Abstract
Objective. To acquire more data about the epidemiologic characteristics of constipation in different kinds of populations in China. Methods. Using “constipation” and “China” as search terms; relevant papers were searched from January 1995 to April 2014. Data on prevalence, gender, diagnostic criteria, geographical area, educational class, age, race, and physician visit results were extracted and analyzed. Results. 36 trials were included. Prevalence rates of constipation in elderly population (18.1%) and pediatric population (18.8%) were significantly higher than that in general population (8.2%). Prevalence of constipation defined by non-Rome criteria was higher than that by Rome criteria in general population. Prevalence rates of constipation were different for different geographical area. People with less education were predisposed to constipation. In pediatric population, prevalence of constipation was the lowest in children aged 2–6 years. Prevalence of constipation in ethnic minorities was higher than that in Han people. People with constipation were predisposed to FD, haemorrhoid, and GERD. Only 22.2% patients seek medical advice in general population. Conclusions. In China, prevalence of constipation was lower compared with most of other countries. The factors including female gender, diagnostic criteria, geographical area, age, educational class, and race seemed to have major effects on prevalence of constipation.
1. Introduction
Constipation is a common problem in the clinical practice. In Western countries, prevalence rate of constipation was reported to be between 2% and 28% [1–4] and was more common among women [5]. In Hong Kong, China, 14% of the general population had this complaint [6]. In recent years, the prevalence of constipation is increasing in China. Although a range of studies concerning epidemiology of constipation has been carried out, results were not uniform. It was reported by Shi et al. [7] and Xiong et al. [8] that prevalence of constipation in rural area was significantly higher compared with that in urban area, while Kan et al. [9] and Zhao et al. [10] reported that there was no significant difference in the prevalence between rural and urban area. On the other hand, Zhao et al. [10] and Wei et al. [11] indicated that there was no association between constipation and education, but Xiong et al. [8] reported that prevalence of constipation increased with less education. Moreover, no systematic review has been reported to evaluate the epidemiology of constipation in China. Therefore, the purpose of this systematic review was to acquire more data about the epidemiologic characteristics of constipation in China.
2. Materials and Methods
2.1. Search Strategy
Using constipation, functional constipation, chronic constipation, idiopathic constipation, prevalence, rate, proportion, epidemiology, morbidity, and China as search terms, relevant papers in English and non-English were searched in PubMed, Embase, Google scholar, ISI Web of Science, CJFD, WeiPu, and WanFang from January 1995 to April 2014. The reference lists of published articles were then used to locate other relevant studies, and the papers that fulfill the inclusion criteria were selected for further investigation. We also wrote email to corresponding authors of the relevant articles we found and asked whether the authors had knowledge of other relevant articles not yet published. When an article provided insufficient information to enter data for an analysis, we wrote email to corresponding author and asked for the needed information.
2.2. Inclusion Criteria and Exclusion Criteria
Inclusion criteria were as follows: (i) studies about prevalence of constipation in China were considered; (ii) results published in full text form; (iii) the data including at least two aspects among prevalence, sex, diagnostic criteria of constipation, age, educational class, race, and physician visit; (iv) diagnosis of constipation defined according to a questionnaire or a physician's diagnosis or based on the self-reported, Rome II or III criteria.
Exclusion criteria were as follows: (i) repetitive studies or patients researched that were duplicated; (ii) abstracts; (iii) studies with insufficient data; and (iv) studies that only investigated the special population, such as students, soldiers, and women.
2.3. Study Selection
All papers were examined separately by two reviewers (Huikuan Chu and Likun Zhong). If there was disagreement, all inconsistencies on article selection were resolved by discussion. If the abstracts met the first two inclusion criteria, the full texts were found manually by contacting the author or other methods to make sure of the integrity and reliability of the data. Choose a recent study with sufficient information if there were several studies written by the authors with the duplicate patients. Otherwise, choose all the papers if the patients were not duplicate in the papers written by the same author.
2.4. Data Extraction
Data were extracted from each study mainly focused on prevalence, gender, diagnostic criteria, geographical area, educational class, age, race, and physician visit results.
2.5. Quality Evaluation
Quality of each study was assessed through the guidelines developed by Loney and colleagues for critical appraisal of research on prevalence and incidence. The scoring system is based on 8 items including setting with random sample or whole population, unbiased sampling frame, adequate sample size, standard criteria used for measurement, health outcome measured in an unbiased fashion, adequate response rate, reports prevalence or incidence with conidence interval by subgroup and detailed description of study subjects. A score of 0 or 1 is assigned for each item, for a possible range of 0 to 8 [12].
2.6. Statistical Analysis
Data were analyzed through SPSS Version 17.0 (SPSS Inc., Chicago, IL, USA) and Excel. Proportions were evaluated by standard formula and proportions of various groups were compared by χ 2 test.
3. Results
3.1. Study Descriptions
A total of 315 potentially relevant studies were identified using the search strategy. After the first round of analysis, 247 of them were excluded and 32 studies were excluded from further evaluation (duplicate 7, abstract 5, gastrointestinal outpatient 6, university students 7, soldiers 3, women 2, nurse 1, and coal miners 1). Finally, 36 relevant studies (29 in Chinese and 7 in English [6, 10, 13–17]) were included in the meta-analysis for data extraction: 15 in the general population, 14 in pediatric population, and 7 in elderly population (Tables 1, 2, and 3).
Table 1.
Characteristics of included papers (in general population).
| Author | Area of origin | Population | Year of publication | Diagnosed criteria | Number of investigated people | Number of patients | Quality score |
|---|---|---|---|---|---|---|---|
| Zhao et al. [10] | Five cities in China | 18–80 years | 2011 | Rome II | 16078 | 948 | 7 |
| Cheng et al. [6] | Hong Kong | 18–80 years | 2003 | Rome II | 3282 | 458 | 7 |
| Wei et al. [11] | Guangzhou City | >18 years | 2001 | Rome II | 2892 | 108 | 5 |
| Xiong et al. [8] | Guangdong Province | 18–80 years | 2004 | Rome II | 3931 | 159 | 6 |
| Shen et al. [68] | Shanghai City | 18–97 years | 2012 | Rome III | 7648 | 211 | 4 |
| Kan et al. [9] | Tianjin City | >18 years | 2003 | <3 BMs/week | 7220 | 838 | 5 |
| Tang et al. [69] | Anhui Province | >18 years | 2008 | Rome III | 3709 | 139 | 4 |
| Zuo and Han [70] | Henan Province | 2–92 years | 2012 | Rome III | 6102 | 1108 | 4 |
| Shi et al. [7] | Xinjiang Autonomous Region | >10 years | 2010 | Rome II | 1354 | 285 | 4 |
| Lv et al. [71] | Nanchang City | 10–91 years | 2005 | Rome II | 3745 | 122 | 4 |
| Guo et al. [72] | Beijing City | 18–70 years | 2001 | Rome II | 2486 | 151 | 6 |
| Xiang et al. [73] | Chongqing City | >18 years | 2004 | Rome II | 1492 | 47 | 4 |
| Zhang et al. [74] | Sichuan Province | 11–90 years | 2008 | Rome II | 2912 | 96 | 5 |
| Zhang et al. [75] | Henan Province | General population | 2008 | <3 BMs/week | 1838 | 163 | 4 |
| Liu et al. [76] | Hangzhou City | 1 y–99 years | 2004 | <2 BMs/week | 5107 | 899 | 4 |
Table 2.
