Abstract
Background & objectives:
Effective pain control following outpatient surgical procedures is an important aspect of patient discharge. This study was carried out with an aim to investigate the histopathological effects of intra-articular dexketoprofen trometamol injection in knee joint on synovium and cartilage in an experimental rat model.
Methods:
In each of 40 rats, the right knee was designated as the study group and the left knee as the control group (NS group). Under aseptic conditions, 35 rats received an injection of 0.25 ml (6.25 mg) dexketoprofen trometamol into the right knee joint and an injection of 0.25 ml 0.9 per cent normal saline solution into the left knee joint. On the 1st, 2nd, 7th, 14th, and 21st days after intra-articular injection, rats in specified groups were sacrificed by intraperitoneal injection of 120 mg/kg sodium thiopental. Knee joints were separated and sectioned for histopathological examination. Inflammatory changes in the joints were recorded according to a grade scale.
Results:
No significant difference in terms of pathological changes both in synovium and cartilage was observed between the NS group and the study group on days 1, 2, 7, 14 and 21 after intra-articular injection of dexketoprofen or saline in the knee joint.
Interpretation & conclusions:
The findings showed no evidence of significant histopathological damage to the cartilage and synovia for a period up to 21 days following intra-articular administration of dexketoprofen trometamol in the knee joints of rats.
Keywords: Cartilage, dexketoprofen, knee, pain, rat models, synovium
Post-operative pain is an acute form of pain that begins with surgical trauma and gradually abates as tissues heal. While the general approach to post-operative pain is to treat it as a natural result of surgery that must be endured, the treatment focuses on pain reduction as opposed to complete elimination1.
Diagnostic or treatment arthroscopy is one of most frequent outpatient surgical procedures. Either separately or in combination, intra-articular application of local anaesthetics, opioids, and non-steroidal anti-inflammatory drugs (NSAIDS) provide effective analgesia for outpatient arthroscopic procedures2,3.
Dexketoprofen is the S(+) enantiomer of ketoprofen, which is a cyclooxygenase (COX)-1 and COX-2 inhibitor arylpropyonic acid4. Enantiomers, of various drugs provide a more controlled profile and minimizes the drugs adverse effects5,6. Intravenous administration of dexketoprofen trometamol after orthopedic surgery has been demonstrated to provide effective analgesia7,8; however, only few studies are available on the safety aspects of clinical and experimental intra-articular administration of the intravenous form of dexketoprofen trometamol on the knee joint9. Study to investigate the histo-pathological effects of intra-articular dexketoprofen trometamol injection in knee joint synovium and cartilage in an experimental rat model.
Material & Methods
The study was conducted during June to August 2010 in the department of Anaesthesiology, Istanbul University, Istanbul, Turkey. The study protocol was approved by the Istanbul University Laboratory Animals Ethics Committee. Forty five female Sprague-Dawley rats weighing 180-250 g were rised at the Istanbul University Experimental Medicine Research Laboratory. The rats were fed with standard laboratory food; there was no food or fluid restriction.
In each of the 40 rats, the right knee was designated as the study group and the left knee as the control group (NS group). Under aseptic conditions, 35 rats received an injection of 0.25 ml (6.25 mg) intravenous form of dexketoprofen trometamol (Arveles® 50 mg / 2 ml ampule, Ibrahim Ethem Ulagay, Turkey) consisting of deksketoprofen trometamol, ethanol, sodium chloride, and sodium hidroxide into the right knee joint and an injection of 0.25 ml 0.9 per cent normal saline solution in to the left knee joint. The remaining five rats received punctures in both knee joints with an empty insulin injection needle and were designated as shamoperated in order to evaluate the possible traumatic effect of puncture on the knee joint. The rats were then placed into cages, five rats per cage, to be sacrificed on days 1, 2, 7, 14, and 21. The sham operated rats were placed in a separate cage.
On the 1st, 2nd, 7th, 14th, and 21st days after intra-articular injection, rats in specified groups were sacrificed by intraperitoneal injection of 120 mg/kg sodiumthiopental. Using a scalpel and surgical scissors, the legs were amputated at the level of the femur head. The soft tissues were removed without disturbing the knee joint, and the samples were macroscopically assessed for the presence of haematoma. On the day the rats were sacrificed, the samples were tagged as right (R), left (L), sham right (SR), and sham left (SL)and placed into 50 ml bottles filled with 10 per cent formaldehyde.
