Introduction
Evidence-based public health focuses on the translation of research into practice in order to improve health outcomes (Brownson, 2009; Brownson, 2010). In 2010, The National Institutes of Health (NIH) published a “roadmap”, which urged the evaluation of research in real-world settings as a primary goal of translational science (NIH, 2010). However, successful implementation and evaluation of evidence-based interventions (programs, policies, strategies) in community settings, other than those in which they were originally shown to be efficacious, has proven challenging (Burgio, 2010; Kerner, Rimer, & Emmons, 2005). Some authors have urged the generation of evidence from practice settings (rather than, or in addition to, strictly controlled research settings) to make evidence-based interventions better matched to community needs (Green, 2008).
When community health planners select an evidence-based intervention that has been developed and tested in one situation and adapt it for use in a different situation or community, best practice suggests needs assessment and formative research in the new setting (Bartholomew et al., 2011; Lau, 2006 ). Cancer prevention planners who are interested in adopting and perhaps adapting an evidence-based approach need to base their choices on a sound understanding of the health or behavioral risk problem in which they mean to intervene (Brownson et al., 2010). This understanding, optimally derived from both the peer reviewed literature and directly from the local community context, includes not only the behavior of risk of the priority group but also the personal and environmental determinants of that behavior (Bartholomew et al., 2011). Other important information is the organizational context and culture of potential implementation sites (Brownson et al., 2010; Green et al., 2006; Kohatsu et al., 2004). Acquiring information on which to base the selection of an evidence-based approach to cancer prevention and control in a new community requires a balancing act of assessing local community needs, weighing community information against a broader perspective from the scientific literature and using the combination to identify and adapt an evidence-based intervention program that is likely to be effective in the new setting (Brownson et al, 2010).
This report is a case study of a community and organizational assessment conducted as a foundation for selecting and recommending adaptation of an evidence-based intervention in the community. The goal of the planning group was to select an intervention to increase mammography among underserved African American women by reducing missed appointments. Research has shown that African American women are less likely to use mammography screening (Schueler et al., 2008; Crump et al., 2000; Legler et al., 2002), more likely to miss scheduled mammography appointments (Smith-Bindman et al., 2006) and therefore more likely to be diagnosed at a later stage of breast cancer (Smith-Bindman et al., 2006) than their Caucasian counterparts. We used a systematic, community informed approach to assess community needs, ideas for solutions, and organizational capacity for intervention selection aimed to reduce mammography non-adherence among African American women.
Methods
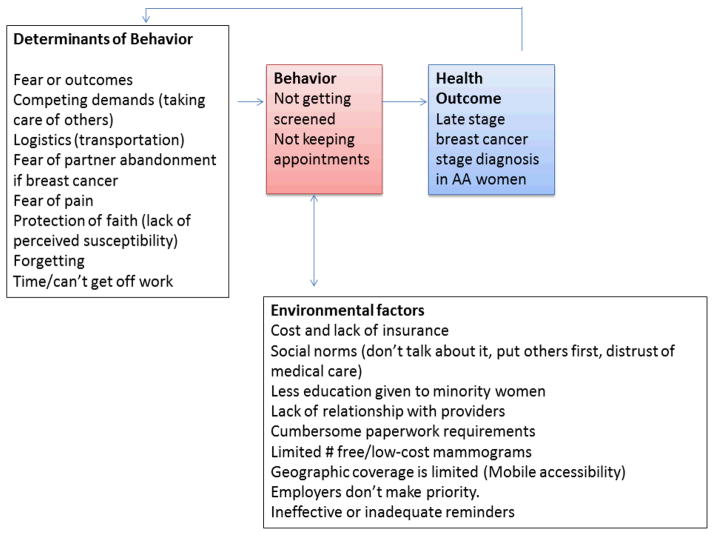
We used an inductive sequential exploratory mixed methods design to inform our search for and selection of an evidence-based intervention program as shown in Figure 1. Each step in the design informed the approach and questions used in the next step.
Figure 1.
Project Phases Flow Chart with Steps and Products Developed.
Project Context: Partners, Priority Population and Neighborhoods of Focus
This project was a partnership between a local health foundation, a collaborative of breast health organizations, a mammography clinical service provider and researchers. The local health foundation was a non-profit organization focused on public health that provided grant funding to area service organizations. The project was initiated by the collaborative of breast health organizations. The priority population was chosen because of the concern of the partners, in particular about the no-show rates for scheduled mammograms among underserved women. This priority population was low income, uninsured African American women aged 35–64. Low income was considered at or below 200% of the Federal Poverty Level (FPL), which was $22,050 for a family of four in 2009.
