Abstract
Background & objectives:
Human immunodeficiency virus (HIV) has infected several million individuals in India. Various interventions have been implemented for early detection and prevention of transmission of HIV infection. This has progressively changed the clinical profile of HIV infected individuals and this study documents the clinical presentation of individuals positive for HIV in 2010, in Pune, Maharashtra, India.
Methods:
This cross-sectional study included subjects who had come to the HIV referral clinic for HIV testing from January to December 2010. Children as well as individuals with indeterminate HIV result were excluded from the study, and data for 1546 subjects were finally analysed.
Results:
The HIV positivity rate among all referred cases for the year 2010 was 35 per cent (male 55% and females 45%). The median age (Q1, Q3) was 31 (25.75, 39) yr. The median CD4 cell count for all HIV infected individuals (whose CD4 count was available n= 345) was 241 cells/µl and for asymptomatic HIV infected individuals was 319 cells/µl. There were 673 (43.5%) symptomatic and 873 (56.5%) asymptomatic participants. Fever, breathlessness, cough with expectoration, weight loss, loss of appetite, generalized weakness, pallor and lymphadenopathy (axillary and cervical) were found to be associated (P< 0.001) with HIV positivity. On multivariate analysis, history of Herpes zoster [AOR 11.314 (6.111-20.949)] and TB [AOR 11.214 (6.111-20.949)] was associated with HIV positivity.
Interpretation & conclusions:
Signs and symptoms associated with HIV positivity observed in this study can be used by health care providers to detect HIV infection early. Moreover, similar to HIV testing in patients with tuberculosis, strategies can be developed for considering Herpes zoster as a predictor of HIV infection.
Keywords: Clinical profile; herpes zoster; HIV; Pune, India; TB
In India, human immunodeficiency virus (HIV) testing is performed as a voluntary test or as a diagnostic procedure in symptomatic individuals1. HIV testing is a part of screening procedure in antenatal clinics as a mode of prevention of parent to child transmission (PPTCT). It is also done in all tuberculosis (TB) patients due to the strong association between HIV and TB2. In spite of these various HIV testing opportunities, earlier a majority of infected individuals became aware of their status only after they developed opportunistic infections in the late stages3,4. This picture was due to the lack of awareness about HIV/ acquired immuno deficiency syndrome (AIDS) in individuals with high risk behaviour such as men having sex with men, sex workers, and injecting drug users.
Various strategies have been developed to increase awareness of HIV and AIDS since the onset of the HIV epidemic in India5. The aim of these interventions is early diagnosis of HIV infection which facilitates better care, ameliorates clinical outcomes and improves strategies by healthcare delivery systems6. Studies show that a person diagnosed and counselled for HIV infection avoids high risk behaviour which is beneficial to the society by limiting the transmission of the virus7.
These interventions and programmes have led to a change in the clinical presentations of individuals coming to health care clinics. In this study all individuals coming to a HIV referral clinic, in Pune, India, in year 2010 were studied with the objective of assessing their clinical profile.
Material & Methods
This cross-sectional study involved individuals who had come to a HIV referral clinic at the National AIDS Research Institute (NARI), Pune, India, for HIV testing from January to December 2010. NARI is a national reference centre for HIV/AIDS and conducts various research studies related to HIV/AIDS in India.
The individuals attending HIV referral clinic at NARI included all those who had voluntarily come to the clinic, as well as those referred by their physicians, other health care institutes (government and private) and the community referral programme of NARI from various parts of Maharashtra State. However, majority of them were referred from Pune district and nearby area. There are 20 more State Government integrated counseling and testing centers (ICTCs) in Pune city where HIV testing is carried out.
