Abstract
Polyinosine-polycytidylic acid (pIC) is a synthetic dsRNA that acts as an immune agonist of TLR3 and RLR to activate dendritic and NK cells that can kill tumor cells. pIC can also trigger apoptosis in pancreatic ductal adenocarcinoma cells but its mechanism of action is obscure. In this study, we investigated the potential therapeutic activity of a formulation of pIC with polyethylenimine ([pIC]PEI) in PDAC and investigated its mechanism of action. [pIC]PEI stimulated apoptosis in PDAC cells without affecting normal pancreatic epithelial cells. Mechanistically, [pIC]PEI repressed XIAP and survivin expression and activated an immune response by inducing MDA-5, RIG-I and NOXA. Phosphorylation of AKT was inhibited by [pIC]PEI in PDAC and this event was critical for stimulating apoptosis through XIAP and survivin degradation. In vivo administration of [pIC]PEI inhibited tumor growth via AKT-mediated XIAP degradation in both subcutaneous and quasi-orthotopic-models of PDAC. Taken together, these results offer a preclinical proof-of-concept for the evaluation of [pIC]PEI as an immunochemotherapy to treat pancreatic cancer.
Keywords: [pI:C], [pIC]PEI, jetPEI, Pancreatic cancer, PDAC, AKT, XIAP
Introduction
Pancreatic cancer is one of the deadliest cancers and ranks fourth in cancer-related deaths in the US (1–4). Pancreatic cancer death rates have been increasing in the US over the past several years, as compared with the downward trend in death rates for most other major cancers (5, 6). The overall 5-year survival rate of patients with pancreatic cancer is less than 6% and this dismal prognosis has not improved in recent years resulting in an increasing number of deaths (7). The high fatality of pancreatic cancer is attributed to failure to diagnosis the disease early (before it has metastasized to other organs) and resistance to current therapies (8).
Surgical removal of pancreatic cancer can cure a small percentage of patients, but survival rates after pancreatectomy are extremely low (9). Chemotherapy or radiation employed alone or in combination, is only palliative and provides little or no benefit for patients suffering from advanced pancreatic cancer (10). The current FDA-approved cytotoxic treatment for advanced pancreatic cancer remains gemcitabine (11). Even though gemcitabine is well tolerated, its efficacy is marginal with a median survival of 6 months. The combination of 5-fluorouracil, leucovorin, irinotecan, oxaliplatin (FOLFIRINOX) showed superiority over single agent gemcitabine in patients with metastatic pancreatic cancer (from 6.8 months with gemcitabine to 11.1 months with FOLFIRINOX) (11). However, FOLFIRINOX had greater toxicity including grade 3 or 4 neutropenia, febrile neutropenia, thrombocytopenia, diarrhea, neuropathy, vomiting, and fatigue (12). Considering its aggressiveness and lack of currently effective therapies, a dire need exists for newer strategies to treat pancreatic cancer. Characterization of new activated oncogenic signaling pathways, defining molecular pathways involved in resistance and/or targeting those genes involved in these pathways in pancreatic cancer cells may lead to more effective therapeutic strategies for pancreatic cancer treatment (13–15).
The immune system plays a pivotal role in pathophysiology of pancreatitis and PDAC development (16). Eukaryotic cells contain pattern recognition receptors that detect viral/bacterial nucleic acids activating antiviral immune responses (17, 18). Toll like receptors (TLRs) function as pattern recognition receptors and primary sensors of bacteria and viruses (19). Activation of TLRs decreases expression of co-stimulatory molecules on tumor cells, immunosuppressive functions of regulatory T cells, and production of anti-proliferative cytokines (20). TLR agonists activate immune responses promoting tolerance to tumor antigens and serve as adjuvants in cancer immunotherapy clinical trials (21).
[pIC], is a synthetic dsRNA directly activating dendritic cells and triggering NK cells to kill tumor cells (22). [pIC] mimics viral RNA serving as an agonist of TLR3 and RLRs, and has been extensively used as an immune adjuvant in clinical trials (23). Although [pIC] initiates apoptosis in several cancers its mechanism of action in human PDAC is not clear. [pIC] induces high levels of type I interferons and activates several nuclear and cytoplasmic enzyme systems including OAS (oligoadenylate synthetase), the dsRNA-dependent protein kinase [PKR], RIG-I Helicase, and MDA-5 [melanoma differentiation associated gene-5] that are involved in antiviral and antitumor host defenses (19, 23). Polyethylenimine (PEI) is a promising reagent increasing transfection efficiency of nucleic acids including DNA, siRNA or RNA when administered in vivo (24). Complexing Jet-PEI with several DNA or other vectors leads to a significant increase in transfection efficiency (25). When [pIC] is co-administered with PEI as a carrier, [pIC]PEI, it profoundly affects cancer cell growth, induces apoptosis and toxic autophagy, and promotes potent immune modulating capacities (25–27). [pIC]PEI induces toxic autophagy by recruitment of Atg-5 in melanoma cells linking toxic autophagy to apoptotic caspases (25). Additionally, [pIC]PEI decreases viability through apoptosis in breast cancer cells in vitro and in vivo in tumor xenograft models through activation of mda-5 (26). The precise role of cellular intermediates and signaling pathways involved in induction of apoptosis and toxic autophagy by [pIC]PEI remains to be determined.
Our main objectives were to assess the biological and molecular effects of [pIC]PEI on human PDAC cells and to decipher the mechanism(s) involved in its antitumor activity. Cytoplasmic delivery of [pIC] using jetPEI induced pancreatic cancer-specific cell death without affecting normal pancreatic epithelial cells. We linked for the first time inhibition of AKT activation followed by XIAP degradation as prime mediators in cancer-specific cell killing by [pIC]PEI. Considering the absence of toxicity in vivo of [pIC]PEI and profound cytotoxic activity on PDAC cells, use of this reagent, alone and in combination with other therapeutic agents, could culminate in a novel, safe and effective approach for treating pancreatic cancer.
Materials and methods
Cells and reagents
Human PDAC cell lines (MIA PaCa-2, PANC-1, BxPC-3 and AsPC-1) and the hTERT-HPNE cell line were purchased from ATCC (Manassas, VA). LT-2 cell line was obtained from Millipore life sciences (Billerica, MA). ATCC authenticates these cell lines using short tandem repeat (STR) analysis. All the cell lines were expanded and frozen immediately after receipt. The cumulative culture length of the cells was fewer than 6 months after resuscitation. Early passage cells were used for all experiments and they were not re-authenticated. All the cell lines were frequently tested for mycoplasma contamination using a mycoplasma detection kit from Sigma (St. Louis, MO). Cell culture conditions and other reagents are described in supplementary methods.
Transfections with [pIC] using jetPEI
All treatments were performed using in vitro jetPEI (Polyplus transfection, New York) transfection reagent using the manufacturer’s protocol. Briefly, [pIC] was mixed with jetPEI (1:2 ratio) in 500 µL of 150 mM sodium chloride and left for 20 minutes to allow complex formation, which was then added to cells in fresh medium.
Plasmid transfection
Plasmid transfection experiments used FuGene HD transfection reagent using the manufacturer’s protocol (Roche, Indianapolis, IN) and described in supplemental methods.
Cell proliferation assays (MTT assay)
Cell growth rate was determined using a modified MTT assay as described (28).
Colony formation assays
Cells were either mock-treated or exposed to [pIC], PEI or [pIC]PEI for 48 hours. Cells were trypsinized and seeded (100 cells) in 6-well plates in triplicate. On Day 14 of incubation, cells were fixed in methanol, stained with Giemsa and colonies (>50 cells) counted. Survival fraction was defined as number of colonies divided by number of plated cells.
LC3 assay
We used a previous protocol with minor changes (29) and described in supplemental methods in detail.
Terminal deoxy nucleotidyl transferase-mediated nick labeling (TUNEL) assay
Induction of apoptosis in PDAC cells treated with [pIC]PEI as well as in xenograft tumor tissue sections of [pIC]PEI-treated mice was detected using TUNEL enzyme reagent (Roche) following the manufacturer’s instructions and as described (30). Apoptotic index (%) = 100 × (apoptotic cells/total cells).
Annexin V assay
PDAC cells were mock treated or exposed to [pIC], or PEI or [pIC]PEI for 48 hours. Cells were harvested through trypsinization, and washed twice with cold PBS, resuspended in 1 × binding buffer (100 µl) at a density of 1–10 × l05 cells per ml. Cells incubated with 5 µl of fluorescein isothiocyanate (FITC)-conjugated Annexin V and 5 µl of PI for 15 min at room temperature in the dark. The 1 × binding buffer (400 µl) was added, and the samples were analyzed by flow cytometry.
Real-Time PCR
Cells cultured in 100-mm plates were mock treated or treated with [pIC], PEI or [pIC]PEI for 48 hours. Total RNA was extracted using RNAeasy kit (Qiagen, Valencia, CA) and equal amounts of RNA were used for cDNA synthesis according to the manufacture’s protocols using SuperScript® VILO™ cDNA Synthesis Kit (Applied Biosystems, Grand Island, NY). Taqman probes for XIAP and survivin were from Applied Biosystems and quantitative real time-PCR was performed (28).