Four Houston area super neighborhoods were selected as communities of focus: Acres Homes, Greater Inwood, Fondren Gardens and Northshore. A super neighborhood refers to a geographic area where residents, civic organizations, institutions and businesses work together to set priorities to address the needs and concerns of their community. These communities of focus were determined by secondary data analysis based on the highest concentration of African American women between the ages 35–64 and highest breast cancer mortality. Since Harris County, including the City of Houston, is considerably large (both in geography and population density) the region was split into four quadrants and an additive index was used to find the super neighborhood in each quadrant with the highest population concentration of African American women between ages 35–64 and highest breast cancer mortality rates using ArcGIS (for example a tract with 2,000 African American women between 35–64 years of age and a breast cancer mortality rate of 20 per 100,000 would receive an index score of 2020) (ESRI, Redlands, CA). Population data were taken from the 2000 U.S. Census at tract level. Data on breast cancer mortality by Census tract was obtained from the Texas Department of State Health Services via the Breast Health Portal (Highfield et al., 2011). Breast cancer mortality data was used as a proxy for potential mammography screening barriers and screening non-adherence (Smith-Bindman et al., 2006).
Phase 1: Community Assessment
For the community assessment, we conducted a literature review, key informant interviews and focus groups. We reviewed the literature regarding barriers and facilitators of mammography in underserved African American women. In PubMed and Google Scholar, we used the search terms of “barriers,” “mammography screening,” “no-shows,” “underserved,” “African American,” “low income,” “appointment adherence.” We then selected additional articles identified from the reference lists of the articles found in the searches.
Within the four neighborhoods at increased need, the research team interviewed 12 key informants who were existing grantees of the health foundation and were knowledgeable about breast health issues in the community from their role as service providers. We used an interview guide with questions and suggested probes based on the literature review to confirm and further explore the need for increasing mammography screening adherence in the community, local barriers to mammography and appointment keeping, and strategies for increasing adherence. The interview guide and data collection tools used for the key informant interviews and focus groups (described below) are available as a supplement to this article. Both the interviewer and the note taker who recorded notes during the interview prepared the notes for analysis by typing their notes. Data were analyzed using content analysis (Bernard & Ryan, 2010).
We then used themes from the key informants and the literature review to inform the focus group guide and elicitation exercises to garner the perspectives of the priority populations. Women from the priority population who had worked with the Foundation on community-based projects used network and snowball sampling to recruit 34 women for one focus group in each of the four neighborhoods. Research staff of the Foundation had previously trained these community women in focus group methods and they served as facilitators or co-facilitators for the focus groups. Facilitators elicited responses through a problem and solution tree exercise that covered the reasons someone [“you or someone you know”] would make an appointment and not keep it; prioritization of the reason(s) stated by women in the groups; discussion of root causes and development of the problem; consequences of the problem; and potential solutions (Snowden et al., 2008). Four note takers sat in the back of the room and recorded conversations verbatim by hand. Four independent coders derived themes inductively using content analysis (Bernard & Ryan, 2010) and discussed the codes until they reached consensus.
Using information gathered from the key informant interviews and focus groups, we modified questions from the National Cancer Institute Health Information National Trends Survey (HINTS), the Forsyth County Cancer Screening Project Survey (FoCAS) and the Texas Behavioral Risk Factor Surveillance Survey (BRFSS) to better elicit barriers to screening in the priority population within the clinical setting. We evaluated questions for their fit with community language and perceptions of breast cancer screening and then cognitive interviewing with 12 participants to refine the survey questions prior to implementation (Beatty, 2007; Knafl, 2007). An outside expert in social psychology and survey design reviewed the survey instrument to assist with question modification based on the cognitive interviews. The final survey had 21 questions on mammography, breast cancer, and barriers to screening (available as a supplement to this article).
Using the survey instrument, the research team conducted a telephone-based survey at the clinical site with patients who clinic staff identified from patient records as having had missed mammography appointments within the last six months. The interviewer made three attempts to reach 100 patients and classified them as non-respondents if they never answered the phone or did not respond to voicemail. Sixty one patients participated in the survey for a response rate of 61%. Survey responses were analyzed using descriptive statistics.
Phase II: Organizational assessment
The purpose of the organizational assessment was to understand the organizational context of the clinical provider related to barriers and facilitators of patients’ appointment adherence and potential system resources for implementing an evidence-based intervention. The project team conducted a site visit, discussion with organizational leadership, and document review of processes at the clinical site pertaining to mobile mammography for underserved patients including: paperwork process including qualifications and restrictions required for reduced cost or free mammography; current practice for appointment reminder calls; geographic coverage; and appointment scheduling and availability. The team reviewed records from the mobile units’ services for one year.
