Abstract
Background:
The area of e-Health is broad and has an excellent growth potential. An increasing number of experts believe that e-Health will fuel the next breakthroughs in health system improvements throughout the world, but there is frequent evidence of unsustainable use of e-Health systems in medical centres, particularly hospitals, for different reasons in different countries. Iran is also a developing country which is presently adopting this promising technology for its traditional healthcare delivery but there is not much information about the use of e-Health systems in its hospitals, and the weakness and opportunities of utilization of such Hospital Information Systems (HIS).
Methods:
For this research, a number of Hospitals from Isfahan, Iran, are selected using convenient sampling. E-health research professionals went there to observe their HIS and collect required data as a qualitative survey. The design of interview questions was based on the researchers’ experiences and knowledge in this area along with elementary interviews with experts on HIS utilization in hospitals.
Results:
Efficient administration of e-health implementation improves the quality of healthcare, reduces costs and medical errors, makes healthcare resources available to rural areas, etc. However, there are numerous issues affecting the successful utilization of e-health in Hospitals, such as a lack of a perfect HIS implementation plan and well-defined strategy, inadequate IT-security for the protection of e-health-related data, improper training and educational issues, legal challenges, privacy concerns, improper documentation of lessons learned, resistance to the application of new technologies, and finally a lack of recovery plan and disaster management. These results along with some informative stories are extracted from interview sessions to uncover associated challenges of HIS utilization in Iranian hospitals.
Conclusion:
The utilization of e-health in Iranian hospitals, particularly those in Isfahan, is subject to several challenges and there is no proper long-term strategy plans for HIS initiation, development, and improvement in Iranian hospitals. In order to address these problems, six recommendations are provided. Hence, human resource and e-health professionals from third party consultancy companies along with medical university scholars have to assist such hospitals to undertake the proposed solutions in order to provide proper plans to overcome future challenges and have a mature HIS in accordance with expected HIS utilization from hospitals and medical universities.
Keywords: Hospital Information System, HIS, E-health, Hospital, Case Study Survey, Iran
1. INTRODUCTION
Computerization of medical information was introduced about 30 years ago (1) under different names such as electronic medical records, health informatics, health information systems, health information technologies, or medical informatics, emphasizing the intersection of several fields including information science, computer science, healthcare, and business. Hereafter, all of these terms will be called e-Health. It is considered a type of service in quality improvement and aims to improve the efficiency and effectiveness of healthcare delivery (2). As yet, there is no universal definitions for e-Health (3, 4), but one of the most comprehensive definitions refers to e-Health as the cost-effective and secure use of Information and Communications Technology (ICT) in support of health and health-related fields, including healthcare services, health surveillance, health literature, and health education, knowledge, and research (5).
The increasing use of e-Health provides a wide range of benefits that this promising technology has for healthcare and can be categorized into six different areas namely clinical, economic, organizational, patient-related, professional, and technical issues (6). Furthermore, these areas can be divided into more detailed motivation drivers, like reduction of operational costs (7-14), improvement of healthcare delivery and administration (8, 11, 15), improvement of healthcare quality (9, 11, 12, 16, 17, 18), reduction of medical errors (11, 13, 19), provision of healthcare resources to rural areas (11, 12, 20), improvement of ethics through privacy issues (21), utilization of e-learning and education (21) , improvement of healthcare equity (16, 22), improvement of patients’ and their families’ awareness (17, 18, 23), enterprise-wide integration of systems (12), improvement of time and workflow efficiency (24, 25), fraud prevention, and citizens’ privacy protection (7).
In spite of promising advantages of e-Health, it is the least developed e-technology (26) compared to other fields such as e-commerce and e-banking. However, there is evidence that largely point to failures or unsustainable e-Health utilization in different countries (27, 28) for different reasons, such as a lack of standardization of e-Health applications (8), cost of such systems (29, 30), costs of training (30), and the diversity of platforms resulting in technical difficulties (31, 32).
The utilization of e-Health systems in hospital also has barriers and obstacles. It should be highlighted that hospitals represent essential components of healthcare systems (33) and are one of the main targets of governments to implement e-Health applications. The applications that are provided through e-Health initiatives within hospitals include Hospital Management Information Systems (HMIS), telemedicine services, and Internet services (34), which are collectively known as HIS. The importance of HIS becomes clear when the great complexity of the nature of medical practice and the large number of interventions that each patient receives cause a high rate of errors in healthcare organizations (35). It is believed that the use of HIS in hospitals is driven by the needs to reduce medical errors (36, 39, 40) and healthcare costs (31). Nevertheless, the challenges associated with the use of such systems in the hospitals worldwide are due to their content complexity, availability of standards for the integration of various work flows, communication of databases, and people involved (17), but Jaana, Paré, and Sicotte (33) believe that hospitals are continually exploring opportunities for investing in IT to improve efficiency, promote patient safety, and provide better-quality care (39). Currently, IT priorities are mostly related to reducing medical errors, upgrading/replacing inpatient clinical systems, and implementing Electronic Medical Records (EMRs) (40).