Characteristics of included papers (in pediatric population).
| Author | Area of origin | Population | Year of publication | Diagnosed criteria | Number of investigated people | Number of patients | Quality score |
|---|---|---|---|---|---|---|---|
| Xu et al. [18] | Guangdong Province | 2–6 years | 2008 | Rome III | 1022 | 32 | 4 |
| Zhou et al. [77] | Guangdong Province | 6-18 years | 2010 | Rome III | 2075 | 130 | 5 |
| Zhou et al. [78] | Shanghai City | 10–18 years | 2008 | Rome II | 51956 | 13467 | 5 |
| Wang et al. [79] | Beijing City | 2–14 years | 2003 | <3 BMs/week or hard | 1001 | 38 | 5 |
| Liu et al. [80] | Chengdu City | 2–7 years | 2007 | Strain or hard or <3 BMs/week | 1132 | 54 | 3 |
| Hu [81] | Xian City | 2–12 years | 2003 | Strain or hard or <3 BMs/week | 1001 | 44 | 4 |
| Zhang et al. [82] | Five cities in north | 4–14 years | 2010 | Rome III | 19286 | 913 | 4 |
| M. F. Chan and Y. L. Chan [13] | Hong Kong | 3–5 years | 2010 | <3 BMs/week | 383 | 28 | 6 |
| Lee et al. [14] | Hong Kong | 3–5 years | 2008 | Rome II | 368 | 106 | 6 |
| Ip et al. [15] | Hong Kong | 3–5 years | 2005 | Rome II | 561 | 166 | 5 |
| Liang and Song [83] | Guangdong Province | 6–8 months | 2003 | Strain or hard or <3 BMs/week | 287 | 78 | 3 |
| Liu et al. [84] | Shanghai City | 0–24 months | 2009 | Rome III | 5030 | 690 | 4 |
| Tam et al. [17] | Hong Kong | 6–15 years | 2012 | Rome III | 2318 | 282 | 5 |
| Zhou et al. [16] | Shanghai City | 12–18 years | 2011 | Rome III | 3671 | 915 | 6 |
Table 3.
Characteristics of included papers (in elderly population).
| Author | Area of origin | Population | Year of publication | Diagnosed criteria | Number of investigated people | Number of patients | Quality score |
|---|---|---|---|---|---|---|---|
| Li et al. [85] | Beijing City | >60 years | 2000 | Strain or hard or <3 BMs/week | 1434 | 291 | 4 |
| Cai et al. [86] | Nanjing City | >60 years | 2004 | Strain or hard or <3 BMs/week | 3731 | 897 | 3 |
| Yu et al. [65] | Beijing City | >60 years | 2001 | Strain or hard or <3 BMs/week | 8252 | 950 | 4 |
| Pan and Shen [87] | Beijing City | >60 years | 2008 | Rome II | 114 | 45 | 4 |
| Liu et al. [19] | Tangshan City | >60 years | 2007 | Strain or hard or <3 BMs/week | 545 | 369 | 3 |
| Guo et al. [88] | Tianjin City | >70 years | 2004 | Strain or hard or <3 BMs/week | 76 | 32 | 3 |
| Huang and Zhang [89] | Sichuan Province | >60 years | 1999 | <3 BMs/week | 741 | 115 | 4 |
3.1.1. Prevalence of Constipation
The overall prevalence rates of constipation in 36 different population groups widely ranged from a low 3.1% in a pediatric population in Guangdong Province [18] to a high 67.8% in an elderly population in Tangshan City [19]. More than half of the studies with prevalence rates range from 3% to 10%. A total of 69796 cases in general population were studied and 5732 patients with constipation were found, with a prevalence rate of 8.2%. 2699 patients were found in 14893 cases in elderly population and the prevalence rate was 18.1%. The mean value of prevalence rate in pediatric population was 18.8% (16943/90091). There were significant differences among general population, pediatric population, and elderly population (χ 2 = 51956.5, P < 0.001).
3.1.2. Diagnostic Criteria Differences in the Prevalence of Constipation
As we know, the diagnostic criteria of constipation range from self-reported to consensus criteria like Rome II criteria and Rome III criteria [20, 21]. The diagnosis of constipation could be on the basis of symptoms self-reported by the individual or defined according to a questionnaire, according to a physician's diagnosis, or based on the Rome II or Rome III criteria. We defined the diagnostic criteria that did not conform to the Rome criteria as non-Rome criteria. Considering the limited number of studies for each criteria, we just investigated the difference between non-Rome criteria and Rome criteria which included Rome II criteria and Rome III criteria.
In general population, 12 papers that defined constipation by Rome criteria were included and the average prevalence of constipation was 6.9%, which was lower than that by non-Rome criteria reported by 3 papers with a prevalence rate of 13.4% (χ 2 = 24635.1, P < 0.001). As one paper reported the prevalence of constipation defined by Rome criteria, differences between Rome criteria and non-Rome criteria were not assessed in elderly population. As we know, prevalence of constipation was different for pediatric population with different age and prevalence rate in Hong Kong being higher than that in Chinese Mainland; we only investigated the difference of prevalence rate for children aged 2–14 years in Chinese Mainland. 2 papers defined constipation by Rome criteria and 3 papers with non-Rome criteria. The result showed that prevalence of constipation was 4.7% by Rome criteria and 4.3% by non-Rome criteria. There was no significant difference between two criteria (χ 2 = 0.6, P = 0.43).
During the following comparing, we just compared the cases diagnosed by Rome criteria in general population and the cases based on same diagnostic criteria in elderly population considering the diagnostic criteria differences in the prevalence of constipation.
3.1.3. Gender Differences in the Prevalence of Constipation
There were 27 trails written about the gender of patients: 11 in general population, 4 in elderly population, and 12 in pediatric population. The result of our research implied that prevalence of constipation in female was higher than that in male for all groups, with the ratio (male/female) of 1 : 1.4 in general population, 1 : 1.1 in elderly population, and 1 : 1.1 in pediatric population (Table 4). Generally speaking, prevalence of constipation in women was higher and females were more likely to report FC than males.