Phase III: Searching and selection of an evidence-based intervention
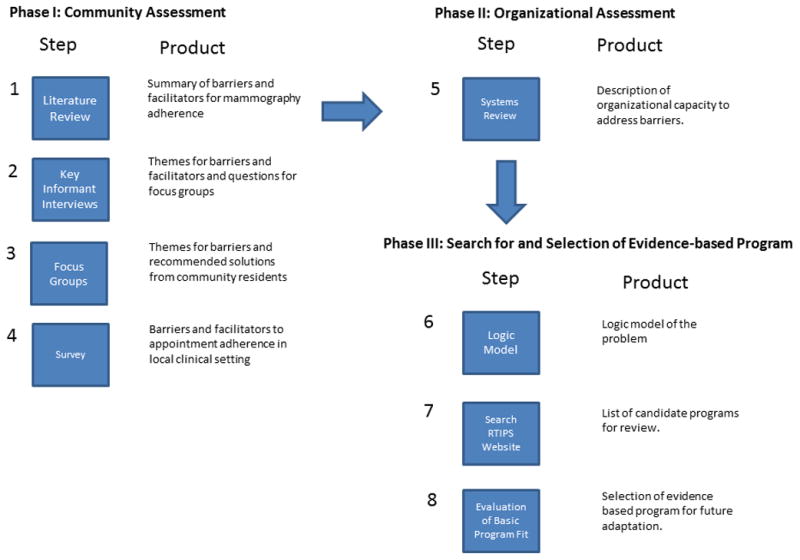
To select an intervention, the team compared the needs of the local community as depicted in a logic model to the characteristics of available research tested interventions. We used the community and organizational assessments to create a logic model of the problem using the PRECEDE model (Green and Kreuter, 2005). Such a logic model describes the behavior of risk of the priority group as well as personal and environmental determinants of that behavior (i.e., barriers, facilitators, organizational factors).
We then searched for existing evidence-based interventions in the National Cancer Institute Research-Tested Intervention Programs (RTIPs) website (Research-Tested Intervention Programs website, 2013). Based on our formative work, the search criteria were: “breast cancer screening,” “adults,” “community,” “clinical,” “urban/inner city,” “Black not of Hispanic or Latino origin,” “female,” and “materials available on RTIPs.”
The team compared found interventions to the logic model parameters of priority population, health problems, behaviors, and determinants of behaviors. We also considered availability and ease of use of materials from RTIPs, ability to implement the intervention successfully in the organizational structure of the clinical site, and the strength of effect from previous studies (Center for Substance Abuse Prevention, 2009). We assigned rankings for each criterion based on the discussion of “fit” on a scale of excellent, good, moderate and poor. The group agreed that any selected intervention must score a ranking of good or higher in each category or be modifiable in a category without making major adaptations that might disrupt essential program elements.
Results
Phase I: Community Assessment
From the literature review, we summarized barriers to mammography screening in underserved African American women including: lack of access (Schueler et al., 2008), lack of coordinated care (O’Malley et al., 2002), lack of insurance (Schueler et al., 2008; Paskett et al., 2004; Tejeda et al., 2009), lack of education (Tejeda et al., 2009), cost (Schueler et al., 2008), transportation (Bernstein et al., 2000; Ko et al., 2003), fear (pain and outcome) (Crump et al., 2000; Ko et al., 2003; Peek et al., 2008; Ogedegbe et al., 2005; Alexandraki & Mooradian, 2010), fear of partner abandonment (Peek et al., 2008), forgetfulness (Crump et al., 2000), distrust of the medical system (Peek et al., 2008), faith (Peek, 2008) and competing priorities (Peek et al., 2008; Ogedegbe et al., 2005; Moy et al., 2006). Facilitators to mammography adherence from the literature included physician recommendation (primary driver), recommendation by another health professional (nurse), patient navigation and mobile mammography programs (Crump, 2000; Wells et al., 2008; Legler et al., 2002).
Six of the barriers identified in the literature were also found in the community assessment (see Table 1). Four barriers found in the literature (lack of access, forgetfulness, lack of coordinated care and distrust of the medical system) were not specifically discussed in the community assessment. Additionally, the language used to describe the barriers varied considerably between the key informants and the focus group participants. The key informants tended to describe the issues more generally and from the provider perspective. For example, in regard to competing demands (Table 1), the key informants noted they perceived the women to think “why inconvenience myself”, whereas the women specifically discussed “taking care of everyone else before myself” and “bad news is devastating.” The local community data, particularly from the focus groups, allowed us to put local language and meanings to the logistical and theory-based barriers found in the literature.
Table 1.