On the other hand, e-Health in Iran dates back to the time medical laboratories started to auto-analyze medical kits and print out the results for the patients. Back then, the first domestic software package covering patient registration to discharge were developed and used in several hospitals. Later, the Social Security Organization started to equip its own medical centers with informatics equipment, and HL7 as well as Electronic Data Interchange For Administration, Commerce and Transport standards introduced into Iranian healthcare sectors. In the 2000s, several different plans were initiated, including open-source standard customization based on Iranian domestic healthcare needs, the strategic plan of the National Health ICT agency (locally it is named the TAKFAB plan), development and distribution of a specific software application for cancer records in the hospitals, and finally pharmacies’ mechanization. In this decade also some pilot and small-scale e-Health projects were initiated, and the ICD-10 standard was introduced into hospitals to record patients’ information. Iranian hospitals were equipped with communication infrastructure and hardware, and HIS were being used. The latest efforts in this area in Iran by the Ministry of Health and Medical Education are electronic health records (EHRs) definition clarification, integration of several different hospitals with different hospital information systems, and development of the SEPAS (meaning Thanks in Iranian) plan, which is a long-term plan to gather and record health-related information of all citizens but isstill in the initial stage.
Nevertheless, the main aim of this article is to clarify challenges associated with e-Health systems’ utilization in Iranian hospitals on the basis of the example of Isfahan as one of the most advanced medical cities in Iran, and provide some solutions to mitigate them.
2. RESEARCH SETTING AND METHODS
This section describes the research setting and research method adopted. Different enterprise hospitals having 100 up to 1020 beds which are active in the city of Isfahan were enlisted to approach HIS-related issues using convenience sampling. The selection of 7 hospitals out of 34 ones active in this zone ensured the appropriate population and sampling method. All of these hospital cases are instructional hospitals and under the administration of Isfahan University of Medical Sciences. The reason why this zone is selected is the accessibility of data in these hospitals due to their being under the administration of Isfahan University of Medical Sciences. Each hospital is well-known in at least one specific area of expertise. For example,hospital B was known for its experts in Orthopaedics and Neurology, hospital F is more famous for its Ophthalmologists, and hospital A is well-known in almost all areas.
In these seven cases, what was interesting was the way IT departments were called. Almost all these cases, except one, have brought a vendor software developer to customize its application for them. Nevertheless, each hospital authority has decided to buy its own preferred e-Health application from vendors which has resulted in different applications running in these hospitals, except in two cases that used the same HIS application. It is note worthy that these hospitals are under the administration of the medical university, and authorities of this university have to select appropriate e-Health applications for them. However, different preferences have made the hospitals buy different HIS and as a result they cannot communicate together because of different data standard formats.
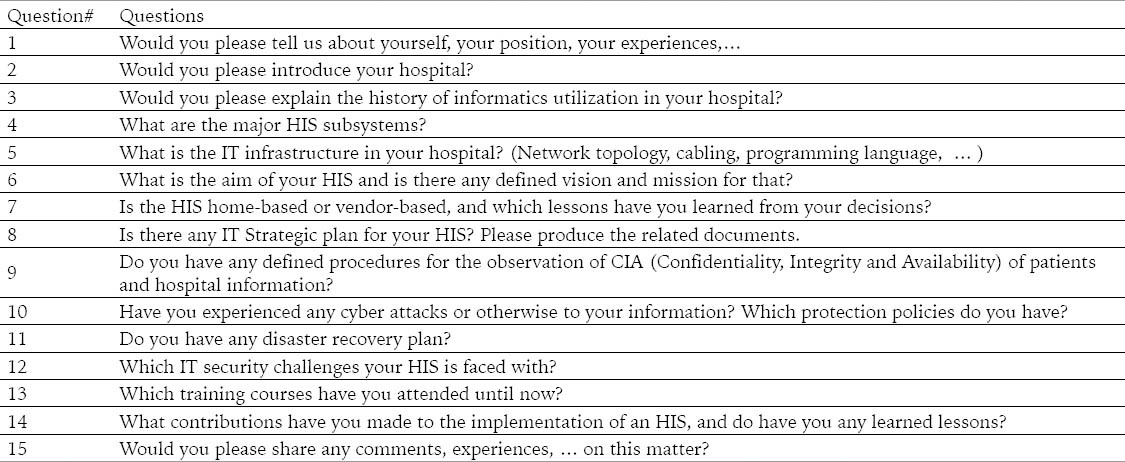
However, the team of interviewers, who were at the same time professionals and lecturers in e-Health, clarified the scope, aim, and methodology of this research. The researchers were experienced enough to ask their questions in different ways to reach the main points and facts of HIS implementation and utilization in these hospitals. Having enough information within the context of HIS in hospitals enabled the preparation of in-depth questions to be asked during interview sessions, and the same questions were delivered to be asked from hospital authorities, particularly Computer units and Information departments. A set of these questions is provided in the Table 1. The objective of these questions was to uncover and extract participants’ information around all aspects of HIS in these hospitals.