Western blotting
Western blotting analysis was performed as described (28, 30).
In vivo studies
To directly evaluate the effect of [pIC]PEI on tumor growth in vivo, we subcutaneously implanted 5 × 106 MIA PaCa-2 cells and tumors that developed received peri-tumoral injections of either [pIC], PEI or pIC complexed with invivo JetPEI on 7, 11, 15 and 21 days post tumor cell implantation. Tumor growth was monitored in mice by measuring tumor size every alternate day until completion of the experiment (sacrificed according to our IACUC protocol). After termination of the experiment tumors were fixed and sections were used for immunohistochemical analysis.
Quasi-orthotopic tumor studies
MIA PaCa-2-luc cells (5 × 106) were injected intra-peritoneally into nude mice. Bioluminescence imaging (BLI) was performed every week after tumor cell implantation. After 2-weeks of cell implantation, mice were divided into two groups with 10 mice per group. One group was used as tumor growth control, without any treatment, and the other group was injected twice weekly with [pIC]PEI (1 mg/Kg) intra-peritoneally (total of 4 doses). Control and treated mice were observed for tumor progression using BLI. All mice were sacrificed once mice either lost body weight or developed impaired mobility.
Statistical analysis
All data are presented as mean ± standard deviation (S.D.) of at least three independent experiments, each performed at least in triplicate. One-way analysis of variance (ANOVA) combined with the Tukey post hoc test of means was used for multiple comparisons. Statistical differences are presented at probability levels of p < 0.05, p < 0.01 and p < 0.001.
Results
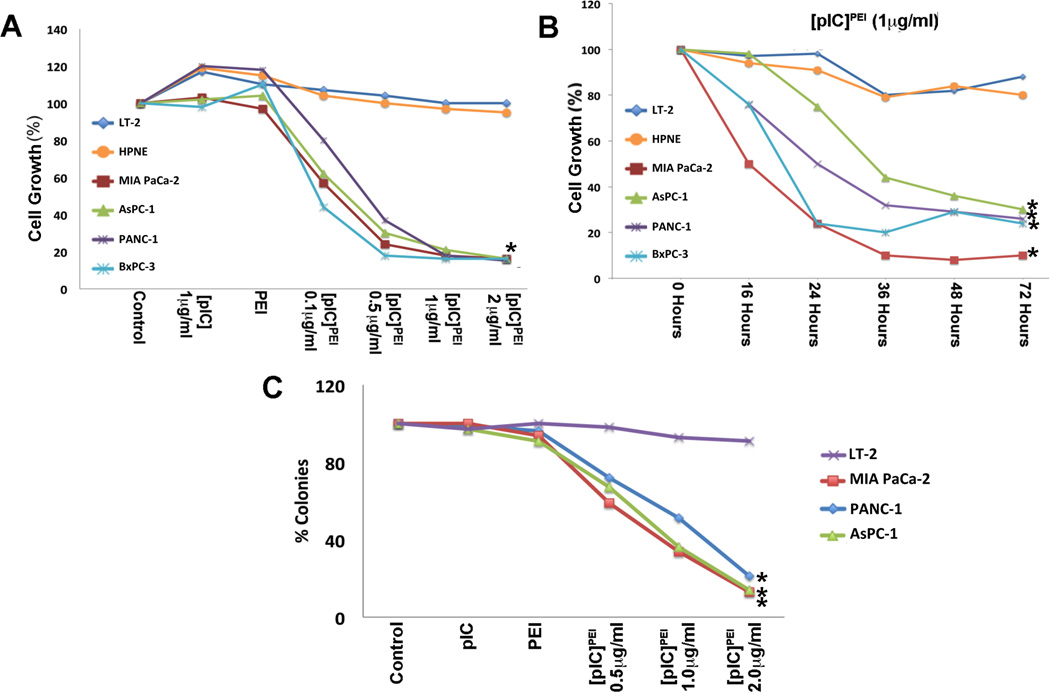
Cytosolic delivery of [pIC] using PEI selectively decreases PDAC cell growth
Cytosolic delivery of [pIC] in human melanoma, breast carcinoma and hepatoma cells in vitro and in vivo inhibits growth and induces apoptosis and toxic autophagy (25–27, 31). However, the precise mechanism(s) underlying these effects are not fully understood. The effect of [pIC]PEI on normal and PDAC cell growth was evaluated using MTT assays (Fig. 1). Treatment of PDAC cells with [pIC]PEI decreased proliferation in a dose- and time-dependent manner reaching 70–80% growth inhibition with 2 µg/ml concentration at 72 hours as compared with either control, pIC- or PEI-treated cells. In contrast, normal immortal pancreatic epithelial cells (LT-2 and hTERT-HPNE) showed minimal growth inhibition (~8% maximum reduction at 72 hours) without any change in proliferation (Figs 1A and B). Clonogenic assays evaluated [pIC]PEI treatment on long-term survival and growth of pancreatic cells. [pIC]PEI treatment decreased PDAC colony formation (both size and number) in a dose-dependent manner reaching 87%, 86% and 79% inhibition in MIA PaCa-2, AsPC-1 and PANC-1, respectively, when compared to [pIC] (~3% reduction), PEI alone (~4% reduction) or mock controls, without altering LT-2 clonogenic ability (~9% reduction) (Fig 1C).
Figure 1. [pIC]PEI treatment inhibits PDAC cell growth.
(A) Normal pancreatic epithelial and PDAC were plated in 96-well plates in quadruplicate and treated with either [pIC], PEI, or indicated doses of [pIC]PEI for 72 hours. Cell growth was measured using MTT assays, shown as percent cell growth compared with control. * p<0.01 vs [pIC] alone. (B) Cells were treated with either [pIC], PEI, or 1 µg/ml of [pIC]PEI and cell growth was quantified at the indicated time points. * p<0.01 vs 0 hours. (C) PDAC were treated as above for 24 hours, trypsinized and 200 cells/well were seeded in 6-well plates in triplicate and grown for 14 days. Colonies were fixed, stained and photographed. Data presented as percent colony formation as compared with colonies formed in the untreated controls. Results are representative of three independent experiments. * p<0.01 vs [pIC] alone.
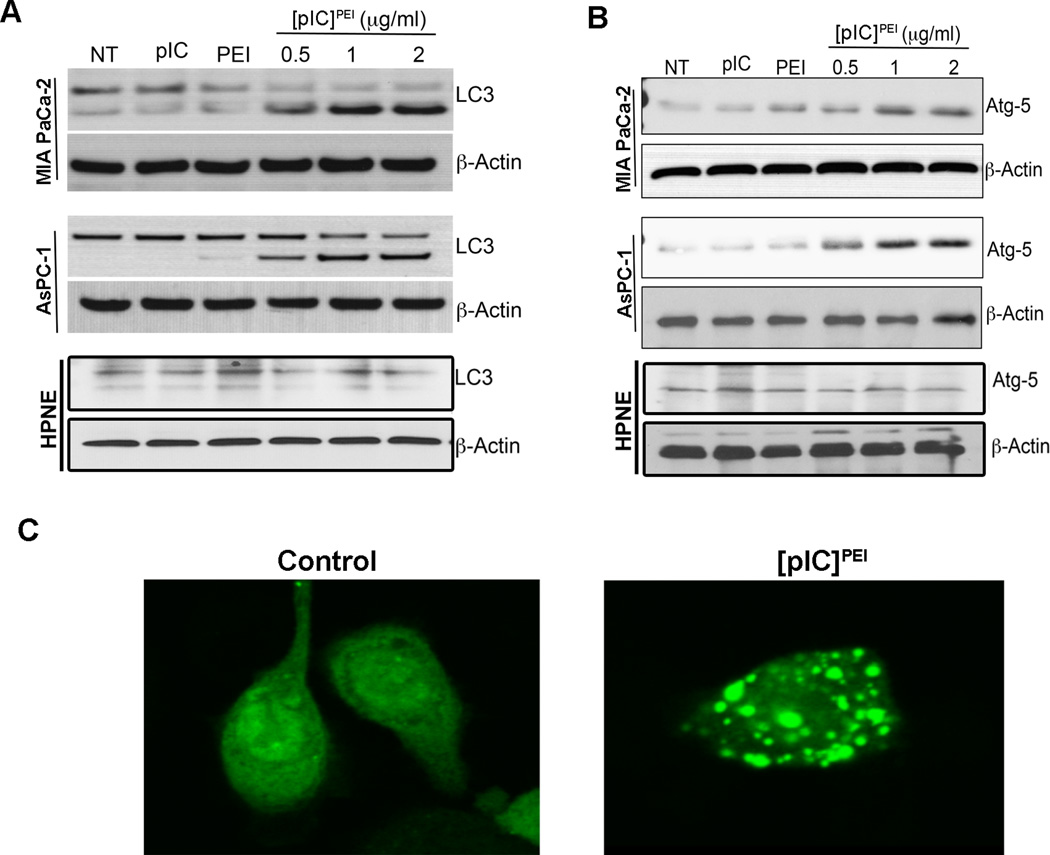
[pIC]PEI induces autophagy in PDAC cells
Previous studies demonstrated that treatment of human melanoma [25] or breast cancer [26] cells with [pIC]PEI induces autophagy. Accordingly, we initially determined whether [pIC]PEI transfection promoted autophagy in PDAC cells. PDAC and HPNE cells were treated with [pIC], PEI, or [pIC]PEI and cultured for 48 hours (Fig. 2). Cells were then collected and cell lysates were assessed for autophagy markers LC3 and Atg-5. [pIC]PEI transfection increased LC3B and Atg-5 levels in PDAC cells in a dose-dependent manner (Fig. 2A and B), while HPNE cells did not show any appreciable changes in either LC3B or Atg-5 level. To further confirm induction of autophagy, we assessed GFP-LC3 lipidation and foci formation in AsPC-1 cells following [pIC]PEI treatment. GFP-LC3 lipidation and foci formation were evident in [pIC]PEI-treated AsPC-1 cells vs. non-treated cells (Fig. 2C).
