Abstract
Background
Recently lumbopelvic control has been linked to pitching performance, kinematics and loading; however, poor lumbopelvic control has not been prospectively investigated as a risk factor for injury in baseball pitchers.
Hypothesis
Pitchers with poor lumbopelvic control during spring training are more likely to miss 30 or more days due to injury through an entire baseball season than pitchers with good lumbopelvic control.
Study design
Cohort study.
Methods
Three hundred forty-seven professional baseball pitchers were enrolled into the study during the last 2 weeks of spring training and stayed with the same team for the entire season. Lumbopelvic control was quantified by peak anterior-posterior deviation of the pelvis relative to starting position during a single leg raise test (APScore). Days missed due to injury through the entire season were recorded by each team's medical staff.
Results
Higher APScore was significantly associated with a higher likelihood of missing 30 days or more (Chi-Square, p=0.023). When divided into tertiles based on their APScore, participants in the highest tertile were 3.0 times and 2.2 times more likely to miss at least 30 days throughout the course of a baseball season relative to those in the lowest or middle tertiles, respectively. Higher APScore was also significantly associated with missing more days due to injury within participants who missed at least one day to injury (ANOVA, p=0.018), with the highest tertile missing significantly more days (mean=98.6 d) than the middle tertile (mean=45.8d, p=0.017) or the lowest tertile (mean=43.8, p=0.017).
Conclusion
This study found that poor lumbopelvic control in professional pitchers was associated with increased risk of missing significant time due to injury.
Keywords: core stability, pelvis, lumbar spine, balance, athlete
Introduction
Injury is a significant problem for pitchers at all levels of baseball. There is a high risk of injury in youth baseball pitchers, with 26-35% of youth pitchers reporting elbow or shoulder pain each season18, 19. This risk extends to Major League Baseball with pitchers losing an average of 22 days per season due to injury8. Identification of biomechanical risk factors to mitigate pitching injuries in children and professionals alike has focused on stresses and loads at the elbow and shoulder10, 11, 17, 22. However, due to the fact that pitching is a whole-body motion requiring the coordination and control of all segments and joints, researchers, clinicians and coaches alike have theorized that deficiencies in the neuromuscular control of the lower extremities, pelvis and trunk may contribute to the etiology of these elbow and shoulder injuries.
The lumbopelvic region, including the “core” muscles crossing the lumbar spine and abdomen as well as the muscles crossing the hip joints, has received considerable attention in particular due to its location bridging the legs to the arms. All of the muscles of this region can influence motion of the pelvic girdle in the sagittal as well as frontal and transverse planes. MacWilliams et al. observed that stronger ground forces correlated with faster pitches, suggesting that a significant component of the energy required to throw a pitch is generated in the lower body20. Putnam described the concept of an ideal “proximal-to-distal sequence of segment motions” whereby the angular velocity of each distal segment builds upon the angular velocity of its proximal segment, which suggests that control of the proximal segment will affect motion of the distal segment29. Similarly, Kibler theorized that the lumbopelvic region provides “proximal stability for distal mobility,” meaning that by remaining stable it can provide a platform for the distal segments to pull against and accelerate16. Based on these theoretical underpinnings, we define lumbopelvic control as the ability to actively mobilize or stabilize the lumbopelvic region in response to internally or externally generated perturbations. Several research groups have investigated lumbopelvic control, motion and muscle activity to identify their associations to throwing velocity and loads on the shoulder and elbow. Opening the pelvis and torso toward home plate earlier30, tilting the trunk forward more at ball release21, and increased contralateral trunk tilt to bring the throwing shoulder over the lead foot28 were all associated with higher pitch velocity, but rotating the trunk towards home plate1, 2 and increased contralateral trunk tilt28 were also associated with increased shoulder axial rotation and elbow valgus loads. The lower extremity muscles are very active during a baseball pitch4, and the gluteal muscle activation patterns of both the drive and stride legs are consistent with controlling pelvis rotation26. These biomechanical studies combined are all consistent with a significant role for lumbopelvic control in baseball pitching.
Early retrospective and prospective data further support the concept that lumbopelvic control may contribute to safe and successful baseball pitching. Reviews of Major League Baseball disabled list reports from 1989-2010 have observed that 4.5% of all injuries to pitchers involve abdominal muscle strains, suggesting that pitchers are placing significant demand on the abdominal muscles8, 9. Lumbopelvic control has been positively associated with pitching performance as well using a standing single leg raise test, as pitchers with better lumbopelvic control pitched significantly more innings and had significantly lower walks plus hits per inning pitched than those with poor lumbopelvic control6.