Themes from Focus Groups on Barriers to Mammography Appointment Adherence Related to Barriers from the Literature and Key Informant Interviews.
| Overarching Theme | Supporting Quote | Supporting Quote |
|---|---|---|
| Barriers from the Research Literature | Similar Themes and Quotations from the Focus Groups | Similar Themes from the Key Informant Interviews |
| Fear of Outcome |
Traumatizing fear of bad news “I just automatically think…it is cancer.” “I am thinking the worst… death is close.” |
“She won’t get it done, maybe out of fear, rather not know because of worry. The worry after the diagnosis.” |
| Competing Demands |
We always put others before ourselves “African American women take care of everyone else before ourselves.” “If young black African American women get bad news, it is devastating.” |
“When you think of work, kids, you say, ‘Why inconvenience myself?” “There is a lot of extenuating circumstances in the community. She may casually say sign me up, but child care, job, time of day, and where the location is all play a part.” |
| Logistics including lack of insurance, cost and transportation |
It all goes back to finances “A lot [of women] won’t think about it unless it’s free.” “…can’t afford to go to the doctor, because [the doctor will] slap a big bill on you.” |
“Lack of transportation.” “Some say they don’t have time, running around, just don’t show up. Lack of time, so they don’t re-schedule.” |
| Fear of partner abandonment |
Feel less than a woman “What man will accept me like this?” because “you have to worry if the boyfriend/significant other will like you.” “What kind of man would like me the way I look without breasts?” “What kind of man would like me the way I look without breasts?” |
Not mentioned |
| Education |
Nobody talks about it Referring to education: “it’s just not enough.” “My doctor told me, “If it don’t bother you, don’t bother it (referring to the breast).” |
“Educate, encourage and empower women to see that it’s not a death sentence.” “Lack of knowledge “it’s not in my family.” People that I talk to on the street are under the influence that breast cancer is heredity.” |
| Fear of Pain |
Painful smashing of the breast “The squeezing is very hard. Just smashing the breast to get behind [the machine] is painful.” “The second time I went back, she used a spatula, and another technician was with her, I was devastated to go back there…” |
“Last mammogram she was too rough to me…just pounded my breast!” “I went one year, when it was painful too, and I told the doctor I wouldn’t go back to that center.” |
| Faith |
It won’t touch me “I am not going to claim it;” “I rebuke it in the name of Jesus! Don’t speak or claim it.” |
“Some can be cultural. Not going to get my body, ***touch it.” “Churches are a biggie, for African American women the church is everything.” |
Key informants responded that mammography adherence could be improved by: educating people about available funding to pay for mammograms; using reminder phone calls; building relationships and rapport with community; providing transportation for appointments; focusing on educating young women; and making the paperwork process easier. Participants also provided ideas for solutions, including: routine education for all age groups, support systems, and mobile mammography in local neighborhoods at regular and frequent intervals. Moreover, the women in the focus groups consistently mentioned that they wanted to “know the provider” and “trust them.” Facilitators from the literature and community assessment overlapped in the recommendation for support systems, which can be considered patient navigation and reminder calls.
Of the 61 patients surveyed, 43 patients (70%) were having their first mammogram. 49 (80%) responded that the reason for scheduling their appointment was as part of a routine prevention physical. Thirty nine (64%) reported delaying health services in the last year due to cost and 33 (54%) had delayed due to lack of insurance. Overall, 33% of women missed their previous mammogram appointment because of time and inconvenience (working or caring for others), 27% forgot, 22% had no money, and 18% had other reasons (miscommunication, not having doctor’s order, transportation and afraid of mammography). When asked the general question, “what is keeping women from getting their mammograms,” the responses were: scared of the outcome of cancer, cost, fear of the pain and putting themselves last (caregiving).
Phase II: Organizational Assessment
The paperwork process for underserved patients seeking mobile mammography appointments began with an application for sponsorship to ascertain information on demographics (age, marital status), income, screening history and other medical information. Patients were also required to bring proof of income through tax returns, or pay stubs to their appointment in order to receive a mammogram on a reduced fee scale with a fee of either $20 or $100 based on income. Staff made reminder calls only if the mobile coordinator had the schedule of appointed patients in advance with enough time to complete the calls. Because the mobile mammography program coordinates appointments with community partners, final schedules are often delayed or incomplete making routine reminder calls impossible.
The geographic coverage of the mobile units included most of Harris County indicating that geographic accessibility was available overall. However, the mobile units’ coverage in neighborhoods at increased need was very limited. Additionally, the number of free/reduced cost mammograms is limited because it is based on availability of offset from proportion of paid mammograms and from federal, state and foundation funds available to cover screening costs for uninsured women.
Phase III: Search for and Selection of an Evidence-based Intervention
The logic model of the problem created from the community assessment is shown in Figure 2.
Figure 2.
Logic model of the problem.
