Abstract
We report the case of a 15-year-old male, presenting with recurrent gross hematuria complicated by acute anemia. Cystoscopy showed little bleeding from the left ureteral orifice. Diagnosis of left renal vein compression at the aortomesenteric space was established through color Doppler ultrasonography and computed tomographic angiography. Therapeutic attitude was interventionist in our case, performing successful management with modified medial nephropexy, with a retroperitoneal approch. To the best of our knowledge, we report the second case of left medial nephropexy for treatment of the anterior nutcracker syndrome. The first case of modified medial nephropexy was done by lowering the left renal vein from its initial position in the aortomesenteric angle through a restrict retroperitoneal approach.
Keywords: Anterior nutcracker syndrome, medial nephropexy, retroperitoneal approach
INTRODUCTION
The anterior nutcracker syndrome refers to compression of the left renal vein between the aorta and superior mesenteric artery. The syndrome is an unusual cause of hematuria; it can also manifest as left flank abdominal pain, and occasionally a varicocele among men.
Different treatments have been proposed for this syndrome. Medial nephropexy, with excision of the renal varicosities through a middle incision is a known modality of treatment for the Neurocutaneous Syndrome (NCS), which was first described by Wendel, in 1980[1]. The aim of this procedure was to correct the posterior ptosis, (assumed to be the cause of NCS) and excise the varices, which were deemed to be the consequence of renal malpositioning. However, simple nephropexy with excision of the varicosities is no more recommended, as it fails to address the primary pathology.[2]
To the best of our knowledge, we report here, the second reported case of left medial nephropexy for treatment of the anterior nutcracker syndrome, with a new modification of the technique, by lowering the left renal vein from its initial position in the aortomesenteric space through a restricted retroperitoneal approach.
CASE REPORT
A 15-year-old male was admitted to the Emergency Service for support of gross hematuria complicated by acute anemia; there were no associated symptoms.
When we asked him again, he reported continuous total hematuria since four years, continuous pelvic and abdominal pain, headache, and fatigue a long time ago, with daily use of increasing doses of analgesics, with no therapeutic success despite a long investigational history, combined with several imaging examinations and laboratory tests.
On physical examination, only a higher bilateral varicocele was detected.
The initial blood tests showed hemoglobin of 8.2 g/dl. The coagulation test results were normal. The patient was resuscitated and transfused.
Abdominal and renal ultrasonography showed a normal renal size, outlined with no other anatomical defects.
The cystoscopic examination showed bloody urine emerging from the left ureteral orifice.
The next day, computed tomographic angiography (CTA) was performed and concluded with a compression of the left renal vein between the aorta and the superior mesenteric artery. The post-anterior diameter of the hilar portion and that of the aorticomesenteric stenotic portion of the left renal vein (LRV) were 9.8 mm and 1.7 mm, respectively, revealed by a grayscale ultrasound, which, with peak velocities, was demonstrated by a spectral Doppler of 25 cm/second and 88 cm/second, respectively. The diameter ratio and the peak velocity ratio between the dilated portion and the stenotic portion were 4.5 and 3.4. The diagnosis of an anterior nutcracker syndrome was suggested [Figures 1 and 2]. The patient refused our suggestion of taking renal venography for further evaluation.
Figure 1.
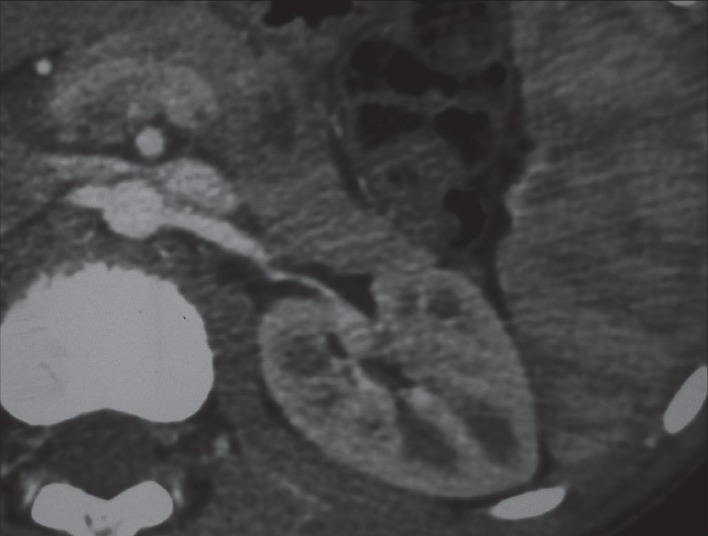
Computer tomography angiography demonstrates compression of the left renal vein between the aorta and superior mesenteric artery with dilation of the distal part of the left renal vein on the axial cuts
Figure 2.