While the above mentioned studies all are consistent with a role for lumbopelvic control in baseball pitching, it remains unknown whether lumbopelvic control is associated with injury rates in baseball pitchers. This information would provide valuable insight into prevention and rehabilitation programs for these athletes. Therefore, the purpose of this study was to test the hypothesis that poor lumbopelvic control, as measured by performance on the single leg raise test, would be associated with a higher likelihood of a pitcher developing injuries over the course of a professional baseball season.
Methods
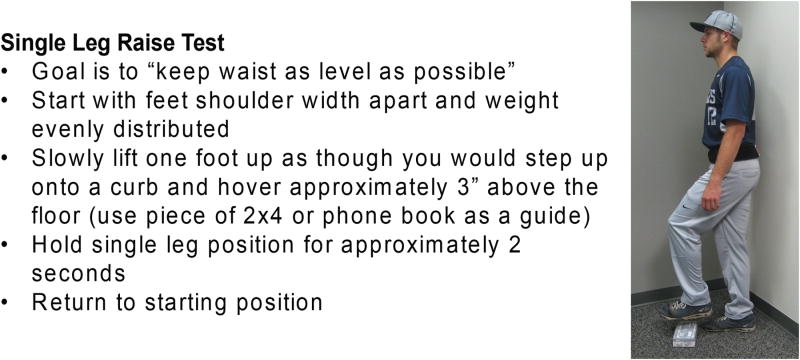
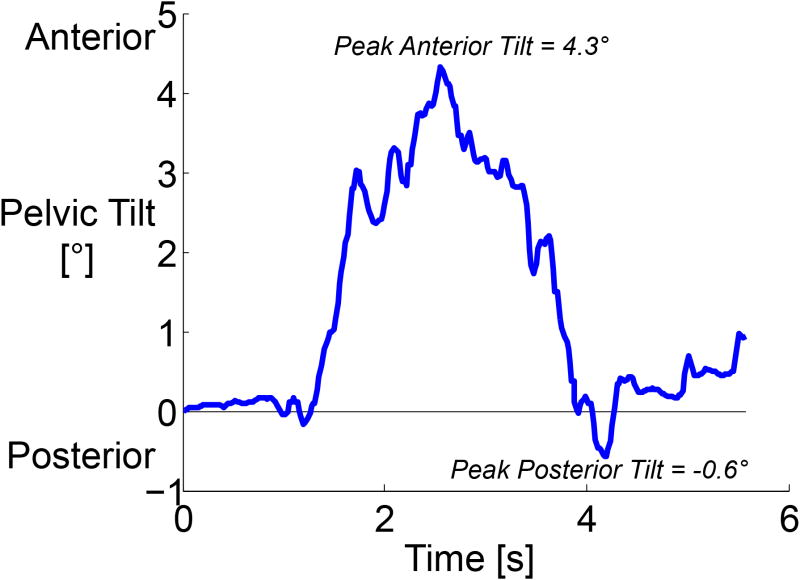
Four hundred and five professional baseball pitchers from five Major League Baseball organizations were initially enrolled in this study during the last 2 weeks of spring training before the 2011 and 2012 baseball seasons. The 347 pitchers who remained with the same organization for the entire season were included in subsequent analysis. All provided IRB-approved informed consent in either English or Spanish. All participants subsequently competed at the developmental, Minor League, or Major League level during the season. Participants arrived at their respective training facility prior to any conditioning that day and performed a previously-described standing single leg raise test6. In this test, participants stood with weight evenly distributed on both feet, lifted the foot of their stride leg approximately 10 cm, held that single-leg stance position for 2 seconds, and then returned to double-leg-stance under control (Figure 1). This test mimics the initiation of movement to step up onto a curb or to begin a pitching motion, and it requires the participant to shift weight to a single leg. The anterior-posterior deviation of the pelvis from its starting position relative to the horizon was measured in degrees using an iPod-based tilt sensor (Level Belt Pro, Perfect Practice, Inc.), and the largest peak absolute pelvic tilt from the starting position was recorded for future analysis (APScore, Figure 2). All measurements were made by a single rater (CSM) and were not shared with the participants, coaches or medical personnel.
Figure 1.
Single leg raise test description
Figure 2.
Plot of anterior-posterior pelvic tilt during a single leg raise test for a typical pitcher. APScore is defined as the largest deviation away from zero. In this example, the peak anterior tilt was 4.3° while the peak posterior tilt was -0.6°, leading to an APScore of 4.3°.
