Abstract
Background
Antenatal care is of core importance for maternal and child health and is therefore a central aspect of mother and child health care. One of the main goals of effective screening in antenatal care is the detection of suboptimal fetal growth. However, the sensitivity of antenatal diagnostic of suboptimal fetal growth (i.e. intrauterine growth restriction; IUGR) through clinical routine fetal ultrasonography has been observed to be low. A study conducted in Germany found that only 30% of IUGR cases and 40% of congenital malformations were diagnosed antenatally. Reasons for this low detection rate remain unclear.
Methods/Design
In the first of two study components, all mothers who delivered or will deliver a small for gestational age (SGA) newborn in one of three hospitals in Bremen (Germany) during recruitment phase are eligible for inclusion in a hospital based case–control study. Cases are defined as neonates with an IUGR that was not detected antenatally, while controls are defined as neonates whose IUGR was identified or at least suspected antenatally. Data collection instruments include a newborn documentation sheet, a standardized, computer-assisted personal interview with mothers, and a copy of pregnancy record books. The second component is a survey among all private practice-based gynecologists in the federal states of Bremen and Lower Saxony. The aim of this survey was to obtain detailed information e.g. on quality of ultrasonography equipment and examiner’s ultrasonography experience and qualification level.
Discussion
To our knowledge, this is one of the few German studies explicitly addressing care-related as well as maternal-related factors influencing the (non-) detection of IUGR by conducting comprehensive interviews with mothers and private practice-based gynecologists. Over the last 15 years there have been substantial technological advances in ultrasonography equipment in gynecological practices; hence there is the need to evaluate whether the detection rates of IUGR in Germany are still as low as previously reported in the late 1990ies. Our study results will contribute to a better understanding of core risk factors for low early detection rates of intrauterine growth restrictions and may support quality development in this important health care sector.
Keywords: Case–control study, Prenatal care, Intrauterine growth restriction, Prenatal ultrasonography
Background
Early detection of intrauterine growth restriction (IUGR) is of core importance for maternal and child health. Pathological small for gestational age births (i.e. IUGR) due to a pathological process are unable to reach their growth potential, resulting in an increased risk for fetal distress or fetal death during pregnancy or delivery [1-3]. Inadequate fetal growth is also associated with perinatal morbidity and an elevated risk for delayed effects such as chronic diseases in later life. These include cerebral palsy, systolic hypertension and cardiovascular disease, metabolic syndrome, obesity, insulin resistance and diabetes type II [4,5]. The incidence of IUGR in Western Europe is approximately 3-8% of all pregnancies but the diagnosis during pregnancy is rather suspected [6-8]. The majority of IUGR fetuses are SGA, defined as a birth weight <10th percentile for gestational age. While approximately 80-85% of the fetuses diagnosed as being SGA are constitutionally small but healthy, 10-15% can be identified as ‘true’ IUGR cases and the remaining 5-10% are due to chromosomal anomalies or chronic intrauterine infections [9].
However, because IUGR is a prenatal condition, SGA at birth serves as a proxy measure for prenatal IUGR [10]. Fetuses identified as SGA comprise a heterogeneous group with regard to underlying causes, management and prognosis [11,12].
There are currently no effective therapies for the treatment of IUGR. Its management during pregnancy involves intensified fetal surveillance as well as choosing the optimal time and method of delivery [5,13]. If they still smoke, the affected women are advised to stop or reduce smoking during the course of the pregnancy. To enable timely monitoring of these pregnancies, it is important that suboptimal fetal growth is detected early. Hence this is one of the main goals of effective screening in antenatal care. In Germany, ultrasonography is an essential part of antenatal care and the main IUGR screening method used. According to the maternity guidelines, three ultrasonography examinations should be routinely conducted during the course of pregnancy. These examinations are typically conducted by practice-based gynecologists. The guidelines also advise that women with suspected IUGR be further examined using Doppler ultrasonography [8] or be transferred to specialists or a hospital for confirmation of the diagnosis.
While studies on the efficacy of ultrasonography screening under study conditions reported high sensitivities of 80-90% for antepartal detection of IUGR [14,15], sensitivity in clinical routine (effectiveness) in the late 1990ies and early 2000 was about 25-30% [16,17]. A study conducted under routine service conditions in the early 1990ies in Germany found that only 30% of cases with IUGR and 40% of congenital malformations were diagnosed antenatally [16,18]. Gynecologists in private practice had the lowest detection rates. These findings indicated that one of the main objectives of routine screening in pregnancy may not be achieved, thereby pointing out a quality problem in antenatal care in Germany. Similar results have been reported for congenital malformations in Germany, with studies reporting an overall antenatal detection rate of 40% at best [19-21]. Possible reasons for non-detection of IUGR during pregnancy remain unclear. More evidence is available on antenatal detection of congenital malformations, with a high correlation being observed between the sensitivity of antenatal diagnosis and the type of medical institution (e.g. practice-based gynecologists, center for prenatal diagnosis or hospital), quality of the ultrasonography equipment, as well as ultrasonography experience and qualification level of the examiner [22-28]. Studies conducted in Austria and Switzerland reported detection rates of 22% for congenital malformations in gynecological practices compared to approximately 90% in centers for prenatal diagnosis and therapy [29,30]. A comprehensive review on the effectiveness of prenatal ultrasonography examinations conducted by the Institute for Quality and Efficiency in Health Care (IQWIG), Germany, confirmed the important influence of the quality of ultrasonography equipment and the qualification of the investigator on the antenatal detection of congenital malformations [31]. However, only a few of the reviewed studies explicitly focused on these factors. The IQWIG clearly expressed the need for analytical studies examining the effect of the following factors on the antenatal detection of diagnoses: examiner’s ultrasonography experience and qualification level, and quality of ultrasonography equipment.
