Abstract
The Contraceptive CHOICE Project was a prospective cohort study of 9,256 women in the St. Louis area. The project provided no-cost reversible contraception to participants for 2-3 years with the goal of increasing uptake of long-acting reversible contraception and decreasing unintended pregnancy in the area. This manuscript will provide a brief summation of the major findings to date including the dramatic effect the project had on unintended pregnancy and abortion rates.
Introduction
In 2006, an anonymous foundation contacted the newly formed family planning group at Washington University in St. Louis. Their request was simple: promote and provide the most effective methods of contraception to women in the St. Louis region. The foundation was willing to support the effort to do so, including the cost of these “most effective methods” and all forms of reversible contraception. As the Vice Chair of Clinical Research, Dr. Peipert saw this as an opportunity to study contraceptive use, including continuation, satisfaction, and how provision of long-acting reversible contraceptive (LARC) methods, including intrauterine devices (IUDs) and implants, might impact unintended pregnancy rates in the region. Thus, the concept for the Contraceptive CHOICE Project was conceived.
The newly formed Division of Clinical Research in the Department of Obstetrics and Gynecology was not equipped and staffed to design and implement a large-scale project such as CHOICE. New staff needed to be hired, and CHOICE needed a project director, leader, and champion. Dr. Gina Secura, an epidemiologist with an interest in sexually transmitted infections and global health, was hired to take on this task.
Under the leadership of Drs. Secura and Peipert, a strong team of clinicians, data managers, and research assistants was formed. The project was committed to adhering to a high standard of clinical research and contraceptive care with carefully designed protocols and quality data collection with the goal of changing the paradigm of how we think about contraception and the provision of care.
Purpose & Goals of the CHOICE Project
The Contraceptive CHOICE Project, or CHOICE (for short), was a prospective cohort study that enrolled 9,256 women in the St. Louis Missouri area. The project was designed to address what family planning specialists have long believed, that high and stagnant rates of unintended pregnancy could be improved with increased uptake of LARC methods. To facilitate this change, the project set out to reduce the most common barriers cited for low use of LARC; cost, patient knowledge, and access. Ultimately, the CHOICE Project sought to reduce unintended pregnancy on a population level in the St. Louis area. 1
Women were eligible to participate if they were 14-45 years old, desiring to avoid pregnancy for at least 12 months, sexually active with a male partner or planned to be, and willing to start a new contraceptive method. Each participant was provided the reversible contraceptive method of her choice at no cost for 2 or 3 years, depending on when she enrolled. Participants were allowed to change their method as frequently as desired during that time. Detailed demographic, reproductive, and medical health histories were collected at baseline. Participants were contacted by telephone at 3 and 6 months and every 6 months following until study completion. Sexually transmitted infection (STI) testing was offered at baseline, annually, and if symptomatic.
Recruitment
Our goal was to recruit a representative sample of reproductive-aged women, including women at the highest-risk for unintended pregnancy. Risk factors for unintended pregnancy include age <25, minority racial or ethnic background, and low socioeconomic status. To ensure that high-risk women could be successfully recruited and retained, we developed four recruitment strategies; first, we identified key community partners including federally qualified health centers, local family planning clinics, and clinics providing abortion services. Community partners were involved throughout the project to ensure a mutually beneficial relationship. Second, we established relationships with private health care providers in the community and provided recruitment material to help facilitate referral. Third, we created a system to continuously evaluate recruitment efforts at each site. Lastly, we provided participants with cards containing contact information for the CHOICE Project to give to their friends and family. 2
These strategies were successful in recruiting and following a representative sample of women including many at high-risk for unintended pregnancy (Table 1). The CHOICE Project enrolled 5595 women <25 years of age, representing 60% of the cohort. Racial or ethnic minorities represented 58% of the cohort, with 50% reporting being African American and 5% identifying as Hispanic. We defined low socioeconomic status(SES) as receipt of public assistance or report of difficulty paying for basic necessities. Many women (40%) in this cohort reported being of low SES. In addition, 40% of our cohort reported a history of a sexually transmitted infection (STI), 63% reported a history of a prior unintended pregnancy, and 42% reported a history of prior abortion. Follow up rates remained high throughout the project (95% at 12 months, 87% 24 months, and 81% at 36 months).
