Abstract
Objectives:
Sachse cold knife is conventionally used for optical internal urethrotomy intended to manage urethral strictures and Ho: YAG laser is an alternative to it. The aim of this study was to evaluate the role of urethral stricture treatment outcomes, efficacy, and complications using cold knife and Ho: YAG (Holmium laser) for optical internal urethrotomy
Materials and Methods:
In this prospective study included, 90 male patients age >18 years, with diagnosis of urethral stricture admitted for internal optical urethrotomy during April 2010 to March 2012. The patients were randomized into two groups containing 45 patients each using computer generated random number. In group A (Holmium group), internal urethrotomy was done with Holmium laser and in group B (Cold knife group) Sachse cold knife was used. Patients were followed up for 6 months after surgery in Out Patient Department on 15, 30 and 180 post-operative days. At each follow up visit physical examination, and uroflowmetry was performed along with noting complaints, if any.
Results:
The peak flow rates (PFR) were compared between the two groups on each follow up. At 180 days (6 month interval) the difference between mean of PFR for Holmium and Cold knife group was statistically highly significant (P < 0.001). Complications were seen in 12.22% of cases.
Conclusion:
Both modalities are effective in providing immediate relief to patients with single and short segment (<2 cm long) urethral strictures but more sustained response was attained with Cold knife urethrotomy.
Keywords: Cold knife urethrotomy, holmium laser urethrotomy, internal urethrotomy, short segment stricture, urethral stricture
INTRODUCTION
Urethral stricture is one of the most difficult urological problems to cure adequately and is known to mankind since ages as it has been documented in ancient literature of the Hindus,[1] Egyptians and Greeks.[2] Different techniques have been employed for the treatment of urethral strictures, depending on the stricture length, location, and depth of scar[3,4] which include simple dilatation, urethrotomy, uroLume stent placement,[2,5] urethroplasty and perineal urethrostomy.[6]
Optical internal urethrotomy (OIU) is one of the most commonly used procedures for urethral stricture.[7,8,9] Data from the National Health Service in the UK during 2006 showed that the OIU or urethral dilatation was used in 93% of cases and urethroplasty in 7% of cases.[10] Optical internal urethrotomy has the advantage of ease, simplicity, speed, and short convalescence. In 1957, Ravasini[11] described internal urethrotomy under direct vision and used electrocautery to incise the stricture, but it was not until 1971 that Sachse[12] introduced the sharp-bladed cold-knife urethrotome under direct vision, reporting 80% success rate with this procedure in 1974.
Lasers have been used for the treatment of urethral strictures since 1977.[13] The types of lasers[5] that have been used for urethrotomy include carbon dioxide, Nd: YAG, the KTP, the Argon, the Ho: YAG and excimer lasers. No superiority of one type of lasers has been demonstrated.[14] Holmium: YAG[5] is a new introduction in the range of laser modalities available; it provides both direct contact cutting and vaporization with minimal forward scatters.
The aim of our study is to evaluate and compare the outcomes of Ho: YAG laser urethrotomy with the conventional cold-knife technique.
MATERIALS AND METHODS
The present prospective study was conducted in the Department of Surgery of one of major teaching hospital of New Delhi India from April 2010 to March 2012. The protocol was approved by the scientific and ethical committee of the hospital. Informed and signed consent was taken from all patients after explaining the nature of the study and the consequences of the procedure to be done in detail in their own language. Patients had option to opt out of the study at any time without compromising their right of treatment. The study was based on Null Hypothesis stating there is no difference in outcome of treatment between two groups. A total of 90 male patients with diagnosed urethral strictures requiring optical internal urethrotomy were included in this study. Patients were randomized into two groups by computer generated random numbers. In group A (Holmium group); the patients underwent internal urethrotomy with Holmium laser. In group B (Cold knife group), Sachse cold knife was used for internal urethrotomy. Surgeon was informed about the group to which patient belonged just prior to surgery.
Inclusion criteria were - (1) Presence of obstructive symptoms, (2) Peak flow rate on uroflowmetry less than 15 ml/s, and (3) Short segment strictures (stricture length <2 cm) as evident on radiological studies, i.e. retrograde urethrography (RGU) and micturating cystourethrography (MCU). Exclusion criteria used were- (1) Complete obliteration of lumen of urethra on urethroscopy, (2) Balanitis Xerotica Obliterans, (3) Age less than 18 years, (4) Multiple strictures, (5) Active urinary tract infection, and (6) Recurrent Strictures.