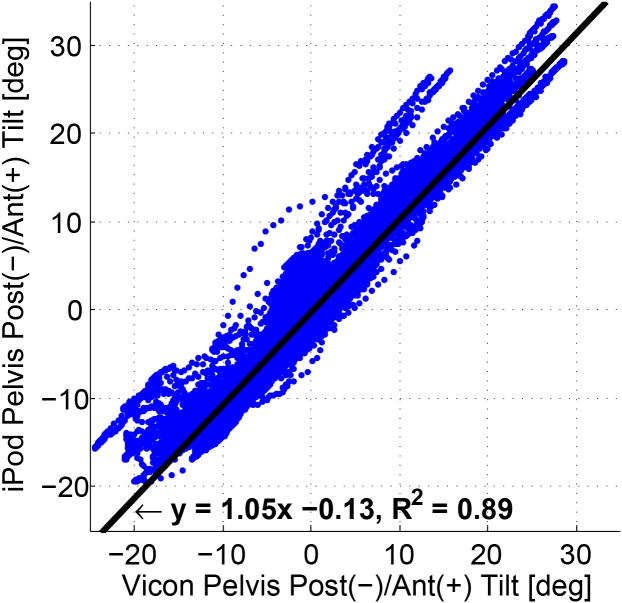
The iPod-based tilt sensor has previously been validated for measuring standing pelvic tilt against 3D motion analysis7, and the single leg raise test has been shown to have excellent intra-rater reliability.31 Brief summaries of these validation and reliability experiments are provided here. Validation of the iPod-based tilt sensor was performed on 10 healthy subjects after providing IRB-approved informed consent. Anterior-posterior pelvic tilt angles during a standing anterior-posterior pelvic range of motion task and a single leg raise task were simultaneously measured with the iPod-based tilt sensor and an opto-electronic 3D motion analysis system (10 Vicon MX-F40, Vicon Corporation) with retroreflective markers placed over the anterior and posterior superior iliac spines (ASIS, PSIS). An anatomical coordinate system was created from the 4 markers to calculate pelvic tilt relative to the horizon. Opto-electronic and iPod-based datasets were synchronized in time using the peak anterior pelvic tilt in the range of motion task, and anterior-posterior pelvic tilt was defined to be zero at the time when the iPod began recording. Regression analysis of all anterior-posterior tilt data from the iPod vs. Vicon for all subjects demonstrated very strong correlation (R2=0.89) with a slope of 1.053±0.001 (Figure 3).7 The iPod-based sensor also showed very high sensitivity, specificity, and accuracy at detecting movement beyond thresholds from 2-10° (Table 1).7 This validation experiment also demonstrates that a single leg raise test may be performed by any appropriate tool to measure pelvic anterior-posterior tilt.
Figure 3.
Plot of anterior-posterior pelvic tilt during ROM and single leg raise movements measured by the iPod-based sensor v. the 3D motion analysis system with linear regression equation displayed. Reproduced from Chaudhari et al.7
Table 1.
Sensitivity, specificity and accuracy of the iPod-based sensor in determining if absolute anterior-posterior tilt of the pelvis away from the starting position exceeded thresholds between 2-10°. Reproduced from Chaudhari et al.7
| Anterior/Posterior Tilt Detection | |||||
|---|---|---|---|---|---|
| Threshold | 2° | 4° | 6° | 8° | 10° |
| Sensitivity | .92 | .92 | .95 | .97 | .93 |
| Specificity | .75 | .89 | .96 | .98 | .99 |
| Accuracy | .83 | .90 | .96 | .98 | .98 |
Intra-rater reliability of the single leg raise test was performed on the same 10 healthy subjects. Two trained raters each placed the belt containing the iPod-based tilt sensor over the subject's ASIS and PSIS three independent times. After placing the belt, the rater read the identical instructions for performing the single leg raise (Figure 1) and administered the test two or more times with each leg. Then the belt was removed and re-applied. Within each belt placement, the two repetitions for each leg were averaged, and intra-rater reliability was assessed by comparing the average single leg raise APScore using Cronbach α. Intra-rater reliabilities for the two raters were 0.885 and 0.932, respectively.31
Through the course of the season, medical staff from each baseball organization recorded days missed within the organization's own electronic medical record. A time-loss methodology was used14, where a day missed was defined as any day in which a participant was unable to complete his scheduled work due to a musculoskeletal injury suffered during baseball-related activity, whether that schedule included a desired number of pitches in practice, bullpen activity or competition. A day normally scheduled for rest after a game appearance was not counted as a day missed, nor was a day missed due to illness or an off-the-field injury such as a motor vehicle accident. Contusions and fractures attributable to collisions and blisters on the hand were also excluded from consideration. After completion of the season, these days missed due to injury and all game participation data were compiled for all participants who remained with the same organization for the entire season. Participants who retired during the season, were traded or released were excluded due to the lack of a complete dataset, leaving 347 participants (86% of those initially enrolled) for subsequent analysis (23.3±2.9 years old). A listing of the injuries reported is provided in Table 2.
Table 2.