Figure 2. [pIC]PEI induces autophagy in PDAC cells.
(A, B) HPNE and PDAC cells were treated with either [pIC], PEI, or indicated doses of [pIC]PEI as in Figure 1 for 48 hours and cell lysates were subjected to Western blotting to detect (A) LC3 and (B) Atg5. β-Actin served as loading control. (C) AsPC-1 cells were treated with 1 µg/ml of [pIC]PEI for 48 hours and stained for LC3 localization. Results are representative of three independent experiments.
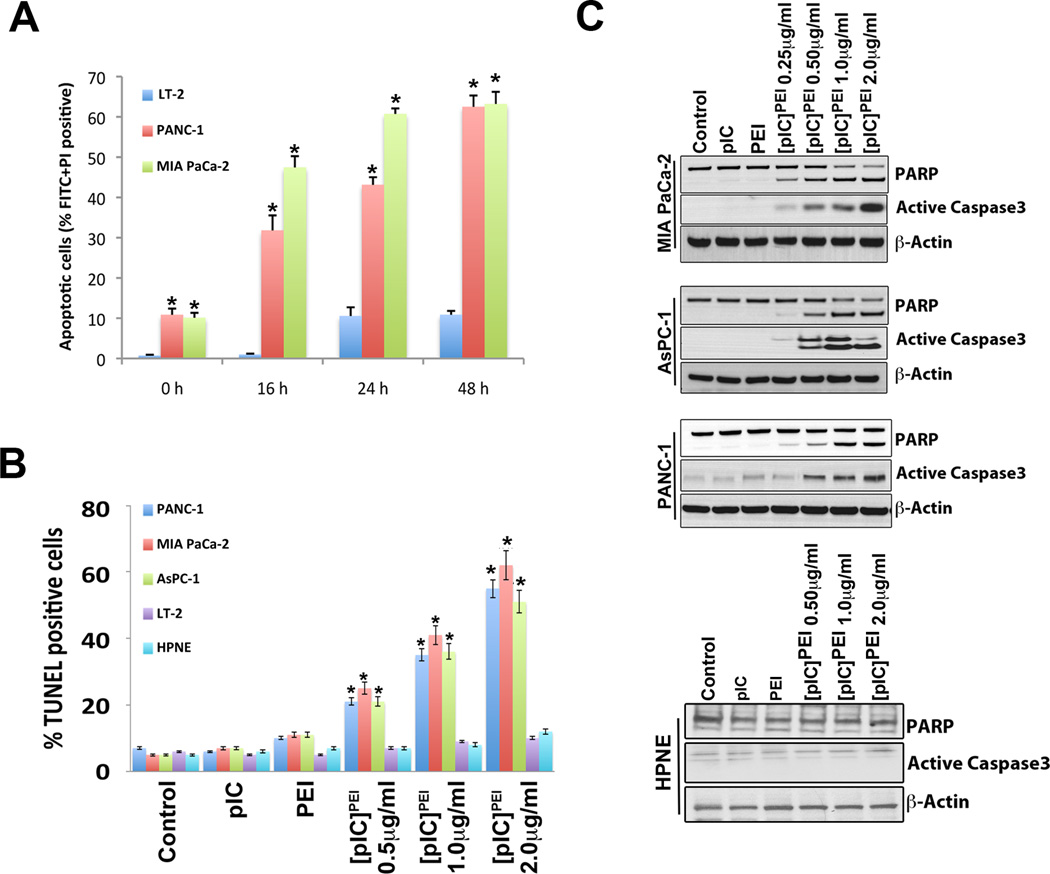
[pIC]PEI selectively induces apoptosis in PDAC cells
Flow cytometric analysis was used to determine if growth inhibition in [pIC]PEI–treated cells was a consequence of cell cycle-related events and/or apoptosis. Propidium iodide staining indicated that [pIC]PEI treatment increased Sub-G1 apoptotic cells by 56%, 42% and 52% in MIA PaCa-2, AsPC-1 and PANC-1, respectively, vs. mock controls (Supplementary Fig. 1). Annexin V and TUNEL assays corroborated these findings (Fig. 3). Flow cytometric analyses demonstrated increased Annexin V-PI positive PDAC cells (~60–70%) following [pIC]PEI treatment, indicating increased cell death (Fig 3A). Additionally, TUNEL positivity was increased in PDAC following [pIC]PEI transfection, but not in normal LT-2 and HPNE cells (Fig. 3B). Western blotting analysis revealed that [pIC]PEI treatment increased cleavage of caspase-3 and PARP in PDAC but not in normal HPNE cells (Fig. 3C). To confirm the involvement of caspases in [pIC]PEI-induced PDAC cell death we used the pan-caspase inhibitor z-VAD, which rescued PDAC from [pIC]PEI-induced cell death (Supplementary Fig 2). These studies confirm that [pIC]PEI treatment inhibits PDAC cell growth by inducing apoptosis, without inhibiting cell proliferation or inducing cell death in normal pancreatic cells.
Figure 3. [pIC]PEI induces apoptosis in PDAC cells.
(A) PDAC were treated with 0.5 µg/ml of [pIC]PEI for 16, 24, or 48 hours and stained with FITC-Annexin V and analyzed by FACS. Columns, mean of triplicate experiments; bars, SD. * p<0.01 vs 0 hours. (B) Pancreatic cancer cells were cultured in an 8-well chamber slide and treated as above for 48 hours. Cells were fixed and TUNEL assays performed. TUNEL positive cells were counted per microscopic field and data presented as percent positive cells vs. untreated control cells. * p<0.01 vs pIC alone. (C) PDAC and HPNE cells were treated as above for 48 hours and cell lysates were subjected to Western blotting for PARP and active Caspase3. β-Actin served as loading control.
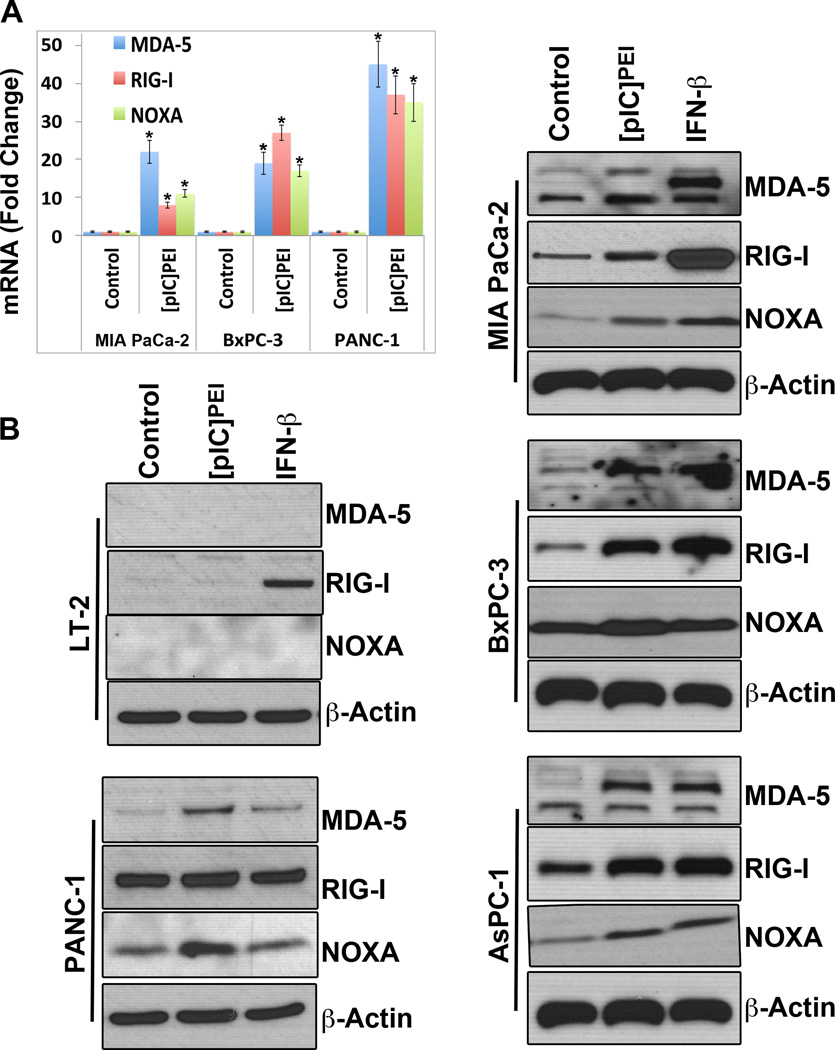
[pIC]PEI induces MDA-5, RIG-I and NOXA in PDAC cells, but not in normal pancreatic epithelial cells
[pIC]PEI induces MDA-5 and TLR-3 in melanoma cells, which was critical for induction of toxic autophagy (25). In breast cancer cells, knockdown of MDA-5 significantly restored viability after transfection with [pIC], whereas knockdown of TLR-3 did not protect cells (26). [pIC]PEI transfection in PDAC increased RIG-I, MDA-5 and NOXA as compared to mock controls (Fig. 4) with IFN-β treatment as a positive control. [pIC] or PEI did not significantly change RIG-I, MDA-5 or NOXA levels (data not shown). To confirm further that [pIC]PEI induces autophagy-mediated apoptosis in PDAC, we used the autophagy inhibitor 3MA (25). Inhibition of autophagy with 3MA rescued PDAC from [pIC]PEI-induced apoptosis (Supplementary Fig 2). The experiments with 3MA and z-VAD indicate that [pIC]PEI treatment in PDAC, but not in normal cells, induce autophagy followed by apoptotic cell death (Supplementary Fig 2).
