Abstract
A patient with Candida spondylitis failed two weeks of fluconazole combined with caspofungin, and the infection relapsed despite six weeks of liposomal amphotericin B followed by two months of fluconazole. Six months therapy with high dose liposomal amphotericin B combined with flucytosine effectively cured the patient.
Keywords: Candida albicans, Spondylitis, Amphotericin B, Flucytosine, Fluconazole
Highlights
-
•
A Candida osteomyelitis case failing caspofungin+fluconazole treatment is described.
-
•
A relapse was diagnosed after ambisome followed by fluconazole therapy.
-
•
Prolonged therapy with increasing dose L-AMB and 5-FC eradicated the infection.
-
•
Further clinical studies are warranted to define optimal treatment strategies.
1. Introduction
Invasive Candida infections are becoming more prevalent, especially in the ICU. Candida was the third most common pathogen in a point prevalence study including ICU patients from 75 countries. Invasive Candida infections are associated with high mortality ranging from 40% to 60% [1]. The clinical presentations include candidemia, spondylodiscitis, endophtalmitis, chronic and acute disseminated candidiasis, endocarditis and meningitis [2,3]. Bone infections with Candida species are rare. The diagnosis is often delayed due to the rarity and diagnostic difficulties. The most common infecting species are Candida albicans, followed by Candida tropicalis and Candida glabrata [4].
Current recommendations for treatment of Candida osteomyelitis are fluconazole 6 mg/kg daily for 6–12 months, which may be preceded by liposomal amphotericin B (L-AMB) 3–5 mg/kg for at least 2 weeks [2]. The role of surgical debridement is not clear in vertebral osteomyelitis [2]. Treatment of bone infections with C. albicans is described with a high cure rate, whether treated medically or with surgery [4]. However, no randomized clinical trials on Candida bone and joint infections have been undertaken, and the management guidelines are based on case reports [3].
We report a case of C. albicans candidemia complicated by spondylitis with no effect of fluconazole combined with caspofungin and with a relapse after 6 weeks of L-AMB. Prolonged treatment (6 months) with high dose (6 mg/kg) L-AMB combined with flucytosine (5-FC) for 11 weeks cured the patient. To our knowledge, relapse of C. albicans bone infection after fluconazole combined with an echinocandin has not previously been described.
2. Case
A 32 year old pregnant woman (11 weeks), previously healthy, was hospitalized with hyperemesis. She developed sepsis and disseminated intravascular coagulation and was thus admitted to the intensive care unit (day 0). C. albicans was cultured from blood (6 positive out of 6 blood cultures) and urine. The isolate was susceptible to all antifungal agents tested. MICs were amphotericin B 0.5 mg/l and caspofungin 0.125 mg/l, both performed by E-test following the manufacturer׳s recommendations (Etest BioMerieux, France), anidulafungin 0.015 mg/l, fluconazole ≤0.125 mg/l, itraconazole ≤0.03 mg/l, micafungin ≤0.008, voriconazole ≤0.03 mg/l and 5-FC ≤0.125 mg/l using the EUCAST reference method EDef 7.2 [5]. Treatment with L-AMB (initially 4 mg/kg, subsequently 2 mg/kg due to creatinine increase to 340 µmol/l), caspofungin 70 mg and broad-spectrum antibiotics was initiated. The patient was treated with the combination for 12 days, and L-AMB and antibiotics were continued for 9 more days. On day 18, she was discharged from intensive care unit to the Department of Gynecology and Obstetrics with a fluctuating C-reactive protein (CRP) (400–600 mg/l) and a slight fever (37.8–38.2 °C). She lost her fetus, and her kidney function never recovered making her dependent on hemodialysis. On day 43, she was discharged from the hospital, with no fever, a WBC of 7.69×109 l−1 and a CRP of 188 mg/l.