Diagnoses for days missed as noted in the medical record by each team's medical personnel and number of pitchers who experienced each diagnosis.
| Region | Diagnosis | Number of Pitchers |
|---|---|---|
| Elbow | Avulsion | 1 |
| Biceps Strain | 1 | |
| Epicondylitis | 1 | |
| Flexor Strain | 5 | |
| Forearm Tightness | 2 | |
| Loose Body | 1 | |
| Strain (unspecified) | 11 | |
| Stress Fracture | 1 | |
| Tendonitis (unspecified) | 1 | |
| Triceps Tendinopathy | 1 | |
| UCL Sprain | 6 | |
| UCL Tear/Reconstruction | 12 | |
| Shoulder | Biceps Strain | 3 |
| Debridement | 1 | |
| Impingement | 1 | |
| Labrum Tear/Repair | 1 | |
| Posterior (unspecified) | 2 | |
| Rotator Cuff (unspecified) | 2 | |
| Rotator Cuff Surgery | 1 | |
| Rotator Cuff Tendonitis | 2 | |
| Strain (unspecified) | 3 | |
| Tendonitis (unspecified) | 11 | |
| Unspecified | 16 | |
| Back/Trunk | Core Muscle Sports Hernia | 1 |
| Intercostal Strain | 1 | |
| Latissimus (unspecified) | 5 | |
| Low Back Pain | 2 | |
| Low Back Strain | 1 | |
| Lumbar Spine (unspecified) | 5 | |
| Oblique (unspecified) | 2 | |
| Oblique Strain | 2 | |
| Thoracic Outlet | 1 | |
| Leg | Ankle Sprain | 3 |
| Gluteal Strain | 1 | |
| Groin (unspecified) | 1 | |
| Groin Strain | 4 | |
| Hamstring Strain | 5 | |
| Hip (unspecified) | 1 | |
| Knee Surgery | 1 | |
| Patellar Tendinopathy | 1 | |
| Quadriceps Strain | 1 | |
| Other (excluded from analysis) | Arm Contusion | 1 |
| Blister | 2 | |
| Elbow Contusion | 2 | |
| Finger (unspecified) | 1 | |
| Finger Fracture | 1 | |
| Illness | 5 | |
| Leg Contusion | 1 | |
| Metacarpal Fracture | 3 | |
| Mild TBI | 1 | |
| Rib Fracture | 1 | |
| Toe Fracture | 1 | |
| Wrist Sprain | 1 |
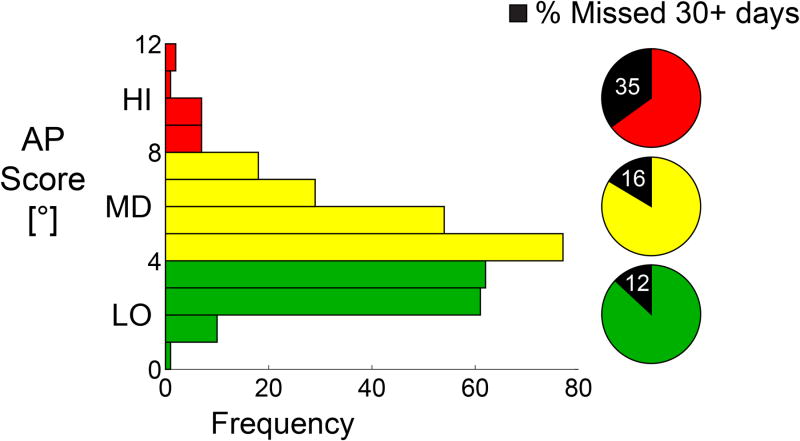
Participants were divided into tertiles based on APScore (LO:<4.0, MD:4.0-7.9, HI:≥8.0; range 1.0-12.5) and into 2 categories based on total number of days missed (<30, ≥30). From our discussions with baseball medical personnel, we concluded that it was not clinically relevant if a pitcher missed 5 days vs. 7 days vs. 15 days – it really only became important if they missed a large number of days. Therefore, we chose 30 days as a round number that the medical personnel believed would be relevant. Pearson Chi-Square tests were performed to test the hypothesis that those with a greater APScore would be more likely to miss 30+ days due to injury. Likelihood ratio Chi-Square tests were also used as a sensitivity analysis. A post-hoc analysis was performed to test the differences among groups in terms of the chance of missing ≥30 days due to injury. Odds ratios were calculated using logistic regression analysis. To further explore these results, a secondary analysis of the number of days missed by participants who missed one or more days was also performed using a one-way ANOVA and Tukey-Kramer post-hoc comparisons to determine whether those with a greater APScore missed more total days when injured. A sensitivity analysis using a non-parametric method (Kruskal-Wallis Test) was also conducted to confirm the robustness of our conclusions. An alpha level of 0.05 was used for statistical significance, and all statistical tests were performed in JMP 10.0 (SAS Institute Inc., Cary, NC).
