a separate study for the indicated association and the number is the number of the respective study included into the meta-analysis (shown in Table 1). (a) allelic comparison, I vs D; (b) additive model, II vs DD; (c) additive model, ID vs DD; (d) recessive model, II vs ID+DD; (e) dominant model, II+ID vs DD.
(DOC)
(1) Table S1 Scale used for quality assessment of studies of the association between ACE I/D polymorphism and SAD risk. (2) Table S2 The univariate meta-regression results of the association of the I/D polymorphism and risk of SAD. (3) Table S3 Results of Begg’s tests and Egger’s tests for overall analyses.
(DOC)
PRISMA Checklist for systematic review and meta-analysis.
(DOC)
Genetic association studies checklist.
(DOCX)
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by grants from the National Basic Research Program of China (973 Program, 2012CB720600). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Mucke L (2009) Neuroscience: Alzheimer's disease. Nature 461: 895–897. [DOI] [PubMed] [Google Scholar]
- 2. Shinohara M, Fujioka S, Murray ME, Wojtas A, Baker M, et al. (2014) Regional distribution of synaptic markers and APP correlate with distinct clinicopathological features in sporadic and familial Alzheimer's disease. Brain 137: 1533–1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thies W, Bleiler L (2013) 2013 Alzheimer's disease facts and figures. Alzheimers Dement 9: 208–245. [DOI] [PubMed] [Google Scholar]
- 4. Drzezga A, Grimmer T, Henriksen G, Muhlau M, Perneczky R, et al. (2009) Effect of APOE genotype on amyloid plaque load and gray matter volume in Alzheimer disease. Neurology 72: 1487–1494. [DOI] [PubMed] [Google Scholar]
- 5. Colton CA, Vitek MP, Wink DA, Xu Q, Cantillana V, et al. (2006) NO synthase 2 (NOS2) deletion promotes multiple pathologies in a mouse model of Alzheimer's disease. Proc Natl Acad Sci U S A 103: 12867–12872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Paula-Lima AC, Brito-Moreira J, Ferreira ST (2013) Deregulation of excitatory neurotransmission underlying synapse failure in Alzheimer's disease. J Neurochem 126: 191–202. [DOI] [PubMed] [Google Scholar]
- 7. Kehoe PG, Miners S, Love S (2009) Angiotensins in Alzheimer's disease - friend or foe? Trends Neurosci 32: 619–628. [DOI] [PubMed] [Google Scholar]
- 8. Biller H, Zissel G, Ruprecht B, Nauck M, Busse Grawitz A, et al. (2006) Genotype-corrected reference values for serum angiotensin-converting enzyme. Eur Respir J 28: 1085–1090. [DOI] [PubMed] [Google Scholar]
- 9. van Esch JH, van Gool JM, de Bruin RJ, Payne JR, Montgomery HE, et al. (2008) Different contributions of the angiotensin-converting enzyme C-domain and N-domain in subjects with the angiotensin-converting enzyme II and DD genotype. J Hypertens 26: 706–713. [DOI] [PubMed] [Google Scholar]
- 10. Wu SJ, Hsieh TJ, Kuo MC, Tsai ML, Tsai KL, et al. (2013) Functional regulation of Alu element of human angiotensin-converting enzyme gene in neuron cells. Neurobiol Aging 34: 1921.e1921–1927. [DOI] [PubMed] [Google Scholar]
- 11. Kehoe PG, Russ C, McIlory S, Williams H, Holmans P, et al. (1999) Variation in DCP1, encoding ACE, is associated with susceptibility to Alzheimer disease. Nat Genet 21: 71–72. [DOI] [PubMed] [Google Scholar]
- 12. Kehoe PG, Katzov H, Feuk L, Bennet AM, Johansson B, et al. (2003) Haplotypes extending across ACE are associated with Alzheimer's disease. Hum Mol Genet 12: 859–867. [DOI] [PubMed] [Google Scholar]
- 13. Elkins JS, Douglas VC, Johnston SC (2004) Alzheimer disease risk and genetic variation in ACE: a meta-analysis. Neurology 62: 363–368. [DOI] [PubMed] [Google Scholar]