Table 1.
Frequently asked questions during interview sessions
The groups being interviewed in these hospitals were IT staff who were working in computer units/departments/centers of these hospitals and who had enough information about all aspects of e-Health applications, particularly through their experiences in these hospitals. The above mentioned criteria were the major factors to select appropriate candidate for interview. All of the selected interviews were experts with several years of experiences in their professional fields. They were normally working in IT or Computer departments/ units and were mature in their responsibilities. The interview with more than twenty experts in these hospitals clarified all aspects of this research and let to capture required information on this matter.
The exploratory approach was used in an attempt to understand the meaning of e-Health from IT staff’ point of view in the respective hospitals to ensure the validity of answers. However, the main aim of these interviews was to capture the coverage, challenges, and lessons learned from the utilization of HIS in hospitals prior to acquiring information about their e-Health strategy and security in these hospitals.
Finally it should be mentioned that the meeting sessions were scheduled and held several times and lasted between 30 to 96 minutes to reach needed results and insure that an adequate amount of information was obtained. This phase lasted four months, beginning from March 2012. Then, the process continued to analyze collected data via a descriptive approach. Although there is sophisticated software readily available which can analyze input voice responses and extract expected phrases and expressions, they may miss some important data, particularly informative stories. Thus, the researchers elected not to use such technologies, met together, and analyzed and categorized the acquired data. This approach was beneficial and powerful, but time-consuming to reach expected outcomes. This phase continued until January 2013.
3. RESULTS
3.1. Hospital A: A Multi-Purpose Hospital
This hospital is the biggest and the most sophisticated hospital in the region in terms of the number of beds and different services provided. More than 20 years of working experience led to having some of the most famous medical professionals in different areas. MRI, CT-Scan (different models), ERCP, etc. are some of the equipment being used in this medical center to serve more than 4700 patients admitted to this hospital per month. Having all specialty and super specialty wards has made this hospital a hub for people in the state and even neighboring ones.
The application and usage of informatics in this hospital dates backs to the time this hospital was opened, as some equipment were able to print out and save out data on cartexes and tapes but no integrated and unique HIS were being used until 5 years ago when a self-developed HIS was utilized within all wards, labs, centers, and departments aiming to increase the efficiency and productivity of staff and equipment, smooth the work flows, enhance data quality, and improve the satisfaction of patients. This HIS, which is able to analyze and categorize collected data, is a typical Decision Support System(DSS) to support management board in this hospital and produce required reports for different stakeholders.
The HIS in this hospital is developed with Delphi software and uses MS-SQL server as the repository for medical and none-medical data. The network topology in this hospital is star and different types of physical communication platforms, mostly optic fiber and Cat 7 cables, are used for communication between different equipment and repositories such as PACS (Picture Archiving and Communication System), etc. Nevertheless, this HIS is not adapted to any standard such as HL7 aimed to enable communication with neighbors or other HIS in different hospitals. Moreover, there are no specific strategies for HIS long-term utilization, but recently some steps have been taken to prepare such strategy plans.
In terms of security issues, all systems are port protected and no one can access USB ports of system. In addition, no data or additional file could be saved on the system as a PC restart will restore all settings to default, and users’ data and files will be eliminated. Thus, no serious virus attacks were reported and the HIS administrators have not decided to install any antivirus software on user’s PCs,just on the hospital unique server. The hospital authorities also conduct regular crisis meetings to be proactive prior to potential threats, both information technology and non-information technology problems,at any time.
3.2. Hospital B: A Hospital specialized in Orthopedics and Neurology
This hospital is one of the oldest hospitals in Isfahan, providing different medical services in 18 different clinical units, but the most famous wards are Orthopedics and Neurology well-known in the region. It is equipped with several medical devices such as CT-SCAN, ECG, EEG, EMG, etc., aimed to give sophisticated services to patients.
This hospital has experienced three periods of using IT systems. During the first, some isolated applications were used to print out different laboratory results and some simple reports. There was no network infrastructure but some islanded DOS-based systems were producing some different medical results. Later, one of the laboratory technicians started to develop an in-house application to support all hospital laboratories with more capabilities almost 10 years ago. This application was developed on the basis of an analysis of users’ requirements, and most of users were happy with that. However, for every required change, the technician (application developer) had to change the source directly and then update the application again. Although this application was a unified tool to connect and manage all data in the whole organization of the hospital, it had an elementary basic structure. It was not able to support management decisions and prepare different reports. Thus, it could not be addressed as an HIS. Moreover, once the technician left the hospital no one could update the tool and the related service support.