Table 4.
Gender differences in the prevalence of constipation.
| Male | Female | Ratio male/female | |
|---|---|---|---|
| General population | 5.6% | 8.1% | 1 : 1.4 |
| Elderly population | 14.9% | 16.7% | 1 : 1.1 |
| Pediatric population | 19.1% | 21.6% | 1 : 1.1 |
3.1.4. Age Differences in the Prevalence of Constipation
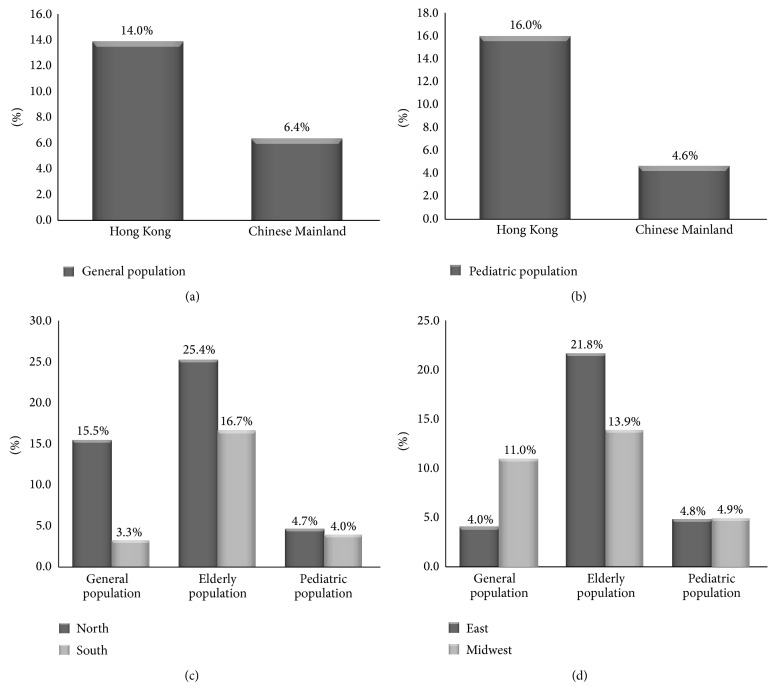
In general population, prevalence of constipation was the lowest in people aged 30–39 years old and prevalence of constipation increases with age for people older than 30 (in general population χ 2 = 357.1, P < 0.001). In elderly population, the results indicated that prevalence of constipation increased with age. There were significant differences among different aged people in elderly population (χ 2 = 3080.8, P < 0.001). In pediatric population, children aged 2–6 years had the lowest prevalence of constipation (4.8%) and children older than 6 years had the highest prevalence rate (21.1%). There were significant differences among different aged people in pediatric population (χ 2 = 1416.3, P < 0.001) (Figure 1).
Figure 1.
Age difference in the prevalence of constipation. Prevalence of constipation was the lowest in people aged 30–39 years old in general population and prevalence of constipation increased with age for people older than 30 in general population and elderly population. Children aged 2–6 years had the lowest prevalence of constipation and older than 6 years had the highest prevalence in pediatric population.
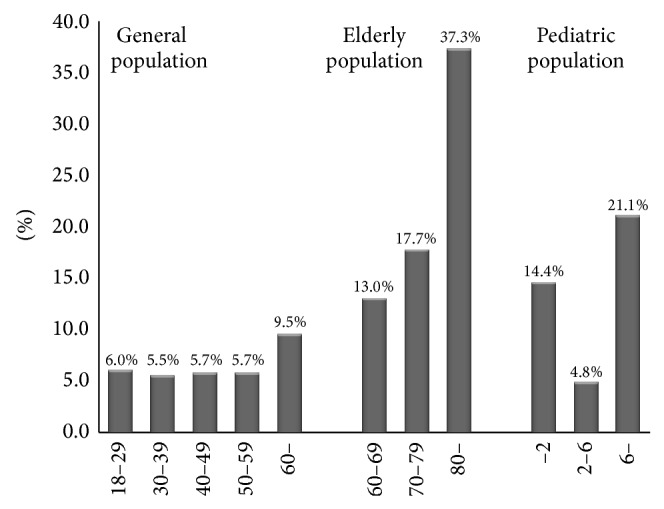
3.1.5. Regional Differences in the Prevalence of Constipation
In general population, we just compared the cases diagnosed by Rome II criteria considering the diagnostic criteria differences in the prevalence of constipation. The prevalence rate of constipation in Hong Kong was significantly higher than that in Chinese Mainland (14.0% versus 6.4%; χ 2 = 43277.5, P < 0.001). Prevalence rate was 15.5% in Northern area and 3.3% in Southern area and there were significant differences between them (χ 2 = 7403.5, P < 0.001). Prevalence rate in Eastern area was 4.0% and that in Midwestern area was 11.0%. There was significant difference between them (χ 2 = 872.7, P < 0.001). In elderly population, as there were limited studies that reported the epidemiology of Hong Kong, we only analyzed the differences between Northern and Southern area and between Eastern and Midwestern area. Prevalence rates were 25.4% in Northern area, 16.7% in Southern area, 21.8% in Eastern area, and 13.9% in Midwestern area. The result implied that there were significant differences for both of them (between Northern area and Southern area χ 2 = 117.1, P < 0.001 and between Eastern area and Midwestern area χ 2 = 5512.2, P < 0.001). In 2- to 15-year-old children, the prevalence of constipation in Hong Kong was 16.0% and that in Chinese Mainland was 4.6%. There were significant differences between them (χ 2 = 711.2, P < 0.001). The prevalence rates were 4.7% in Northern area, 4.0% in Southern area, 4.8% in Eastern area, and 4.9% in Midwestern area. There were no significant differences between Northern and Southern area (χ 2 = 2.1, P = 0.15), as well as between Eastern and Midwestern area (χ 2 = 0.15, P = 0.7) (Figure 2).
Figure 2.
Regional difference in the prevalence of constipation. (a) In general population, the prevalence rate of constipation in Hong Kong was higher than that in Chinese Mainland. (b) In pediatric population, the prevalence rate of constipation in Hong Kong was higher than that in Chinese Mainland. (c) Prevalence rate of constipation in Northern area was significantly higher than that in Southern area in general population and elderly population, while there was no significant difference between Northern area and Southern area in pediatric population. (d) Prevalence rate of constipation in Eastern area was significantly lower than that in Midwestern area in general population, while prevalence rate in Eastern area was significantly higher than that in Midwestern area in elderly population, and there was no significant difference between Eastern area and Midwestern area in pediatric population.