A month later (day 77), she was admitted to Department of Infectious Diseases with lumbar back pain located over the lumbar spine and pyrexia. The CRP was 150 mg/l, and a bone scintigraphy on day 85 showed uptake around the right hip, left sacroiliac joint and lower spine. Magnetic resonance imaging (MRI) revealed vertebral infection at Th11–12 and L3–4 with no involvement of the discs or spinal cavity, and a fungal etiology was suspected (day 90) (Fig. 1). Treatment with caspofungin (70 mg as loading dose, subsequently 50 mg) and fluconazole (initially 200 mg daily due to kidney function, subsequently 400 mg daily) was initiated. PCR and culture from the biopsy (obtained one day after initiation of antifungal treatment) were negative. The back pain progressed during the next 14 days of treatment, the CRP was only declined from 100 to 60 mg/l and a new MRI showed no regression (day 106) (Fig. 2). The patient was considered to have a treatment failure, and treatment was changed to L-AMB 4 mg/kg/day. The patient slowly improved during six weeks of treatment. When discharged on day 148, she was asymptomatic and with normal CRP (<8 mg/l). She was continuously in hemodialysis (HD) three times a week, and during the following two months, 600 mg of fluconazole was administered after each HD. The serum fluconazole concentration was measured to 9 mg/L, which is considered therapeutic level.
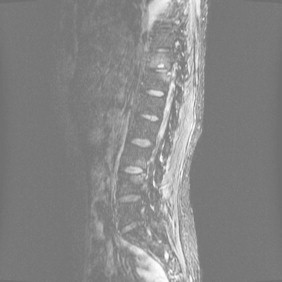
Fig. 1.

Day 90. MRI showed vertebral infection at Th11–12 and L3–4 with no involvement of the discs or spinal cavity.
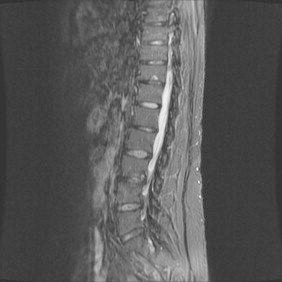
Fig. 2.
Day 106. MRI showed no regression on caspofungin and fluconazole.
Two weeks after the last dose of fluconazole (day 233), the patient experienced malaise, vomiting, fluctuating temperature (37–38 °C) and low back pain radiating to right hip. After another two weeks (day 247), she was readmitted to hospital with increasing back pain and pyrexia (39.5 °C). CRP was <8 mg/l, increasing in one day to 80 mg/l, and erythrocyte sedimentation rate (ESR) was 50 (normal <20 mm hour). L-AMB 4 mg/kg daily was initiated on day 252 and led to temporal relief of her symptoms. After four weeks of treatment, the pain returned and increased, and the L-AMB dose was increased to 5 mg/kg a day. MRI showed progression of the L3–4 destruction (day 293) (Fig. 3). On day 301, L-AMB dose was increased to 6 mg/kg and combined with 5-FC (3500 mg, corresponding to approx. 50 mg/kg) after each HD (3/week) for 11 weeks (from day 301 to day 378). When 5-FC treatment was discontinued, the PET-CT was unchanged, MRI showed minimal regression, but a bone scintigraphy showed regression of the Th12-L1 uptake (Fig. 4). High dose L-AMB (6 mg/kg) was continued for 3 more months until day 465 (a total period of 6 months). At this time, leukocyte scintigraphy as well as MRI showed further reduced enhancement and edema of L3–4 (Fig. 5). Life-long prophylaxis was discussed for this patient. She was considered for a kidney transplant requiring full clearance of the fungal infection proven before transplantation. Hence all anti-fungal treatment was discontinued on day 465.
Fig. 3.

Day 293. MRI showed relapse of spondylitis in L3–4 after six weeks of liposomal amphotericin and two months of fluconazole.
Fig. 4.

Day 357. MRI showed minimal regression after 8 weeks of high-dose liposomal amphotericin combined with flucytosine (MRI after 11 weeks was not available).
Fig. 5.
Day 465. MRI showed reduced enhancement and edema of L3–4.
Three months later, ESR remained normal; bone scintigraphy showed minimal activity, and no progression was detected on MRI. She successfully received a family donor kidney transplant six months after her anti-fungal treatment was terminated (day 678) (Fig. 6), gave birth to a healthy child two years after transplant and has now been without signs of relapse for 5 years (Fig. 7).
Fig. 6.

Day 714, five weeks after kidney transplant. No progression was detected on MRI.
Fig. 7.

Day 1762. No sign of progression on MRI three and a half years after termination of antifungal treatment.