Table 1. Baseline Demographic and Reproductive Characteristics (N=9,256).
| Characteristic | N | % |
|---|---|---|
| Age(y) | ||
| 14-17 | 484 | 5.2 |
| 18-20 | 1,547 | 16.7 |
| 21-25 | 3,564 | 38.5 |
| 26-35 | 3,026 | 32.7 |
| 36-45 | 635 | 6.9 |
| Race | ||
| Black | 4,670 | 50.5 |
| White | 3,870 | 41.8 |
| Other | 715 | 7.7 |
| Hispanic ethnicity | 475 | 5.1 |
| Education | ||
| High school or less | 3,205 | 34.6 |
| Some college | 3,902 | 42.2 |
| College or more | 2,146 | 23.2 |
| Receiving public assistance * | 3,442 | 37.2 |
| Trouble paying for basic expenses + | 3,639 | 39.4 |
| Insurance | ||
| None | 3,782 | 41.1 |
| Private | 3,957 | 43.1 |
| Public | 1,455 | 15.8 |
| Parity | ||
| 0 | 4,369 | 47.2 |
| 1 | 2,279 | 24.6 |
| 2 | 1,606 | 17.4 |
| 3 or more | 1,002 | 10.8 |
| Unintended pregnancies | ||
| 0 | 3,413 | 36.9 |
| 1 | 2,492 | 26.9 |
| 2 | 1,551 | 16.8 |
| 3 or more | 1,794 | 19.4 |
| History of abortion | 3,871 | 41.8 |
| History of sexually transmitted infection ‡ | 3,746 | 40.5 |
Current receipt of food stamps, Woman Infants and Children (WIC), welfare, or unemployment
Transportation, housing, health or medical care, or food
Self-reported chlamydia, gonorrhea, syphilis, trichomoniasis, genital herpes, human papilloma virus or human immunodeficiency virus
Counseling
To address patient knowledge about contraceptive methods, specifically effectiveness, advantages, and disadvantages, a standardized counseling script was developed. 3 The frame work for this script was based on the GATHER process for counseling.4 Briefly, this method focuses on a patient-centered approach, specifically addressing the patient's expressed needs, problems, issues and concerns. With a goal of providing accurate and unbiased information on every reversible method, we used the GATHER framework to establish rapport with patients during the counseling session: Greet each potential participant. Ask participants about their lives. Tell participants about contraceptive methods and STI protection in the context of their lives. Help the participant decide what method fits her contraceptive needs. Explain everything about her chosen method including, how it works, potential side-effects, and when to call the clinic. Return visits to the clinic, or phone calls to the project are used to discuss the method and the participant's concerns.
All women who called inquiring about CHOICE were read a brief script stating that the intrauterine device and the implant (LARC methods) are the most effective methods of contraception. A sentence describing the three available LARC methods (levonorgestrel intrauterine system, the copper intrauterine device, and the etonogestrel implant) followed this statement. All participants who enrolled at our university clinical research site (n=6,931, 75%) underwent standardized contraceptive counseling regardless of their prior contraceptive knowledge. The script described the effectiveness, advantages, and disadvantages of reversible contraceptive methods in order of method effectiveness. Models of all methods were available and demonstration of the LARC insertion procedures was reviewed. Once the participant decided upon a method, the counselor would seek approval from the research clinician of the day for the desired method. Participants who enrolled at a community partner site (n=2,325, 25%) underwent the typical contraceptive counseling for that site. Methods were dispensed at that visit with every attempt to provide same day LARC insertion when pregnancy could be reasonably ruled out.
What We Have Learned
Contraceptive knowledge
Early in the implementation of the project, we performed a cross-sectional study evaluating baseline contraceptive knowledge of participants.5 Knowledge of each method's effectiveness was assessed by asking what percentage of women (<1%, 1-5%, 6-10%, >10%, don't know) the respondent thought would get pregnant in one year when using the method. Most participants (86%) correctly identified the chance of pregnancy when no contraception is used. The correct effectiveness of sterilization, IUD's, and implants were identified by 76%, 65%, and 55% respectively. Respondents typically underestimated the effectiveness of LARC methods. Less than 20% of participants correctly estimated the effectiveness of the pill, patch, and vaginal ring, with 45% overestimating the effectiveness of these methods.