Figure 4. [pIC]PEI induces RIG-I, MDA-5 and Noxa in PDAC cells.
(A) PDAC were treated with 1 µg/ml of [pIC]PEI for 48 hours. RNA was isolated, cDNA was synthesized using first strand cDNA synthesis kit and real time PCR was performed for MDA-5, RIG-I and NOXA. Results presented are normalized to GAPDH. Columns, mean of triplicate experiments; bars, S.D. * p<0.01 vs control. (B) Normal pancreatic epithelial and PDAC were treated with either [pIC]PEI or interferon-β for 48 hours. Cells were lysed and equal amounts of protein were resolved on SDS-PAGE. Blots were probed for MDA-5, RIG-I and NOXA. β-actin was used as loading control. Results are representative of three independent experiments.
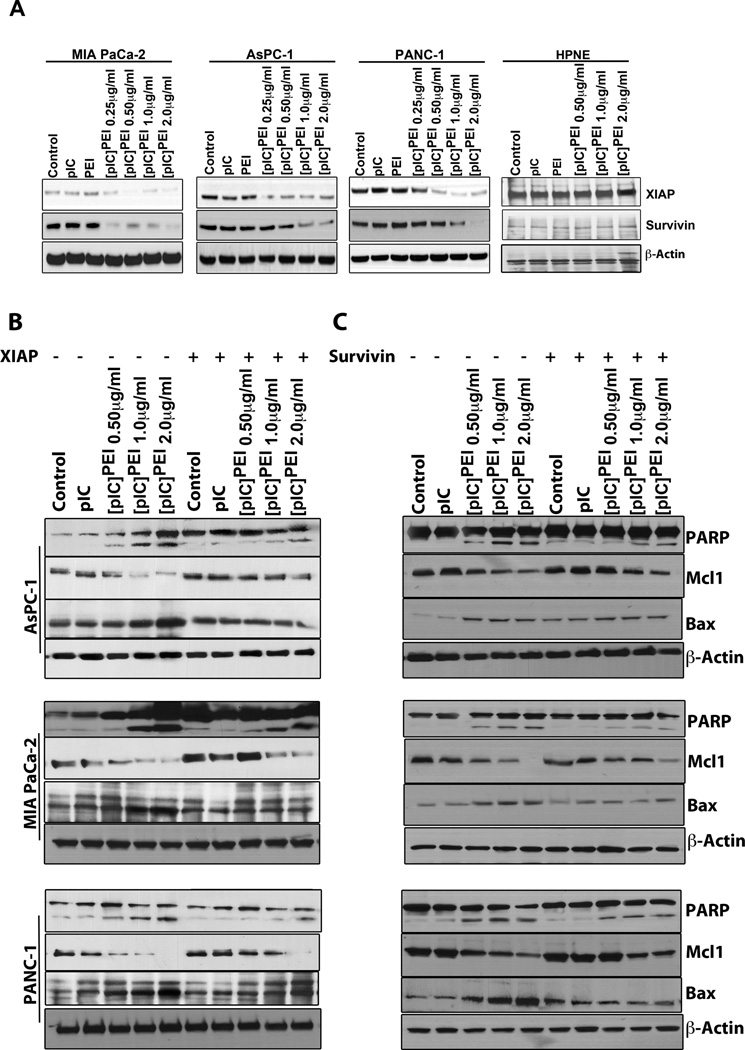
[pIC]PEI triggers X-linked inhibitor of apoptosis protein (XIAP) and survivin degradation in PDAC cells
Overexpression of the Bcl-2 family of anti-apoptotic proteins is a frequent occurrence in PDAC and serves as a barrier to effective treatment (3, 4). XIAP overexpression is frequently observed in PDAC and XIAP degradation or inhibition can sensitize PDAC to apoptosis (12). Based on these considerations, the effect of [pIC]PEI on the expressions of Bcl-2 family and other relevant anti-apoptotic proteins commonly overexpressed in PDAC, including XIAP and survivin, were determined by Western blotting. Treatment of PDAC with [pIC]PEI decreased MCL-1, survivin and XIAP levels (Fig.5A and 5B), but did not alter either XIAP or survivin in HPNE cells. Interestingly, [pIC]PEI also increased the amount of the pro-apoptotic protein, Bax (Fig. 5B).
Figure 5. [pIC]PEI triggers XIAP and survivin degradation and overexpression of XIAP or survivin partially rescues PDAC cells from [pIC]PEI-induced death.
(A) HPNE and PDAC were treated as in Figure 1A for 48 hours and cell lysates were subjected to Western blotting and probed with XIAP, survivin and β-actin antibodies. (B, C) PDAC were transiently transfected either with XIAP (B) or survivin (C) for 24 hours and treated as above for 48 hours. Cell lysates were collected and Western blotting was performed using PARP-, Mcl-1-, Bax- and β-actin-specific antibodies. Results are representative of three independent experiments.
Blocking XIAP degradation does not block apoptosis, whereas over expressing XIAP rescues [pIC]PEI-mediated apoptosis in PDAC cells
[pIC]PEI transfection in PDAC decreased XIAP protein levels, whereas RNA levels were not altered significantly, suggesting that XIAP degradation may be translationally or post-translationally regulated (Supplementary Fig. 3). To determine if XIAP degradation plays a key role in [pIC]PEI-induced apoptosis, we overexpressed XIAP in PDAC and then treated cells with different doses of [pIC]PEI. Overexpression of XIAP partially rescued PDAC from [pIC]PEI-induced cell death (Fig. 5B). However, when a proteasome inhibitor, MG132, was used to block [pIC]PEI-induced degradation of XIAP (Supplementary Fig. 4), PDAC were not rescued from [pIC]PEI-mediated apoptosis. This phenomenon was confirmed using TUNEL analysis, which shows that MG132 did not rescue PDAC cells from [pIC]PEI-induced death (Supplementary Fig. 4B). These results suggest that an additional pathway(s) may contribute to [pIC]PEI-induced cell death.
Overexpression of survivin partially rescues PDAC cells from [pIC]PEI-mediated cell death
Survivin is over-expressed in PDAC (32) and provides a biomarker for monitoring prognosis of pancreatic cancer patients. Our results demonstrate that [pIC]PEI dose-dependently inhibits survivin expression in PDAC but not in HPNE cells (Fig 5A). To explore the relevance of this molecule in [pIC]PEI-induced cell death we transiently transfected PDAC with a survivin expression plasmid and then treated with [pIC]PEI. Overexpression of Survivin in PDAC partially rescued these cells from [pIC]PEI-induced cell death (Fig. 5C, Supplementary Fig. 5B) As, XIAP and survivin play significant roles in PDAC development, we determined the effects of combined over-expression of survivin and XIAP on [pIC]PEI treatment. Combination XIAP and survivin expression greatly enhanced the rescue of PDAC following [pIC]PEI treatment (Supplemental Fig. 5C). Taken together, these results confirm that both XIAP and survivin contribute to [pIC]PEI-induced PDAC death.