Having this experience made the hospital authorities think seriously, as they understood the importance of HIS without which created a bottleneck for their hospital. They preferred to buy an HIS system. So, they consulted with experts and implemented required infrastructure, especially a high capacity network with star topology. The new HIS replaced the old one 2 years ago. Now, the authorities are satisfied with the new HIS as it satisfies almost all their requirements, such as a DSS; financial, reception, and patient medical document support in compliance with International Classification of Diseases (ICD)-10; communication with the PACS system; nurses’ observing patient’s results without physically attending laboratories, and so forth. This 3-tier application-which aims to minimize communication between server and user’s PCs-smoothes all activities and steps from reception (to register patient’s data) through all wards, pharmacy, and other laboratory results, to the end of process where the patient’s financial information is ready to be announced and printed out for that patient.
Currently, this hospital has no e-Health strategy and the management board has not considered future needs and plans. The Computer Site staff are only working to manage daily needs of the hospital and are mostly reactive to IT requirements of the users. Moreover, the HIS system has been attacked by different viruses previously, and they are using network antivirus software to protect their valuable data. However, hackers are still able to attack their system and manipulate or broadcast the patients’ data without prior permission. In addition, there are no IT security protection mechanisms and the staff are not familiar with IT security standards such as ISO/IEC 27001. Although the crisis committee holds regular meetings, the IT and non-IT staff are not familiar with its importance.
3.3. Hospital C: A Hospital specialized in Urology
This hospital is one of the oldest hospitals in the region with more than 92 years of service to patients. Neurology and Renal Transplantation, Hemodialysis, and Peritoneal Dialysis are major services of this hospital, making it renowned as a hub in this specific area of expertise. The Spirometry, Muscle tape (EMG), Electroencephalography (EEG), Electrocardiography (ECG), and Electroconvulsive Therapy (ECT) are some services provided in this hospital as well.
This hospital’s almost 100 years of experience demonstrates the whole process of informatics development from the beginning. The first tapes and Indexes were used in this hospital and then an isolated DOS based system was installed to facilitate reception and financial services. However, the new HIS system was ordered by medical university and a vendor from Tehran installed a network-based application to integrate, to among all areas of the hospital; wards,pharmacy, reception, financial departments. This HIS is developed with Delphi software, uses an SQL database, and runs on star topology network platform.
However, the major HIS-related issues in this hospital could be listed as follows:
The hospital has no e-Health strategies.
The vendor is far from them and it takes some time to update their system on the basis of their needs.
IT authorities have experienced several virus attacks which infected even their server.
The selection of the big bang approach to implement the new HIS stimulated some major resistance from staff, particularly seniors.
Nevertheless, the hospital has regular crisis meeting, but the role of IT is not considered important in this hospital and there is no plan for IT security protection such as ISO/IEC 27001. Moreover, the users and server are only using a password method to protect their systems and data,and there are not applied any data encryption methods.
3.4. Hospital D: A Hospital specialized in Disaster and Burn
This hospital is considered a hub for burn patients from south, west and center of the country, and more than 2300 patients are accepted per year. Having six different wards, including separate children’s, females’, and males’ burn wards, along with the plastic and reconstructive surgery one has made a sophisticated hospital for patients in a major part of the country.
Having such an important position would require a mature infrastructure and perfect human resource to prepare and manage information systems, but only limited equipment and one IT expert is available to manage this vital part of hospital. Some major challenges of the HIS in this hospital are thus:
An inadequate server is installed with poor equipment to serve users and patients.
No external access is available for stakeholders due to inadequate information security protection mechanisms in place,and virus attacks which were experienced before. For example, this hospital has experienced USB ports abuses like other hospitals in the region and the authorities have also experienced an occurrence of server shutdown before due to hardware failure which stopped all related activities for a while.
No secondary servers are still available and the same terrible occurrences are still likely.
Application change due to different requests received from users and insurance companies is a common activity in the Computer Center Office but the vendor is far from the hospital and simple changes in the HIS needs take almost one month to occur.
This hospital suffers from a lack of any well-defined missions and visions, and there are no IT strategic plans to determine the long-term IT utilization in this hospital. The staff are not kept up-to-date with the new technologies and IT is considered a supportive rather than a strategic component of this hospital. Thus, user’s resistance to use the HIS and to buy expensive hardware and equipment due to a lack of awareness of the importance of this technology are always matters to discuss about with users and management board of the hospital.
3.5. Hospital E: A Hospital specialized in Cardiovascular Diseases
This is the most famous hospital in terms of cardiovascular diseases in the region, and Transposition of the Great Arteries (TGA), Truncus Arterious and Heart Transplant are common surgeries in this hospital.