All patients were assessed by a history and a full physical examination, complete blood count, urine analysis, urine culture and sensitivity test, renal function tests, uroflowmetry, micturatingcystourethrography (MCU), retrogradeurethrography (RGU), and urethroscopy using 00 Scope. A note was made about the possible etiology of the stricture. Any active UTI was treated before surgery with appropriate antibiotics based upon sensitivity test. Uroflowmetry was done in all patients except those who had suprapubic cystostomy and in these patients peak flow rate (PFR) was taken as zero. Urethroscopy was done with 17 F sheath and 0° telescope. The site and length of the stricture along with the ability of telescope to pass through the stricture was noted on urethroscopy.
The procedure was performed under spinal anesthesia in lithotomy position. Antibiotic (Ciprofloxacin, 500 mg) was given just before and 12 h after procedure and continued for next 5 days. Normal saline was used for irrigation during the procedure.
The cold knife technique
The Sachse Urethrotome was introduced per urethra using a 21 F sheath and 0o telescope. It was advanced into the urethra up to the stricture site keeping the knife drawn in. If required a 5F guide wire or a ureteric catheter was introduced through the side channel to guide the urethrotome. The stricture was then incised open using the knife at 12’o clock position while withdrawing the instrument knife, simultaneously. The procedure was repeated till the stricture was adequately opened up.
The holmium laser technique
The holmium laser fiber was introduced through a side channel once the stricture was visualized by urethroscopy. The frequency was set at 7 Hertz and the power used was 13-15 watts. The fiber was positioned about 1 mm away from the tissue and the laser was fired at 12’o clock position or where the stricture was asymmetric until adequate caliber of urethra was attained comparable to the proximal urethra. The machine used was Odessy 30, the Pulsed CTH: YAG (Holmium: YAG) Laser machine with Laser Wavelength-2100 nm; Pulse Duration-350 to 700 μs and pulse energy-0.4 to 3.0 J.
Procedure was completed with cystoscopy. Post-procedure negotiation of telescope into the urinary bladder was taken as success of procedure. Operative time was recorded as the time interval beginning with insertion of optical urethrotome from external urethral meatus, continuing with procedure either by laser or cold knife, and ending with the removal of urethrotome from external urethral meatus. A 16-18 F silicone Foley catheter was inserted per urethra at the end of the procedure which was removed after 24 h followed by uroflowmetry. Visual analog pain score was used for the assessment of post-operative pain. Analgesic (Diclofenac sodium) was used if required. All patients were discharged on the second day.
Spontaneous voiding with peak flow rate more than 15 ml/seconds without any requirement of post- operative urethral dilatation was taken as a successful procedure. Patients were followed up in Out Patient Department on 15, 30, and 180 post-operative days. At each follow up visit uroflowmetry (repeated if voided volume was <200 ml) was performed. If the peak flow rate on uroflowmetry dropped to less than 15/seconds, urethral dilatation was performed. Suprapubic cystostomy tube was removed if patients who had it, maintained peak flow rate of more than 15 ml/s for more than 3 months. Reduction of peak flow rate to less than 10 ml/s during follow up was taken as failure of the procedure and these patients were offered to undergo another procedure.
Statistical Analysis
All parametric data were expressed as mean ± standard deviation. Independent sample t-test and Mann–Whitney U-tests were used for the comparison of parametric data when appropriate, while the Pearson's Chi-squared (χ2) test was used to compare the non-parametric data. A P < 0.05 was considered significant.
RESULTS
In the Holmium group, 23 patients had inflammatory, 16 patients had post-catheterization, and two patients had traumatic strictures, while etiology of stricture could not be decided in four patients. In Cold knife group, etiology of stricture in 19 patients was inflammatory, in 13 patients post-catheterization, in 8 patients traumatic and in five patients it was unknown [Figure 1]. In Holmium group, 10 patients had strictures in penile urethra, 13 patients had it in bulbar urethra, in 16 patients it was present at BM junction and it was present in posterior urethra in 6 patients. In Cold knife group, there were 11 patients with strictures in penile urethra and 9 patients in bulbar urethra; 20 patients had it at BM junction and 5 patients in posterior urethra [Figure 2]. On applying Pearson-chi squared test, it was concluded that the two groups were comparable with respect to age distribution, etiology of stricture, and site of stricture.