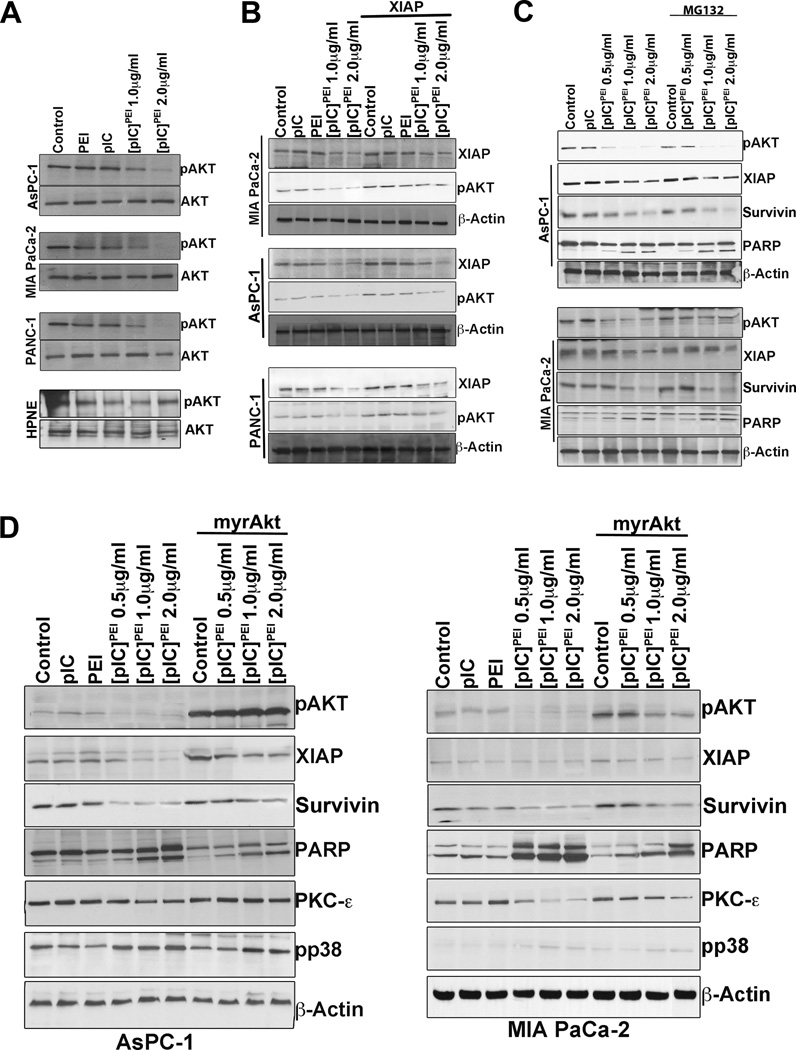
[pIC]PEI induces AKT-mediated XIAP degradation and overexpression of AKT rescues PDAC cells from [pIC]PEI-mediated cell death
Overexpression of XIAP plus survivin increases survival in [pIC]PEI-treated PDAC. Treatment with MG132 suggests that blocking XIAP-degradation alone cannot rescue cells from apoptosis. Based on these observations, we hypothesized that upstream regulators of XIAP may play an important role in [pIC]PEI-induced apoptosis. Previous reports suggest that phosphorylation of XIAP by AKT protects XIAP from ubiquitination and degradation (33). We therefore determined the levels of total AKT and its phosphorylation upon [pIC]PEI-treatment in PDAC. [pIC]PEI decreased the levels of pAKT in three pancreatic cancer cell lines (AsPC-1, MIA PaCa-2 and PANC-1) as compared with [pIC], PEI or mock controls, whereas total AKT levels were unchanged (Fig. 6A). To check the specificity of the [pIC]PEI effect on PDAC, we also determined levels of pAKT and total AKT in HPNE cells. [pIC]PEI did not alter the levels of pAKT or total AKT in HPNE cells as compared with [pIC], PEI or mock controls (Fig 6A).
Figure 6. [pIC]PEI induces AKT-mediated XIAP degradation in PDAC cells.
(A) HPNE and PDAC were either treated with [pIC] or PEI alone or with indicated doses of [pIC]PEI complex for 48 hours and cell lysates were assessed for pAKT and total AKT levels. (B) PDAC were transiently transfected with XIAP for 24 hours and then treated as in (A) for 48 hours. Cell lysates were assessed for XIAP and pAKT using specific antibodies. (C) PDAC treated as in (A) for 24 hours were treated with MG132. Western blotting was performed using pAKT-, XIAP-, survivin-, PARP- and β-actin-specific antibodies. (D) PDAC were transiently transfected with myr-AKT for 24 hours and then treated as in (A) for 48 hours. Cell lysates were assessed for pAKT, XIAP, survivin, PARP, PKC-ε, and phospho-p38 by Western blotting. β-actin served as loading control. Results are representative of three independent experiments.
To confirm that AKT is an upstream modulator of XIAP, PDAC cells were transiently transfected with an XIAP expression plasmid for 24 hours and then treated with [pIC], PEI or [pIC]PEI for an additional 48 hours. Cell lysates were prepared and subjected to Western blotting analysis for XIAP and pAKT. XIAP over-expression in PDAC partially rescued cells from [pIC]PEI-induced apoptosis (Supplementary Fig. 5A), without substantially altering pAKT levels (Fig. 6B). Similarly, when MG132 blocked [pIC]PEI-induced XIAP degradation, pAKT levels remained unchanged (Fig. 6C). To confirm further a role of AKT in [pIC]PEI-induced PDAC death, cells were transiently transfected with a myr-AKT for 24 hours and then treated with [pIC], PEI or [pIC]PEI for an additional 48 hours. Cells were collected, lysates prepared and Western blotting was performed to monitor levels of pAKT, XIAP, survivin, and PARP cleavage. AKT overexpression in the PDAC increased the levels of pAKT, survivin, and XIAP, and rescued cells from [pIC]PEI-induced cell death (Fig. 6D). TUNEL assay confirmed that AKT over-expression significantly rescued PDAC cells from [pIC]PEI-induced cell death (Supplementary Fig 6). Taken together, these results elucidate the downstream pathways by which [pIC]PEI promotes cell death selectively in PDAC, but not in normal pancreatic epithelial cells, demonstrating that AKT serves as an upstream regulator of XIAP in mediating [pIC]PEI anticancer activity.
[pIC]PEI mediates mTOR-PKC-ε-mediated AKT regulation in PDAC cells
Previous studies show that mTOR can regulate AKT in several cancers (34). AKT has also been reported to be a downstream effector of PKC-ε in ethanol-induced cardioprotection, and inhibition of PKC-ε prevented the increase in AKT activity (35). To define the effects of [pIC]PEI on mTOR-PKC-ε link, we performed western blotting analysis for mTOR and PKC-ε. [pIC]PEI transfection in PDAC decreased mTOR protein levels and mTOR activation in a dose-dependent manner (Supplementary Fig 7). We also showed that [pIC]PEI treatment of PDAC decreased PKC-ε in a dose-dependent manner (Figure 6 and Supplementary Fig 7). Our results emphasize that PKC-ε and AKT act in a positive feed back loop, since AKT overexpression led to an increase in PKC-ε in PDAC cells (Figure 6D). These results suggest a potential role of mTOR-PKC-ε in regulating AKT following [pIC]PEI treatment, which warrant further future investigation.
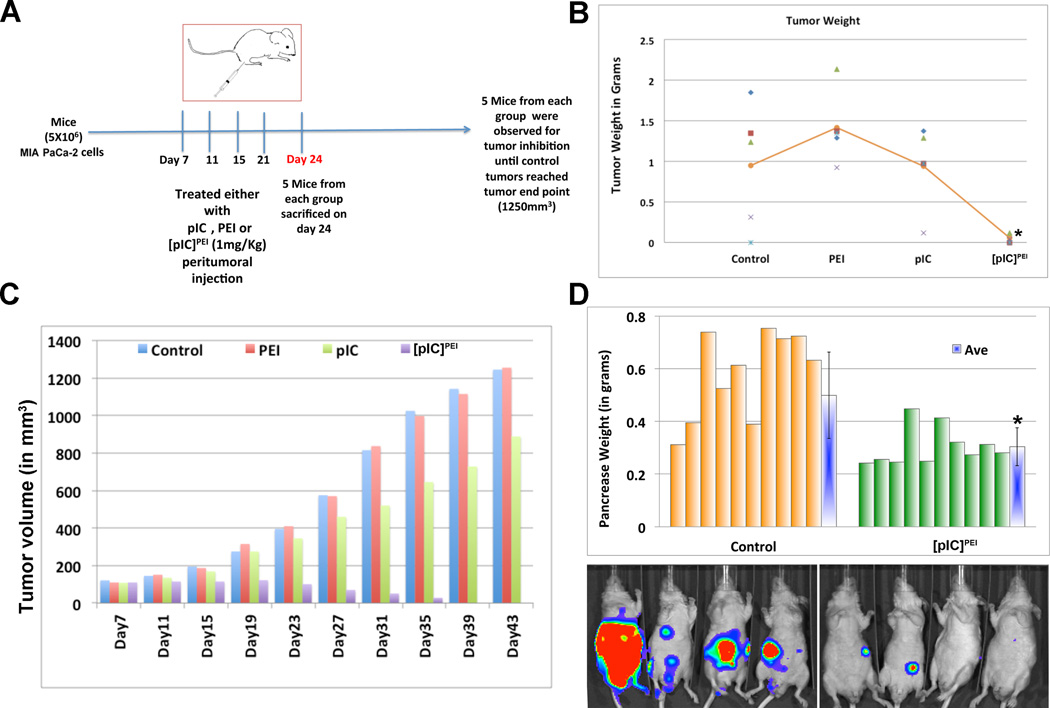
In vivo delivery of [pIC] using in vivo jetPEI decreases human pancreatic tumor growth in subcutaneous and quasi-orthotopic xenograft mouse models
MIA PaCa-2 (5 × 106) cells were subcutaneously injected into male nude mice and when the tumor reached ~75 mm3, they were mock treated (PBS, Control) or treated with [pIC], PEI or [pIC]PEI peri-tumorally and tumor growth was monitored. A significant decrease in tumor volume and tumor mass was evident in mice receiving [pIC]PEI as compared to mock-treated (PBS) control mice or mice treated with [pIC] or PEI. Analysis of tumor mass and volume showed ~90% inhibition in tumor growth in [pIC]PEI-treated animals (Fig. 7B and C). To determine whether [pIC]PEI also induced AKT- and XIAP-mediated apoptosis in vivo, tumor sections were prepared and immunohistochemistry (IHC) was performed. IHC confirmed downregulation of XIAP and survivin in [pIC]PEI-treated tumor sections when compared to [pIC] or PEI alone or in control PBS-treated tumor sections (Supplementary Fig. 8). TUNEL analysis for apoptosis in tumors confirmed enhanced TUNEL-positivity in the [pIC]PEI-treated tumor sections (Supplementary Fig. 8). Taken together, these results show that [pIC]PEI treatment in vivo inhibits PDAC tumor growth through increased apoptosis as evidenced by increased TUNEL and cleaved Caspase-3 staining and this effect is mediated through the AKT-XIAP pathway.