This hospital is using a new HIS installed three years ago and the vendor is a company far from the location. The distance between the vendor and hospital has imposed some limitations and problems on users. For example, having major requests to change the HIS has produced only one version update till now. Moreover, the vendor has installed the new HIS and few instructional workshops are held. Thus, users,who are mostly nurses, were confused with the new HIS, along with some resistance and then complaints followed. To overcome those issues during HIS initiation, the IT department had to stay in the hospital for 24 hours and it took almost 5 days to mitigate the emerging challenges. Once users became comfortable with the new HIS, and some useful changes were made in the new system to satisfy users, the HIS was accepted as a part of hospital system and no longer were complaints received.
The infrastructure of this hospital is more complete compared to some other hospitals. The HIS is using one main server and another back-up server to save data. The star topology which is a typical type of networking topology is installed in this hospital, and different subsystems and users can communicate via cable media, but the media does not have a high-enough capacity to convey video and high capacity messages.
This hospital has no IT strategic plans and there are no independent committees to manage IT-related activities to mitigate or eliminate the challenges. The security issues such as virus attacks are reported but no major problems arose. The USB ports are blocked but hospital’s critical data are still at risk.
3.6. Hospital F: A Hospital specialized in Ophthalmology
This hospital was built almost 80 years ago to serve particularly eye patients. Electroretinogram (ERG) and other sophisticated equipment of this hospital have made it a centre to serve 800 patients per day. Yet, only two people are active in the Informatics Unit, one technician and one bachelor degree expert.
The new HIS system was installed almost two years ago and the vendor is from the same city. The possibility to communicate more frequently with vendor has led to updating and making changes quickly in the HIS as required and the staff were so happy with the support received. Also, the staff were trained before and after HIS installation,enabling them to utilize the HIS as quickly as possible.
One major issue is a lack of an IT strategy in this hospital,but the authorities have plans to prepare one. Another issue is IT security worries and a lack of any proper approaches to prevent virus attacks as well as other possible abuses. However, the new HIS system has automated several different work flows in the hospital and users can easily work with that. They also are pleased to work with an improved HIS with high-level support.
3.7. Hospital G: A Gynecological Hospital
This hospital is only serving women with female nurses and medical and non-medical staff who are working in Oncology, Internal Medicine, Infectious Diseases, General Surgery, Urology, Rheumatology, Orthopedics, Ophthalmology, and Dermatology wards. Around 300 receptions per day highlight the importance of this hospital as the unique hospital with this specification in the region.
The Informatics Unit is operating with only one staff, showing the improper attention to IT aspect of hospital services, and the HIS was bought 6 years ago from a vendor far from the hospital. The problem of distance between customer (hospital) and vendor is found again in this hospital. Also HIT committee is holding regular meetings every three to four months to decide on IT matters in the hospital.
Also this hospital has no proper IT strategies or security plans, but has implemented ISO 9000 before. Based on this standard some documents are prepared which are able to support parts of HIS work flows in the hospital and clarify the rules and responsibilities of Informatics Unit and related staff.
4. DISCUSSION, CONCLUSIONS, AND FUTURE WORK
As stated before, e-Health is a cost-effective and secure application of ICT in support of health and health-related fields, but it suffers from several shortcomings during its utilization in healthcare organizations, including a lack of a clear definition of e-Health as well as ambiguous plans to pursue the effective application of e-Health systems in medical care centers, particularly hospitals. Nevertheless, this paper is based on a review of e-Health situation, coverage, and strategy in different hospital cases. The advantage of the selection of different case studies with different e-Health applications and HIS was to have a multidimensional viewpoint toward e-Health coverage, situation, and strategy in Iranian hospitals.
It is believed that, e-Health has excellent potential to grow in the future as it will fuel breakthroughs via the improvement of efficiency and effectiveness of healthcare delivery in medical sectors. Despite the advantages of e-Health applications such as enhanced patient access to better healthcare, reduced total healthcare costs, and higher overall quality of healthcare delivery in different areas such as clinical, economic, organizational, patient-related, professional, technical issues, etc., e-Health remains the least developed e-technology compared to other e-technologies because of several challenges mentioned above.
Iran is a developing country that has national plans such as TAKFAB and SEPAS as well as organizational e-Health projects such as HISs in hospitals where they have been implemented or are under development. The findings of this study emphasize that almost all of these mentioned hospital case studies do not have any e-Health development strategies at all. Nevertheless, the challenges of e-Health utilization in Iran relates to some fundamental issues, primarily a lack of e-Health strategy for HIS development, standardization of e-Health applications and also improper privacy and security mechanisms. Moreover, improper management support and technical administration and also resistance to change along with improper vendor selection are major barriers to utilize e-Health concept and HIS in Iranian hospitals. Finally, the administration of medical university has no proper knowledge about management and sharing systems to save and deliver those informative lessons learned. Thus, one major mistake such as selection of vendors with no perfect support has happened several times and this sub-story can recur.