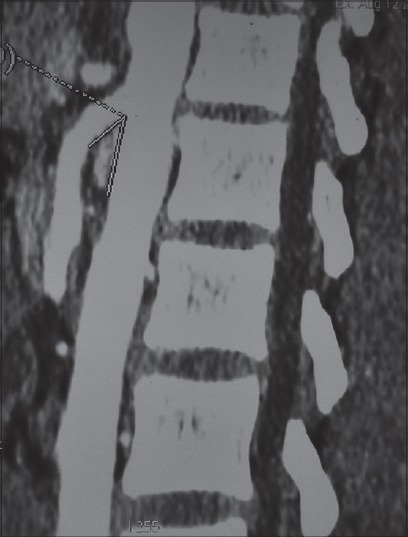
CT angiography demonstrates the acute angle between the aorta and superior mesenteric artery
Surgery was suggested. However, the patient refused, and was lost to follow up thereafter.
Three months after, he presented with a second painless gross hematuria (hemoglobin 7 g/dl).
Surgical exploration through a large lobotomy was conducted. The Gerota's fascia was incised and the perinephric fat was sharply dissected off the renal capsule. The left renal vein was carefully isolated from the surrounding tissue. The dilated gonadal, adrenal, and lumbar veins were identified, ligated, and transected at their insertion on the left renal vein. Careful dissection of the renal artery was performed toward the aorta. The ureter tube was dissected and isolated.
The superior mesenteric artery (SMA) was elevated easily from the left renal vein and an apparent compressed vein was noted. The left renal vein was lowered 2 cm from its initial position between the aorta and the superior mesenteric artery. The kidney was lowered and a medial nephropexy with forward fixation to the fascia of the psoas muscle was performed. Care was taken to avoid positioning the kidney so as to produce an obstruction of the ureter.
The patient had an uneventful postoperative hospital course and was discharged from the hospital two weeks later. The hematuria disappeared on the fourth postoperative day. Repeated Color Doppler ultrasonography of the LRV, one week and one month after operation, showed normal blood flow. A CT scan, performed one month later, showed no compression of the left renal vein with normal aspect of the kidney, except for a small hematoma at the upper pole of the kidney [Figure 3] that disappeared on the following scan.
Figure 3.
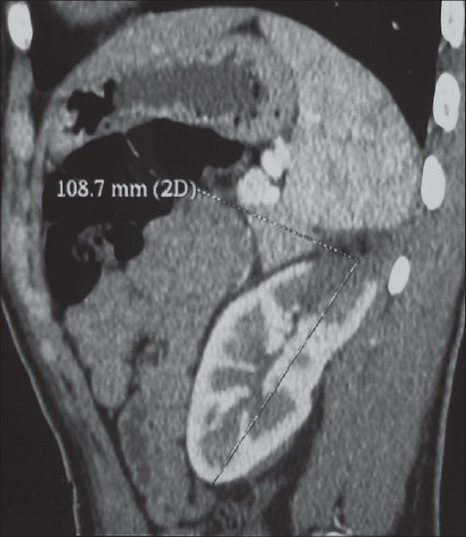
CT scan performed one month later shows the normal aspect of the kidney, except a little hematoma at the upper pole of the kidney and no compression of the left renal vein
At the 20-month follow up, the patient is doing well, without recurrence of hematuria or lumbar pain. The last Color Doppler ultrasonography of the LRV shows normal blood flow, without compression [Figure 4]. The CT scan shows a normal aspect of the kidney and no compression of the LRV. The patient remains asymptomatic and has returned to his usual life. The varicocele has improved significantly after the operation.