The knee joints of the rats sacrificed in the first 24 h after intra-articular injection were designated as group 1 (n=9). A total of 18 samples were collected from eight right, eight left, and two right and left knee joints of sham rats, and named 24R, 24L, 24SR, and 24SL, respectively. The knee joints of the rats sacrificed in the first 48 h after intra-articular injection were designated as group 2 (n=9). The 18 samples collected were lebelled as from eight right, eight left, and two right and left knee joints of sham rats, and named 48R, 48L, 48SR, and 48SL, respectively. The knee joints of the rats sacrificed on the 7th day after intra-articular injection were designated as group 3 (n=9). The 18 samples collected were labelled as 7R, 7L, 7SR, and 7SL, respectively. The knee joints of the rats sacrificed on the 14th day after intra-articular injection were designated as group 4 (n=9), and the 18 samples collected were labelled as 14R, 14L, 14SR, and 14SL, respectively. The knee joints of the rats sacrificed on the 21st day were designated as group 5 (n=7) and the samples (n=18) collected were named 21R, 21L, 21SR, and 21SL, respectively.
The samples were decalcified with a 10 per cent formic acid solution, cut into 5 μm slices with a microtome in prepared paraffin blocks, stained with haematoxylin-eosin (H&E), and examined under a light microscope.
Histopathological examination of knee joint samples was done as follows:
Synovial reaction evaluation: Normal microscopy-0; increase in synovial cells, presence of neutrophils and fibroblasts- +1; and increase in synovial cells, presence of neutrophils and fibroblasts, and increase in fibrin- +2.
Cartilage evaluation: Normal microscopy -0; focal synovial adhesion- +1; focal surface erosion- +2; and reactive fibroblastic proliferation: +3.
When calculating the total grade, points assigned for synovial reaction and joint cartilage evaluation were added up, and one extra point was added if there were changes in both synovium and cartilage. Grades were evaluated as follows: 0= normal, 1= very mild, 2= mild, 3= moderate, 4= severe, and 5-6= very severe. Grade 0 was described as negative (for the undestroyed joint group), whereas grades 1 through 6 were described as positive (for the destroyed joint group).
Statistical analysis: The NCSS 2007 software package (NCSS, LLC, Utah, USA) was used for statistical analysis. The Chi-square test and Fisher's exact test were used for comparison of qualitative variables, and P<0.05 was considered as significant.
Results & Discussion
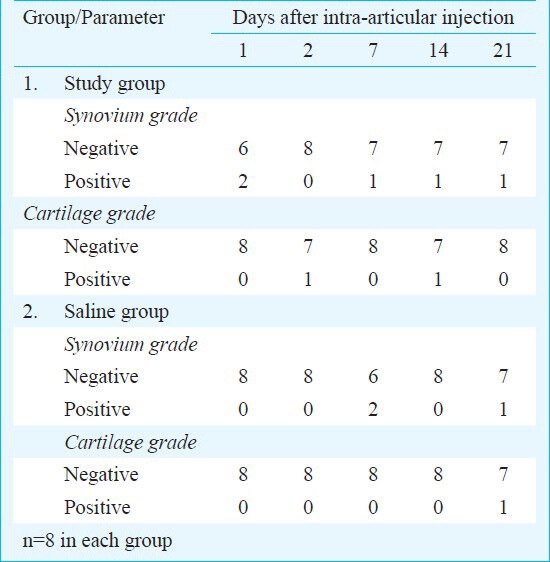
None of the rats died during the experiment. There were no macroscopic signs of haematoma seen in any of the groups. Two samples in group 1 and one each in groups 3, 4 and 5 showed grade 1 changes in synovium and cartilage in the saline treated controls of group 3 and one in group 5. Two samples also showed grade 1 changes. One sample each of groups 2, 4 and one control sample in group 5 showed grade 3 changes. The remaining samples received a grade 0. A mild synovial reaction was seen in the right knee joint of sham-operated rats from groups 1 and 2. The microscopy of other sham-operated samples was normal.
No significant difference in terms of pathological changes in synovium and cartilage was obtained between the NS group and the study group (Table).
Table.