However considering these barriers, the best propositions for these challenges are presented to provide long-term successful HIS utilization in Iranian hospitals. These solutions within six general areas are proposed to mitigate or remove these indefinite challenges:
Hospitals in Iran are administrated by both Ministry of Healthcare and Medical Education, and Ministry of National Welfare. It is known that the hospitals under the administration of Ministry and Healthcare and Medical education are developing their HIS without any well-defined approaches. It is observed that in some hospital HIS are selected on the basis of observation and analysis of different available HIS proposed by different vendors in the country and they have not paid attention to the optimal requirements of their hospital needs. Thus, the ministry should manage teams of experts with previous experience aimed to first define a clear IT strategy on this matter for HIS in the hospitals, and then collect general e-Health requirements of hospitals and define a clear strategy to select vendors to propose their HIS according to hospital needs. Moreover, vendors have to support their applications fully as all hospital cases with outsourced HIS faced supplementary issues on the vendors’ part. Those vendors which are far from hospitals have to open an office nearby or inside the hospitals. It may not be cost-effective but a lack of such supports has caused major detriment to hospitals and patients. It may be better to select the same vendor for more than one hospital to solve this problem and automatically solve the problem of different standard formats as well.
All interviewers had experienced the negative effects of isolated systems which caused duplication of data entry, patient’s dissatisfaction with the system, several discounts from multiple different services, but even in some cases more than total costs. The same issue is problematic between hospitals. Although all hospitals are operating under the administration of one medical university, medical university authorities have to ask from the statistics departments of each hospital to produce physical (paper-based) reports, analyze them, and then send them to the medical university. Having a standard format of HIS (in spite of its being developed by different vendors) can lead to the monitoring of the hospitals’ data without direct review of physical paper reports. In general, a lack of standardization is a major issue throughout the world, but some countries have developed proper plans to mitigate negative effects of it.
All hospital cases received virus attacks; even one of them had experienced virus infection of their unique server. Moreover, all cases had their own experimental solutions to block ports, particularly USB ports of users’ PCs. However, the IT security issues are inadequate in the healthcare centres despite strong physical security they have. No one of the servers were protected by data encryption tools, thus it is possible to support patient’s privacy in these hospitals. As a part of the HIS strategy, hospital authorities have to prepare a national IT security framework, preferably according to ISO/IEC 27000 family standard, to protect all data available on healthcare servers. Such mechanisms can lead to the protection of healthcare data, and an increase in patient privacy in these hospitals.
The methodology to select directors of hospitals in Iran is still traditional and based on the eligibility of one of the most famouss super specialists in the hospital. This person may not necessarily be a good manager and familiar with management fundamentals. Such hospital administration has caused several problems, and this method of head selection has not changed yet. The director of hospital have to be familiar with different areas of expertise in addition to general information about healthcare. Moreover, there is not such a defined position as a Chief Information Officer (CIO) in hospitals and the roles of IT departments vary from one hospital to another. As mentioned before, even the same department is called differently in different hospitals. Thus, the administration of hospitals would better be granted to an eligible person who is familiar with management principles. Moreover, the roles of IT departments have to be redefined in accordance with the importance of HIS in hospitals.
Resistance to change is always a matter of concern during any technology implementation in different organizations, and hospitals are not an exception. A lack of knowledge and experience of hospital management to transfer HIS technology to hospitals always causes resistance from medical and none-medical staff. Normally, after the implementation of HIS system, the training sessions start. These behaviors make users unhappy, especially once they have experienced previous systems and they are satisfied with them. Thus, following experts ‘guidance led to the mitigation of potential resistance from users. Moreover, proper implementation plans including training sessions, distribution of users’ manuals, and small gatherings help to increase the HIS systems’ acceptance in hospitals. In accordance with Electronic Medical Record Adoption Model (EMRAM) (www.himss.org) for HIS utilization in hospitals, the most mature HIS has tobe able to deliver a paper-less system with a complete EMR; Continuity of Care Document (CCD) transactions to share data; Data warehousing; and Data continuity with ED specifications. However, there are some barriers to attain the top level of this ranking system by Iranian hospitals. Beside the barriers mentioned before, there is a legal barrier imposed by the government and the judicial system. The problem is that all medical records have to be archived in physical format for at least 5 years. Moreover, the surgery information of every patient has to be in physical format. Although some improvements are being made, insurance companies also require the a paper-based physical format of patient’s documents. Thus, some initiatives are needed in order to find solutions to protect patients’ rights and also EMRAM requirements.
The authors aim to extend their scope of research to other dimensions within the country. Clarification of on-going national e-Health projects in line with the Iranian 5-year national plan helps to uncover the government’s efforts and achievements, and probably provides lessons learned within each hospital during HIS utilization.
Research Limitations
The researchers were able to look at all areas of interest within the scope of this research in the respective hospitals. Thus, there were no problems with data and document access in these hospitals. However, major information resources were obtained from oral interviews and almost limited trusted sources of collected data as evidence for this research are found.