Figure 7. In vivo cytoplasmic delivery of [pIC] using invivo jetPEI decreases human pancreatic tumor growth in subcutaneous and quasi-orthotopic models.
(A) Mice were injected subcutaneously with MIA PaCa-2 cells (5 × 106) and once tumors reached ~75 mm3 they were divided into 4 groups. Each group was treated with 4 doses of [pIC], PEI or [pIC]PEI (1 mg/kg) as indicated in the schematic. One set of mice (5 mice from each group) were sacrificed 3 days after the last dose of [pIC]PEI. The other group was continued until the control tumors reached the IACUC end point (1250 mm3). (B) Tumor weights were measured and presented graphically. Mean of the tumor weights of each group of mice was shown in line graph. * p<0.01 vs Control. (C) Tumor volumes were measured periodically using a vernier caliper and presented graphically. (D) MIA PaCa-2-luc cells (5 × 106) were injected intra-peritoneally into nude mice. BLI was performed every week after tumor cell implantation. After 2 weeks following cell implantation, mice were divided into two groups of 10 mice each. One group was used as control, without treatment, and the other group was injected twice weekly with [pIC]PEI (1mg/Kg) intra-peritoneally (total 4 doses). Control and treated mice were observed for tumor progression using BLI. Once the mice were sacrificed, the pancreas was weighed and data presented graphically. * p<0.01 vs Control.
To confirm further that [pIC]PEI could inhibit growth of human PDAC in vivo we used a quasi-orthotopic model in which 5 × 106 MIA PaCa-2-luc cells were injected intra-peritoneally (IP) into nude mice (Fig. 7D). After 2 weeks, mice received [pIC]PEI IP and BLI monitored tumor growth. Mice were sacrificed once control tumors reached the termination point, as indicated by compromised health. The total pancreatic region with tumors for each mouse was collected and weighted (Fig. 7D). The pancreas in control group mice with tumors weighted ~0.5 grams, whereas the [pIC]PEI-treated animals’ pancreas weighted ~0.3 grams (Fig. 7D). BLI also showed high luminescence in control mice compared to [pIC]PEI-treated animals (Fig. 7D). Taken together, these results demonstrate that [pIC]PEI treatment significantly reduced tumor burden in a quasi-orthotopic pancreatic tumor model.
Discussion
Pancreatic cancer remains one of the most difficult cancers to treat effectively. Rapid progression of the disease and diagnosis only after the primary tumor has metastasized are factors contributing to the failure of current approaches to mitigate this disease. Moreover, the lack of noteworthy benefits of current treatment modalities highlights the need for innovative approaches to combat this invariably lethal neoplasm. We presently demonstrate that delivery of [pIC] into the cytosol using PEI selectively promotes PDAC apoptosis without affecting normal pancreatic epithelial cells. This effect is observed both in cells in culture and in two in vivo pancreatic cancer xenograft models, involving subcutaneous tumor injection and quasi-orthotopic intraperitoneal delivery of human PDAC. Additionally, through a series of hypothesis-based experiments we define the mechanism of this selective activity of [pIC]PEI, which involves AKT-mediated XIAP degradation resulting in apoptosis and toxic autophagy uniquely in PDAC.
Ideally, optimum anticancer therapies should not alter the immunological status of cancer patients, but instead should boost immune system responses since immunological status significantly impacts on therapeutic outcome of cancer patients (26). [pIC] has been used for decades as a synthetic dsRNA mimic to enhance the immune system in an IFN-dependent manner (25) and was tested in multiple clinical cancer therapy trials. However, clinical trials with naked [pIC] were not promising in melanoma because of poor stability of [pIC] and IFN induction (25). [pIC] complexed with low molecular weight poly-L-lysine, carboxymethylcellulose, liposomes, or PEI increased therapeutic activity via IFN-dependent immune responses (25, 27). [pIC] activates professional antigen-presenting cells, such as dendritic cells that secrete type-I IFN, resulting in effective activation of NK cells (25). Interestingly, [pIC]PEI also displayed efficient anti-tumor activity in animals with defective NK, T, or B cell signaling (25, 26).
[pIC] induces death in a panel of human cancer cell lines, however, it is only in the last few years that receptors for pIC recognition (MDA-5, TLR3 and PKR) have been discovered (27). Transfection of [pIC] into human melanoma cells induced cell death through the cytosolic [pIC] receptor, MDA-5 (25). When [pIC] was delivered into the cytosol by PEI endogenous MDA-5 was induced which facilitated killing of melanoma cells by activation of NOXA. However, when MDA-5 or NOXA was depleted it did not abrogate cell death completely following [pIC]PEI treatment suggesting the involvement of additional death mechanism(s). [pIC] induced an IFN-independent pro-apoptotic signaling pathway that was activated by RIG-I and MDA-5 in normal cells as well as in melanoma cells, which led to apoptosis only in melanoma cells (27). Interestingly, primary cells were less susceptible due to an intact Bcl-xL pathway, resulting in preferential tumor cell death in vitro and in vivo in immune deficient mice. In hepatoma cells, [pIC]-liposomes induced caspase-dependent apoptosis and up-regulated RIG-I and MDA-5 (31). Transfection of [pIC] into breast cancer cells resulted in growth inhibition and apoptosis by inducing MDA-5 and TLR3 and selective knockdown of MDA-5, but not TLR3, partially protected cells from the [pIC]. We show that [pIC]PEI transfection selectively inhibits cell growth and induces apoptosis in PDAC without affecting normal pancreatic epithelial cells. Moreover, [pIC]PEI transfection in PDAC increased RIG-I, MDA-5 and NOXA both at the mRNA and protein level, which is consistent with recent reports (25,27,31). Apoptosis induction in PDAC is caspase-dependent since using a pan-caspase inhibitor z-VAD, rescued PDAC from [pIC]PEI-induced cell death. In line with the previous reports, we also found that [pIC]PEI induced autophagy in PDAC as evidenced by LC3 cleavage and Atg5 induction. Inhibition of autophagy by treatment with 3-MA in PDAC reduced [pIC]PEI –mediated apoptosis.
IAP’s are deregulated in PDAC and contribute to therapy-resistance (36, 37). XIAP and survivin are two essential members of the IAP family, which are overexpressed in numerous human malignancies including PDAC and predict poor prognosis (38–43). Interestingly, [pIC]PEI treatment in PDAC degraded survivin and XIAP in a dose-dependent manner. Overexpression of survivin or XIAP individually in PDAC resulted in partial resistance to [pIC]PEI treatment, whereas overexpression in combination provided greater resistance to [pIC]PEI. Although XIAP degradation contributes to [pIC]PEI-induced PDAC death, rescue of XIAP degradation by MG132 did not provide resistance to apoptosis. AKT can phosphorylate XIAP at serine 87 in vitro and in vivo and can also interact with XIAP (33). The XIAP phosphorylation at serine 87 by AKT inhibits its autoubiquitination and ubiquitination functions promoting resistance to cisplatin-induced XIAP degradation, caspase-3 activation, and apoptosis (33, 44, 45). AKT, also known as protein kinase B, is a serine/threonine kinase involved in regulation of cell proliferation, survival/apoptosis, angiogenesis, metabolism, and protein synthesis (46). AKT plays a seminal role in various cancers (47–53). [pIC]PEI treatment of PDAC decreased activation of AKT in a dose-dependent manner. A myristoylated, constitutively active form of Akt (myr-Akt) rescued PDAC from XIAP degradation and [pIC]PEI-induced apoptosis, whereas XIAP overexpression failed to rescue inhibition of AKT phosphorylation by [pIC]PEI. Taken together, these studies suggest that AKT functions upstream of XIAP and regulates degradation of XIAP resulting in cell death. Interestingly, we found that [pIC]PEI treatment dramatically decreases mTOR phosphorylation in PDAC in a dose-dependent manner. Moreover, we found that [pIC]PEI treatment of PDAC decreased PKC-ε, which was shown previously to act in a positive feedback loop with AKT (35). We plan to extend this interesting observation in future studies.