All individuals who came to the clinic were initially counselled about HIV infection and then written consents were taken from them which was approved by NARI ethics committee. They were screened for HIV infection as per the NACO guidelines. Strategy III of the NACO guidelines was followed for the HIV testing8. Test for HIV antibodies by ELISA test (Microlisa HIV manufactured by J. Mitra and Co. Pvt Ltd, New Delhi) was carried out. Individuals testing negative by ELISA were reported as nonreactive for HIV antibodies and those who tested positive were retested with two rapid tests. The rapid tests used for testing were Tridot HIV (HIV TRIDOT manufactured by Diagnostic enterprises, Parwanoo, Himachal Pradesh, India) and Immunocomb (Immunocomb II - HIV 1 & 2 BiSpot Orgenics manufactured by Orgenics, Yavneh, Israel). These individuals were reported to be reactive for HIV antibodies when all three tests were positive. In case of discordance in these three test results, the Western blot test (Genetic system HIV-1 manufactured by Bio-Rad, California, US) was performed to confirm the HIV status of the patient. Symptomatic treatment was given to all the patients who had symptoms.
The CD4 cell count was done by immunopheno-typing of lymphocytes. It was carried out by 4-colour analysis on FACS calibur (Becton Dickinson, Singapore). Lymphocytes were stained according to the protocol suggested by the manufacturer. In brief, 50µl of EDTA blood was mixed with 20 µl of monoclonal antibodies (CD4 – APC, CD3 – FITC, CD8 PE, and CD45 per CP). The red cells were lysed using lysing solution (FACS lysin, BD, Singapore) and incubated for 15 min. Gating for lymphocytes was carried out by leucogate reagent CD45 vs SSC gating. Individuals fitting in the inclusion criteria for indigenous clinical trials at National AIDS Research Institute (NARI; website www.nari-icmr.res.in) were enrolled in the study and those eligible for antiretroviral treatment (ART) were referred to ART centre.
Data required were extracted from the questionnaires filled by the counselors and clinicians who attended the patients and standard protocols were followed to ensure confidentiality of the information collected. Patient identification numbers were used to identify each case and all test reports were obtained from the records after linking the data. The data was entered in Excel sheets and statistical analysis was done using Statistical Package for Social Sciences (SPSS, Inc. Chicago, IL) 15.0 version. In this analysis, ELISA for HIV test result (Positive/Negative) was considered as a dependent variable. The signs, symptoms and opportunistic infections (OI) reported were considered as possible covariates. In univariate analysis one covariate was inserted in the model at a time to run the model. The covariates which were significant in univariate model were retained in multivariate logistic regression. Two tailed P values were considered in univariate and multivariate analyses. While calculating sensitivity, specificity and positive predictive value, past history of opportunistic infection was used as screening test and ELISA for HIV as gold standard and calculated using a statistical software (Primer of Biostatistics version 7 Inc. Chicago, IL). Thus, ‘past history of opportunistic infection’ was used as a predictor of HIV infection in that individual.
Results
A total of 1640 individuals were tested for HIV in 2010 at the NARI HIV referral clinic. Children (<18 yr) as well as individuals with indeterminate ELISA test result were excluded from the study and data were analyzed for the remaining 1546 individuals tested. Of the 1546 individuals analyzed, 692 (44.8%) were males and 854 (55.2%) were females. A majority of them 375 (43.7%) belonged to the age group of 26 to 35 yr and the median (Q1, Q3) age was 31 (25.75, 39) yr. Most of them 1163 (75.2%) had come from an urban background. A total of 611(39.5%) were referred by community referral programmes, 253 (16.4%) by physicians and 682 (44.1%) came on their own. It was observed that among those who came from the referrals by the community programme 462 (75.6%) were females, while in those who came voluntarily for HIV testing, males were more in number 406 (59.5%). Those referred by physicians had almost equal number of male 137 (55%) and females 116 (45%) (1: 0.8).