3.1.6. Urban and Rural Differences in the Prevalence of Constipation
4 trails in general population and 3 papers in elderly population investigated differences of the prevalence of constipation between urban and rural area. In general population, prevalence of constipation in urban area was 6.7%, which was significantly lower than that in rural area with a prevalence rate of 7.2% (χ 2 = 154.4, P < 0.001). In elderly population, prevalence rate in urban area was 12.0%, lower than that in rural area with a prevalence rate of 14.1% (χ 2 = 10.5, P < 0.001). Four papers assessed the difference of the prevalence of constipation between urban and rural area people in pediatric population. Prevalence of constipation in urban area (4.1%) was lower than that in rural area (4.6%); however, there was no significant difference between them (χ 2 = 0.45, P = 0.5).
3.1.7. Educational Differences in the Prevalence of Constipation
In general population and elderly population, prevalence rate of constipation increased with less education (in general population χ 2 = 8468.4, P < 0.001; in elderly population χ 2 = 2618.7, P < 0.001) (Figure 3).
Figure 3.
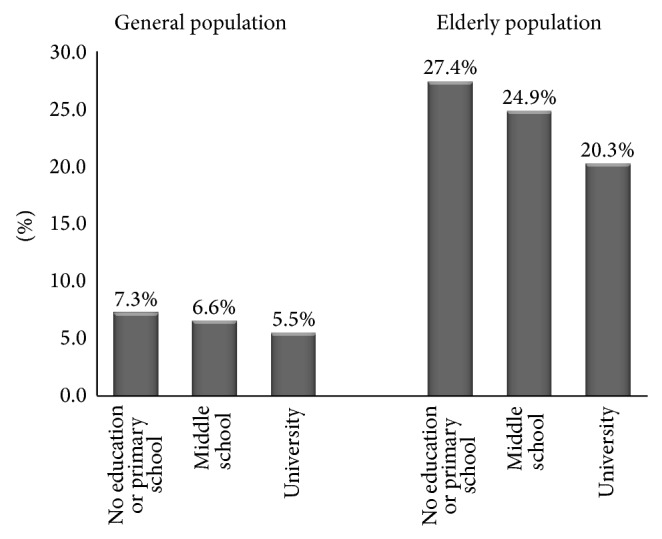
Education difference in the prevalence of constipation. Prevalence rate of constipation increased with less education in general population and elderly population.
3.1.8. Racial Differences in the Prevalence of Constipation
In general population, 2 papers reported the race difference in the prevalence of constipation. 149 patients were found in 811 cases in ethnic minorities, with a result that prevalence of constipation was 18.4%, which was higher than that in Han people with a prevalence rate of 12.5% (χ 2 = 22.2, P < 0.001).
3.1.9. Incidence of Other Digestive Disorders for People with Constipation
In general population, 2 papers reported the relationship between constipation and FD, with a result of people with constipation being predisposed to FD (χ 2 = 712.0, P < 0.001). Kan et al. [9] reported that prevalence of hemorrhoid (χ 2 = 312.2, P < 0.001) and GERD (χ 2 = 60.3, P < 0.001) was higher in patients with constipation.
3.1.10. Physician Visit
We could only assess the physician visit of general population and pediatric population because of the limited report of elderly population. 6 trails studied the physician visit of general population with a result of 22.2%; 5 papers reported the physician visit of pediatric population with a result of 27.8%. On the other hand, the symptoms improved in 50.2% patients with constipation by increasing activity or more fiber intake instead of visiting physician in general population. 17.5% children improved their constipation by more activity or more fiber intake.
4. Discussion
The prevalence rate of constipation in general population in China was 8.2% in this review, which was lower than most of other countries such as 17.1% in Europe and Oceania [22], 16.5% in Korea [23], 19.4% in USA [24], and 14.9%–27.2% in Canada [25]. The difference may partially be due to the different dietary habits [26, 27]. Constipation in individuals with previously normal bowel function was associated with specific dietary patterns, such as low fiber intake which is involved with the pathogenesis of constipation [15, 28, 29]. Most people in our country have dietary habits consisting of increased consumption of fibers. On the other hand, life style and physical inactivity [30, 31] were risk factors for constipation. Compared with other countries, people in our country have different life style and more physical activity [32].
In general population, prevalence rate of constipation defined with Rome criteria was lower than that with non-Rome criteria. This may be due to different diagnostic criteria resulting in significant differences in prevalence rates [33] and every symptom was explicitly defined in Rome criteria whereas symptoms were simply described in non-Rome criteria, resulting in some patients who were included by non-Rome criteria rather than excluded by Rome criteria.
We found that females were more likely to report FC than males, which was consistent with that in North America [1, 34], Europe, and Oceania [22]. This predominance of females may be attributed to hormonal factors, inducing a higher risk of constipation during the luteal phase of the menstrual cycle, under the effects of progesterone, anatomic features of female pelvic floor, and the pelvic floor muscles and nerves damaged during delivery [35–38]. Posterior colpocele was an independent risk factor for constipation [39].
The prevalence of constipation increased with age in general population for people older than 30 and in elderly population. The trend that prevalence of constipation increased with age was consistent with other countries [22, 34], which may be due to the healthy status, medication [40], and physical inactivity [30]. For people older than 80 years old, the prevalence rate reached to 37.7%, which was in the range of the elderly constipation epidemiology in Western countries [1, 41–48]. The underlying reason for constipation in elderly population include insufficient intake of fluid and dietary fiber, reduced daily activities, lack of exercise, and diseases such as neurological and metabolic disorders [44–46, 49], in addition to drugs [50–57]. Healthy condition becomes poor and incidence of diabetes [58, 59], stroke, Parkinson's disease, and local neurogenic disorders [60–62] increased with age and people have to take more medicine to treat their disease condition. On the other hand, physical activities would be reduced with age. We should pay attention to that the established fact that the higher prevalence of constipation for elderly can cause a range of complications, such as anorectal pathology (e.g., fissures, hemorrhoids, rectal prolapse, etc.), sigmoid volvulus, fecal impaction, fecal incontinence, and urinary dysfunction [21, 63, 64].
In pediatric population, prevalence of constipation was highest in children older than 6 years who were school-aged children, which may be attributed to the high level of psychological stress caused by fast-paced and greatly competitive school environment [16].
In general and elderly population, prevalence of constipation in Northern area was higher than that in Southern area, which might be due to different dietary habits and socioeconomic status [65]. It was reported that increased intakes of rice at breakfast, lunch, and dinner were all associated with a decreased prevalence of constipation and low socioeconomic status is a risk factor for constipation [66]. In China, people in Southern area have the dietary habits with rice and socioeconomic status in Southern area was higher than Northern area. On the other hand, we could not exclude the cold and dry weather of Northern area which result in a higher prevalence of constipation [65]. Prevalence of constipation in Midwestern area was higher than that in Eastern area in general population and this may be attributed to the low socioeconomic status and dry weather of Midwestern area [7].