Histological changes seen in synovium and cartilage of knee joints
In outpatient surgeries, preference is given to analgesic methods with a rapid onset of action, a long-term effect, and minimal side effects. Intra-articular drugs are widely used to secure preemptive and post-operative analgesia in various arthroscopic procedures. The most commonly used drugs are NSAIDs, bupivacaine, and morphine. Many studies have been published on the intra-articular effects of these drugs7,8,10. Elhakim et al11 compared intravenous normal saline with 20 mg intra-articular tenoxicam and found the latter to have a stronger analgesic effect than the placebo. Colbert et al12 compared intravenous and intra-articular tenoxicam and found the latter to be more effective in providing analgesia. Another group compared intra-articular neostigmine, tramadol, bupivacaine, and tenoxicam and found all four to be similarly effective and safe, with a few side effects13.
Talu et al14 compared intra-articular tenoxicam, bupivacaine, and a combination of the two in arthroscopic knee surgery. Bupivacaine was found to have a stronger analgesic effect when used alone, while the patients who received a combination of bupivacaine and tenoxicam were reported to have a more comfortable recovery period. Güler et al15 compared intra-articular tenoxicam and morphine and reported a similar analgesic effect in both groups.
In studies on chondrocyte culture cartilage harvested from osteoarthritis patients different NSAIDs have been shown to have different effects in vitro on cartilage metabolism and proteoglycan synthesis16,17. In a study in which NSAIDs were applied locally, Romsing et al18 found that systemic use of many NSAIDs might inhibit proteoglycan synthesis and disrupt chondrocyte metabolism. Sagis et al9 showed that in vitro application of dexketoprofen in primary culture caused significant toxicity.
In a study by Balabonova et al19, rheumatoid arthritis patients received 8 mg intra-articular injections of lornoxicam into the knee joint once a week for 3 weeks. Ultrasonographic monitoring of changes in the joint revealed synovial membrane thickening and a reduced amount of exudate in the joint cavity indicating that it did not damage the knee joint; on the contrary, it reduced inflammation.
One of the limitations of our study was that in absense of preservative-free form of dexketoprofen trometamol, we used an intravenous form to apply intra-articularly. Another limitation was a lack of randomization and blinding.
In conclusion, no significant histopathological damage was observed in the cartilage and synovium up to 21 days after intra-articular administration of dexketoprofen trometamol in the keen joint of experimental rat model. The changes seen in rat joints may not be consistent with findings in the humans. There is a need for further research involving electron microscopic examination, a preservative-free form of dexketoprofen, and animals with joint size and structure closer to humans. Follow up investigations of the long-term effects of dexketoprofen and studies of its histopathological effect and analgesic effectiveness in humans are necessessary to determine the safety of intra-articular administration of dexketoprofen alone or in combination with other drugs.
References
- 1.Clarke IM. Management of postoperative pain. Lancet. 1993;341:27. doi: 10.1016/0140-6736(93)92492-c. [DOI] [PubMed] [Google Scholar]
- 2.Denti M, Randelli P, Bigoni M, Vitale G, Marino MR, Fraschini N. Pre- and postoperative intra-articular analgesia for arthroscopic surgery of the knee and arthroscopy-assisted anterior cruciate ligament reconstruction. A double-blind randomized, prospective study. Knee Surg Sports Traumatol Arthrosc. 1997;5:206–12. doi: 10.1007/s001670050051. [DOI] [PubMed] [Google Scholar]
- 3.Calmet J, Esteve C, Boada S, Gine J. Analgesic effect of intra-articular ketorolac in knee arthroscopy: comparison of morphine and bupivacaine. Knee Surg Sports Traumatol Arthrosc. 2004;12:552–5. doi: 10.1007/s00167-003-0483-3. [DOI] [PubMed] [Google Scholar]