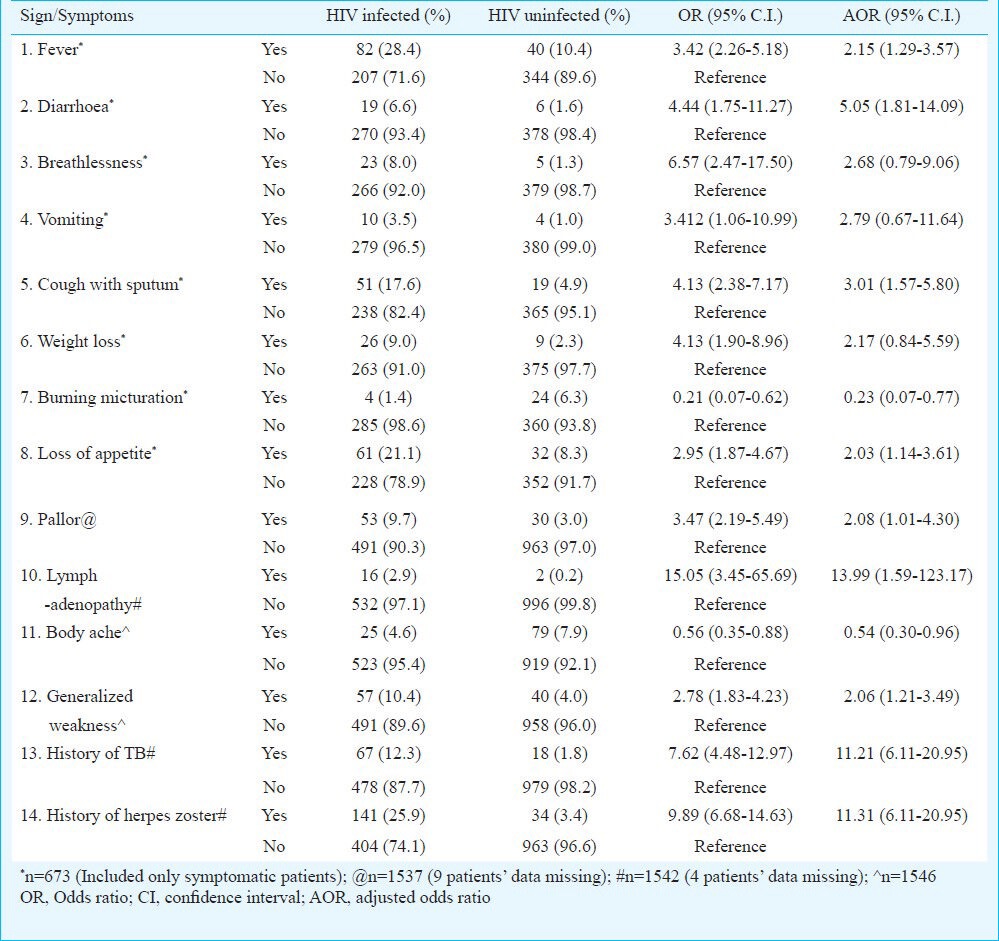
The HIV seropositivity rate was (548/1546) 35 per cent. There were 299 (55%) males of the 1546 individuals tested (47.9%) had got HIV test done earlier. Of these 548 HIV infected, 537 (34.7%) were HIV 1 reactive and 8 (0.5%) were HIV 2 reactive. There were 3 (0.2%) patients who were dually infected with HIV 1 and HIV 2. It was observed that 673 (43.5%) were symptomatic and 873 (56.5%) were asymptomatic. Symptoms found to be significant on univariate analysis are described in the Table I. Fever, breathlessness, cough with sputum, weight loss, loss of appetite, pallor, lymphadenopathy (cervical and axillary) and generalized weakness were found to be significantly associated (P<0.001) with HIV positivity. Those covariates that were significant in univariate model were retained in multivariate logistic regression. In multivariate analysis, it was seen that individuals with lymphadenopathy (cervical and axillary), fever, diarrhoea, cough with sputum, generalized weakness, body ache and loss of appetite were more likely to be HIV infected (P<0.05).
Table I.
Clinical profile of individuals tested in year 2010
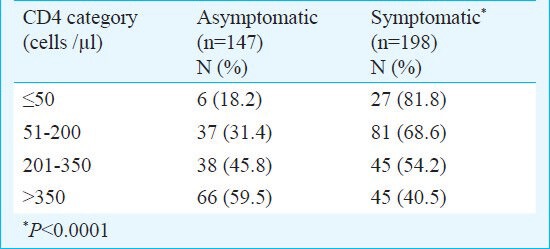
The CD4 cell count was available for 345 (63%) of the 548 HIV infected individuals. Median (Q1, Q3) CD4 count for all HIV infected individuals was 241 (112, 427) cells/µl, and for HIV infected asymptomatic individuals (n=147) was 319 (174, 500) cells/µl. CD4 was not done for the remaining 203(37%) individuals. Of these 203 individuals, 69 (34%) did not collect their ELISA test report and the remaining 134 (66%) had either come to confirm their HIV status and hence were not willing to get their CD4 count testing carried out or went to the nearest ART center for CD4 testing and further follow up. The CD4 count was categorized as <50, 51-200, 201-350 and >350 cells/µl and associated with their clinical presentation status in Table II. It was observed that a high proportion of individuals who had CD4 count >350 cells/µl were asymptomatic.