In general population and elderly population, prevalence of constipation in rural was higher than that in city. This may be attributed to the low socioeconomic condition [66] and less educational class [67]. In China, socioeconomic condition and educational class was lower for people living in rural area.
In this study, we found that there were racial differences in the prevalence of constipation. Prevalence of constipation in ethnic minorities was higher than that in Han people. This was similar with the result of America that prevalence of constipation was higher in non-Caucasians than in Caucasians [1]. This might be caused by the different dietary habits [26] and living style between different races.
In conclusion, compared with most of other countries, prevalence rate of constipation in China was lower and more common for women. The prevalence of constipation in general population was influenced by diagnostic criteria, area, age, educational class, and race. Risk factors of constipation in elderly population include geographical area, rural area, age, and educational class and that in children was mainly due to age. Only a small proportion of patients suffering from constipation seek medical consultation.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (NSFC) (2011 81070300) and Project of the National Key Technologies R&D Program in the 11th Five Plan period (2007 BAI04B01).
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Authors’ Contribution
Huikuan Chu designed the study and wrote the manuscript; Likun Zhong helped to search and selected studies; Hai Li, Xiujing Zhang, and Jingzhi Zhang helped to analyze data and give comments on the paper; and Xiaohua Hou checked and revised the paper.
References
- 1.Higgins P. D. R., Johanson J. F. Epidemiology of constipation in North America: a systematic review. The American Journal of Gastroenterology. 2004;99(4):750–759. doi: 10.1111/j.1572-0241.2004.04114.x. [DOI] [PubMed] [Google Scholar]
- 2.Adibi P., Behzad E., Pirzadeh S., Mohseni M. Bowel habit reference values and abnormalities in young Iranian healthy adults. Digestive Diseases and Sciences. 2007;52(8):1810–1813. doi: 10.1007/s10620-006-9509-2. [DOI] [PubMed] [Google Scholar]
- 3.Corazziari E. Definition and epidemiology of functional gastrointestinal disorders. Best Practice and Research: Clinical Gastroenterology. 2004;18(4):613–631. doi: 10.1016/j.bpg.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 4.Harris L. A. Prevalence and ramifications of chronic constipation. Managed Care Interface. 2005;18(8):23–30. [PubMed] [Google Scholar]
- 5.Talley N. J., O'Keefe E. A., Zinsmeister A. R., Melton L. J., III Prevalence of gastrointestinal symptoms in the elderly: a population-based study. Gastroenterology. 1992;102(3):895–901. doi: 10.1016/0016-5085(92)90175-x. [DOI] [PubMed] [Google Scholar]
- 6.Cheng C., Chan A. O. O., Hui W. M., Lam S. K. Coping strategies, illness perception, anxiety and depression of patients with idiopathic constipation: a population-based study. Alimentary Pharmacology and Therapeutics. 2003;18(3):319–326. doi: 10.1046/j.1365-2036.2003.01663.x. [DOI] [PubMed] [Google Scholar]
- 7.Shi H., Yao L., Zhou M. X. Analysis of the correlation between functional constipation and dry weather of west in China. Xinjiang Journal of Traditional Chinese Medicine. 2010;28(2):5–6. [Google Scholar]
- 8.Xiong L., Chen M., Chen H., et al. A community population-based epidemiologic study of chronic constipation in guangdong province. Chinese Journal of Digestion. 2004;24(8):488–491. [Google Scholar]
- 9.Kan Z. C., Yao H. C., Liu Z. W., et al. An Epidemiological Study of Chronic Constipation in Tianjin Residents. Chinese American Medical Society; 2003. The first constipation seminars. [Google Scholar]
- 10.Zhao Y.-F., Ma X.-Q., Wang R., Yan X.-Y., Li Z.-S., Zou D.-W., He J. Epidemiology of functional constipation and comparison with constipation-predominant irritable bowel syndrome: the Systematic Investigation of Gastrointestinal Diseases in China (SILC) Alimentary Pharmacology and Therapeutics. 2011;34(8):1020–1029. doi: 10.1111/j.1365-2036.2011.04809.x. [DOI] [PubMed] [Google Scholar]
- 11.Wei X. Q., Chen M. H., Wang J. H., et al. The epidemiology of irritable bowel syndrome and functional constipation of Guangzhou residents. Chinese Journal of Internal Medicine. 2001;40(8):517–520. [PubMed] [Google Scholar]
- 12.Loney P. L., Chambers L. W., Bennett K. J., Roberts J. G., Stratford P. W. Critical appraisal of the health research literature: prevalence or incidence of a health problem. Chronic Diseases in Canada. 1998;19(4):170–176. [PubMed] [Google Scholar]
- 13.Chan M. F., Chan Y. L. Investigating factors associated with functional constipation of primary school children in Hong Kong. Journal of Clinical Nursing. 2010;19(23-24):3390–3400. doi: 10.1111/j.1365-2702.2010.03362.x. [DOI] [PubMed] [Google Scholar]
- 14.Lee W. T. K., Ip K. S., Chan J. S. H., Lui N. W. M., Young B. W. Y. Increased prevalence of constipation in pre-school children is attributable to under-consumption of plant foods: a community-based study. Journal of Paediatrics and Child Health. 2008;44(4):170–175. doi: 10.1111/j.1440-1754.2007.01212.x. [DOI] [PubMed] [Google Scholar]
- 15.Ip K. S., Lee W. T. K., Chan J. S. H., Young B. W. Y. A community-based study of the prevalence of constipation in young children and the role of dietary fibre. Hong Kong Medical Journal. 2005;11(6):431–436. [PubMed] [Google Scholar]
- 16.Zhou H., Yao M., Cheng G.-Y., Chen Y.-P., Li D.-G. Prevalence and associated factors of functional gastrointestinal disorders and bowel habits in chinese adolescents: a school-based study. Journal of Pediatric Gastroenterology and Nutrition. 2011;53(2):168–173. doi: 10.1097/MPG.0b013e3182125388. [DOI] [PubMed] [Google Scholar]
- 17.Tam Y. H., Li A. M., So H. K., Shit K. Y., Pang K. K., Wong Y. S., Tsui S. Y., Mou J. W., Chan K. W., Lee K. H. Socioenvironmental factors associated with constipation in Hong Kong children and Rome III Criteria. Journal of Pediatric Gastroenterology and Nutrition. 2012;55(1):56–61. doi: 10.1097/MPG.0b013e31824741ce. [DOI] [PubMed] [Google Scholar]