- 14. Lehmann DJ, Cortina-Borja M, Warden DR, Smith AD, Sleegers K, et al. (2005) Large meta-analysis establishes the ACE insertion-deletion polymorphism as a marker of Alzheimer's disease. Am J Epidemiol 162: 305–317. [DOI] [PubMed] [Google Scholar]
- 15. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Thakkinstian A, McEvoy M, Minelli C, Gibson P, Hancox B, et al. (2005) Systematic review and meta-analysis of the association between {beta}2-adrenoceptor polymorphisms and asthma: a HuGE review. Am J Epidemiol 162: 201–211. [DOI] [PubMed] [Google Scholar]
- 17. Wu J, Liu J, Zhou Y, Ying J, Zou H, et al. (2012) Predictive value of XRCC1 gene polymorphisms on platinum-based chemotherapy in advanced non-small cell lung cancer patients: a systematic review and meta-analysis. Clin Cancer Res 18: 3972–3981. [DOI] [PubMed] [Google Scholar]
- 18. Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. Bmj 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. DerSimonian R, Kacker R (2007) Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials 28: 105–114. [DOI] [PubMed] [Google Scholar]
- 20. Lau J, Ioannidis JP, Schmid CH (1997) Quantitative synthesis in systematic reviews. Ann Intern Med 127: 820–826. [DOI] [PubMed] [Google Scholar]
- 21. Zintzaras E, Lau J (2008) Synthesis of genetic association studies for pertinent gene-disease associations requires appropriate methodological and statistical approaches. J Clin Epidemiol 61: 634–645. [DOI] [PubMed] [Google Scholar]
- 22. Huy NT, Thao NT, Diep DT, Kikuchi M, Zamora J, et al. (2010) Cerebrospinal fluid lactate concentration to distinguish bacterial from aseptic meningitis: a systemic review and meta-analysis. Crit Care 14: R240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Langan D, Higgins JP, Gregory W, Sutton AJ (2012) Graphical augmentations to the funnel plot assess the impact of additional evidence on a meta-analysis. J Clin Epidemiol 65: 511–519. [DOI] [PubMed] [Google Scholar]
- 24. Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. Bmj 315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50: 1088–1101. [PubMed] [Google Scholar]
- 26. Wacholder S, Chanock S, Garcia-Closas M, El Ghormli L, Rothman N (2004) Assessing the probability that a positive report is false: an approach for molecular epidemiology studies. J Natl Cancer Inst 96: 434–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Thomas DC, Clayton DG (2004) Betting odds and genetic associations. J Natl Cancer Inst 96: 421–423. [DOI] [PubMed] [Google Scholar]
- 28. Schjeide BM, McQueen MB, Mullin K, DiVito J, Hogan MF, et al. (2009) Assessment of Alzheimer's disease case-control associations using family-based methods. Neurogenetics 10: 19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zhang Z, Deng L, Yu H, Shi Y, Bai F, et al. (2012) Association of angiotensin-converting enzyme functional gene I/D polymorphism with amnestic mild cognitive impairment. Neurosci Lett. 514: 131–135. [DOI] [PubMed] [Google Scholar]
- 30. Arlt S, Demiralay C, Tharun B, Geisel O, Storm N, et al. (2013) Genetic risk factors for depression in Alzheimer’s disease patients. Curr Alzheimer Res 10: 72–81. [PubMed] [Google Scholar]
- 31. Yang YH, Liu CK (2008) Angiotensin-converting enzyme gene in Alzheimer's disease. Tohoku J Exp Med 215: 295–298. [DOI] [PubMed] [Google Scholar]
- 32. Sayed-Tabatabaei FA, Oostra BA, Isaacs A, van Duijn CM, Witteman JC (2006) ACE polymorphisms. Circ Res 98: 1123–1133. [DOI] [PubMed] [Google Scholar]
- 33. Amouyel P, Richard F, Berr C, David-Fromentin I, Helbecque N (2000) The renin angiotensin system and Alzheimer's disease. Ann N Y Acad Sci 903: 437–441. [DOI] [PubMed] [Google Scholar]