Results
Distribution of the APScore along with the division into tertiles and the percent of participants in each tertile who missed 30 or more days are shown in Figure 4. Fifty-three of the 347 (15.3%) participants missed 30 or more days due to the included injuries as listed in Table 2. Lumbopelvic control group was a significant factor in the likelihood to miss 30 or more days (p=0.023, two sided Pearson Chi-Square test). As shown in Table 3, the chance of missing 30 or more days among the participants with poor lumbopelvic control (HI group) was 3.0 times as high as in those with good lumbopelvic control (LO group) (OR= 4.11, 95% CI: 1.43-11.8), and 2.2 times as high as in those with moderate lumbopelvic control (MD group) (OR=2.85, 95% CI: 1.05-7.74). Post-hoc analysis did not show a significant difference in the likelihood of missing 30 or more days between the moderate and good groups (OR=1.44, 95% CI: 0.75-2.76).
Figure 4.
Histogram of APScore showing uneven distribution of pitchers into the three tertiles of LO, MD, and HI amounts of pelvic movement during the single leg raise test. Pie charts show the percentage of pitchers in each tertile who missed 30 or more days due to injury during the season.
Table 3.
Those with poor lumbopelvic control (HI group) were significantly more likely to miss 30 or more days due to injury than those with moderate or good lumbopelvic control (MD and LO groups) (Chi-Square p=0.023).
| Single Leg Raise APScore | Missed < 30 days due to injury | Missed 30+ days due to injury | Total |
|---|---|---|---|
| LO: Less than 4.0 | 122 (88.4%) | 16 (11.6%) | 138 |
| MD: 4.0 - 7.9 | 159 (84.1%) | 30 (15.9%) | 189 |
| HI: 8.0 or greater | 13 (65.0%)* | 7 (35.0%)* | 20 |
| All | 294 (84.7%) | 53 (15.3%) | 347 |
indicates a significant difference from all other groups (p<0.05).
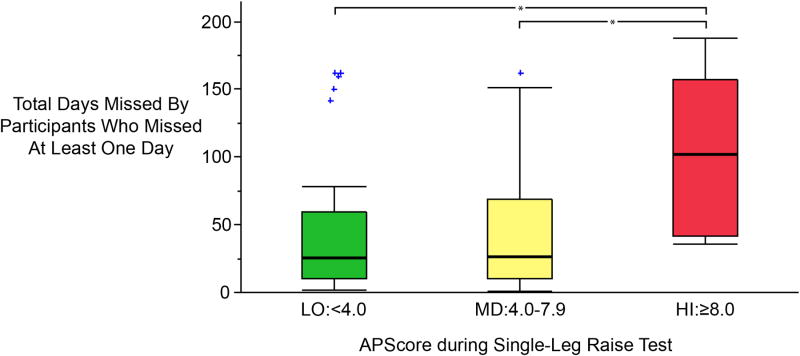
Out of the 108 (31.1%) of the 347 participants who missed at least one day due to injury, the average number of days missed was significantly different among the three groups (ANOVA, p=0.018). Those with poor lumbopelvic control (HI group) missed more days due to injury (mean 98.6 days) than those with moderate (MD group, mean 45.8 days, p=0.017) or good (LO group, mean 43.8 days, p=0.017) lumbopelvic control (Figure 5).
Figure 5.
Box-and-whisker plots of total number of days missed for all participants who missed at least one day due to injury (108 out of 347 participants). Boxes indicate the interquartile range, whiskers indicate 1.5* the interquartile range, and outliers are marked by (+).Those with poor lumbopelvic control (HI APScore in the single leg raise test) missed more days due to injury (mean 98.6 days) than those with moderate (MD group, mean 45.8 days, p=0.017) or good (LO group, mean 43.8 days, p=0.017) lumbopelvic control. * indicates a significant difference between groups (p<0.05).
Discussion
To the authors' knowledge, this study is the first to demonstrate that lumbopelvic control is related to injuries in professional baseball pitchers. Within the levels of competition represented by the tested population, a regular season can last between approximately 90 days (Short-A or Rookie League) and 180 days (Major League including playoffs), so missing 30 days or more represents 17-33% of the entire season. It should be noted that a day was counted as missed if any limitation was placed on the pitcher's activity, whether or not the scheduled activity was in a practice or a game situation. In the counting method used for this study, if a pitcher would normally be scheduled to have a day off, any soreness experienced during that day would not be counted as a day missed if the pitcher was able to fully participate at the next scheduled time he was required to throw. However, if a pitcher was held to a reduced number of pitches due to health concerns, the total number of days between the first day of limited duty and the last day of limited duty would be counted as days missed.