- 18.Xu H. L., Lin S. H., Lin L. R., Ni M. Y., Ji X. F., Wu X. l. Epidemiologic survey of children with functional constipation in Jieyang City. Hainan Medical Journal. 2008;19(11):103–104. [Google Scholar]
- 19.Liu G. Q., Chen C. X., Wang Z. J., Zhao H. Investigation of prevalence and risk factor of constipation for elderly population in Tangshan. Modern Preventive Medicine. 2007;34(9):1749–1750. [Google Scholar]
- 20.Drossman D. A., Corazziari E., Talley N. J., Thompson W. G., Whitehead W. E. Rome II. The Functional Gastrointestinal Disorders. Diagnosis, Pathophysiology and Treatment: A Multinational Consensus. 2nd. McLean, Va, USA: Degnon Associates; 2000. [Google Scholar]
- 21.Drossman D. A. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006;130(5):1377–1390. doi: 10.1053/j.gastro.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 22.Peppas G., Alexiou V. G., Mourtzoukou E., Falagas M. E. Epidemiology of constipation in Europe and Oceania: a systematic review. BMC Gastroenterology. 2008;8, article 5 doi: 10.1186/1471-230X-8-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jun D. W., Park H. Y., Lee O. Y., Lee H. L., Yoon B. C., Choi H. S., Hahm J. S., Lee M. H., Lee D. H., Kee C. S. A population-based study on bowel habits in a Korean community: prevalence of functional constipation and self-reported constipation. Digestive Diseases and Sciences. 2006;51(8):1471–1477. doi: 10.1007/s10620-006-9087-3. [DOI] [PubMed] [Google Scholar]
- 24.Johanson J. F., Kralstein J. Chronic constipation: a survey of the patient perspective. Alimentary Pharmacology and Therapeutics. 2007;25(5):599–608. doi: 10.1111/j.1365-2036.2006.03238.x. [DOI] [PubMed] [Google Scholar]
- 25.Pare P., Ferrazzi S., Thompson W. G., Irvine E. J., Rance L. An epidemiological survey of constipation in Canada: definitions, rates, demographics, and predictors of health care seeking. The American Journal of Gastroenterology. 2001;96(11):3130–3137. doi: 10.1016/S0002-9270(01)03821-7. [DOI] [PubMed] [Google Scholar]
- 26.Sandler R. S., Jordan M. C., Shelton B. J. Demographic and dietary determinants of constipation in the US population. The American Journal of Public Health. 1990;80(2):185–189. doi: 10.2105/AJPH.80.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vives A. C., Allué I. P., Grupo de Trabajo Español para el Estudio del Estreñimiento en la Población Infantil Case-control study of risk factors associated with constipation. The FREI study. Anales de Pediatría. 2005;62(4):340–345. doi: 10.1157/13073247. [DOI] [PubMed] [Google Scholar]
- 28.Gomes R. C., Maranhão H. S., Pedrosa L. D. F. C., Morais M. B. Fiber and nutrients intake in constipated children. Arquivos de Gastroenterologia. 2003;40(3):181–187. doi: 10.1590/s0004-28032003000300009. [DOI] [PubMed] [Google Scholar]
- 29.Morais M. B., Vítolo M. R., Aguirre A. N. C., Fagundes-Neto U. Measurement of low dietary fiber intake as a risk factor for chronic constipation in children. Journal of Pediatric Gastroenterology and Nutrition. 1999;29(2):132–135. doi: 10.1097/00005176-199908000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Peters H. P. F., De Vries W. R., Vanberge-Henegouwen G. P., Akkermans L. M. A. Potential benefits and hazards of physical activity and exercise on the gastrointestinal tract. Gut. 2001;48(3):435–439. doi: 10.1136/gut.48.3.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khatri P. K., Ali A. D., Alzadjali N., Bhagia G., Khaliqdina S. J., Aziz S. Frequency of functional constipation in 3 different populations and its causative factors. Journal of the Pakistan Medical Association. 2011;61(11):1149–1152. [PubMed] [Google Scholar]
- 32.Kim S., Popkin B. M., Siega-Riz A. M., Haines P. S., Arab L. A cross-national comparison of lifestyle between China and the United States, using a comprehensive cross-national measurement tool of the healthfulness of lifestyles: the Lifestyle Index. Preventive Medicine. 2004;38(2):160–171. doi: 10.1016/j.ypmed.2003.09.028. [DOI] [PubMed] [Google Scholar]
- 33.Garrigues V., Gálvez C., Ortiz V., Ponce M., Nos P., Ponce J. Prevalence of constipation: agreement among several criteria and evaluation of the diagnostic accuracy of qualifying symptoms and self-reported definition in a population-based survey in Spain. The American Journal of Epidemiology. 2004;159(5):520–526. doi: 10.1093/aje/kwh072. [DOI] [PubMed] [Google Scholar]
- 34.McCrea G. L., Miaskowski C., Stotts N. A., Macera L., Varma M. G. A review of the literature on gender and age differences in the prevalence and characteristics of constipation in North America. Journal of Pain and Symptom Management. 2009;37(4):737–745. doi: 10.1016/j.jpainsymman.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 35.Wu J.-X., Liu X.-H., Liu W., Ke M.-Y., Fang X.-C. Investigation of female chronic constipation: a multi-center cross-sectional clinical study. Zhonghua Yi Xue Za Zhi. 2009;89(18):1255–1258. [PubMed] [Google Scholar]
- 36.Scott S. M., Knowles C. H., Newell M., Garvie N., Williams N. S., Lunniss P. J. Scintigraphic assessment of colonic transit in women with slow-transit constipation arising de novo and following pelvic surgery or childbirth. British Journal of Surgery. 2001;88(3):405–411. doi: 10.1046/j.1365-2168.2001.01699.x. [DOI] [PubMed] [Google Scholar]
- 37.Sloots C. E. J., Felt-Bersma R. J. F., Meuwissen S. G. M., Kuipers E. J. Influence of gender, parity, and caloric load on gastrorectal response in healthy subjects: A barostat study. Digestive Diseases and Sciences. 2003;48(3):516–521. doi: 10.1023/A:1022584632011. [DOI] [PubMed] [Google Scholar]
- 38.Chiarelli P., Brown W., McElduff P. Constipation in Australian women: prevalence and associated factors. International Urogynecology Journal and Pelvic Floor Dysfunction. 2000;11(2):71–78. doi: 10.1007/s001920050073. [DOI] [PubMed] [Google Scholar]