Further factors that possibly influence the effectiveness of ultrasonography screening in antenatal care are equity of access to antenatal care and the actual process of care. Several studies have reported differences in use and timing of antenatal care and also indicated differences in quality of care between women depending on social class and migrant background. These differences may result in an increased risk of unfavorable pregnancy and birth outcomes for socially disadvantaged groups [32-35]. Among those with a migrant background, factors such as cultural and religious background, length of stay in new country of residence, access to health care information, differences in health systems between country of origin and new country of residence, language proficiency, education level and social status may also affect their participation as well as the examination process during antenatal care [36]. Using the quality of documentation of maternity records as a proxy indicator for the quality of care, researchers in Germany observed differences in the quality of antenatal care between women of German and non-German nationality [37]. The completeness of anamnestic data and documentation of consultation were found to be lower among women of non-German nationality than among German women. Thus, in Germany, it can be assumed that the documentation of prenatal diagnoses (e.g. IUGR) among women with migrant background is of lower quality than among those without migrant background, possibly resulting in insufficient surveillance of intrauterine growth among the former.
Furthermore, an analysis of the national perinatal registry in Germany showed a higher probability of stillbirth in combination with SGA for women with migrant background compared to German women [32]. As the associated risk factors for stillbirth were similarly distributed in both groups, it can be assumed that the observed stillbirth differences may be partly attributed to differences in the quality of antenatal care.
Up to now, most of the literature on antenatal diagnoses has focused on the detection of congenital malformations. Thus, there is a need to directly address IUGR detection through dedicated investigations. The objective of this paper is to describe the aims and study design of the ongoing BIUS project, entitled “Care-related factors associated with antenatal diagnosis of intrauterine growth restrictions – A case–control study”. The BIUS project is funded by the German Federal Ministry of Education and Research (BMBF).
Methods/Design
Aims of the study
The aim of this hospital-based case–control-study is to identify care-related and maternal risk factors for non-detection of intrauterine growth restrictions during pregnancy. The study will also examine differences in quality of care, course of treatment and access to care in relation to maternal characteristics such as age, parity, socio-economic status and migrant status.
The specific aims of the study are:
To describe the sensitivity of antepartal diagnosis of IUGR and compare it with the reported low rates in an earlier study by Jahn et al. in 1998 [16].
To identify care-related and maternal risk factors (e.g. ultrasonography experience and qualification level of examiner, type of medical institution, quality of ultrasonography equipment, maternal smoking) that are associated with an inadequate diagnosis and treatment of IUGR during pregnancy.
To investigate if there are specific groups having a higher chance of non-detected IUGR (e.g. women with a migrant background).
Study design
The ongoing BIUS study is a hospital-based case–control study in which newborns that are SGA are prospectively sampled. The recruitment of cases and controls is carried out in cooperation with the obstetric units of three hospitals in the federal city-state of Bremen, Germany. The study region covers a geographical area of 419.38 km2 with 654.774 residents and 5.657 deliveries in 2012. Approximately 4.935 of these deliveries were in the three cooperating hospitals, out of six hospitals with an obstetric unit overall.
The study has two main components. In the first, mothers of newborns that are SGA participate in computer assisted personal interviews during which information on pregnancy risk factors, uptake and quality of prenatal care is collected. The second component is a survey among all private practice-based gynecologists in the federal states of Bremen and Lower Saxony. The physician survey was also conducted in Lower Saxony because a considerable proportion of the eligible women who deliver their newborns in the participating hospitals live in Lower Saxony. The aim of this survey is to gather information on the physicians’ ultrasonography experience and qualification level as well as on the quality of ultrasonography equipment. All gynecologists in the federal states of Bremen and Lower Saxony were informed about the study beforehand via hospitals, the Ethics board of the Bremen Medical Association and the media (Figure 1).
Figure 1.
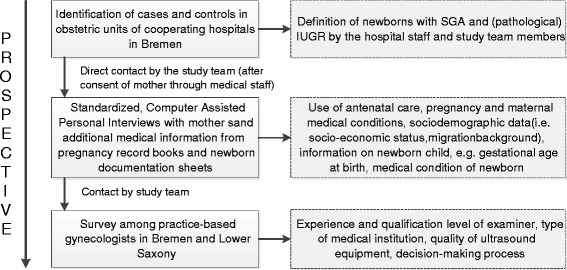
Flow chart of study procedure and stages.