Table II.
CD4 category wise distribution of HIV infected individuals tested in year 2010 (n=345)
The illnesses suggestive of HIV associated infections with reference to their CD4 counts are analyzed in Fig. 1. As compared to individuals with higher CD4 counts, those with CD4 count within the range of 51-200 cells/µl had more symptoms, which included fever, breathlessness, cough with sputum, weight loss, diarrhoea, vomiting and loss of appetite. Cachexia and difficulty in swallowing was seen equally in CD4 categories <50 and 51-200 cells/µl.
Fig. 1.
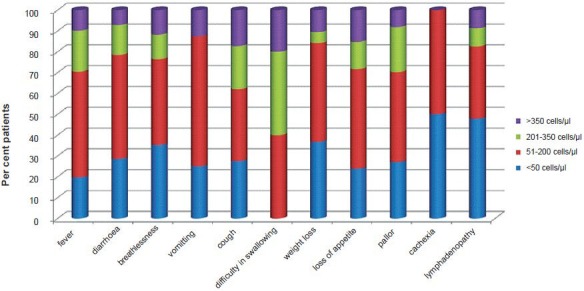
Presenting complaint and CD4 category-wise distribution of cases (n=265).
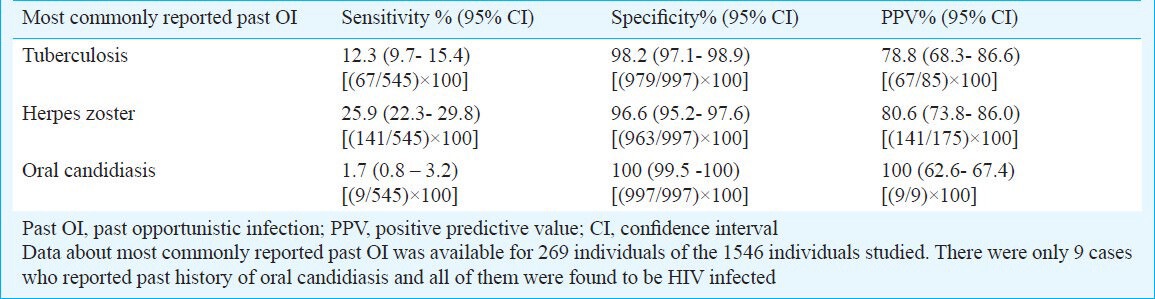
Among all those with past history of HIV associated infections, tuberculosis, Herpes zoster and oral candidiasis (269 individuals) were the most commonly reported infections. As observed in Table III, the positive predictive value for past history of oral candidiasis (100%) was highest followed by Herpes zoster (80.6%) and Tuberculosis (78.8%). On multivariate regression analysis, it was seen that the chance of a patient testing reactive for HIV was at least 11 times higher when there was a past history of TB. The chance of a patient testing reactive for HIV antibodies was also 11 times higher when there was a past history of Herpes zoster as compared to those who did not have such history.
Table III.
Sensitivity, specificity and positive predictive value for most commonly reported past opportunistic infections (OI) (n=269)
Among the 269 individuals who gave a past history of HIV associated illness, CD4 count was available for 185 individuals. The most common past history of illness was Herpes zoster, followed by tuberculosis and oral candidiasis. The past history of all three infections was mostly seen in the category of the patients with CD4 count between 51-200 CD4 cells/µl (Fig. 2).
Fig. 2.