3. Discussion
Candida spondylitis is rare, and most cases have been reported in adults. The most frequent symptom is localized pain [4]. Rapid diagnosis and treatment is important in order to prevent vertebral collapse [6]. Risk factors for candidaemia have been identified; critical illness with a prolonged stay at the ICU, abdominal surgery, low birth weight, acute necrotizing pancreatitis, malignant disease, organ transplantation, Candida colonization, treatment with broad-spectrum antibiotics, central venous catheter, receipt of parental nutrition, HD, burns and neutropenia/immunosuppression [4,7]. For the vertebral infection with Candida, the most frequent risk factors are central venous catheter and antibiotic treatment [4]. Prior to the candidemia and the bone infection, the patient was treated in an ICU with broad-spectrum antibiotics, received HD and had a central intravascular catheter.
For candidemia, the use of an echinocandin and removal of central venous lines were significantly associated with improved outcome in a recent quantitative review of randomized trials [8] but this case clearly demonstrates that the combination of caspofungin and fluconazole was not effective. A case report has described failure of fluconazole monotherapy in sternal osteomyelitis, subsequently cured with amphotericin B, but there was no information regarding the susceptibility of the C. albicans isolates [9]. The C. albicans in the blood cultures from our patient was susceptible to all antifungal agents, and the Candida septicemia resolved on 2 mg/kg liposomal amphotericin B, a low dose according to current guidelines [2,3]. One month later, the Candida spondylitis was diagnosed. It is uncertain whether a higher dose or longer treatment with amphotericin B could have prevented this. According to recent guidelines, the appropriate treatment would have been fluconazole 6 mg/kg for 6–12 months possibly preceded by L-AMB 3–5 mg/kg for at least two weeks [2,3]. Hence, according to today׳s recommendations, the fluconazole duration (two months) was suboptimal which may have contributed to the unsuccessful outcome. A review of 53 cases of osteomyelitis reported a mean treatment duration of only 54.9 days [10]. Relapse after 12 weeks follow-up was unknown. Pharmacokinetic/pharmacodynamic animal models suggest that the combination of amphotericin B and 5-FC has an additive effect when treating disseminated candidiasis [11]. The additive fungicidal effect of 5-FC was neglectable when the amphotericin B dose was high. Furthermore, short course treatment with L-AMB has shown to be effective in a few cases [12], suggesting that this drug may be superior in bone infections. A combination of 5-FC and fluconazole successfully treated a case of Candida discitis [13]. 5-FC has great penetrance due to its small size and is thus recommended in combination with amphotericin B for treatment of Candida endocarditis, Candida CNS-infections and ocular candidiasis [2,3]. However, 5-FC is not included as recommended treatment of osteomyelitis in current guidelines [2,3]. Further studies are needed in order to determine the role of this drug in the therapy of Candida osteomyelitis.
In conclusion, although it is not possible to determine whether it was the increased dose, prolonged therapy of L-AMB or the addition of 5-FC that finally resulted in eradication of the infection, it is likely that the combination of the three factors played in concert. In cases with a relapse of Candida osteomyelitis, prolonged therapy with high dose L-AMB combined with 5-FC seems to be an effective treatment option.
Conflict of interest statement
None related to this particular work, but outside this Maiken Cavling Arendrup has the following disclosures: MCA has received research grants and served on the speakers board for Astellas Pharma US, Gilead Sciences, MSD and Pfizer, and been a consultant for Gilead, MSD and Pcovery.
Acknowledgments
The authors wish to thank Birgit Brandt for excellent technical assistance.