Previous studies have shown a relationship between peak ground reaction forces and pitching velocity20, suggesting that a successful pitch depends on energy generation from the legs and transfer of that energy through the lumbopelvic region to the throwing hand. Moreover, as mentioned above several recent cross-sectional biomechanical studies have demonstrated relationships between lumbopelvic control, kinematics and muscle activations to both increased pitch velocity and higher shoulder/elbow loads1, 2, 21, 25-28, 30. A lack of lumbopelvic control may lead to an inability of the pitcher to efficiently transfer energy from the legs to the hand, leading to excessive use of the shoulder, arm and wrist muscles to generate ball velocity. It could also lead to early “opening up” of the torso towards the target30, forcing the torso, shoulder and elbow to the extremes of the range of motion in a whip-like motion, which may cause excessive joint moments that strain the ligaments and other soft tissues leading to overuse injuries. Future research is necessary to determine whether those with poor lumbopelvic control do use their upper extremity muscles more or experience higher moments at the extremes of the range of motion when generating the same pitch velocity.
These results suggest that focused attention on improving lumbopelvic control could potentially lower the rate of injuries in baseball pitchers. The number of days missed by those in the poor lumbopelvic control group was significantly greater than the moderate or good groups (Figure 5), which is consistent with either an increased number of injuries or increased severity of injuries in the poor control group. Improving lumbopelvic strength, endurance and control have been reported to lower the occurrence of lower extremity injuries or improve lower extremity biomechanics in numerous sporting situations3, 5, 12, 13, 15, 23, and these results suggest that a similar result may happen in baseball pitching. Therefore, work is currently underway to test whether an exercise program focused on lumbopelvic control will lead to a reduction in the number of injuries sustained or days missed during the season due to injuries.
The results of this study should be considered in light of its limitations. A larger sample size would permit a more robust estimate of the difference in injury rates between groups as well as a multi-factorial examination of the relative importance of lumbopelvic control versus other potential injury risk factors. In spite of the large total population of the study, the number of participants who missed 30 or more days was small, especially in the poor pelvic control group (HI, Table 3). These small numbers precluded an analysis of injuries by region (e.g. shoulder vs. elbow). In addition, the participants who were released, traded, or retired may have been released due to poor performance or prior injury history that may or may not have been related to lumbopelvic control deficits to some degree.
The choices of aggregating days missed over the season and of including days when participation was limited as days missed have both limitations and advantages that affect interpretation of the results. Aggregating total days missed have confounded the examination of a relationship between lumbopelvic control at spring training and days missed, because either the first injury itself or any rehabilitation efforts in response to that injury could potentially alter the participant's lumbopelvic control and make the preseason lumbopelvic control measurement irrelevant to subsequent injuries. In an ideal world, one would like to assess lumbopelvic control on a regular basis so that the lumbopelvic control immediately prior to any injury could be known. However, in addition to being impossible within the time constraints of a professional baseball organization where games are played almost every day, such an approach would ignore the possibility that during the season, an injury deemed relatively minor may never be completely addressed. If a pitcher is asked to reduce his workload until the pain or tightness goes away and he is desirous of maintaining his position as a useful member of the team, he may under-report the severity and over-report the recovery24. In this case, it is possible that an initial assessment of poor lumbopelvic control may persist and lead to an increased likelihood of injury throughout an entire season. Given this possibility, we chose to aggregate all of these injuries to investigate whether a pervasive association exists, even though any changes in lumbopelvic control during the season would create statistical uncertainty, making it more difficult to observe a true association between lumbopelvic control and injury.
On the other hand, aggregating all missed days together precludes the possibility of directly examining if lumbopelvic control is associated with injury severity. If only the initial injury was examined, then the duration of this injury could also be subjected to a group comparison by lumbopelvic control. However, it has previously been hypothesized that the same root biomechanical or neuromuscular control deficit could result in varying symptoms. For example, Aguinaldo observed that earlier “opening up” of the trunk towards home plate was associated both with higher shoulder and elbow loads1, 2. Given the theoretical basis and biomechanical evidence suggesting that lumbopelvic control may play a role in lower extremity, torso, shoulder and elbow injuries, we deemed it most appropriate for this first study on this topic to test the association of preseason lumbopelvic control to the aggregate of days missed due to all injuries.
Another potential limitation is that the single leg raise test is relatively non-specific and easy to perform for an athlete. It does not assess isolated strength, muscle length, or the individual control contributions of the muscles that influence lumbopelvic control. Moreover, one cannot discount the possibility that performance on this test may be influenced by contributors outside the lumbopelvic region, such as muscles controlling the knee, ankle or foot. While this test does replicate the initiation of a pitching motion, when the pitcher would lift his stride leg, the test does not replicate either the quickness or force with which a pitcher would raise his stride leg to complete a pitch. Therefore, it is possible that a more strenuous, sport-specific test may better identify participants who have a lumbopelvic control deficit that only manifests during the pitching motion. However, previous results using this single leg raise test have demonstrated associations to both pitching performance6 and risk of days missed due to injury (this study) in professional pitchers, validating the use of this test in spite of its lack of task specificity and low level of difficulty.