- 34. Isbir T, Agachan B, Yilmaz H, Aydin M (2000) Angiotensin converting enzyme gene polymorphism in Alzheimer's disease. Cell Biochem Funct 18: 141–142. [DOI] [PubMed] [Google Scholar]
- 35.Panza F, Solfrizzi V, D'Introno A, Capurso C, Colaiccco AM, et al.. (2002) Lack of association between ace polymorphism and Alzheimer's disease in southern Italy. Arch Gerontol Geriatr Suppl 8: 239–245. [DOI] [PubMed]
- 36. Shcherbatykh TV, Kiryanov SA, Korovaitseva GI, Selezneva ND, Voskresenskaya NI, et al. (2001) The angiotensin-converting enzyme gene as a possible risk or protective factor in Alzheimer's disease. Neurosci Behav Physiol 31: 179–181. [DOI] [PubMed] [Google Scholar]
- 37. Wakutani Y, Kowa H, Kusumi M, Yamagata K, Wada-Isoe K, et al. (2002) Genetic analysis of vascular factors in Alzheimer's disease. Ann N Y Acad Sci 977: 232–238. [DOI] [PubMed] [Google Scholar]
- 38. Vardy ER, Rice PJ, Bowie PC, Holmes JD, Catto AJ, et al. (2009) Plasma angiotensin-converting enzyme in Alzheimer's disease. J Alzheimers Dis 16: 609–618. [DOI] [PubMed] [Google Scholar]
- 39. Farrer LA, Sherbatich T, Keryanov SA, Korovaitseva GI, Rogaeva EA, et al. (2000) Association between angiotensin-converting enzyme and Alzheimer disease. Arch Neurol 57: 210–214. [DOI] [PubMed] [Google Scholar]
- 40. Richard F, Fromentin-David I, Ricolfi F, Ducimetiere P, Di Menza C, et al. (2001) The angiotensin I converting enzyme gene as a susceptibility factor for dementia. Neurology 56: 1593–1595. [DOI] [PubMed] [Google Scholar]
- 41. Seripa D, Forno GD, Matera MG, Gravina C, Margaglione M, et al. (2003) Methylenetetrahydrofolate reductase and angiotensin converting enzyme gene polymorphisms in two genetically and diagnostically distinct cohort of Alzheimer patients. Neurobiol Aging 24: 933–939. [DOI] [PubMed] [Google Scholar]
- 42. Scacchi R, De Bernardini L, Mantuano E, Vilardo T, Donini LM, et al. (1998) DNA polymorphisms of apolipoprotein B and angiotensin I-converting enzyme genes and relationships with lipid levels in Italian patients with vascular dementia or Alzheimer's disease. Dement Geriatr Cogn Disord 9: 186–190. [DOI] [PubMed] [Google Scholar]
- 43. Chapman J, Wang N, Treves TA, Korczyn AD, Bornstein NM (1998) ACE, MTHFR, factor V Leiden, and APOE polymorphisms in patients with vascular and Alzheimer's dementia. Stroke. 29: 1401–1404. [DOI] [PubMed] [Google Scholar]
- 44. Palumbo B, Cadini D, Nocentini G, Filipponi E, Fravolini ML, et al. (1999) Angiotensin converting enzyme deletion allele in different kinds of dementia disorders. Neurosci Lett 267: 97–100. [DOI] [PubMed] [Google Scholar]
- 45. Hu J, Miyatake F, Aizu Y, Nakagawa H, Nakamura S, et al. (1999) Angiotensin-converting enzyme genotype is associated with Alzheimer disease in the Japanese population. Neurosci Lett 277: 65–67. [DOI] [PubMed] [Google Scholar]
- 46. Alvarez R, Alvarez V, Lahoz CH, Martinez C, Pena J, et al. (1999) Angiotensin converting enzyme and endothelial nitric oxide synthase DNA polymorphisms and late onset Alzheimer's disease. J Neurol Neurosurg Psychiatry 67: 733–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mattila KM, Rinne JO, Roytta M, Laippala P, Pietila T, et al. (2000) Dipeptidyl carboxypeptidase 1 (DCP1) and butyrylcholinesterase (BCHE) gene interactions with the apolipoprotein E epsilon4 allele as risk factors in Alzheimer's disease and in Parkinson's disease with coexisting Alzheimer pathology. J Med Genet 37: 766–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Crawford F, Abdullah L, Schinka J, Suo Z, Gold M, et al. (2000) Gender-specific association of the angiotensin converting enzyme gene with Alzheimer's disease. Neurosci Lett 280: 215–219. [DOI] [PubMed] [Google Scholar]