Method choice and continuation
In 2007, at the launch of CHOICE, we estimated that less than 5 percent of women at sentinel clinics in St. Louis were using LARC methods. When the barriers of cost, knowledge, and access were removed, 75% of the CHOICE cohort chose a LARC method at baseline enrollment (Table 2). Forty-six percent of women chose the levonorgestrel IUD (LNG-IUD), 12% chose the copper IUD, and 17% chose the etonogestrel implant. Not only did women choose LARC methods at astonishing rates, they also had high rates of continuation and satisfaction. 6
Table 2. Baseline Chosen Method (N=9,256).
| Method | N | % |
|---|---|---|
| Levonorgestrel intrauterine device | 4,261 | 46.0 |
| Copper intrauterine device | 1,101 | 11.9 |
| Etonogestrel implant | 1,566 | 16.9 |
| Depot medroxyprogesterone acetate | 638 | 6.9 |
| Oral contraceptive pill | 874 | 9.4 |
| Contraceptive vaginal ring | 646 | 7.0 |
| Contraceptive patch | 166 | 1.8 |
| Natural family planning | 3 | <.01 |
| Diaphragm | 1 | <.01 |
LARC users were more likely than non-LARC users to continue use at 12 and 24 months (86% vs. 55% at 12 months, 77% vs. 41% at 24 months).7 At 12 months, the two IUDs had the highest continuation rates, 88% for the LNG-IUD and 84% for the copper IUD. The same pattern was confirmed at 24 months with 79% of LNG-IUD users and 77% of copper IUD users continuing. Continuation of implant was also much higher than other non-LARC methods; 83% at 12 months and 69% at 24 months. Satisfaction rates were similarly high and mirrored continuation rates. Among women who discontinued use of their LARC method within 6 months, single marital status was the only demographic characteristic associated with early discontinuation. The most common reason cited for discontinuation of an IUD was cramping, and for the implant was irregular or frequent bleeding. 8
Impact of increased LARC uptake
Some groups have raised the concern that increased uptake of highly effective contraception may lead to increased high-risk sexual behavior. The CHOICE Project has evaluated this concern in several ways; evaluating sexual behavior patterns of participants in the project, evaluating the risk of unintended pregnancy in the cohort, and assessing abortion rates. 9 We found no evidence to suggest that the provision of no-cost contraception was associated with increased sexual risk-taking behaviors. Most participants (71%) reported no change in their number of sexual partners at 6 and 12 months. Only 16% reported an increase, and of those more than 80% experienced a change from zero partners to one partner. Furthermore, the percent of women reporting multiple partners at baseline, was significantly reduced at 6 and 12 months (5.2%, 3.5%, 3.3%, respectively). 10
In addition to no change in sexual behavior patterns, we also saw a reduction in the rates of unintended pregnancy within the cohort. This can be largely attributed to the distribution of method selection, with so many women choosing the most effective, user-independent methods. One of the most impactful findings of the CHOICE Project was the quantification of how much more effective LARC methods are at preventing unintended pregnancy than are short-acting methods such as pills, patch and the vaginal ring. Failure rates for pill, patch, and ring users were 4.8%, 7.8%, and 9.4% at 1, 2, and 3 years, respectively. Failure rates for LARC users remained less than 1% throughout the three year follow-up (cumulative failure rates of 0.3% at 1 year, 0.6% by 2 years, and 0.9% at 3 years). Non-LARC users were more than 22 times as likely to experience an unintended pregnancy compared to their LARC counterparts. Furthermore, adolescent (<21 years) users of the pill, patch, or vaginal ring were twice as likely as older women using the same method to experience an unintended pregnancy (HR: 1.9). This was not true in LARC users, where we found no difference in the risk of unintended pregnancy by age. 11