In summary, we demonstrate that cytosolic delivery of [pIC] using PEI in PDAC results in AKT-XIAP-mediated apoptosis in vitro and in vivo. [pIC]PEI displayed strong antitumor activity in immunodeficient mice, using both human pancreatic tumor xenograft and quasi-orthotopic models, demonstrating that an intact immune system is not mandatory for anticancer activity, supporting previous studies in melanoma (25, 27) and breast cancer (26). Apoptosis is sequentially triggered by inhibition of AKT activation followed by XIAP degradation in [pIC]PEI-treated PDAC. This conclusion is supported by the observations that AKT modulation regulated XIAP expression, but XIAP alteration did not affect AKT expression. Our in vivo and in vitro experimental data suggest that, [pIC]PEI may provide a clinically relevant treatment strategy for aggressive and invariably fatal pancreatic cancer.
Supplementary Material
Acknowledgements
The present study was supported in part by NIH, NCI Grant 1R01 CA127641, VCU MCC Developmental Funds (P.B.F.) and a VCU MCC Pilot Project (L.E., S.R.G., P.B.F.). D.S. is a Harrison Scholar in the VCU MCC. P.B.F. holds the Thelma Newmeyer Corman Chair in Cancer Research in the VCU MCC. We thank Dr. Richard A. Roth (Department of Molecular Pharmacology, Stanford University School of Medicine, Stanford, CA) for providing plasmid myr-AKT delta4–129. We thank Dr. Paola M. Barral for assistance with Western blotting.
Footnotes
Conflict of Interest: There are no conflicts of interest for any of the authors on this paper.
References
- 1.Sarkar S, Azab B, Quinn BA, Shen X, Dent P, Klibanov AL, et al. Chemoprevention gene therapy (CGT) of pancreatic cancer using perillyl alcohol and a novel chimeric serotype cancer terminator virus. Curr Mol Med. 2014;14:125–140. doi: 10.2174/1566524013666131118110827. [DOI] [PubMed] [Google Scholar]
- 2.Sarkar S, Azab BM, Das SK, Quinn BA, Shen X, Dash R, et al. Chemoprevention gene therapy (CGT): novel combinatorial approach for preventing and treating pancreatic cancer. Curr Mol Med. 2013;13:1140–1159. doi: 10.2174/1566524011313070008. [DOI] [PubMed] [Google Scholar]
- 3.Lebedeva IV, Su ZZ, Vozhilla N, Chatman L, Sarkar D, Dent P, et al. Mechanism of in vitro pancreatic cancer cell growth inhibition by melanoma differentiation-associated gene-7/interleukin-24 and perillyl alcohol. Cancer Res. 2008;68:7439–7447. doi: 10.1158/0008-5472.CAN-08-0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lebedeva IV, Su ZZ, Vozhilla N, Chatman L, Sarkar D, Dent P, et al. Chemoprevention by perillyl alcohol coupled with viral gene therapy reduces pancreatic cancer pathogenesis. Mol Cancer Ther. 2008;7:2042–2050. doi: 10.1158/1535-7163.MCT-08-0245. [DOI] [PubMed] [Google Scholar]
- 5.Al Haddad AH, Adrian TE. Challenges and future directions in therapeutics for pancreatic ductal adenocarcinoma. Expert Opin Investig Drugs. 2014:1–17. doi: 10.1517/13543784.2014.933206. [DOI] [PubMed] [Google Scholar]
- 6.Ma J, Siegel R, Jemal A. Pancreatic cancer death rates by race among US men and women, 1970–2009. J Natl Cancer Inst. 2013;105:1694–1700. doi: 10.1093/jnci/djt292. [DOI] [PubMed] [Google Scholar]
- 7.Shankar S, Marsh L, Srivastava RK. EGCG inhibits growth of human pancreatic tumors orthotopically implanted in Balb C nude mice through modulation of FKHRL1/FOXO3a and neuropilin. Mol Cell Biochem. 2013;372:83–94. doi: 10.1007/s11010-012-1448-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoos WA, James PM, Rahib L, Talley AW, Fleshman JM, Matrisian LM. Pancreatic cancer clinical trials and accrual in the United States. J Clin Oncol. 2013;31:3432–3438. doi: 10.1200/JCO.2013.49.4823. [DOI] [PubMed] [Google Scholar]
- 9.Petzel MQ, Parker NH, Valentine AD, Simard S, Nogueras-Gonzalez GM, Lee JE, et al. Fear of cancer recurrence after curative pancreatectomy: a cross-sectional study in survivors of pancreatic and periampullary tumors. Ann Surg Oncol. 2012;19:4078–4084. doi: 10.1245/s10434-012-2566-1. [DOI] [PubMed] [Google Scholar]
- 10.Roeder F, Timke C, Uhl M, Habl G, Hensley FW, Buechler MW, et al. Aggressive local treatment containing intraoperative radiation therapy (IORT) for patients with isolated local recurrences of pancreatic cancer: a retrospective analysis. BMC Cancer. 2012;12:295. doi: 10.1186/1471-2407-12-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saif MW. Advancements in the management of pancreatic cancer: 2013. JOP. 2013;14:112–118. doi: 10.6092/1590-8577/1481. [DOI] [PubMed] [Google Scholar]
- 12.Paulson AS, Tran Cao HS, Tempero MA, Lowy AM. Therapeutic advances in pancreatic cancer. Gastroenterology. 2013;144:1316–1326. doi: 10.1053/j.gastro.2013.01.078. [DOI] [PubMed] [Google Scholar]
- 13.Alexandrov LB, Nik-Zainal S, Wedge DC, Aparicio SA, Behjati S, Biankin AV, et al. Signatures of mutational processes in human cancer. Nature. 2013;500:415–421. doi: 10.1038/nature12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Biankin AV, Waddell N, Kassahn KS, Gingras MC, Muthuswamy LB, Johns AL, et al. Pancreatic cancer genomes reveal aberrations in axon guidance pathway genes. Nature. 2012;491:399–405. doi: 10.1038/nature11547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eser S, Reiff N, Messer M, Seidler B, Gottschalk K, Dobler M, et al. Selective requirement of PI3K/PDK1 signaling for Kras oncogene-driven pancreatic cell plasticity and cancer. Cancer Cell. 2013;23:406–420. doi: 10.1016/j.ccr.2013.01.023. [DOI] [PubMed] [Google Scholar]
- 16.Zheng L, Xue J, Jaffee EM, Habtezion A. Role of immune cells and immune-based therapies in pancreatitis and pancreatic ductal adenocarcinoma. Gastroenterology. 2013;144:1230–1240. doi: 10.1053/j.gastro.2012.12.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kane M, Case LK, Wang C, Yurkovetskiy L, Dikiy S, Golovkina TV. Innate immune sensing of retroviral infection via Toll-like receptor 7 occurs upon viral entry. Immunity. 2011;35:135–145. doi: 10.1016/j.immuni.2011.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kang DC, Gopalkrishnan RV, Wu Q, Jankowsky E, Pyle AM, Fisher PB. mda-5: An interferon-inducible putative RNA helicase with double-stranded RNA-dependent ATPase activity and melanoma growth-suppressive properties. Proc Natl Acad Sci U S A. 2002;99:637–642. doi: 10.1073/pnas.022637199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barral PM, Sarkar D, Su ZZ, Barber GN, DeSalle R, Racaniello VR, et al. Functions of the cytoplasmic RNA sensors RIG-I and MDA-5: key regulators of innate immunity. Pharmacol Ther. 2009;124:219–234. doi: 10.1016/j.pharmthera.2009.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu G, Zhang L, Zhao Y. Modulation of immune responses through direct activation of Toll-like receptors to T cells. Clin Exp Immunol. 2010;160:168–175. doi: 10.1111/j.1365-2249.2010.04091.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Adams S. Toll-like receptor agonists in cancer therapy. Immunotherapy. 2009;1:949–964. doi: 10.2217/imt.09.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perrot I, Deauvieau F, Massacrier C, Hughes N, Garrone P, Durand I, et al. TLR3 and Rig-like receptor on myeloid dendritic cells and Rig-like receptor on human NK cells are both mandatory for production of IFN-gamma in response to double-stranded RNA. J Immunol. 2010;185:2080–2088. doi: 10.4049/jimmunol.1000532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gnjatic S, Sawhney NB, Bhardwaj N. Toll-like receptor agonists: are they good adjuvants? Cancer J. 2010;16:382–391. doi: 10.1097/PPO.0b013e3181eaca65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bhang HE, Gabrielson KL, Laterra J, Fisher PB, Pomper MG. Tumor-specific imaging through progression elevated gene-3 promoter-driven gene expression. Nat Med. 2011;17:123–129. doi: 10.1038/nm.2269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tormo D, Checinska A, Alonso-Curbelo D, Perez-Guijarro E, Canon E, Riveiro-Falkenbach E, et al. Targeted activation of innate immunity for therapeutic induction of autophagy and apoptosis in melanoma cells. Cancer Cell. 2009;16:103–114. doi: 10.1016/j.ccr.2009.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Inao T, Harashima N, Monma H, Okano S, Itakura M, Tanaka T, et al. Antitumor effects of cytoplasmic delivery of an innate adjuvant receptor ligand, poly(I:C), on human breast cancer. Breast Cancer Res Treat. 2012;134:89–100. doi: 10.1007/s10549-011-1930-3. [DOI] [PubMed] [Google Scholar]