- 49. Myllykangas L, Polvikoski T, Sulkava R, Verkkoniemi A, Tienari P, et al. (2000) Cardiovascular risk factors and Alzheimer's disease: a genetic association study in a population aged 85 or over. Neurosci Lett 292: 195–198. [DOI] [PubMed] [Google Scholar]
- 50. Yang JD, Feng G, Zhang J, Lin ZX, Shen T, et al. (2000) Association between angiotensin-converting enzyme gene and late onset Alzheimer's disease in Han chinese. Neurosci Lett 295: 41–44. [DOI] [PubMed] [Google Scholar]
- 51. Isbir T, Agachan B, Yilmaz H, Aydin M, Kara I, et al. (2001) Interaction between apolipoprotein-E and angiotensin-converting enzyme genotype in Alzheimer's disease. Am J Alzheimers Dis Other Demen 16: 205–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Narain Y, Yip A, Murphy T, Brayne C, Easton D, et al. (2000) The ACE gene and Alzheimer's disease susceptibility. J Med Genet 37: 695–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Zuliani G, Ble A, Zanca R, Munari MR, Zurlo A, et al. (2001) Genetic polymorphisms in older subjects with vascular or Alzheimer's dementia. Acta Neurol Scand 103: 304–308. [DOI] [PubMed] [Google Scholar]
- 54. Perry RT, Collins JS, Harrell LE, Acton RT, Go RC (2001) Investigation of association of 13 polymorphisms in eight genes in southeastern African American Alzheimer disease patients as compared to age-matched controls. Am J Med Genet 105: 332–342. [DOI] [PubMed] [Google Scholar]
- 55. Buss S, Muller-Thomsen T, Hock C, Alberici A, Binetti G, et al. (2002) No association between DCP1 genotype and late-onset Alzheimer disease. Am J Med Genet 114: 440–445. [DOI] [PubMed] [Google Scholar]
- 56. Wu C, Zhou D, Guan Z, Fan J, Qiao Y (2002) The association between angiotensin I converting enzyme gene polymorphism and Chinese late onset Alzheimer disease. Zhonghua Yi Xue Yi Chuan Xue Za Zhi 19: 401–404. [PubMed] [Google Scholar]
- 57. Lendon CL, Thaker U, Harris JM, McDonagh AM, Lambert JC, et al. (2002) The angiotensin 1-converting enzyme insertion (I)/deletion (D) polymorphism does not influence the extent of amyloid or tau pathology in patients with sporadic Alzheimer's disease. Neurosci Lett 328: 314–318. [DOI] [PubMed] [Google Scholar]
- 58. Monastero R, Caldarella R, Mannino M, Cefalu AB, Lopez G, et al. (2002) Lack of association between angiotensin converting enzyme polymorphism and sporadic Alzheimer's disease. Neurosci Lett 335: 147–149. [DOI] [PubMed] [Google Scholar]
- 59. Cheng CY, Hong CJ, Liu HC, Liu TY, Tsai SJ (2002) Study of the association between Alzheimer's disease and angiotensin-converting enzyme gene polymorphism using DNA from lymphocytes. Eur Neurol 47: 26–29. [DOI] [PubMed] [Google Scholar]
- 60. Panza F, Solfrizzi V, D'Introno A, Colacicco AM, Capurso C, et al. (2003) Shifts in angiotensin I converting enzyme insertion allele frequency across Europe: implications for Alzheimer's disease risk. J Neurol Neurosurg Psychiatry 74: 1159–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Carbonell J, Allen R, Kalsi G, McQuillin A, Livingston G, et al. (2003) Variation in the DCP1 gene, encoding the angiotensin converting enzyme ACE, is not associated with increased susceptibility to Alzheimer's disease. Psychiatr Genet 13: 47–50. [DOI] [PubMed] [Google Scholar]
- 62. Camelo D, Arboleda G, Yunis JJ, Pardo R, Arango G, et al. (2004) Angiotensin-converting enzyme and alpha-2-macroglobulin gene polymorphisms are not associated with Alzheimer's disease in Colombian patients. J Neurol Sci 218: 47–51. [DOI] [PubMed] [Google Scholar]