To evaluate the population impact of this dramatic increase of LARC use in the area, we analyzed abortion rates, the percentage of abortions that were repeat abortions, and teen birth rates. The overall rate of abortion among participants in the project was less than half the regional and national rates. When comparing the St. Louis region to the Kansas City region, an area that is similar in size and demographic profile, we observed a significant reduction in the percent of repeat abortions. These findings highlight the important potential public health impact that increased access to LARC methods has; fewer unintended pregnancies and reduced rates of abortion.9
Special Populations
Contraception in the adolescent population
The adolescent population can provide unique challenges to the provision of contraception. Interestingly, among the first 1054 group of adolescent and young women age 21 and younger enrolled in the study, LARC methods were chosen at similar rates to older women. Among the first 5086 women enrolled, 70% chose a LARC method. Among the young adolescent group (14-17 year olds) 69% chose a LARC method. Older adolescents (18-20) chose a LARC method 61% of the time. One important difference was noted in the type of LARC method selected by young women: 14-17 year-old LARC users favored the contraceptive implant (63%), whereas the 18-20 year-old LARC users favored the IUD (71%). 11
Despite lack of evidence to support the fear, there has been concern voiced by clinician's about use of LARC methods in this population with regard to the high upfront cost of LARC and the risk of “early discontinuation.” We found that 12-month continuation among the entire cohort of adolescents using LARC was similar to older women. LARC users aged 14-19 demonstrated a continuation rate of 81% at 12 months, as compared to 84% for women aged 20-25 and 86% for women 26 and older.12 One important finding was the significantly lower rates of continuation in the youngest women using shorter acting methods. Users of shorter acting methods age 14-19 had a 12-month continuation rate of only 44%, as compared to 56% in women 20 years or older (Figure 1). Overall, we found that LARC users' satisfaction rates were high among each age stratum (75% for age 14-19 years, 82% for age 20-25 years, and 83% for age 26 and older).
Figure 1.
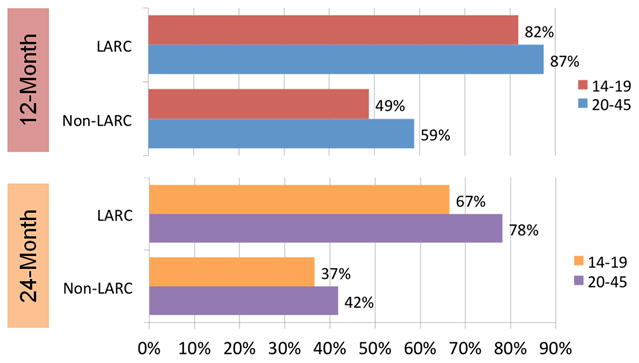
Twelve and Twenty-four Month Continuation of LARC and non-LARC methods stratified by age.
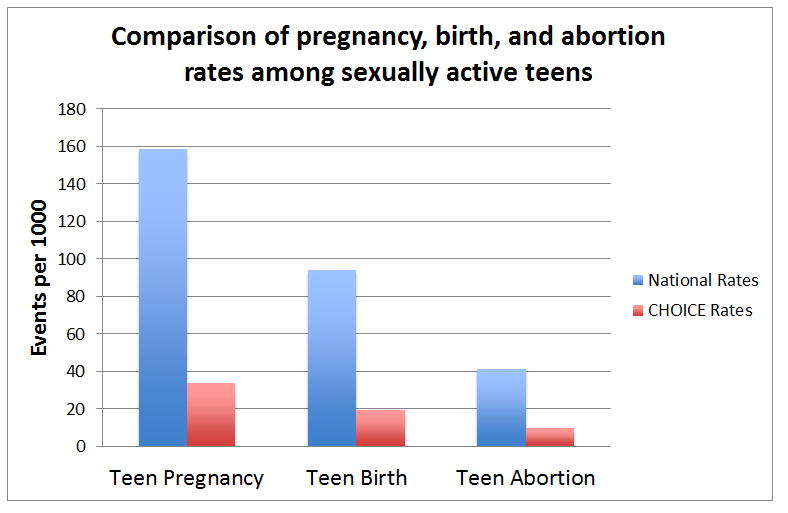
With equivalent rates of LARC use in the adolescent population, and previous evidence of decreased abortion rates in our overall cohort, we analyzed pregnancy data and outcomes specifically in women age 14-19 years (Figure 2). The average annual rate of teen pregnancy, birth, and induced abortion among CHOICE participants was significantly lower than the national rates. Rates among CHOICE teens were 34 per 1000; 19.4 per 1000; and 9.7 per 1000, respectively. National averages of pregnancy, birth and induced abortion among sexually-experienced teens evaluated during the same time were 158.5 per 1000; 94 per 1000; and 41.5 per 1000, respectively. When compared to national data, the CHOICE Project showed a greater than 75% reduction in all three outcomes.13
Figure 2. Comparison of pregnancy, birth, and abortion rates among sexually active teens.