- 27.Besch R, Poeck H, Hohenauer T, Senft D, Hacker G, Berking C, et al. Proapoptotic signaling induced by RIG-I and MDA-5 results in type I interferon-independent apoptosis in human melanoma cells. J Clin Invest. 2009;119:2399–2411. doi: 10.1172/JCI37155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dash R, Richards JE, Su ZZ, Bhutia SK, Azab B, Rahmani M, et al. Mechanism by which Mcl-1 regulates cancer-specific apoptosis triggered by mda-7/IL-24, an IL-10-related cytokine. Cancer Res. 2010;70:5034–5045. doi: 10.1158/0008-5472.CAN-10-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee JW, Kim KS, An HK, Kim CH, Moon HI, Lee YC. Dendropanoxide Induces Autophagy through ERK1/2 Activation in MG-63 Human Osteosarcoma Cells and Autophagy Inhibition Enhances Dendropanoxide-Induced Apoptosis. PLoS One. 2013;8:e83611. doi: 10.1371/journal.pone.0083611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bhoopathi P, Chetty C, Kunigal S, Vanamala SK, Rao JS, Lakka SS. Blockade of tumor growth due to matrix metalloproteinase-9 inhibition is mediated by sequential activation of beta1-integrin, ERK, and NF-kappaB. J Biol Chem. 2008;283:1545–1552. doi: 10.1074/jbc.M707931200. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 31.Peng S, Geng J, Sun R, Tian Z, Wei H. Polyinosinic-polycytidylic acid liposome induces human hepatoma cells apoptosis which correlates to the up-regulation of RIG-I like receptors. Cancer Sci. 2009;100:529–536. doi: 10.1111/j.1349-7006.2008.01062.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Qiao JG, Zhang YQ, Yin YC, Tan Z. Expression of Survivin in pancreatic cancer and its correlation to expression of Bcl-2. World J Gastroenterol. 2004;10:2759–2761. doi: 10.3748/wjg.v10.i18.2759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dan HC, Sun M, Kaneko S, Feldman RI, Nicosia SV, Wang HG, et al. Akt phosphorylation and stabilization of X-linked inhibitor of apoptosis protein (XIAP) J Biol Chem. 2004;279:5405–5412. doi: 10.1074/jbc.M312044200. [DOI] [PubMed] [Google Scholar]
- 34.Moschella PC, McKillop J, Pleasant DL, Harston RK, Balasubramanian S, Kuppuswamy D. mTOR complex 2 mediates Akt phosphorylation that requires PKCepsilon in adult cardiac muscle cells. Cell Signal. 2013;25:1904–1912. doi: 10.1016/j.cellsig.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Basu A, Sivaprasad U. Protein kinase Cepsilon makes the life and death decision. Cell Signal. 2007;19:1633–1642. doi: 10.1016/j.cellsig.2007.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lopes RB, Gangeswaran R, McNeish IA, Wang Y, Lemoine NR. Expression of the IAP protein family is dysregulated in pancreatic cancer cells and is important for resistance to chemotherapy. Int J Cancer. 2007;120:2344–2352. doi: 10.1002/ijc.22554. [DOI] [PubMed] [Google Scholar]
- 37.Jiang C, Tan T, Yi XP, Shen H, Li YX. Lentivirus-mediated shRNA targeting XIAP and survivin inhibit SW1990 pancreatic cancer cell proliferation in vitro and in vivo. Mol Med Rep. 2011;4:667–674. doi: 10.3892/mmr.2011.472. [DOI] [PubMed] [Google Scholar]
- 38.Li Y, Jian Z, Xia K, Li X, Lv X, Pei H, et al. XIAP is related to the chemoresistance and inhibited its expression by RNA interference sensitize pancreatic carcinoma cells to chemotherapeutics. Pancreas. 2006;32:288–296. doi: 10.1097/01.mpa.0000218314.67111.fb. [DOI] [PubMed] [Google Scholar]
- 39.Trauzold A, Schmiedel S, Roder C, Tams C, Christgen M, Oestern S, et al. Multiple and synergistic deregulations of apoptosis-controlling genes in pancreatic carcinoma cells. Br J Cancer. 2003;89:1714–1721. doi: 10.1038/sj.bjc.6601330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yang J, Ouyang J, Ouyang L, Ouyang L, Chen Y. Inhibition of cell proliferation and increase of chemosensitivity by simultaneous knockdown of XIAP and survivin in pancreatic carcinoma cells. Oncol Res. 2013;21:43–50. doi: 10.3727/096504013X13793555706722. [DOI] [PubMed] [Google Scholar]
- 41.Altieri DC. Validating survivin as a cancer therapeutic target. Nat Rev Cancer. 2003;3:46–54. doi: 10.1038/nrc968. [DOI] [PubMed] [Google Scholar]
- 42.Yang L, Cao Z, Yan H, Wood WC. Coexistence of high levels of apoptotic signaling and inhibitor of apoptosis proteins in human tumor cells: implication for cancer specific therapy. Cancer Res. 2003;63:6815–6824. [PubMed] [Google Scholar]
- 43.Sagol O, Yavuzsen T, Oztop I, Ulukus C, Ylmaz U, Alakavuklar M, et al. The effect of apoptotic activity, survivin, Ki-67, and P-glycoprotein expression on prognosis in pancreatic carcinoma. Pancreas. 2005;30:343–348. doi: 10.1097/01.mpa.0000160285.87322.3e. [DOI] [PubMed] [Google Scholar]
- 44.Shrader M, Pino MS, Lashinger L, Bar-Eli M, Adam L, Dinney CP, et al. Gefitinib reverses TRAIL resistance in human bladder cancer cell lines via inhibition of AKT-mediated X-linked inhibitor of apoptosis protein expression. Cancer Res. 2007;67:1430–1435. doi: 10.1158/0008-5472.CAN-06-1224. [DOI] [PubMed] [Google Scholar]
- 45.Ui T, Morishima K, Saito S, Sakuma Y, Fujii H, Hosoya Y, et al. The HSP90 inhibitor 17-N-allylamino-17-demethoxy geldanamycin (17-AAG) synergizes with cisplatin and induces apoptosis in cisplatin-resistant esophageal squamous cell carcinoma cell lines via the Akt/XIAP pathway. Oncol Rep. 2014;31:619–624. doi: 10.3892/or.2013.2899. [DOI] [PubMed] [Google Scholar]
- 46.Hemmings BA, Restuccia DF. PI3K-PKB/Akt pathway. Cold Spring Harb Perspect Biol. 2012;4:a011189. doi: 10.1101/cshperspect.a011189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cicenas J. The potential role of Akt phosphorylation in human cancers. Int J Biol Markers. 2008;23:1–9. doi: 10.1177/172460080802300101. [DOI] [PubMed] [Google Scholar]
- 48.Davies MA. Regulation, role, and targeting of Akt in cancer. J Clin Oncol. 2011;29:4715–4717. doi: 10.1200/JCO.2011.37.4751. [DOI] [PubMed] [Google Scholar]
- 49.Badescu A, Couvelard A, Handra-Luca A. Akt pathway protein expression in gastrointestinal Kaposi sarcomas: relevance for tumor biology. APMIS. 2014;122:518–525. doi: 10.1111/apm.12190. [DOI] [PubMed] [Google Scholar]
- 50.Cheung M, Testa JR. Diverse mechanisms of AKT pathway activation in human malignancy. Curr Cancer Drug Targets. 2013;13:234–244. doi: 10.2174/1568009611313030002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cheng GZ, Park S, Shu S, He L, Kong W, Zhang W, et al. Advances of AKT pathway in human oncogenesis and as a target for anti-cancer drug discovery. Curr Cancer Drug Targets. 2008;8:2–6. [PubMed] [Google Scholar]
- 52.Liu W, Bagaitkar J, Watabe K. Roles of AKT signal in breast cancer. Front Biosci. 2007;12:4011–4019. doi: 10.2741/2367. [DOI] [PubMed] [Google Scholar]
- 53.Testa JR, Bellacosa A. AKT plays a central role in tumorigenesis. Proc Natl Acad Sci U S A. 2001;98:10983–10985. doi: 10.1073/pnas.211430998. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.