- 63. Chalmers KA, Culpan D, Kehoe PG, Wilcock GK, Hughes A, et al. (2004) APOE promoter, ACE1 and CYP46 polymorphisms and beta-amyloid in Alzheimer's disease. Neuroreport 15: 95–98. [DOI] [PubMed] [Google Scholar]
- 64. Feng YQ, Wang JH, Guo X, Zhao DW, Gao JS, et al. (2004) Analysis of the polymorphism of apoE gene and ACE gene in Alzheimer's disease and vascular dementia.. Chin J Geriatr Heart Brain Vessel Dis 6: 181–183. [Google Scholar]
- 65. Kolsch H, Jessen F, Freymann N, Kreis M, Hentschel F, et al. (2005) ACE I/D polymorphism is a risk factor of Alzheimer's disease but not of vascular dementia. Neurosci Lett. 377: 37–39. [DOI] [PubMed] [Google Scholar]
- 66. Zhang JW, Li XQ, Zhang ZX, Chen D, Zhao HL, et al. (2005) Association between angiotensin-converting enzyme gene polymorphism and Alzheimer's disease in a Chinese population. Dement Geriatr Cogn Disord 20: 52–56. [DOI] [PubMed] [Google Scholar]
- 67. Sleegers K, den Heijer T, van Dijk EJ, Hofman A, Bertoli-Avella AM, et al. (2005) ACE gene is associated with Alzheimer's disease and atrophy of hippocampus and amygdala. Neurobiol Aging 26: 1153–1159. [DOI] [PubMed] [Google Scholar]
- 68. Keikhaee MR, Hashemi SB, Najmabadi H, Noroozian M (2006) C677T methylentetrahydrofulate reductase and angiotensin converting enzyme gene polymorphisms in patients with Alzheimer's disease in Iranian population. Neurochem Res 31: 1079–1083. [DOI] [PubMed] [Google Scholar]
- 69. Meng Y, Baldwin CT, Bowirrat A, Waraska K, Inzelberg R, et al. (2006) Association of polymorphisms in the Angiotensin-converting enzyme gene with Alzheimer disease in an Israeli Arab community. Am J Hum Genet 78: 871–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Wehr H, Bednarska-Makaruk M, Lojkowska W, Graban A, Hoffman-Zacharska D, et al. (2006) Differences in risk factors for dementia with neurodegenerative traits and for vascular dementia. Dement Geriatr Cogn Disord 22: 1–7. [DOI] [PubMed] [Google Scholar]
- 71. Wang B, Jin F, Yang Z, Lu Z, Kan R, et al. (2006) The insertion polymorphism in angiotensin-converting enzyme gene associated with the APOE epsilon 4 allele increases the risk of late-onset Alzheimer disease. J Mol Neurosci 30: 267–271. [DOI] [PubMed] [Google Scholar]
- 72. Wang HK, Fung HC, Hsu WC, Wu YR, Lin JC, et al. (2006) Apolipoprotein E, angiotensin-converting enzyme and kallikrein gene polymorphisms and the risk of Alzheimer's disease and vascular dementia. J Neural Transm 113: 1499–1509. [DOI] [PubMed] [Google Scholar]
- 73. Nacmias B, Bagnoli S, Tedde A, Cellini E, Bessi V, et al. (2007) Angiotensin converting enzyme insertion/deletion polymorphism in sporadic and familial Alzheimer's disease and longevity. Arch Gerontol Geriatr 45: 201–206. [DOI] [PubMed] [Google Scholar]
- 74. Liu M, Zhang YD, Zhao KR, Liu Y (2007) Association of angiotensin converting enzyme activity and agiotensin converting enzyme gene polymorphism with vascular dementia and Alzheimer's disease. Chinese journal of practical internal medicine 13: 1028–1030. [Google Scholar]
- 75. Han B, Zhang SL (2008) Association of apoE gene, A2M gene and ACE gene polymorphism with Alzheimer's disease. J Shanxi Med Univ 39: 692–696. [Google Scholar]
- 76. Miners S, Ashby E, Baig S, Harrison R, Tayler H, et al. (2009) Angiotensin-converting enzyme levels and activity in Alzheimer's disease: differences in brain and CSF ACE and association with ACE1 genotypes. Am J Transl Res 1: 163–177. [PMC free article] [PubMed] [Google Scholar]