Figure 1.
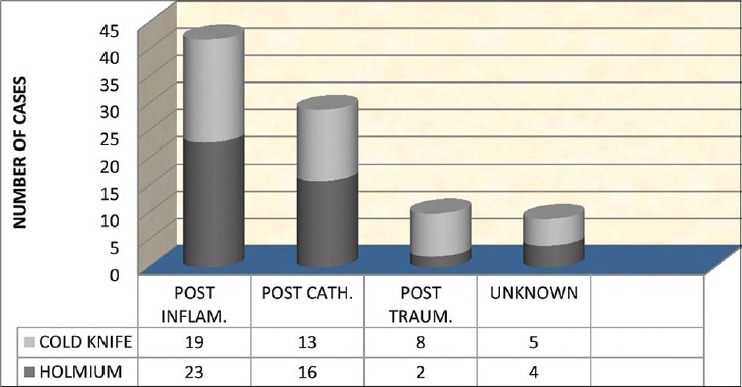
Etiology of Stricture
Figure 2.
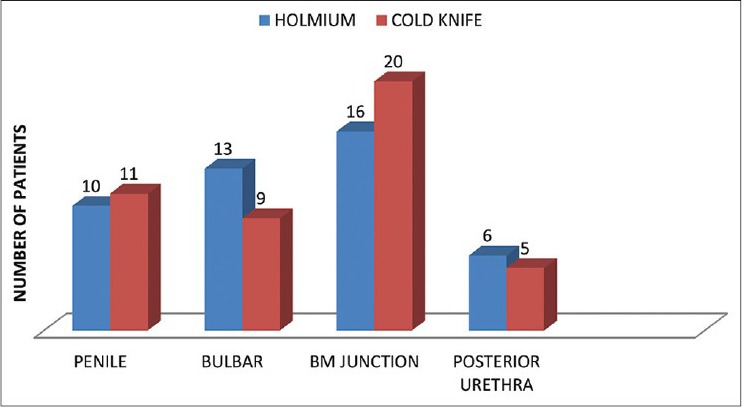
Stricture site
The peak flow rates were compared between the two groups pre- and post-operatively at 0, 1, 15, 30, and 180 days [Table 1]. At day 0, 1, 15 and 30, the difference between the means of PFRs was not statistically significant and was comparable. At 180 days (6 month interval) the difference between mean of PFR for Holmium and Cold knife group was statistically highly significant (P value <0.001) [Figure 3]. The percentage fall of PFR in the two groups was observed with each visit in the postoperative period [Figure 4]. Mann–Whitney test was applied and a statistically significant difference was observed in the fall of mean PFR at 6 months interval between the two groups (P value = 0.044).
Table 1.
Changes in peak flow rate
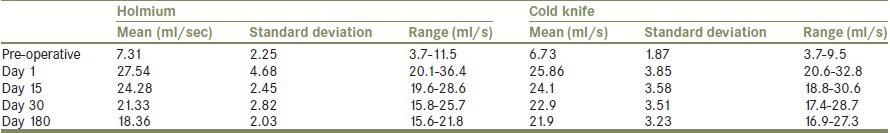
Figure 3.
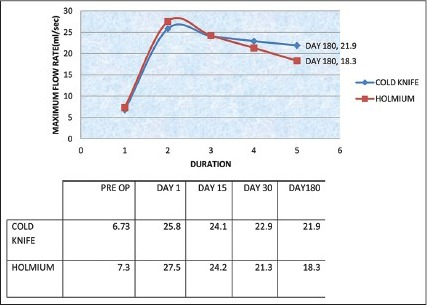
Changes in PFR
Figure 4.