Conclusion
Poor lumbopelvic control during a standing single leg raise test during spring training was significantly associated with missing 30 or more days due to injury through the course of an entire season in professional baseball pitchers. These results suggest that an increased emphasis on appropriate lumbopelvic control training may reduce the burden of injury in baseball pitchers.
Acknowledgments
S. McConoughey and M. Manring are gratefully acknowledged for their editorial assistance, and J. Yedimenko is gratefully acknowledged for her contributions to the validation study.
Funding disclosure: Partial funding received from National Institutes of Health, OSU Sports Medicine Initiative Grants Program, and TechColumbusTechGenesis Program
Footnotes
Conflict of interest statement: A. Chaudhari and C. McKenzie are co-owners of Perfect Practice, Inc., the producer of the Level Belt Pro app used to make measurements of pelvic motion in this study. The other authors report no potential conflict of interest.
References
- 1.Aguinaldo AL, Buttermore J, Chambers H. Effects of upper trunk rotation on shoulder joint torque among baseball pitchers of various levels. J Appl Biomech. 2007;23(1):42–51. doi: 10.1123/jab.23.1.42. [DOI] [PubMed] [Google Scholar]
- 2.Aguinaldo AL, Chambers H. Correlation of throwing mechanics with elbow valgus load in adult baseball pitchers. Am J Sports Med. 2009;37(10):2043–2048. doi: 10.1177/0363546509336721. [DOI] [PubMed] [Google Scholar]
- 3.Akuthota V, Ferreiro A, Moore T, Fredericson M. Core stability exercise principles. Curr Sports Med Rep. 2008;7(1):39–44. doi: 10.1097/01.CSMR.0000308663.13278.69. [DOI] [PubMed] [Google Scholar]
- 4.Campbell BM, Stodden DF, Nixon MK. Lower extremity muscle activation during baseball pitching. J Strength Cond Res. 2010;24(4):964–971. doi: 10.1519/JSC.0b013e3181cb241b. [DOI] [PubMed] [Google Scholar]
- 5.Chappell JD, Limpisvasti O. Effect of a neuromuscular training program on the kinetics and kinematics of jumping tasks. Am J Sports Med. 2008;36(6):1081–1086. doi: 10.1177/0363546508314425. [DOI] [PubMed] [Google Scholar]
- 6.Chaudhari AM, McKenzie CS, Borchers JR, Best TM. Lumbopelvic control and pitching performance of professional baseball pitchers. J Strength Cond Res. 2011;25(8):2127–2132. doi: 10.1519/JSC.0b013e31820f5075. [DOI] [PubMed] [Google Scholar]
- 7.Chaudhari AMW, Yedimenko J, Jamison ST, McNally M, McKenzie C, Onate J. Validation of a Novel Clinical Tool to Measure Pelvic Tilt. Paper presented at: Gait & Clinical Movement Analysis Society Annual Meeting; May 14-17, 2013; Cincinnati, OH. [Accessed March 3, 2014]. Available at: http://www.hbr1.net/2013%20GCMAS%20Proceedings.pdf. [Google Scholar]
- 8.Conte S, Requa RK, Garrick JG. Disability Days in Major League Baseball. Am J Sports Med. 2001;29(4):431–436. doi: 10.1177/03635465010290040801. [DOI] [PubMed] [Google Scholar]
- 9.Conte SA, Thompson MM, Marks MA, Dines JS. Abdominal muscle strains in professional baseball: 1991-2010. Am J Sports Med. 2012;40(3):650–656. doi: 10.1177/0363546511433030. [DOI] [PubMed] [Google Scholar]
- 10.Davis JT, Limpisvasti O, Fluhme D, et al. The Effect of Pitching Biomechanics on the Upper Extremity in Youth and Adolescent Baseball Pitchers. Am J Sports Med. 2009;37(8):1484–1491. doi: 10.1177/0363546509340226. [DOI] [PubMed] [Google Scholar]
- 11.Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of Baseball Pitching with Implications About Injury Mechanisms. Am J Sports Med. 1995;23(2):233–239. doi: 10.1177/036354659502300218. [DOI] [PubMed] [Google Scholar]
- 12.Fredericson M, Cookingham CL, Chaudhari AM, Dowdell BC, Oestreicher N, Sahrmann SA. Hip abductor weakness in distance runners with iliotibial band syndrome. Clin J Sport Med. 2000;10(3):169–175. doi: 10.1097/00042752-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Fredericson M, Moore T. Muscular balance, core stability, and injury prevention for middle- and long-distance runners. Phys Med Rehabil Clin N Am. 2005;16(3):669–689. doi: 10.1016/j.pmr.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 14.Fuller CW, Ekstrand J, Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Scand J Med Sci Sports. 2006;16(2):83–92. doi: 10.1111/j.1600-0838.2006.00528.x. [DOI] [PubMed] [Google Scholar]