Contraception in the overweight and obese populations
The obesity epidemic in reproductive age women in the United States continues to grow. Preventing unintended pregnancy in this population is especially important to reduce both maternal and neonatal morbidity and mortality. The impact of weight on the provision of contraception is a somewhat new research interest. Two reports from the CHOICE Project evaluated the impact of weight on the effectiveness of the combined hormonal contraceptives 14 and the etonogestrel subdermal implant. 15 We also evaluated perceived 16 and objectively measured17 weight change in women using progestin-only methods.
Among 1,523 women choosing a combined hormonal contraceptive method, the pill, patch, or vaginal ring, there were 334 unintended pregnancies. Of those pregnancies, 128 were determined to be contraceptive failures. Body mass index (BMI) was not found to be a significant factor associated with increased risk of method failure.
A similar analysis was completed in women using the subdermal etonogestrel implant. Of 1,168 implant users, 28% were overweight, and 35% were classified as obese. The 3-year cumulative failure rate was less than 1 per 100 women-years and did not vary by BMI.
Concerns about weight gain, especially with progestin-only methods, can influence contraceptive choice and use. Validity of perceived weight gain among participants was evaluated by comparing self-reported weight-gain to objective weight measurement. Women who perceived weight gain were more likely to be implant or depot medroxyprogesterone acetate (DMPA) users. Objective weight gain was, on average, 10.3 pounds in women who reported perceived weight gain. The sensitivity and specificity of perceived weight gain was 74.6% and 84.4% respectively. A separate analysis compared objectively measured body weight at baseline and 12 months in participants that were continuous users of a progestin-only method to users of the Cu-IUD. Weight change among participants was variable by method used. The mean change for ENG-implant users was 2.1k g, 1.0k g for LNG-IUD users, and 2.2 kg for DMPA. Although unadjusted linear regression models suggested that the ENG-implant and DMPA were associated with increased weight gain when compared to the copper IUD, adjusted models only identified black race as having a significant association with weight gain at 12 months.
Contraception in women seeking abortion
Because so many women report having used a contraceptive method at the time of an unintended pregnancy, women seeking abortion may be particularly motivated to initiate a LARC method at the time of procedure. As a result of relationships developed with community sites, the CHOICE Project was able to recruit potential participants at community centers providing abortion services. Of 3,410 women enrolled with a recent history of abortion, 937 received immediate (on the day of procedure) contraception. Those receiving immediate provision of their method were more than 3 times as likely to choose an IUD (RR= 3.3, 95% CI: 2.67, 4.85) and more than 50% more likely to choose an implant (RR=1.5) when compared to women without a recent history of abortion. This suggests that if women have access to LARC at the time of abortion, many of them will initiate one of these highly-effective methods.18
A separate analysis evaluated the continuation rates of participants choosing and receiving the ENG-implant at the time of abortion. Continuation rates in this population were compared to those receiving interval placement of the implant. The 12-month continuation rates were similar: 81.5% among those receiving immediate placement, and 82.8% in those undergoing interval placement. Women undergoing immediate placement were no more likely to discontinue the method than were those undergoing delayed insertion. Irregular or frequent bleeding was the most common reason cited by both groups for discontinuation. 19
Sexually transmitted infection
Sexually transmitted infection (STI) testing was offered to all CHOICE participants at baseline, annually, and if ever symptomatic. Nearly all participants agreed to be screened at enrollment. Of the 8,347 women for whom results were available, 656 (7.9%) were positive for one or more infection (Neisseria gonorrhoeae (GC), Chlamydia trachomatis (CT), and Trichomonas vaginalis (TV)). Prevalence of GC was 0.4%, CT 3.1%, and TV 4.9%. Black women were four times more likely to test positive for all three infections, and accounted for 81% of TV infections.20 The prevalence of each infection in the CHOICE Project was higher than national estimates.21 When applying current screening guidelines to our cohort, (i.e., screen all sexually active women age less than 26 years old or with high-risk sexual behavior) we found that 16% of the STIs identified with a more universal screening approach would have been missed. Interestingly, we found age to be an important epidemiologic difference between women diagnosed with CT and TV: young age (14-21 years of age) being associated with CT and older age (36-45 years of age) associated with TV.