We identified four candidate programs. Table 2 presents each program with the parameters of comparison from the logic model. One RTIP program met the combined evaluation criteria. We selected “Breast Cancer Screening Among Non-Adherent Women,” a tailored telephone counseling program developed by Duke University and Kaiser Foundation Health Plan(Lipkus, 2000). The program, based on the Transtheoretical Model of Change (DiClemente and Prochaska, 1998) assessed a woman’s readiness to obtain mammography through a series of survey questions and counseled her through any barriers to appointment attendance.
Table 2.
Results of RTIPs Intervention Search
| Program Name | Priority Population and Strength of Effect | Logic Model of the Problem: Health, Behavior, Determinants | Organizational Fit (Resources) | Adaptations Needed? |
|---|---|---|---|---|
|
Breast Cancer Screening among Nonadherent Women (Lipkus et al., 2000) |
Good: Females age 40+; African American and White Un- or under-screened Non-compliant HMO members Good: Intervention Impact 3.5 |
Good: Targets breast cancer; mammography, and most barriers. Does not target fear of abandonment if cancer is discovered. Although, most barriers are covered, does not include local language or detail. Does not target the specific behavior of appointment keeping once an appointment is made. | Excellent: Phone based counseling program; One call per patient; Average call time 6 minutes. Fits with organizational assessment. Original implementation by research staff rather than clinic staff. |
Add appointment keeping as specific behavior. Streamline implementation to adjust to clinical setting. Edit barrier scripts to include specific local barriers, language and detail. Develop communication training to help clinic staff (rather than research staff hold natural conversations on the telephone while still eliciting and addressing specific barriers. |
|
The Forsyth County Cancer Screening Project (FoCaS) (Paskett, 1999) |
Good: Females age 40+ African American Medically underserved Moderate: Intervention Impact 2.0 |
Good: Breast cancer, mammography, targets fear barriers and faith. Also, environmental change not relevant to logic model of the problem |
Poor: Resource intensive clinic and community outreach (e.g., monthly classes, parties, and one-to-one) Also, physician behavior change (increasing referrals) is part of the program and not possible in current project |
NA. Intervention is not a good fit based on community outreach vs. clinical implementation. |
|
Friend to Friend (Slater, 1988) |
Good: Females ages 40+ African American, Hispanic, White Medically underserved Excellent: Intervention Impact 4.35 |
Good: Breast cancer, mammography, social networks, peer pressure, social support, modeling. Most of the barriers targeted do not match the logic model of the problem (physician recommendation, age, no family history, fear of radiation). | Moderate: Requires community outreach and education and continued outreach by participants | NA. Intervention is not a good fit based on community outreach vs clinical implementation. |
|
Witness Project (Erwin, 1999) |
Moderate: Females ages 19+ African American Medically underserved Moderate: Intervention Impact 3.0 |
Good: Breast Cancer, Mammography, modeling, social support. Targets fear related barriers. Other barriers targeted are context specific and depend on the experience of the women serving as witnesses. | Poor: Requires site visits, 8 hours of training followed by program sessions conducted in local churches. | NA. Program is not a good fit based on community outreach vs. clinical implementation. |
We considered the selected intervention a good match with the priority population because it targeted women aged 40 and over, included African American and un/under-screened women and targeted most of the determinants of behavior found in the focus groups (see Figure 2).. However, it did not focus on specifically on underserved women (uninsured and in need of financial assistance) and did not address all of the barriers identified in this study, including the fear of partner abandonment or the inability to take time off from work, and did not emphasize appointment keeping. Therefore, the intervention required adaptation to fit with the specific needs of our population. Proposed adaptations are also listed in Table 2.
We considered the intervention an excellent fit for our organizational context. It is a phone-based counseling program requiring only a brief phone call with each woman (average is under 6 minutes). This approach addressed the needs identified in the literature and community assessment for support systems, such as patient navigation and appointment reminder calls. Proposed adaptations for improving organizational fit as also listed in Table 2.
Discussion
In this study, our purpose was to conduct a community assessment and identify and select an evidence-based intervention program to reduce the no-show rates for mammography screening collaboratively with researchers and practitioners. With that in mind, we used an inductive exploratory sequential mixed methods design that incorporated organizational partners and community residents at various stages of the study and was conducted both within the community and the practice-based setting. We believe that this approach strengthened data collection by including the community in the process. One of the challenges noted to bridging research and practice has been the practitioners’ “need for speed” and relevance to the local community and problem and the researchers’ inherent desire to carefully evaluate the evidence base (Jansen et al., 2010). In this study, we were able to balance this issue by working in a participatory manner with the organizational partners and by conducting the needs assessment within a period of about three months.