Acknowledgements
The authors would like to thanks from the hospital staff and managers as well as Isfahan medical university for their kinds collaborations and supports.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Jahanbakhsh M, Tavakoli N, Mokhtari H. Challenges of EHR implementation and related guidelines in Isfahan. Proc Comput Sci. 2011;3:1199–1204. [Google Scholar]
- 2.Kwankam S. What e-health can offer. World Health Organization. Bull World Health Organ. 2004;82:800–802. [PMC free article] [PubMed] [Google Scholar]
- 3.Pagliari C, Sloan D, Gregor P, Sullivan F, Detmer D, Kahan J, Oortwijn W, MacGillivray S. What is e-health (4):A scoping exercise to map the field. J Med Internet Res. 2005;7:e9. doi: 10.2196/jmir.7.1.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bashshur R, Shannon G, Krupinski E, Grigsby J. The taxonomy of telemedicine. Telemed J E Health. 2011;17:484–494. doi: 10.1089/tmj.2011.0103. [DOI] [PubMed] [Google Scholar]
- 5.Sauer C, Willcocks LP. Unreasonable expectations - NHS IT, Greek choruses and the games institutions play around mega-programmes. J Inform Technol. 2007;22:195–201. [Google Scholar]
- 6.Fitzgerald G, Piris L, Serrano A. Piscataway, NJ: Proceedings of the ITI 2008 30th International Conference on Information Technology Interfaces, IEEE; 2008. Identification of benefits and barriers for the adoption of e-health information systems using a socio-technical approach; pp. 23–26. [Google Scholar]
- 7.Peng Y. European eHealth programs and smart cards:An enabler for ehealth services. 2009 [Google Scholar]
- 8.Lorenzi NM, Kouroubali A, Detmer DE, Bloomrosen M. How to successfully select and implement electronic health records (EHR) in small ambulatory practice settings. BMC Med Inform Decis Mak. 2009;9:15. doi: 10.1186/1472-6947-9-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abdul Karim NS, Ahmad M. Proceedings of the 2010 IEEE ICMIT; 2010. An Overview of Electronic Health Record (EHR) Implementation Framework and Impact on Health Care Organizations In Malaysia:A Case Study; pp. 84–90. [Google Scholar]
- 10.Chattopadhyay S, Li J, Land L, Ray P. Piscataway, NJ: 10th IEEE International Conference on e-Health Networking, Applications and Service (HEALTHCOM 2008), IEEE; 2008. A Framework for assessing ICT preparedness for e-health implementations. [Google Scholar]
- 11.Varshney U. New York: Springer Science, Business Media; 2009. Pervasive healthcare vomputing:EMR/EHR, wireless and health monitoring; pp. 17–38. [Google Scholar]
- 12.MacKinnon W, Wasserman M. Piscataway, NJ: Proceedings of the 42nd Hawaii International Conference on System Sciences, IEEE; 2009. Integrated electronic medical record systems:Critical success factors for implementation. [Google Scholar]
- 13.Ball MJ, Lillis J. E-health:Transforming the physician/patient relationship. Int J Med Inform. 2001;61:1–10. doi: 10.1016/s1386-5056(00)00130-1. [DOI] [PubMed] [Google Scholar]
- 14.Mair F, Whitten P. Systematic review of studies of patient satisfaction with telemedicine. BMJ. 2000;320:1517–1520. doi: 10.1136/bmj.320.7248.1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nelson R. Connecting the providers in your healthcare community:One step at a time. Front Health Serv Manage. 2005;22:13–28. [PubMed] [Google Scholar]
- 16.Skok W, Ryder G. An evaluation of conventional wisdom of the factors underlying the digital divide:A case study of the Isle of Man. Stategic Change. 2004;13:423–428. [Google Scholar]
- 17.Swartz N. A prescription for electronic health records. Inform Manage J. 2004;38(4):20. [Google Scholar]
- 18.Taylor R, Bower A, Girosi F, Bigelow J, Fonkych K, Hillestad R. Promoting health information technology:Is there a case for more-aggressive government action? Health Aff (Millwood) 2005;24:1234–1245. doi: 10.1377/hlthaff.24.5.1234. [DOI] [PubMed] [Google Scholar]
- 19.Hersh WR, Wallace JA, Patterson PK, Shapiro SE, Kraemer DF, Eilers GM, Chan BK, Greenlick MR, Helfand M. Telemedicine for the Medicare population:Pediatric, obstetric, and clinician-indirect home interventions. Evid Rep Technol Assess (Summ) 2001;24(Suppl):1–32. [PMC free article] [PubMed] [Google Scholar]
- 20.Wootton R. Recent advances:Telemedicine. BMJ. 2001;323:557–560. doi: 10.1136/bmj.323.7312.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wickramasinghe NS, Fadlalla AMA, Geisler E, Schaffer JL. A framework for assessing e-health preparedness. Int J Electron Health. 2005;1:316–334. doi: 10.1504/IJEH.2005.006478. [DOI] [PubMed] [Google Scholar]