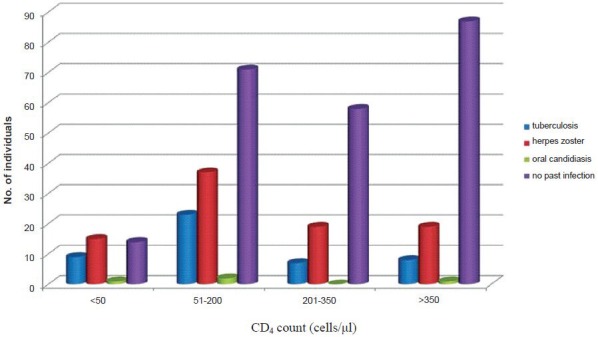
CD4 category-wise distribution of cases of past opportunistic infection (n= 185).
Discussion
Unlike prior studies (Varanasi - 25% females were tested9, Ahmadabad- 26 % females were tested10, Canada- equal proportions of male and female tested excluding probable prenatal screening tests done)11, in this study the females coming for HIV testing were in larger numbers than males since most of the individuals were referred by community workers who are mostly female. This helped to overcome social barriers for HIV testing and was in line with the recommendation of WHO about the development of a network of women at all levels to promote equitable access to ART and care for women and girls12.
The community programme of the institute (NARI, Pune) aims at increasing awareness about HIV/AIDS through group meetings as well as couple or one-to-one counselling, resulting in early detection of HIV infection even while one is asymptomatic. The maximum numbers of individuals were between 26 to 35 yr. In the Indian setting, this is important since this age group is economically productive and about 90 per cent of newly HIV infected individuals are believed to have acquired the infection during unprotected sex13.
The mean and median CD4 count observed in this study was 295 and 241 cells/µl respectively, which was higher when compared to a similar study conducted in Pune in 1996-97 (mean and median CD4 count 238 and 185 cells/µl)14. However, CD4 counts could not be done for 37 per cent of HIV infected subjects in the current study and the actual values could have been lower than that found. The asymptomatic individuals presented with a mean and median CD4 count of 369 and 319 cells/µl. This indicates that the trend towards earlier diagnosis of HIV infection is increasing.
The most common symptoms reported by the individuals who came for HIV testing were the same as reported in studies conducted at Pune and Varanasi but differed in proportion9,14. The combined sensitivity of constitutional symptoms of TB (fever, cough, weight loss and loss of appetite) was 0.868. High positive predictive values for the three past HIV associated infections (TB, Herpes zoster, oral candidiasis) suggested use of these infections as an indicator of HIV infection. Positive predictive value of Herpes zoster was 80.6 per cent in this study which was more than double as compared to a study conducted in Manipur, Imphal in India15.
In India, HIV testing for all TB patients has already been started, considering TB as a predictor for HIV2. Similarly, past history of Herpes zoster can also be considered as a predictor of HIV infection. One limitation of the study was that the information was collected in a HIV clinic and was not representative of the general population. Unlike some of the other Indian studies where the clinical presentation was studied in a group of HIV infected subjects16,17, this study presented clinical data from both HIV infected and HIV uninfected subjects coming to an HIV clinic. In addition, the time interval between onset of HIV infection and detection of opportunistic infection was unknown in individuals studied. There were no data to give concrete reason for the delay in diagnosis of HIV infected individuals who came in late stages.
It can be concluded from the results of this study that the proportion of individuals getting detected at an early stage of their infection has increased as compared to previous studies. The signs and symptoms strongly associated with HIV infection can be used for vigilance and early detection of HIV. There is a significant occurrence of tuberculosis, Herpes zoster and oral candidiasis in HIV infected patient. Strategies can be developed using Herpes zoster also as a positive predictors for detection of HIV infection.