The process used to search for and select an evidence-based intervention program in this study also provides a model to practice for cancer control planners. To date, very little has been published about how practitioners and/or researchers choose intervention programs for adaptation and implementation. Most peer-reviewed articles describe needs assessments and/or begin with program description and subsequent program adaptation (Krivitsky et al., 2012). Practitioners are often left to wonder how the authors arrived at their selected program and how they decided it was the “best” program for their implementation context. In this study, one of our practice partners noted she had been familiar with the National Cancer Institute RTIPs website since its inception, but couldn’t figure out how to decide what program would “fit” her organization and patient needs at the same time and how to interpret all the data provided about each intervention and make it into something she could actually use (personal communication, clinical site).
Additionally, it has been noted that practitioners often use brainstorming and colleague’s experience to make decisions about program selection, while not considering their validity (Jansen et al., 2010). In this study, we were able to address this issue by blending practice-based evidence with the peer-reviewed literature and needs assessment findings in order to create a logic model of the problem that incorporated both practice and academic evidence and using it to subsequently evaluate existing research-tested interventions in combination with the guiding questions developed by SAMHSA (Center for Substance Abuse Prevention, 2009). The use of SAMHSA’s guiding questions provided a structure for the assessment of basic fit for the identified research-tested intervention programs, while not being too onerous for the organizational partners. In addition, it allowed the partners to focus not just on the practical fit (e.g., organizational constraints) but also on the strength of the evidence for each program and the conceptual fit (matched with the priority population and logic model).
While the guiding questions were useful overall for evaluating basic fit, there were some limitations. The guiding questions are just that--general questions that practitioners/planners are to ask themselves when evaluating an intervention programs basic fit. No guidance is given on how to operationalize or weigh the questions to select a single “best” program. In this study, we used a four point scale from excellent through poor to help compare programs. However, our ranking for each program was ultimately subjective and based on group discussion. More detailed guidance and metrics for evaluation of basic program fit would be helpful for practitioners interested in comparing and selecting programs for use in the real world. This is an area for future research.
In conclusion, for future translational research and practice, more detailed guidance and metrics for evaluation of basic program fit would be helpful to enable selecting evidence-based programs for use in the real world. In addition, future studies that incorporate findings from needs assessment into the adaptation of the selected intervention program may promote the effective dissemination of evidence-based programs.
Supplementary Material
Acknowledgments
Data was shared by the Breast Health Collaborative of Texas, The Rose and Episcopal Health Charities for this study. Primary funding was provided by the Avon Foundation (grant numbers 05-2010-004, 05-2011-008). M.A. Hartman was supported by the Postdoctoral Fellowship, University of Texas – School of Public Health Cancer Education and Career Development Program – National Cancer Institute (NIH Grant R25 CA57712). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Biographies
Dr. L. Highfield, PhD., MS., is an Assistant Professor in Community Health Practice at the University of Texas School of Public Health Houston.
Dr. M. A. Hartman is a Postdoctoral Fellow at the University of Texas School of Public Health Houston; Cancer Education and Career Development Program of the National Cancer Institute.
Dr. L. Kay Bartholomew, EdD., is a Professor in Behavioral Sciences and Health Promotion at the University of Texas School of Public Health. She is also the Associate Dean for Academic Affairs.
Molly is a grants associate at the Episcopal Health Charities and maintains a joint appointment in the Center for Community Based Research at the Episcopal Health Charities.
Philomene is a statistician in the Center for Community Based Research at the Episcopal Health Charities.
Contributor Information
L. Highfield, Email: linda.d.highfield@uth.tmc.edu.
L.K. Bartholomew, Email: Leona.k.bartholomew@uth.tmc.edu.
M. A. Hartman, Email: Marieke.A.Hartman@uth.tmc.edu.
M.M. Ford, Email: mford@sleh.com.