References
- 1.Delaloye J., Calandra T. Invasive candidiasis as a cause of sepsis in the critically ill patient. Virulence. 2013;5(1):161–169. doi: 10.4161/viru.26187. (PubMed PMID: 24157707) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pappas P.G., Kauffman C.A., Andes D., Benjamin D.K., Jr., Calandra T.F., Edwards J.E., Jr. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis: Off Publ Infect Dis Soc Am. 2009;48(5):503–535. doi: 10.1086/596757. (PubMed PMID: 19191635) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cornely O.A., Bassetti M., Calandra T., Garbino J., Kullberg B.J., Lortholary O. ESCMID* guideline for the diagnosis and management of Candida diseases 2012: non-neutropenic adult patients. Clin Microbiol Infect: Off Publ Eur Soc Clin Microbiol Infect Dis. 2012;(Suppl. 7):S19–S37. doi: 10.1111/1469-0691.12039. (PubMed PMID: 23137135) [DOI] [PubMed] [Google Scholar]
- 4.Gamaletsou M.N., Kontoyiannis D.P., Sipsas N.V., Moriyama B., Alexander E., Roilides E. Candida osteomyelitis: analysis of 207 pediatric and adult cases (1970–2011) Clin Infect Dis: Off Publ Infect Dis Soc Am. 2012;55(10):1338–1351. doi: 10.1093/cid/cis660. (PubMed PMID: 22911646) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arendrup M.C., Cuenca-Estrella M., Lass-Florl C., Hope W., Eucast A. EUCAST technical note on the EUCAST definitive document EDef 7.2: method for the determination of broth dilution minimum inhibitory concentrations of antifungal agents for yeasts EDef 7.2 (EUCAST-AFST) Clin Microbiol Infect: Off Publ Eur Soc Clin Microbiol Infect Dis. 2012;18(7):E246–E247. doi: 10.1111/j.1469-0691.2012.03880.x. (PubMed PMID: 22563750) [DOI] [PubMed] [Google Scholar]
- 6.Khazim R.M., Debnath U.K., Fares Y. Candida albicans osteomyelitis of the spine: progressive clinical and radiological features and surgical management in three cases. Eur Spine J: Off Publ Eur Spine Soc, Eur Spinal Deform Soc, Eur Sect Cervical Spine Res Soc. 2006;15(9):1404–1410. doi: 10.1007/s00586-005-0038-z. (PubMed PMID: 16429290) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arendrup M.C., Sulim S., Holm A., Nielsen L., Nielsen S.D., Knudsen J.D. Diagnostic issues, clinical characteristics, and outcomes for patients with fungemia. J Clin Microbiol. 2011;49(9):3300–3308. doi: 10.1128/JCM.00179-11. (PubMed PMID: 21715585) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andes D.R., Safdar N., Baddley J.W., Playford G., Reboli A.C., Rex J.H. Impact of treatment strategy on outcomes in patients with candidemia and other forms of invasive candidiasis: a patient-level quantitative review of randomized trials. Clin Infect Dis: Off Publ Infect Dis Soc Am. 2012;54(8):1110–1122. doi: 10.1093/cid/cis021. (PubMed PMID: 22412055) [DOI] [PubMed] [Google Scholar]
- 9.Dan M., Priel I. Failure of fluconazole therapy for sternal osteomyelitis due to Candida albicans. Clin Infect Dis: Off Publ Infect Dis Soc Am. 1994;18(1):126–127. doi: 10.1093/clinids/18.1.126. (PubMed PMID: 8054430) [DOI] [PubMed] [Google Scholar]
- 10.Neofytos D., Huprikar S., Reboli A., Schuster M., Azie N., Franks B. Treatment and outcomes of Candida osteomyelitis: review of 53 cases from the PATH Alliance(R) registry. Eur J Clin Microbiol Infect Dis: Off Publ Eur Soc Clin Microbiol. 2014;33(1):135–141. doi: 10.1007/s10096-013-1939-0. (PubMed PMID: 23907587) [DOI] [PubMed] [Google Scholar]
- 11.Hope W.W., Warn P.A., Sharp A., Reed P., Keevil B., Louie A. Optimization of the dosage of flucytosine in combination with amphotericin B for disseminated candidiasis: a pharmacodynamic rationale for reduced dosing. Antimicrob Agents Chemother. 2007;51(10):3760–3762. doi: 10.1128/AAC.00488-07. (PubMed PMID: 17682101) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cone L.A., Byrd R.G., Potts B.E., Wuesthoff M. Diagnosis and treatment of Candida vertebral osteomyelitis: clinical experience with a short course therapy of amphotericin B lipid complex. Surg Neurol. 2004;62(3):234–237. doi: 10.1016/j.surneu.2003.11.018. (discussion 7, PubMed PMID: 15336867) [DOI] [PubMed] [Google Scholar]
- 13.Rachapalli S.M., Malaiya R., Mohd T.A., Hughes R.A. Successful treatment of Candida discitis with 5-flucytosine and fluconazole. Rheumatol Int. 2010;30(11):1543–1544. doi: 10.1007/s00296-009-1215-x. (PubMed PMID: 19859714) [DOI] [PubMed] [Google Scholar]