- 39.Soligo M., Salvatore S., Emmanuel A. V., de Ponti E., Zoccatelli M., Cortese M., Milani R. Patterns of constipation in urogynecology: clinical importance and pathophysiologic insights. The American Journal of Obstetrics and Gynecology. 2006;195(1):50–55. doi: 10.1016/j.ajog.2005.12.046. [DOI] [PubMed] [Google Scholar]
- 40.Talley N. J., Jones M., Nuyts G., Dubois D. Risk factors for chronic constipation based on a general practice sample. The American Journal of Gastroenterology. 2003;98(5):1107–1111. doi: 10.1111/j.1572-0241.2003.07465.x. [DOI] [PubMed] [Google Scholar]
- 41.O'Keefe E. A., Talley N. J., Zinsmeister A. R., Jacobsen S. J. Bowel disorders impair functional status and quality of life in the elderly: a population-based study. Journals of Gerontology—Series A Biological Sciences and Medical Sciences. 1995;50(4):M184–M189. doi: 10.1093/gerona/50a.4.m184. [DOI] [PubMed] [Google Scholar]
- 42.Belsey J., Greenfield S., Candy D., Geraint M. Systematic review: impact of constipation on quality of life in adults and children. Alimentary Pharmacology and Therapeutics. 2010;31(9):938–949. doi: 10.1111/j.1365-2036.2010.04273.x. [DOI] [PubMed] [Google Scholar]
- 43.Gallagher P., O'Mahony D. Constipation in old age. Best practice and research: clinical gastroenterology. 2009;23(6):875–887. doi: 10.1016/j.bpg.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 44.Hosia-Randell H., Suominen M., Muurinen S., Pitkälä K. H. Use of laxatives among older nursing home residents in Helsinki, Finland. Drugs and Aging. 2007;24(2):147–154. doi: 10.2165/00002512-200724020-00006. [DOI] [PubMed] [Google Scholar]
- 45.van Dijk K. N., de Vries C. S., van Den Berg P. B., Dijkema A. M., Brouwers J. R. B. J., de Jong-van Den Berg L. T. W. Constipation as an adverse effect of drug use in nursing home patients: an overestimated risk. British Journal of Clinical Pharmacology. 1998;46(3):255–261. doi: 10.1046/j.1365-2125.1998.00777.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rao S. S. C., Go J. T. Update on the management of constipation in the elderly: new treatment options. Clinical interventions in aging. 2010;5:163–171. doi: 10.2147/cia.s8100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Talley N. J., Fleming K. C., Evans J. M., O'Keefe E. A., Weaver A. L., Zinsmeister A. R., Melton L. J., III Constipation in an elderly community: a study of prevalence and potential risk factors. The American Journal of Gastroenterology. 1996;91(1):19–25. [PubMed] [Google Scholar]
- 48.Wolfsen C. R., Barker J. C., Mitteness L. S. Constipation in the daily lives of frail elderly people. Archives of Family Medicine. 1993;2(8):853–858. doi: 10.1001/archfami.2.8.853. [DOI] [PubMed] [Google Scholar]
- 49.Locke G. R., Locke G. R., III, Pemberton J. H., Phillips S. F. Aga technical review on constipation. Gastroenterology. 2000;119(6):1766–1778. doi: 10.1053/gast.2000.20392. [DOI] [PubMed] [Google Scholar]
- 50.Gurwitz J. H., Field T. S., Judge J., Rochon P., Harrold L. R., Cadoret C., Lee M., White K., LaPrino J., Erramuspe-Mainard J., DeFlorio M., Gavendo L., Auger J., Bates D. W. The incidence of adverse drug events in two large academic long-term care facilities. The American Journal of Medicine. 2005;118(3):251–258. doi: 10.1016/j.amjmed.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 51.Milton J. C., Hill-Smith I., Jackson S. H. D. Prescribing for older people. British Medical Journal. 2008;336(7644):606–609. doi: 10.1136/bmj.39503.424653.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ruths S., Straand J., Nygaard H. A. Multidisciplinary medication review in nursing home residents: What are the most significant drug-related problems? The Bergen District Nursing Home (BEDNURS) study. Quality and Safety in Health Care. 2003;12(3):176–180. doi: 10.1136/qhc.12.3.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Halvorsen K. H., Ruths S., Granas A. G., Viktil K. K. Multidisciplinary intervention to identify and resolve drug-related problems in Norwegian nursing homes. Scandinavian Journal of Primary Health Care. 2010;28(2):82–88. doi: 10.3109/02813431003765455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Doshi J. A., Shaffer T., Briesacher B. A. National estimates of medication use in nursing homes: findings from the 1997 medicare current beneficiary survey and the 1996 medical expenditure survey. Journal of the American Geriatrics Society. 2005;53(3):438–443. doi: 10.1111/j.1532-5415.2005.53161.x. [DOI] [PubMed] [Google Scholar]
- 55.McLean A. J., le Couteur D. G. Aging biology and geriatric clinical pharmacology. Pharmacological Reviews. 2004;56(2):163–184. doi: 10.1124/pr.56.2.4. [DOI] [PubMed] [Google Scholar]
- 56.Field T. S., Gurwitz J. H., Avorn J., McCormick D., Jain S., Eckler M., Benser M., Bates D. W. Risk factors for adverse drug events among nursing home residents. Archives of Internal Medicine. 2001;161(13):1629–1634. doi: 10.1001/archinte.161.13.1629. [DOI] [PubMed] [Google Scholar]
- 57.Hajjar E. R., Hanlon J. T., Artz M. B., Lindblad C. I., Pieper C. F., Sloane R. J., Ruby C. M., Schmader K. E. Adverse drug reaction risk factors in older outpatients. The American Journal Geriatric Pharmacotherapy. 2003;1(2):82–89. doi: 10.1016/S1543-5946(03)90004-3. [DOI] [PubMed] [Google Scholar]
- 58.Shakil A., Church R. J., Rao S. S. Gastrointestinal complications of diabetes. American Family Physician. 2008;77(12):1697–1702. [PubMed] [Google Scholar]
- 59.Bhowmik B., Afsana F., Diep L. M., Munir S. B., Wright E., Mahmood S., Azad Khan A. K., Hussain A. Increasing prevalence of type 2 diabetes in a rural Bangladeshi population: a population based study for 10 years. Diabetes and Metabolism Journal. 2013;37(1):46–53. doi: 10.4093/dmj.2013.37.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kessmann J. Hirschsprung's disease: diagnosis and management. American Family Physician. 2006;74(8):1319–1322. [PubMed] [Google Scholar]