P. Balihe, Email: pbalihe@sleh.com.
References
- Alexandraki I, Mooradian AD. Barriers related to mammography use for breast cancer screening among minority women. Journal of the National Medical Association. 2010;102(3):206–218. doi: 10.1016/s0027-9684(15)30527-7. [DOI] [PubMed] [Google Scholar]
- Bartholomew LK, Parcel GS, Kok G, Gottlieb NH, Fernandez ME. Planning health promotion programs: an intervention mapping approach. Jossey-Bass; 2011. [Google Scholar]
- Beatty PC, Willis GB. Research synthesis: The practice of cognitive interviewing. Public Opinion Quarterly. 2007;71(2):287–311. [Google Scholar]
- Bernstein J, Mutschler P, Bernstein E. Keeping mammography referral appointments: motivation, health beliefs, and access barriers experienced by older minority women. Journal of Midwifery & Women’s Health. 2000;45(4):308–313. doi: 10.1016/s1526-9523(00)00037-4. [DOI] [PubMed] [Google Scholar]
- Brownson RC, Baker EA, Leet TL, Gillespie KN, True WR. Evidence-based public health. New York, NY: Oxford University Press; 2010. [Google Scholar]
- Brownson RC, Fielding JE, Maylahn CM. Evidence-based public health: a fundamental concept for public health practice. Annual review of public health. 2009;30:175–201. doi: 10.1146/annurev.publhealth.031308.100134. [DOI] [PubMed] [Google Scholar]
- Burgio LD. Disentangling the translational sciences: A social science perspective. Research and Theory for Nursing Practice. 2010;24(1):56–63. doi: 10.1891/1541-6577.24.1.56. [DOI] [PubMed] [Google Scholar]
- Center for Substance Abuse Prevention. HHS Pub No (SMA) 09-4205. Rockville, MD: Center for Substance Abuse Prevention, Substance Abuse and Mental Health Services Administration; 2009. Identifying and Selecting Evidence-Based Interventions Revised Guidance Document for the Strategic Prevention Framework State Incentive Grant Program. [Google Scholar]
- Crump SR, Mayberry RM, Taylor BD, Barefield KP, Thomas PE. Factors related to noncompliance with screening mammogram appointments among low-income African-American women. Journal of the National Medical Association. 2000;92(5):237. [PMC free article] [PubMed] [Google Scholar]
- DiClemente CC, Prochaska JO. Toward a comprehensive Transtheoretical Model of change. In: Miller W, Heather N, editors. Treating addictive behaviors. Plenum Press; 1998. pp. 3–24. [Google Scholar]
- Erwin DO, Spatz TS, Stotts RC, Hollenberg JA. Increasing mammography practice by African American women. Cancer Practice. 1999;7(2):78–85. doi: 10.1046/j.1523-5394.1999.07204.x. [DOI] [PubMed] [Google Scholar]
- Green LW, Kreuter MW. Health program planning: An educational and ecological approach. 4. San Francisco, CA: McGraw Hill Professional; 2005. [Google Scholar]
- Green LW. Making research relevant: if it is an evidence-based practice, where’s the practice-based evidence? Family Practice. 2008;25(suppl 1):i20–i24. doi: 10.1093/fampra/cmn055. [DOI] [PubMed] [Google Scholar]
- Green LW. Public health asks of systems science: to advance our evidence-based practice, can you help us get more practice-based evidence? American Journal of Public Health. 2006;96(3):406–409. doi: 10.2105/AJPH.2005.066035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green LW, Ottoson J, Garcia C, Robert H. Diffusion theory and knowledge dissemination, utilization, and integration in public health. Annual Review of Public Health. 2009;30:151. doi: 10.1146/annurev.publhealth.031308.100049. [DOI] [PubMed] [Google Scholar]
- Highfield L, Arthasarnprasit J, Ottenweller CA, Dasprez A. Interactive webbased mapping: bridging technology and data for health. Int J Health Geogr. 2011;10:69. doi: 10.1186/1476-072X-10-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansen MW, Van Oers HA, Kok G, De Vries NK. Public health: disconnections between policy, practice and research. Health Res Policy Syst. 2010;8:37–49. doi: 10.1186/1478-4505-8-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerner J, Rimer B, Emmons K. Introduction to the special section on dissemination: dissemination research and research dissemination: how can we close the gap? Health Psychology. 2005;24(5):443. doi: 10.1037/0278-6133.24.5.443. [DOI] [PubMed] [Google Scholar]
- Knafl K, Deatrick J, Gallo A, Holcombe G, Bakitas M, Dixon J, Grey M. The analysis and interpretation of cognitive interviews for instrument development. Research in Nursing & Health. 2007;30(2):224–234. doi: 10.1002/nur.20195. [DOI] [PubMed] [Google Scholar]
- Ko CM, Sadler GR, Ryujin L, Dong A. Filipina American women’s breast cancer knowledge, attitudes, and screening behaviors. BMC Public Health. 2003;3(1):27. doi: 10.1186/1471-2458-3-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohatsu ND, Robinson JG, Torner JC. Evidence-based public health: an evolving concept. American Journal of Preventive Medicine. 2004;27(5):417–421. doi: 10.1016/j.amepre.2004.07.019. [DOI] [PubMed] [Google Scholar]
- Krivitsky LN, Parker SJ, Pal A, Meckler L, Shengelia R, Reid MC. A systematic review of health promotion and disease prevention program adaptations: How are programs adapted? In: Wethington E, Dunifon R, editors. Translational research for improving outcomes across the life course. Washington, DC: American Psychological Association Press; 2012. pp. 73–99. [Google Scholar]
- Lau A. Making the case for selective and directed cultural adaptations of evidence-based: Examples from parent training. Clinical Psych-Sci and Pract. 2006;13:295–310. [Google Scholar]
- Legler J, Meissner HI, Coyne C, Breen N, Chollette V, Rimer BK. The effectiveness of interventions to promote mammography among women with historically lower rates of screening. Cancer Epidemiology Biomarkers & Prevention. 2002;11(1):59–71. [PubMed] [Google Scholar]
- Lipkus IM, Rimer BK, Halabi S, Strigo TS. Can tailored interventions increase mammography use among HMO women? American Journal of Preventive Medicine. 2000;18(1):1–10. doi: 10.1016/s0749-3797(99)00106-3. [DOI] [PubMed] [Google Scholar]
- Moy B, Park ER, Feibelmann S, Chiang S, Weissman JS. Barriers to repeat mammography: cultural perspectives of African-American, Asian, and Hispanic women. Psycho-Oncology. 2006;15(7):623–634. doi: 10.1002/pon.994. [DOI] [PubMed] [Google Scholar]
- [Accessed July 2013];NIH Roadmap for Clinical Research: Clinical Research Networks and NECTAR. http://nihroadmap.nih.gov/clinicalresearch/overview-networks.asp.