- 4.Barbanoj MJ, Antonijoan RM, Gich I. Clinical pharma-cokinetics of dexketoprofen. Clin Pharmacokinet. 2001;40:245–62. doi: 10.2165/00003088-200140040-00002. [DOI] [PubMed] [Google Scholar]
- 5.Mauleón D, Artigas R, García ML, Carganico G. Preclinical and clinical development of dexketoprofen. Drugs. 1996;52(Suppl 5):24–46. doi: 10.2165/00003495-199600525-00005. [DOI] [PubMed] [Google Scholar]
- 6.Caldwell J, Hutt AJ, Fournel-Gigleux S. The metabolic chiral inversion and dispositional enantioselectivity of the 2-arylpropionic acids and their biological consequences. Biochem Pharmacol. 1988;37:105–14. doi: 10.1016/0006-2952(88)90762-9. [DOI] [PubMed] [Google Scholar]
- 7.Zippel H, Wagenitz A. Comparison of the efficacy and safety of intravenously administered dexketoprofen trometamol and ketoprofen in the management of pain after orthopaedic surgery: a multicentre, double-blind, randomised, parallel-group clinical trial. Clin Drug Investig. 2006;26:517–28. doi: 10.2165/00044011-200626090-00005. [DOI] [PubMed] [Google Scholar]
- 8.Berti M, Albertin A, Casati A, Palmisano S, Municino G, da Gama Malcher M, et al. A prospective, randomized comparison of dexketoprofen, ketoprofen or paracetamol for postoperative analgesia after outpatient knee arthroscopy. Minerva Anestesiol. 2000;66:549–54. [PubMed] [Google Scholar]
- 9.Sagir O, Sunay FB, Yildirim H, Aksoz E, Ozaslan S, Koroglu A, et al. Evaluation of the effects of dexketoprofen trometamol on knee joint: an in vivo & in vitro study. Indian J Med Res. 2013;138:912–8. [PMC free article] [PubMed] [Google Scholar]
- 10.Smith I, Shiuley RA, White PF. Effects of ketorolac and bupivacaine on recovery after outpatient arthroscopy. Anesth Analg. 1992;75:208–12. doi: 10.1097/00000542-199209001-00208. [DOI] [PubMed] [Google Scholar]
- 11.Elhakim M, Fathy A, Elkott M, Said MM. İntra-artikular tenoxicam relieves post-arthroscopy pain. Açta Anaesthesiol Scand. 1996;40:1223–6. doi: 10.1111/j.1399-6576.1996.tb05554.x. [DOI] [PubMed] [Google Scholar]
- 12.Colbert ST, Curran E, O’Hanlon DM, Moran R, McCarroll M. İntra-articular tenoxicam improves post operative analgesia in knee arthroscopy. Can J Anesth. 1999;46:653–7. doi: 10.1007/BF03013953. [DOI] [PubMed] [Google Scholar]
- 13.Kayacan N, Boztug N, Arici G, Karslı B, Erman M. The effect of intra-articular neostigmine, tramadol, tenoxicam and bupivacaine on post-operative pain. Ambul Surg. 2002;10:29–32. [Google Scholar]
- 14.Talu GK, Özyalçin S, Koltka K, Erturk E, Akinci O, Asik M, et al0. Comparison of effıcacy of intraarticular application of tenoxicam, bupivacaine and tenoxicam: bupivacaine combination in arthroscopic knee surgery. Knee Surg Sports Traumatol Arthros. 2002;10:355–60. doi: 10.1007/s00167-002-0306-y. [DOI] [PubMed] [Google Scholar]
- 15.Güler G, Karaoğlu S, Velibaþoğlu H, Ramazanogullari N, Boyaci A. Corparison of analgesic effects of intra-articular tenoxicam and morphine in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthros. 2002;10:229–32. doi: 10.1007/s00167-002-0286-y. [DOI] [PubMed] [Google Scholar]
- 16.Fjuii K, Tajiri K, Kajiwara T, Tanaka T, Murota K. Effects of NSAID on collagen and proteoglycan synthesis of cultured chondrocytes. J Rheumatol (Suppl) 1989;18:28–31. [PubMed] [Google Scholar]
- 17.David MJ, Vignon E, Peschard MJ, Broquet P, Louisot P, Richard M. Effect of non-steroidal anti-inflammatory drugs (NSAIDS) on glycosyltransferase activity from human osteoarthritic cartilage. Br J Rheumatol. 1992;31(Suppl 1):13–7. [PubMed] [Google Scholar]
- 18.Romsing J, Moiniche S, Ostergaard D, Dahl JB. Local infiltration with NSAIDs for postoperative analgesia: evidence for a peripheral analgesic action. Acta Anaesthesiol Scand. 2000;44:672–83. doi: 10.1034/j.1399-6576.2000.440607.x. [DOI] [PubMed] [Google Scholar]
- 19.Balabanova RM, Fedina TP, Tsurko VV, Mach ES, Khitrov NA, Agapova LA, et al. Dynamic changes in synovitis activity after intra-articular administration of xefocam in patients with rheumatoid arthritis (according to clinical and device examinations) Ter Arkh. 2003;75:33–5. [PubMed] [Google Scholar]