- 22.Williams T, May C, Mair F, Mort M, Gask L. Normative models of health technology assessment and the social production of evidence about telehealthcare. Health Policy. 2003;64:39–54. doi: 10.1016/s0168-8510(02)00179-3. [DOI] [PubMed] [Google Scholar]
- 23.Jennett P, Jackson A, Healy T, Ho K, Kazanjian A, Woollard R. A study of a rural community's readiness for telehealth. J Telemed Telecare. 2003;9:259–263. doi: 10.1258/135763303769211265. [DOI] [PubMed] [Google Scholar]
- 24.Bates DW, Ebell M, Gotlieb E, Zapp J, Mullins HC. A proposal for electronic medical records in U.S. primary care. J Am Med Inform Assoc. 2003;10:1–10. doi: 10.1197/jamia.M1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Poissant L, Pereira J, Tamblyn R, Kawasumi Y. The impact of electronic health records on Time efficiency of physicians and nurses:A systematic review. J Am Med Inform Assoc. 2005;12:505–516. doi: 10.1197/jamia.M1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.MacKinnon G. eHealth in the Commonwealth:Building health-care systems in the digital age, private sector perspectives, opportunities and challenges in e-health:Private sector perspectives. CBC E-health Report. Commonwealth Business Council. 2009:6–8. [Google Scholar]
- 27.Mushtaq U, Hall K. TIC-STH Conference; 2009. Power and agency in health information technology:Towards a more meaningful participatory design for sustainable development; pp. 26–27. [Google Scholar]
- 28.Heeks R. Information systems and developing countries:Failure, success, and local improvisation. Inform Soc. 2002;18:101–112. [Google Scholar]
- 29.Ferreira A, Cruz-Correia R, Chadwick D, Antunes L. Piscataway, NJ: 42nd Annual IEEE International Carnahan Conference on Security Technology, IEEE; 2008. Improving the implementation of access control in EMR; pp. 13–16. [Google Scholar]
- 30.Richards H, King G, Reid M, Selvaraj S, McNicol I, Brebner E, Godden D. Remote working:Survey of attitudes to ehealth of doctors and nurses in rural general practices in the United Kingdom. FamPract. 2005;22:2–7. doi: 10.1093/fampra/cmh716. [DOI] [PubMed] [Google Scholar]
- 31.Ammenwerth E, Gräber S, Herrmann G, Bürkle T, Konig J. Evaluation of health information systems—Problems and challenges. Int J Med Inform. 2003;71(2-3):125–135. doi: 10.1016/s1386-5056(03)00131-x. [DOI] [PubMed] [Google Scholar]
- 32.Aoki N, Dunn K, Johnson-Throop KA, Turley JP. Outcomes and methods in telemedicine evaluation. Telemed J E Health. 2003;9:393–401. doi: 10.1089/153056203772744734. [DOI] [PubMed] [Google Scholar]
- 33.Jaana M, Paré G, Sicotte C. Hawaii, USA: Proceedings of the 42nd Hawaii International Conference on System Sciences; 2009. “IT Capacities Assessment Tool:A Survey of Hospitals in Canada”. [Google Scholar]
- 34.Essien EE, Williams EE. “E-health services in rural communities in thedeveloping countries”. Adaptive Science and Technology (ICAST 2009) 2009 [Google Scholar]
- 35.Carvalho M. Jornal de pediatria. Rio de Janero: 2002. [Accessed 2 Aug 2011]. Erro medico em pacientes hospitalizados. Disponivel em: http://www.scielo.br/pdf/jped/v78n4/v78n4a04.pdf . [DOI] [PubMed] [Google Scholar]
- 36.Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support system:a systematic review of trails to identify features critical to success. [Accessed 14 March 2011];British Medical Journal. 2005 doi: 10.1136/bmj.38398.500764.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Assaad A, Fayek D. IEEE Publications; 2006. General Hospitals Network Models for the support of E-Health Applications. [Google Scholar]
- 38.National Centre for Research Resources; 2006. Apr, Electronic Health Records Overview, National Health Institue of Health. [Google Scholar]
- 39.Chaudhry B, Wang J, Wu Sh, Maglione M, Mojica W, Roth E, Morton SC, Shekelle PG. Systematic Review:Impact of Health Information Technology on Quality, Efficiency, and Costs of Medical Care. Annals ofInternal Medicine. 2006;144(10):742–752. doi: 10.7326/0003-4819-144-10-200605160-00125. [DOI] [PubMed] [Google Scholar]
- 40.18th the Annual HIMSS Leadership Survey, Final Report, Healthcare CIO; 2007. [Accessed 4 March 2011]. Healthcare Information and Management Systems Society. http://www.himss.org/2007survey/docs/18thannualleadershipsurvey.pdf . [Google Scholar]