- Ogedegbe G, Cassells AN, Robinson CM, DuHamel K, Tobin JN, Sox CH, Dietrich AJ. Perceptions of barriers and facilitators of cancer early detection among low-income minority women in community health centers. Journal of the National Medical Association. 2005;97(2):162. [PMC free article] [PubMed] [Google Scholar]
- O’Malley AS, Forrest CB, Mandelblatt J. Adherence of Low-income Women to Cancer Screening Recommendations. Journal of General Internal Medicine. 2002;17(2):144–154. doi: 10.1046/j.1525-1497.2002.10431.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paskett ED, Tatum CM, D’Agostino R, Rushing J, Velez R, Michielutte R, Dignan M. Community-based interventions to improve breast and cervical cancer screening: results of the Forsyth County Cancer Screening (FoCaS) Project. Cancer Epidemiology Biomarkers & Prevention. 1999;8(5):453–459. [PubMed] [Google Scholar]
- Paskett ED, Tatum C, Rushing J, Michielutte R, Bell R, Foley KL, Dickinson S. Racial differences in knowledge, attitudes, and cancer screening practices among a triracial rural population. Cancer. 2004;101(11):2650–2659. doi: 10.1002/cncr.20671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peek ME, Sayad JV. Fear, fatalism and breast cancer screening in low-income African-American women: The role of clinicians and the health care system. Journal of General Internal Medicine. 2008;23(11):1847–1853. doi: 10.1007/s11606-008-0756-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Research-tested Interventions Programs website. National Cancer Institute and Substance Abuse and Mental Health Services Administration; [Accessed on: 09/24/2013]. http://rtips.cancer.gov/rtips/. Last Updated: 09/24/2013. [Google Scholar]
- Ryan GW, Bernard HR. Data management and analysis methods. In: Denzin N, Lincoln Y, editors. Handbook of qualitative research. Thousand Oaks, CA: Sage; 2000. pp. 769–802. [Google Scholar]
- Schueler KM, Chu PW, Smith-Bindman R. Factors associated with mammography utilization: a systematic quantitative review of the literature. Journal of Women’s Health. 2008;17(9):1477–1498. doi: 10.1089/jwh.2007.0603. [DOI] [PubMed] [Google Scholar]
- Slater JS, Nim Ha C, Malone ME, McGovern P, Madigan SD, Finnegan JR, Lurie N. A randomized community trial to increase mammography utilization among low-income women living in public housing. Preventive Medicine. 1998;27(6):862–870. doi: 10.1006/pmed.1998.0370. [DOI] [PubMed] [Google Scholar]
- Smith-Bindman R, Miglioretti DL, Lurie N, Abraham L, Barbash R, Strzelczyk J, Kerlikowske K. Does Utilization of Screening Mammography Explain Racial and Ethnic Differences in Breast Cancer? Annals Of Internal Medicine. 2006;144(8):541–W89. doi: 10.7326/0003-4819-144-8-200604180-00004. [DOI] [PubMed] [Google Scholar]
- Snowdon W, Schultz J, Swinburn B. Problem and solution trees: a practical approach for identifying potential interventions to improve population nutrition. Health Promotion International. 2008;23(4):345–353. doi: 10.1093/heapro/dan027. [DOI] [PubMed] [Google Scholar]
- Tejeda S, Thompson B, Coronado GD, Martin DP. Barriers and facilitators related to mammography use among lower educated Mexican women in the USA. Social Science & Medicine. 2009;68(5):832–839. doi: 10.1016/j.socscimed.2008.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells KJ, Battaglia TA, Dudley DJ, Garcia R, Greene A, Calhoun E, Raich PC. Patient navigation: state of the art or is it science? Cancer. 2008;113(8):1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.