Figure 4.
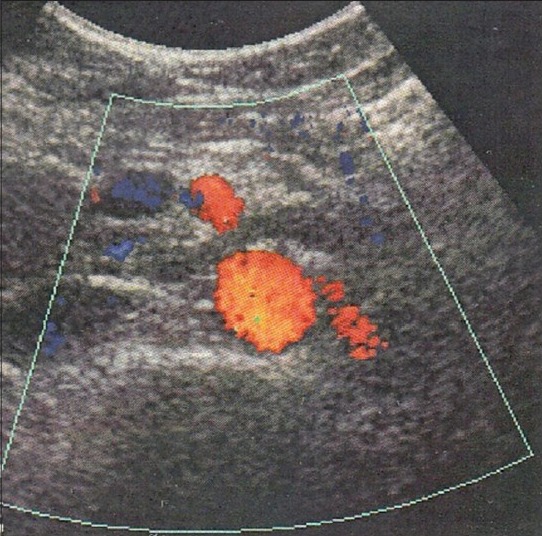
Doppler ultrasonography of the left renal vein showed normal blood flow without compression
DISCUSSION
The Nutcracker Syndrome (NCS), in its anterior form, is caused by a compression of the left renal vein between the aorta and the superior mesenteric artery (SMA).[3] This results in left renal venous hypertension and the subsequent development of venous varicosities of the renal pelvis, ureter, and gonadal vein. The true prevalence of the Nutcracker Syndrome remains unknown and it may be underdiagnosed. The NCS can manifest as hematuria and/or left flank abdominal pain and occasionally a varicocele among men.
When the diagnosis is suspected, the detection of the NCS can be made by several newer imaging modalities. Computed tomographic angiography and magnetic resonance angiography have powerful abilities for providing accurate, three-dimensional reconstructive images in any desired plane and allowing better identification of these anomalies. Spectral Doppler ultrasound can give more details of the hemodynamics of the LRV at the site of compression.[4]
Cystoscopy performed in the acute phase of haematuria showed an unilateral left hematuria.
Treatment of the NCS is controversial. Different treatment options have been proposed for this syndrome, including follow-up, conservative treatment, and surgical therapy.
The available surgical procedures include intra- or extravascular stents[5] and open surgical procedures employed to rectify the problem include, the transposition of the left renal vein[6] transposition of the superior mesenteric artery[7] renal autotransplantation[8] and gonadocaval bypass[9] or nephrectomy, when there is severe organ damage.[10] The indications for laparoscopic surgery continue to expand for the treatment of the Nutcracker Syndrome: Retroperitoneal laparoscopic nephrectomy with ex-vitro autograft repair and autotransplantation[11] laparoscopic splenorenal venous bypass[12] laparoscopic extravascular renal vein stent placement[13] and laparoscopic inferior mesenteric-gonadal vein bypass.[14]
Medial nephropexy with excision of the renal varicosities through a middle incision as a known modality for the treatment of NCS, was first described in a 45-year-old woman, by Wendel, in 1980[1] but the surgical technique was not well described, the author did not mention if he lowered the LRV or not.
Nephropexy with excision of varicosities is no more recommended by some authors, because it fails to correct the underlying pathology. The authors explain that the aim of this procedure (simple nephropexy with excision of varicosities) is to correct posterior ptosis (assumed to be the cause of NCS) and excise the varices, which are deemed to be the consequence of renal malpositioning, but it fails to address the primary pathology.[2]
Medial nephropexy was not considered as an etiological treatment of NCS in the absence of lowering the LRV to avoid the compression, which is not the case in our patient, in whom the LRV was lowered from its initial position in the aortomesenteric space. Here we report the second case of this kind of surgery, but with lowering of the LRV through a large lobotomy and a retroperitoneal approach, in an adolescent male, with good results after 19 months of follow up.
Compared to the other open approaches (laparotomy), medial nephropexy with excision of the renal varicosities and lowering of the LRV through a large lobotomy and a retroperitoneal approach is feasible, with a lower chance of lesions in the intraperitoneal organs.