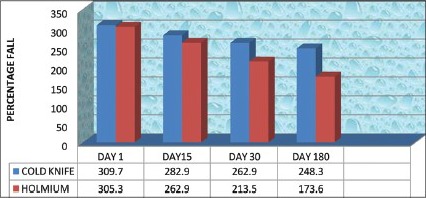
Mean PFR fall
In Group A (Holmium group), we were not able to negotiate telescope completely into the urinary bladder in eight patients (17.78%) which was indicative of incompleteness of the procedure, the mean operative time was 19.8 min (range 15-30 min), four patients (8.89%) had extravasations of irrigating fluid in the perineum which was managed conservatively and during follow up at sixth month, peak flow rate of less than 10 ml/s was recorded on uroflowmetry in six patients (13.33%) and regarded as recurrence. On the other hand, in Group B (Cold knife group), internal urethrotomy was completed successfully in all patients allotted under it, the mean operative time was 7.44 min (range 5-10 min.), seven patients (15.56%) had intra-operative bleeding which was managed well with perineal compression.
The Visual Analog Pain Score in Holmium group was 1 in 60% patients, 2 in 26.7% patients and 3 in 13.3 patients while in Cold knife group 80% patients scored 1, 6.7% scored 2 and 13.3% patients scored 3. None of the patients had pain score more than three in either group. The two groups were comparable for pain score.
DISCUSSION
Optical internal urethrotomy is one of the standard modalities of treatment in non-occlusive strictures for last four decades with varied success rates. There have been a few prospective randomized clinical trials in the recent past on comparative study of Holmium laser over conventional cold knife for internal urethrotomy. In a study, done by Atak et al.,[15] 51 male patients with single, iatrogenic, annular strictures of the urethra were randomly divided into two groups; 21 patients underwent urethrotomy with Ho: YAG laser and 30 patients underwent direct vision urethrotomy with cold-knife. The results obtained were analyzed and compared at 3 months, 6 months, 9 months, and 12 months postoperatively. Operative time was shorter in laser group (16.4-8.04 min) when compared with cold-knife group (23.8-5.47 min). Recurrence-free rate at 3 months was similar between two groups. However, recurrence-free rates thereafter were significantly higher in laser group when compared with cold-knife group. No complications were encountered in any study groups. Authors concluded Ho: YAG laser as safe and reliable as conventional cold-knife urethrotomy and our results are in concurrence with this study
A similar randomized comparative study was conducted by Dutkiewicz et al.,[16] in Poland. They objectively analyzed the results of urethrotomy using the Ho: YAG laser with classical urethrotomy (each group contained 25, without statistically significant differences in etiology of stricture, their number, localization, length, or relevant symptoms). Assessment of treatment effectiveness and complications were made on the basis of Uroflowmetry in the third, sixth, and twelfth months after treatment. The results obtained and their evaluation on the basis of adopted criteria did not confirm a higher treatment effectiveness of the Holmium laser Urethrotomy over the classical internal urethrotomy at 1-year follow-up.
In our study, 90 male patients, of age group 18-60 years were randomly divided into Holmium and Cold knife group, 45 patients in each arm. Based upon uroflowmetry, assessment of treatment effectiveness and complications were made at 6 months follow-up. Post-operative fall in the peak flow rate was noted during the follow up in both groups, but the rate of fall was different. Initially, on first post-operative day, peak flow rate in Holmium group was higher than Cold knife group, reached at parallel level at around day 15. Thereafter persistent fall in peak flow rate in uroflowmetry was observed in Holmium group compared to Cold Knife Group and at the end of sixth month, the difference was statistically significant indicating persistent effect of urethrotomy in later group.
In short segment stricture, it is possible to divide fibrous tissue completely with cold knife separating the scarred epithelium so that the healing occurs by secondary intention. The sense of depth perception is lacking with Holmium, responsible for inadequate cutting or over cutting, leading to complications in the form of extravasations of irrigating fluid, an early complication, as was observed in four cases (8.89%) in our study and recurrence of stricture later on due to fibrosis. We preferred a lower frequency, 7 Hz, to minimize deep tissue penetration and coagulation on urethra. In eight patients (17.78%), we were not able to open up the stricture completely because of eccentric position and difficulty in sighting the laser beam during urethrotomy with Holmium laser. Working with Holmium laser is technically demanding as it is not possible to pass guide wire through cystoscope across the stricture while using laser fiber; while, handling both simultaneously with guide wire passed outside the cystoscope sheath is difficult.