The high prevalence of STIs across the United States has been at least partly attributed to poor adherence to screening guidelines. With the increase in LARC uptake, there is further concern that women may not seek care as frequently and as a result go unscreened for STIs. A randomized controlled trial comparing home-based screening for GC and CT to traditional clinic-based screening in a cohort of LARC users was performed to assess if screening rates could be improved.22 Women randomized to home-based screening were mailed swabs for self-collection. Screening rates were significantly higher in the home-based screening group (56.3%) when compared to clinic-based screening group (25.0%; RR=2.2). This study provides evidence to suggest that options for STI screening may be more effective and preferred by women. LARC users may not seek care as frequently as they had when using non-LARC methods; thus, they may be ideal for self-collected STI screening.
Conclusions
The Contraceptive CHOICE Project is one of the largest prospective cohort studies of women in the U.S. seeking reversible contraception. Findings from the project indicate that when the barriers of cost, access, and knowledge are removed, women choose the most effective and least user-dependent methods. Not only do they choose these methods, they continue using them and they are highly satisfied with their contraceptive choice. Perhaps the most encouraging finding of CHOICE is the potential to impact the epidemic of unintended pregnancy in the U.S. Increasing the uptake of LARC can decrease unintended pregnancy and abortion rates, which may ultimately translate into better financial, economic, educational, and social situations for women and their families.
Acknowledgments
Disclosures: This research was supported in part by: 1) An Anonymous Foundation, and 2) Washington University Institute of Clinical and Translational Science grants UL1TR000448 and TL1 TR000449 from the National Center for Advancing Translational Sciences; and, 3) the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Numbers T32HD055172 and K23HD070979.
Footnotes
Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NICHD or NIH.
References
- 1.Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010 Aug;203(2):115, e111–117. doi: 10.1016/j.ajog.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spain JE, Peipert JF, Madden T, Allsworth JE, Secura GM. The Contraceptive CHOICE Project: recruiting women at highest risk for unintended pregnancy and sexually transmitted infection. Journal of women's health. 2010 Dec;19(12):2233–2238. doi: 10.1089/jwh.2010.2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Madden T, Mullersman JL, Omvig KJ, Secura GM, Peipert JF. Structured contraceptive counseling provided by the Contraceptive CHOICE Project. Contraception. 2013 Aug;88(2):243–249. doi: 10.1016/j.contraception.2012.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rinehart W, Rudy S, Drennan M. GATHER guide to counseling. Population reports Series J, Family planning programs. 1998 Dec;(48):1–31. [PubMed] [Google Scholar]
- 5.Eisenberg DL, Secura GM, Madden TE, Allsworth JE, Zhao Q, Peipert JF. Knowledge of contraceptive effectiveness. Am J Obstet Gynecol. 2012 Jun;206(6):479, e471–479. doi: 10.1016/j.ajog.2012.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peipert JF, Zhao Q, Allsworth JE, et al. Continuation and satisfaction of reversible contraception. Obstet Gynecol. 2011 May;117(5):1105–1113. doi: 10.1097/AOG.0b013e31821188ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O'Neil-Callahan M, Peipert JF, Zhao Q, Madden T, Secura G. Twenty-four-month continuation of reversible contraception. Obstet Gynecol. 2013 Nov;122(5):1083–1091. doi: 10.1097/AOG.0b013e3182a91f45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grunloh DS, Casner T, Secura GM, Peipert JF, Madden T. Characteristics associated with discontinuation of long-acting reversible contraception within the first 6 months of use. Obstet Gynecol. 