On the basis of the advantages of retroperitoneal surgery with lowering of the LRV, this approach should be recommended and should become an alternative method for anterior Nutcracker Syndrome repair in young patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Wendel RG, Crawford ED, Hehman KN. The Nutcracker phenomenon; an unusual cause for renal varicosities with hematuria. J Urol. 1980;123:761–3. doi: 10.1016/s0022-5347(17)56121-2. [DOI] [PubMed] [Google Scholar]
- 2.Ahmed K, Sampath R, Khan MS. Current trends in the diagnosis and management of renal nutcracker syndrome: A review. Eur J Vasc Endovasc Surg. 2006;31:410–6. doi: 10.1016/j.ejvs.2005.05.045. [DOI] [PubMed] [Google Scholar]
- 3.Lau X, Lo R, Chan FL, Wong KK. The posterior: Hematuria secondary to retroaortic left renal vein. Urology. 1986;28:437–9. doi: 10.1016/0090-4295(86)90085-3. [DOI] [PubMed] [Google Scholar]
- 4.Luo XL, Qian GN, Xiao H, Zhao CL, Zhou XD. Posterior nutcracker syndrome associated with interrupted left inferior vena cava with azygos continuation and retroaortic right renal vein. Korean J Radiol. 2012;13:345–9. doi: 10.3348/kjr.2012.13.3.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnes R, Fleisher Hr, Redman J, Smith JW, Harshfield DL, Ferris EJ. Mesoaortic compression of the left renal vein (the so-called nutcracker syndrome): Repair by a new stenting procedure. J Vasc Surg. 1988;8:415–21. doi: 10.1067/mva.1988.avs0080415. [DOI] [PubMed] [Google Scholar]
- 6.Stewart BH, Reiman G. Left renal venous hypertension «nutcracker» syndrome: Managed by direct renocaval reimplantation. Urology. 1982;20:365–9. doi: 10.1016/0090-4295(82)90457-5. [DOI] [PubMed] [Google Scholar]
- 7.Thompson P, Darling RR, Chang B, Shah DM, Leather RP. A case of nutcracker syndrome: Treatment by mesoaortic transposition. J Vasc Surg. 1992;16:663–5. doi: 10.1016/0741-5214(92)90176-9. [DOI] [PubMed] [Google Scholar]
- 8.Chuang C, Chu S, Lai P. The nutcracker syndrome managed by autotransplantation. J Urol. 1997;157:1833–4. [PubMed] [Google Scholar]
- 9.El-Sadr AR, Mina E. Anatomical and surgical aspects in the operative management of varicoceles. Urol Cut Rev. 1950;54:257–62. [PubMed] [Google Scholar]
- 10.Russo D, Minutotto R, Iacavino V. Gross hematuria of un-unknown origin: The nutcracker syndrome. Am J Kidney Dis. 1998;32:23–9. doi: 10.1053/ajkd.1998.v32.pm10074588. [DOI] [PubMed] [Google Scholar]
- 11.Xu D, Liu Y, Gao Y, Zhang L, Wang J, Che J, et al. Management of renal nutcracker syndrome by retroperitoneal laparoscopic nephrectomy with ex vivo autograft repair and autotransplantation: A case report and review of the literature. J Medi Case Rep. 2009;3:82. doi: 10.1186/1752-1947-3-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chung BI, Gill IS. Laparoscopic splenorenal venous bypass for nutcracker syndrome. J Vasc Surg. 2009;49:1319–23. doi: 10.1016/j.jvs.2008.11.062. [DOI] [PubMed] [Google Scholar]
- 13.Zhang Q, Zhang Y, Lou S, Liu F, Ye Z, Zhang D. Laparoscopic extravascular renal vein stent placement for nutcracker syndrome. J Endourol. 2010;24:1631–5. doi: 10.1089/end.2010.0001. [DOI] [PubMed] [Google Scholar]
- 14.Xu D, Gao Y, Chen J, Wang J, Ye J, Liu Y. Laparoscopic inferior mesenteric-gonadal vein bypass for the treatment of nutcracker syndrome. J Vasc Surg. 2013;57:1429–31. doi: 10.1016/j.jvs.2012.10.092. [DOI] [PubMed] [Google Scholar]