Untreated perioperative urinary infection increases the recurrence rate significantly, from 28% if uninfected to 72% if infected, and use of antibiotic might reduce recurrence.[9] We used perioperative antibiotic (Ciprofloxacin) and thereafter prescribed it for 5 days following operation.
Our mean operative time for Holmium group [19.8 min (range 15-30 min)] is comparable to the study of Atak et al.,[15] (16.4-8.04 min). Kamal[17] reported mean (range) operative time as 22.3 (15 ± 35) min, working with diode laser. With Cold knife mean operative time of 7.44 min (range 5-10 min) is much shorter than the study of Atak et al.,[15] (23.8-5.47 min).
The complications associated with internal urethrotomy include bleeding, UTI, urosepsis, extravasation, incontinence, impotence, and recurrence of stricture.[18] The overall post-operative complications in our study were seen in 12.22% of cases. All were minor in nature; seven patients had bleeding in Cold knife group during the procedure which was managed well and four patients developed extravasations of irrigating fluid in perineum in Holmium group. None of the patients had pain score more than 3 on Visual Analog Pain Score.
Duration of urethral catheterization after internal urethrotomy is still a controversial issue. In the literature, this duration ranges from 24 h up to 3 months.[9] Postoperative prolonged urethral catheterization is accepted as the most important risk factor for urinary tract infections.[16] To avoid related complications, we performed urethral catheterization for 24 h in our study. Kamp[15] reported that the stricture site, operative time, and the duration of catheterization had no impact on the recurrence of stricture or success of treatment.
Various techniques have been employed to follow up patients following visual internal urethrotomy. These include urethral calibration with a catheter, uroflowmetry, flexible cystourethroscopy, AUA symptom index and urethrographic studies, and the need for a repeat procedure.[9] There is no uniformly accepted method of follow up. Hussain et al.,[18] defined excellent result as catheter free status with Q max more than 15 ml/s and no requirement for any other intervention. In our study, reduction of peak flow rate to less than 10 ml/s in uroflowmetry during follow up was taken as failure of the procedure.
In a meta analysis done by Tao et al.,[19] a total of 44 articles, including of 3230 cases were reviewed. Success rate of patients treated with laser was 74.9% (371/495) compared with 68.5% (1874/2735) with cold knife. Santucci[20] showed a success rate of only 8% for the first urethrotomy, repeat urethrotomy, upto five procedures, also had poor success rates ranging from 0 to 9% and recommended that urethrotomy should be reserved as a temporizing measure for poor surgical candidates or until further reconstruction can be planned and executed.
In our study, recurrence was high in Holmium group (in 6 out of 45 patients) and none for Cold knife group, which may be due to shorter duration of follow up.
CONCLUSION
Both, cold knife and holmium laser, have been effective in providing immediate relief to patients with single and short segment (<2 cm long) urethral strictures but more sustained response was attained in those undergoing procedure with the cold knife. Holmium laser is technically more demanding and its operative period is twice longer than cold knife for internal urethrotomy. The complications of both modalities are low and easily manageable. As the course of urethral stricture recurrence is rather long spreading over many years, further comparative studies with longer follow ups are required to compare the two modalities.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Das S. Urology in ancient India. Indian J Urol. 2007;23:2–5. doi: 10.4103/0970-1591.30253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peterson AC, Webster GD. Management of urethral stricture disease: Developing options for surgical intervention. BJU Int. 2004;94:971–6. doi: 10.1111/j.1464-410X.2004.05088.x. [DOI] [PubMed] [Google Scholar]