2013 Dec;122(6):1214–1221. doi: 10.1097/01.AOG.0000435452.86108.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peipert JF, Madden T, Allsworth JE, Secura GM. Preventing Unintended Pregnancies by Providing No-Cost Contraception. Obstet Gynecol. 2012 Oct 3; doi: 10.1097/aog.0b013e318273eb56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Secura GM, Adams T, Buckel CM, Zhao Q, Peipert JF. Change in sexual behavior with provision of no-cost contraception. Obstet Gynecol. 2014 Apr;123(4):771–776. doi: 10.1097/AOG.0000000000000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mestad R, Secura G, Allsworth JE, Madden T, Zhao Q, Peipert JF. Acceptance of long-acting reversible contraceptive methods by adolescent participants in the Contraceptive CHOICE Project. Contraception. 2011 Nov;84(5):493–498. doi: 10.1016/j.contraception.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenstock JR, Peipert JF, Madden T, Zhao Q, Secura GM. Continuation of reversible contraception in teenagers and young women. Obstet Gynecol. 2012 Dec;120(6):1298–1305. doi: 10.1097/aog.0b013e31827499bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Secura G, Madden T, McNicholas C, Mullersman J, Buckel C, Zhao Q, Peipert J. Provision of No-Cost Long-Acting Contraception and Teen Pregnancy. NEJM. 2014 doi: 10.1056/NEJMoa1400506. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McNicholas C, Zhao Q, Secura G, Allsworth JE, Madden T, Peipert JF. Contraceptive failures in overweight and obese combined hormonal contraceptive users. Obstet Gynecol. 2013 Mar;121(3):585–592. doi: 10.1097/AOG.0b013e31828317cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu H, Wade JA, Peipert JF, Zhao Q, Madden T, Secura GM. Contraceptive failure rates of etonogestrel subdermal implants in overweight and obese women. Obstet Gynecol. 2012 Jul;120(1):21–26. doi: 10.1097/AOG.0b013e318259565a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nault AM, Peipert JF, Zhao Q, Madden T, Secura GM. Validity of perceived weight gain in women using long-acting reversible contraception and depot medroxyprogesterone acetate. Am J Obstet Gynecol. 2013 Jan;208(1):48, e41–48. doi: 10.1016/j.ajog.2012.10.876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vickery Z, Madden T, Zhao Q, Secura GM, Allsworth JE, Peipert JF. Weight change at 12 months in users of three progestin-only contraceptive methods. Contraception. 2013 Oct;88(4):503–508. doi: 10.1016/j.contraception.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Madden T, Secura GM, Allsworth JE, Peipert JF. Comparison of contraceptive method chosen by women with and without a recent history of induced abortion. Contraception. 2011 Dec;84(6):571–577. doi: 10.1016/j.contraception.2011.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Madden T, Eisenberg DL, Zhao Q, Buckel C, Secura GM, Peipert JF. Continuation of the etonogestrel implant in women undergoing immediate postabortion placement. Obstet Gynecol. 2012 Nov;120(5):1053–1059. doi: 10.1097/aog.0b013e3182632cd6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McNicholas C, Peipert JF, Maddipati R, Madden T, Allsworth JE, Secura GM. Sexually transmitted infection prevalence in a population seeking no-cost contraception. Sexually transmitted diseases. 2013 Jul;40(7):546–551. doi: 10.1097/OLQ.0b013e31829529eb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance. 2010. Available at: http://www.cdc.gov/std/stats10/default.htm.
- 22.Graseck AS, Secura GM, Allsworth JE, Madden T, Peipert JF. Home compared with clinic-based screening for sexually transmitted infections: a randomized controlled trial. Obstet Gynecol. 2010 Dec;116(6):1311–1318. doi: 10.1097/AOG.0b013e3181fae60d. [DOI] [PMC free article] [PubMed] [Google Scholar]