- 77. Ning M, Yang Y, Zhang Z, Chen Z, Zhao T, et al. (2010) Amyloid-beta-Related Genes SORL1 and ACE are Genetically Associated With Risk for Late-onset Alzheimer Disease in the Chinese Population. Alzheimer Dis Assoc Disord 24: 390–396. [DOI] [PubMed] [Google Scholar]
- 78. Nirmal S, Tripathi M, Shastri SS, Sagar R, S V (2011) Association of Angiotensin-converting enzyme insertion(I)/deletion (D) genotype in Alzheimer's disease patients of north Indian population. Int J Neurosci 121: 557–561. [DOI] [PubMed] [Google Scholar]
- 79. Cousin E, Mace S, Rocher C, Dib C, Muzard G, et al. (2011) No replication of genetic association between candidate polymorphisms and Alzheimer's disease. Neurobiol Aging 32: 1443–1451. [DOI] [PubMed] [Google Scholar]
- 80. Lucatelli JF, Barros AC, Silva VK, Machado Fda S, Constantin PC, et al. (2011) Genetic influences on Alzheimer's disease: evidence of interactions between the genes APOE, APOC1 and ACE in a sample population from the South of Brazil. Neurochem Res 36: 1533–1539. [DOI] [PubMed] [Google Scholar]
- 81. Yang YH, Lai CL, Tyan YC, Chou MC, Wang LC, et al. (2011) Angiotensin-converting enzyme gene and plasma protein level in Alzheimer's disease in Taiwanese. Age Ageing 40: 238–242. [DOI] [PubMed] [Google Scholar]
- 82. Zhang SP, Xuan ZB, Huang ZY, Liu YQ, Liu Q, et al. (2014) The association between angiotensin converting enzyme gene polymorphism and Alzheimer's disease in Jiamusi region. Chinese journal of tissue engineering research 18: 259–264. [Google Scholar]
- 83. Fogarty DG, Maxwell AP, Doherty CC, Hughes AE, Nevin NC (1994) ACE gene typing. Lancet 343: 851. [DOI] [PubMed] [Google Scholar]
- 84. Wang B, Huang G, Wang D, Li A, Xu Z, et al. (2010) Null genotypes of GSTM1 and GSTT1 contribute to hepatocellular carcinoma risk: evidence from an updated meta-analysis. J Hepatol 53: 508–518. [DOI] [PubMed] [Google Scholar]
- 85. Dong LM, Potter JD, White E, Ulrich CM, Cardon LR, et al. (2008) Genetic susceptibility to cancer: the role of polymorphisms in candidate genes. Jama 299: 2423–2436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Ioannidis JP, Ntzani EE, Trikalinos TA, Contopoulos-Ioannidis DG (2001) Replication validity of genetic association studies. Nat Genet 29: 306–309. [DOI] [PubMed] [Google Scholar]
- 87. Dechartres A, Trinquart L, Boutron I, Ravaud P (2013) Influence of trial sample size on treatment effect estimates: meta-epidemiological study. Bmj 346: f2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Cumulative meta-analysis of the relation between ACE I/D polymorphism and risk of SAD (I vs D). Each study was used as an information step. The vertical dotted line is the summary odds ratio. Bars represent 95% confidence interval (CIs)
(TIF)
Galbraith plots of association between I/D polymorphism and SAD risk. Each number represents a separate study for the indicated association and the number is the number of the respective study included into the meta-analysis (shown in Table 1). (a) allelic comparison, I vs D; (b) additive model, II vs DD; (c) additive model, ID vs DD; (d) recessive model, II vs ID+DD; (e) dominant model, II+ID vs DD.
(DOC)
(1) Table S1 Scale used for quality assessment of studies of the association between ACE I/D polymorphism and SAD risk. (2) Table S2 The univariate meta-regression results of the association of the I/D polymorphism and risk of SAD. (3) Table S3 Results of Begg’s tests and Egger’s tests for overall analyses.
(DOC)
PRISMA Checklist for systematic review and meta-analysis.
(DOC)
Genetic association studies checklist.
(DOCX)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.