- 61.Akushevich I., Kravchenko J., Ukraintseva S., Arbeev K., Yashin A. I. Time trends of incidence of age-associated diseases in the US elderly population: medicare-based analysis. Age and Ageing. 2013;42(4):494–500. doi: 10.1093/ageing/aft032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Barbosa M. T., Caramelli P., Cunningham M. C. Q., Maia D. P., Lima-Costa M. F. F., Cardoso F. Prevalence and clinical classification of tremor in elderly-A community-based survey in Brazil. Movement Disorders. 2013;28(5):640–646. doi: 10.1002/mds.25355. [DOI] [PubMed] [Google Scholar]
- 63.Arora G., Mannalithara A., Mithal A., Triadafilopoulos G., Singh G. Concurrent conditions in patients with chronic constipation: a population-based study. PLoS ONE. 2012;7(10) doi: 10.1371/journal.pone.0042910.e42910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Riss S., Weiser F. A., Schwameis K., Mittlböck M., Stift A. Haemorrhoids, constipation and faecal incontinence: is there any relationship? Colorectal Disease. 2011;13(8):e227–e233. doi: 10.1111/j.1463-1318.2011.02632.x. [DOI] [PubMed] [Google Scholar]
- 65.Yu P. L., Li Z. J., Zheng H., et al. The survey of the current status and distribution of elderly constipation in China. Chinese Journal of Geriatrics. 2001;20(2):132–134. [Google Scholar]
- 66.Ebling B., Gulić S., Jurcić D., et al. Demographic, anthropometric and socioeconomic characteristics of functional constipation in Eastern Croatia. Collegium Antropologicum. 2014;38(2):539–546. [PubMed] [Google Scholar]
- 67.Howell S., Quine S., Talley N. Low social class is linked to upper gastrointestinal symptoms in an Australian sample of urban adults. Scandinavian Journal of Gastroenterology. 2006;41(6):657–666. doi: 10.1080/00365520500442567. [DOI] [PubMed] [Google Scholar]
- 68.Shen F., Zhou H. Q., Chen G. Y., Fan J. G., Zong C. H., Wang Z. J., Zhang Y., Li D. G. An epidemiologic study on functional constipation among adult communities in Shanghai. Chinese Journal of Epidemiology. 2012;33(3):296–301. [PubMed] [Google Scholar]
- 69.Tang W., Wang Q. M., Li M. Z., et al. A community population-based epidemiologic investigation of chronic constipation in Lu'an city. Anhui Medical and Pharmaceutical Journal. 2008;12(5):426–428. [Google Scholar]
- 70.Zuo Z. K., Han J. R. Population-based epidemiological survey on constipation of Zhengzhou city. Chinese Journal of Coloproctology. 2012;32(6):50–52. [Google Scholar]
- 71.Lv N. H., Xie Y., Huang D. Q., et al. An epidemiologic investigation of chronic constipation in Nanchang city. Chinese Journal of Practical Internal Medicine. 2005;25(3):236–237. [Google Scholar]
- 72.Guo X. F., Ke M. Y., Pan G. Z., et al. Investigation of prevalence and risk factor of chronic constipation for people in Beijing. Chinese Journal of Digestion. 2002;22(10):637–638. [Google Scholar]
- 73.Xiang G. C., Long Q., Liu L. The epidemic investigation of residents with constipation in Chongqing. Chongqing Yixue. 2004;33(10):1541–1543. [Google Scholar]
- 74.Zhang H., Zhang Z. F., Lin G. Y. An epidemiologic Investigation of chronic constipation in Deyang city. Chinese Journal of Clinical Medical Research. 2008;182:60–61. [Google Scholar]
- 75.Zhang S. X., Zhang W., Fang Q. J. An epidemiologic study and Nursing measures on slow transit constipation. Journal of Qilu Nursing. 2008;14(21):114–115. [Google Scholar]
- 76.Liu Z. Y., Yang G. G., Shen Z., et al. The epidemic investigation of residents with constipation in Hangzhou. Chinese Journal of Digestion. 2004;24(7):435–436. [Google Scholar]
- 77.Zhou L., Deng L., Huang G., Guo L., Tang N., Cai W. Epidemiologic study on functional constipation in adolescents. Chinese Journal of Child Health Care. 2010;18(7):566–568. [Google Scholar]
- 78.Zhou H. Q., Li D. G., Song Y. Y., et al. Risk factors of functional constipation in adolescents in China. Journal of Clinical Pediatrics. 2008;26(2):113–115. [Google Scholar]
- 79.Wang B. X., Wang M. G., Chen J., et al. Epidemic investigation and clinical data analysis of children with functional constipation. Journal of Applied Clinical Pediatrics. 2003;18(4):253–254. [Google Scholar]
- 80.Liu Y. H., Hong M. X., Liao P. D. The epidemic investigation of children with functional constipation in Chengdu city. Modern Medicine & Health. 2007;23(5):777–778. [Google Scholar]
- 81.Hu J. J. Preliminary analysis on epidemiological characteristics of functional constipation in children. Chinese Journal of Child Health Care. 2003;11(2):127–128. [Google Scholar]
- 82.Zhang S. C., Wang W. L., Qu R. B., Su P. J., Zhang S. W., Zhang H. R., Tan S. Y., Chen X. J., Zhang W., Ai D.-B., Wu H.-T., Gong L.-C., Wang J.-L., He Y., Wan C., Dong G.-H. Epidemiologic survey on the prevalence and distribution of childhood functional constipation in the northern areas of China: a population-based study. Chinese Journal of Epidemiology. 2010;31(7):751–754. [PubMed] [Google Scholar]
- 83.Liang F., Song L. X. Epidemiologic study on constipation in 287 cases of infant. Journal of Chinese Clinical Medicine. 2003;4(8):75–76. [Google Scholar]
- 84.Liu W., Xiao L.-P., Li Y., Wang X.-Q., Xu C.-D. Epidemiology of mild gastrointestinal disorders among infants and young children in Shanghai area. Chinese Journal of Pediatrics. 2009;47(12):917–921. [PubMed] [Google Scholar]
- 85.Li Z. J., Yu P. L., Shi Q. K., et al. Epidemiologic survey on the prevalence of constipation among elderly population in Beijing. Chinese Journal of Gerontology. 2000;20(1):1–2. [Google Scholar]
- 86.Cai Y. Q., Wang H. J., Zhang X., et al. The survey of constipation and sub-health of elderly in Nanjing. Chinese Journal of Geriatrics. 2004;23(4):267–269. [Google Scholar]
- 87.Pan J. X., Shen L. Investigation of constipation in elderly population. Chinese Journal of Modern Nursing. 2008;14(7):887–889. [Google Scholar]
- 88.Guo L., Li B. Q., Liang G. X., et al. The current investigation of constipation in elderly population. Journal of Health Care and Medicine in Chinese PLA. 2004;6(1):42. [Google Scholar]
- 89.Huang X. Z., Zhang T. D. Epidemiologic survey on the prevalence of age-related diseases in rural area. Practical Preventive Medicine. 1999;6(5):344–345. [Google Scholar]