- 15.Heiderscheit BC, Sherry M, MacAuley D, Best TM. What effect do core strength and stability have on injury prevention and recovery? In: MacAuley D, Best TM, editors. Evidence-based sports medicine. Vol. 2. Ames, IA: Blackwell BMJ Books; pp. 2007pp. 59–72. [Google Scholar]
- 16.Kibler WB, Press J, Sciascia A. The role of core stability in athletic function. Sports Med. 2006;36(3):189–198. doi: 10.2165/00007256-200636030-00001. [DOI] [PubMed] [Google Scholar]
- 17.Lintner D, Noonan TJ, Ben Kibler W. Injury Patterns and Biomechanics of the Athlete's Shoulder. Clin Sports Med. 2008;27(4):527. doi: 10.1016/j.csm.2008.07.007. + [DOI] [PubMed] [Google Scholar]
- 18.Lyman S, Fleisig GS, Andrews JR, Osinski ED. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002;30(4):463–468. doi: 10.1177/03635465020300040201. [DOI] [PubMed] [Google Scholar]
- 19.Lyman S, Fleisig GS, Waterbor JW, et al. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001;33(11):1803–1810. doi: 10.1097/00005768-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 20.MacWilliams BA, Choi T, Perezous MK, Chao EYS, McFarland EG. Characteristic Ground-Reaction Forces in Baseball Pitching. Am J Sports Med. 1998;26(1):66–71. doi: 10.1177/03635465980260014101. [DOI] [PubMed] [Google Scholar]
- 21.Matsuo T, Escamilla RF, Fleisig GS, Barrentine SW, Andrews JR. Comparison of Kinematic and Temporal Parameters Between Different Pitch Velocity Groups. J Appl Biomech. 2001;17:1–13. [Google Scholar]
- 22.Matsuo T, Fleisig GS. Influence of shoulder abduction and lateral trunk tilt on peak elbow varus torque for college baseball pitchers during simulated pitching. J Appl Biomech. 2006;22(2):93–102. doi: 10.1123/jab.22.2.93. [DOI] [PubMed] [Google Scholar]
- 23.Myer GD, Brent JL, Ford KR, Hewett TE. A pilot study to determine the effect of trunk and hip focused neuromuscular training on hip and knee isokinetic strength. Br J Sports Med. 2008;42(7):614–619. doi: 10.1136/bjsm.2007.046086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ojeda RM. My left arm. New York Times. 2012 May 27; 2012;Sports. [Google Scholar]
- 25.Oliver GD. Relationship between gluteal muscle activation and upper extremity kinematics and kinetics in softball position players. Med Biol Eng Comput. 2013:1–6. doi: 10.1007/s11517-013-1056-3. [DOI] [PubMed] [Google Scholar]
- 26.Oliver GD, Keeley DW. Gluteal muscle group activation and its relationship with pelvis and torso kinematics in high-school baseball pitchers. J Strength Cond Res. 2010;24(11):3015–3022. doi: 10.1519/JSC.0b013e3181c865ce. [DOI] [PubMed] [Google Scholar]
- 27.Oliver GD, Keeley DW. Pelvis and torso kinematics and their relationship to shoulder kinematics in high-school baseball pitchers. J Strength Cond Res. 2010;24(12):3241–3246. doi: 10.1519/JSC.0b013e3181cc22de. [DOI] [PubMed] [Google Scholar]
- 28.Oyama S, Yu B, Blackburn JT, Padua DA, Li L, Myers JB. Effect of Excessive Contralateral Trunk Tilt on Pitching Biomechanics and Performance in High School Baseball Pitchers. Am J Sports Med. 2013;41(10):2430–2438. doi: 10.1177/0363546513496547. [DOI] [PubMed] [Google Scholar]
- 29.Putnam CA. Sequential motions of body segments in striking and throwing skills: descriptions and explanations. J Biomech. 1993;26(Suppl 1):125–135. doi: 10.1016/0021-9290(93)90084-r. [DOI] [PubMed] [Google Scholar]
- 30.Stodden DF, Fleisig GS, McLean SP, Lyman SL, Andrews JR. Relationship of pelvis and upper torso kinematics to pitched baseball velocity. J Appl Biomech. 2001;17(2):164–172. [Google Scholar]
- 31.Yedimenko J, Jamison ST, McNally MP, McKenzie CS, Onate JA, Chaudhari AM. Intra- and Inter-rater Reliability of a Single-Leg Raise Test of Pelvic Sagittal Control. Paper presented at: American College of Sports Medicine Annual Meeting; May 29, 2013; Indianapolis, IN. [Accessed March 3 2014]. Available at: http://journals.lww.com/acsm-msse/Fulltext/2013/05001/B_34_Free_Communication_Poster___Spine_Trunk_Core.44.aspx. [Google Scholar]