- 3.Tavakkoli Tabassi K, Yarmohamadi A, Mohammadi S. Triamcinolone injection following internal urethrotomy for treatment of urethral stricture. Urol J. 2011;8:132–6. [PubMed] [Google Scholar]
- 4.Singh O, Gupta SS, Arvind NK. Anterior urethral strictures: A brief review of the current surgical treatment. Urol Int. 2011;86:1–10. doi: 10.1159/000319501. [DOI] [PubMed] [Google Scholar]
- 5.Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA. 10th ed. Philadelphia: Elsevier Saunders; 2012. Campbell-walsh urology; pp. 967–73. [Google Scholar]
- 6.Myers JB, McAninch JW. Perineal urethrostomy. BJU Int. 2011;107:856–65. doi: 10.1111/j.1464-410X.2011.10139.x. [DOI] [PubMed] [Google Scholar]
- 7.Ghosh B, Dorairajan LN, Kumar S, Manikandan R, Muruganandham K, Kumar A. Randomized clinical trial comparing effectiveness of intracorpusspongiosum block versus topical anesthesia for performing visual internal urethrotomy for urethral stricture disease. Urology. 2013;81:204–7. doi: 10.1016/j.urology.2012.09.020. [DOI] [PubMed] [Google Scholar]
- 8.Kumar S, Prasad S, Parmar K, Ganesamoni R, Batra YK. A randomized controlled trial comparing combined spongiosum block and intraurethral lignocaine with intraurethral lignocaine alone in optical internal urethrotomy for urethral stricture. J Endourol. 2012;26:1049–52. doi: 10.1089/end.2011.0583. [DOI] [PubMed] [Google Scholar]
- 9.Dubey D. The current role of direct vision internal urethrotomy and self-catheterization for anterior urethral strictures. Indian J Urol. 2011;27:392–6. doi: 10.4103/0970-1591.85445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heyns CF, van der Merwe J, Basson J, van der Merwe A. Treatment of male urethral strictures-possible reasons for the use of repeated dilatation or internal urethrotomy rather than urethroplasty. S Afr J Surg. 2012;50:82–7. doi: 10.7196/sajs.1081. [DOI] [PubMed] [Google Scholar]
- 11.Smith P, Dunn M, Dounis A. Sachse optical urethrotome in management of urethral stricture in the male: Preliminary communication. J R Soc Med. 1978;71:596–9. doi: 10.1177/014107687807100810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saavedra-Briones DV, Merayo-Chalico CE, Sanchez-Turati G, Cantellano-Orozco M, Shuck-Bello C, Camarena-Reynoso HR, et al. Urethral stricture recurrence following internal urethrotomy. Rev Mex Urol. 2009;69:153–8. [Google Scholar]
- 13.Jabłonowski Z, Kedzierski R, Miekoś E, Sosnowski M. Comparison of neodymium-doped yttrium aluminum garnet laser treatment with cold knife endoscopic incision of urethral strictures in male patients. Photomed Laser Surg. 2010;28:239–44. doi: 10.1089/pho.2009.2516. [DOI] [PubMed] [Google Scholar]
- 14.Herrmann TR, Liatsikos EN, Nagele U, Traxer O, Merseburger AS. EAU Guidelines Panel on Lasers, Technologies. EAU Guidelines on Laser Technologies. Eur Urol. 2012;61:783–95. doi: 10.1016/j.eururo.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 15.Atak M, Tokgoz H, Akduman B, Erol B, Donmez I, Hancı V, et al. Low-power holmium: YAG laser urethrotomy for urethral stricture disease: Comparison of outcomes with the cold-knife technique. Kaohsiung J Med Sci. 2011;27:503–7. doi: 10.1016/j.kjms.2011.06.013. [DOI] [PubMed] [Google Scholar]
- 16.Dutkiewicz SA, Wroblewski M. Comparison of treatment results between holmium laser endourethrotomy and optical internal urethrotomy for urethral stricture. Int Urol Nephrol. 2012;44:717–24. doi: 10.1007/s11255-011-0094-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kamal BA. The use of the diode laser for treating urethral strictures. BJU Int. 2002;87:831–3. doi: 10.1046/j.1464-410x.2001.02183.x. [DOI] [PubMed] [Google Scholar]
- 18.Hussain M, Lal M, Askari SH, Hashmi A, Rizvi SA. Holmium laser urethrotomy for treatment of traumatic stricture urethra: A review of 78 patients. J Pak Med Assoc. 2010;60:829–32. [PubMed] [Google Scholar]
- 19.Jin T, Li H, Jiang LH, Wang L, Wang KJ. Safety and efficacy of laser and cold knife urethrotomy for urethral stricture. Chin Med J (Engl) 2010;123:1589–95. [PubMed] [Google Scholar]
- 20.Santucci R, Eisenberg L. Urethrotomy Has a much lower success rate than previously reported. J Urol. 2010;183:1859–62. doi: 10.1016/j.juro.2010.01.020. [DOI] [PubMed] [Google Scholar]