References
- 1.National AIDS Control Organisation (NACO) New Delhi: NACO; 2011. Department of AIDS Control, Ministry of Health and Family Welfare, Government of India, New Delhi, Annual Report 2010-11. [Google Scholar]
- 2.National AIDS Control Organisation and Central TB Division. New Delhi: National AIDS Control Organisation and Central TB Division, Ministry of Health and Family Welfare, Government of India; 2009. National Framework for Joint HIV/TB Collaborative Activities. October 2009; p. 12. [Google Scholar]
- 3.Wortley PM, Chu SY, Diaz T, Ward JW, Doyle B, Davidson AJ, et al. HIV testing patterns: where, why, and when were persons with AIDS tested for HIV? AIDS. 1995;9:487–92. [PubMed] [Google Scholar]
- 4.Kumarasamy N, Solomon S, Chaguturu SK, Cecelia AJ, Vallabhaneni S, Flanigan TP, et al. The changing natural history of HIV disease: Before and after the introduction of generic antiretroviral therapy in Southern India. J Clin Infect Dis. 2005;41:1525–8. doi: 10.1086/497267. [DOI] [PubMed] [Google Scholar]
- 5.National AIDS prevention and control policy. [accessed on November 11, 2011]. Available from: http://www.hsph.harvard.edu/population/ vasaids/india.aids.02.pdf .
- 6.Sobhani R, Basavaraj A, Gupta A, Bhave AS, Kadam DB, Sangle SA. Mortality & clinical characteristics of hospitalized adult patients with HIV in Pune, India. Indian J Med Res. 2007;126:116–21. [PubMed] [Google Scholar]
- 7.Girardi E, Sabin CA, Monforte AD. Late diagnosis of HIV infection: Epidemiological features, consequences and strategies to encourage earlier testing. J Acquir Immune Defic Syndr. 2007;46(Suppl 1):S3–8. doi: 10.1097/01.qai.0000286597.57066.2b. [DOI] [PubMed] [Google Scholar]
- 8.National AIDS Control Organization. New Delhi: National AIDS Control Organization, Ministry of Health and Family Welfare, Government of India; 2007. Mar, Guidelines for HIV testing. [Google Scholar]
- 9.Pandey S, Sundar S, Hasan H, Shankar R, Singh SP. Clinical profile and opportunistic infection in HIV/AIDS patients attending SS Hospital, Varanasi. Indian J Prev Soc Med. 2008;39:17–20. [Google Scholar]
- 10.Sharma R. Profile of attendee for voluntary counseling and testing in the ICTC, Ahmedabad. Indian J Sex Transm Dis. 2009;30:31–6. doi: 10.4103/2589-0557.55479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gahagan JC, Fuller JL, Proctor-Simms EM, Hatchette TF, Baxter LN. Barriers to gender-equitable HIV testing: going beyond routine screening for pregnant women in Nova Scotia, Canada. Int J Equity Health. 2011;10:18. doi: 10.1186/1475-9276-10-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization/UNAIDS. Ensuring equitable access to antiretroviral treatment for women. WHO/UNAIDS policy statement. 2004. [accessed on November 18, 2011]. Available from: http://data.unaids.org/publications/external-documents/who-equitable-access-en.pdf .
- 13.Joint United Nations Programme on HIV/AIDS (UNAIDS) Global Report. UNAIDS Report on the Global AIDS epidemic. 2010. [accessed on November 21, 2011]. Available from: http://www.unaids.org/en/media/unaids/contentassets/ documents/unaidspublication/2010/20101123_globalreport_en.pdf .
- 14.Ghate MV, Mehendale SM, Mahajan BA, Yadav R, Brahme RG, Divekar AD, et al. RS Relationship between clinical conditions and CD4 counts in HIV-infected persons in Pune, Maharashtra, India. Natl Med J India. 2000;13:183–7. [PubMed] [Google Scholar]
- 15.Agarwal A, Zamzaching G, Devendra NS, Morens DK. Herpes zoster as a predictor of HIV infection. 12th International AIDS Conference 1998 June 28-July 3; Geneva, Switzerland. Int Conf AIDS. 1998;12:798. [Google Scholar]
- 16.Sobhani R, Basavaraj A, Gupta A, Bhave AS, Kadam DB, Sangle SA, et al. Mortality & clinical characteristics of hospitalized adult patients with HIV in Pune, India. Indian J Med Res. 2007;126:116–21. [PubMed] [Google Scholar]
- 17.Rajasekaran S, Mahilmaran A, Annadurai S, Kumar S, Raja K. Manifestation of tuberculosis in patients with human immunodeficiency virus: a large Indian study. Ann Thorac Med. 2007;2:58–60. doi: 10.4103/1817-1737.32231. [DOI] [PMC free article] [PubMed] [Google Scholar]