Case–control-definition and recruitment of participants
All women who delivered an SGA newborn from 01.01.2013 up to 30.06.2015 (*in one hospital the recruitment period began on 01.08.2012) in one of the participating obstetric units in Bremen are eligible for the study and invited to participate. During the recruitment period, SGA newborns are identified using two independent approaches. Firstly, SGA is diagnosed by the attending obstetricians based on the birth weight in relation to gestational age, sex and findings and symptoms at birth. Secondly, to avoid missing the diagnosis of any SGA newborn, all birth records as from 01.01.2013 are screened by the project team and information on birth weight in relation to gestational age, sex and findings and symptoms at birth is extracted. We use a three stage approach to enroll study participants. After the initial information about the study, women are contacted by mail through the study nurses working in the hospital. Reminders are sent three and six weeks after initial contact, including a non-responder questionnaire after six weeks.
In compliance with routinely used growth references for newborns in Germany [38], in both approaches SGA is defined as birth weight <10th percentile for gestational age and sex. For the purpose of our study, cases are defined as neonates with an undetected IUGR during pregnancy and controls as neonates whose IUGR was successfully identified antenatally. Newborns with suspected IUGR documented in medical records are also defined as controls. The final assignment to the case or the control group, i.e. antenatally detected versus non-detected IUGR, will be done taking further information from the medical records and pregnancy record books into account (e.g. condition and timing of IUGR diagnosis, date of birth, gestational age at birth, birth weight, diseases and infections during pregnancy).
In line with local ethical and data protection requirements, mothers of all SGA newborns are initially informed about the study by the attending obstetricians during their hospital stay or via mail if they have already left the hospital. The obstetricians obtain the initial consent for the mothers to be contacted by the research team. This process of enrolment is supported by several study nurses who are employed at the cooperating hospitals during the course of the study. Once the initial written consent has been given, the mothers’ personal identifying information is forwarded to the research institute. Thereafter the mothers are provided with detailed information on the study procedures and an appointment for the personal interview is set.
As the obstetric units in Bremen cater for an ethnic diverse population, study materials (i.e. study information, study flyer) are available in Russian and Turkish, the languages spoken by the two main migrant groups in the region. Where required, the maternal interviews can also be conducted in each of these languages.
Ethics statement and consent
Ethical approval for all study procedures was obtained from the ethics review board of the Bremen Medical Association. All women who deliver an SGA newborn in one of the cooperating hospitals receive written and oral information about the study. All participating women have to give written informed consent for data collection.
Data collection
Newborn documentation
All SGA newborns are identified during medical examinations immediately after birth and/or through retrospective screening of the birth record books. Basic information such as birth weight, birth length and head circumference, gestational age at birth and mode of delivery are documented by obstetricians or study nurses on a study-specific newborn documentation sheet. Details on the form and severity and timing of IUGR diagnosis (e.g. antenatal vs. at birth) are added by the attending obstetrician or pediatrician in the hospital (Table 1).
Table 1.
Data collection: source of information and variables concerning
| Data source | Field | Variables concerning |
|---|---|---|
| Computer-assisted personal Interview (CAPI) | General information | Age*, Weight*, lengths* |
| CAPI; pregnancy record book | Pregnancy and maternal medical conditions | Weight gain during pregnancy, diseases and infections during pregnancy**, number, time and reason for any hospitalization during pregnancy |
| CAPI | Tobacco, coffee and substance consumption | Smoking habits*, alcohol intake*, drug intake, coffee consumption |
| CAPI; pregnancy record book | Use of antenatal care | Number and time of antenatal care visits, Number and time of routine ultrasonography, further examinations during pregnancy (specialists), parity (live/stillbirth, miscarriages, etc.), type of medical institution |
| Pregnancy record book; newborn documentation sheet | Newborn child | Date of birth, sex, gestational age at birth, birth weight, birth lengths, head circumference, APGAR score, mode of delivery, IUGR/SGA diagnosis, number of siblings, birth order, diseases or birth defects of newborn (e.g. trisomy 21, congenital malformations) |
| CAPI | Socio-demographic and economic information | Marital status, migrant background, family size, school and professional education, occupation, family income |
| Self-administered questionnaire (physician survey) | Further care-related factors | Quality of ultrasonography equipment, examiner’s ultrasonography experience and qualification level, decision-making process, certificate for ultrasonography, prenatal health information on IUGR |
*Information on both mother and father.
**Confirmed by a doctor.
Maternal survey
All mothers who consent to the study are interviewed in the hospital shortly after delivery or at home should they have already been discharged. The questionnaire is designed as a standardized Computer Assisted Personal or Telephone Interview (CAPI/CATI). To account for different individual circumstances of each participating woman after birth and selection bias (e.g. due to severity of IUGR and that the mothers may want to focus their full attention on their infants), we offer three interview options, either a CAPI directly in the hospital, a CAPI after birth at home or a CATI. The questionnaire, which was developed in close collaboration with obstetric experts, covers aspects on socio-demographic information, medical conditions and risk factors for IUGR during pregnancy, as well as use, timing and content of antenatal care (Table 1). Additionally, detailed information on medical conditions, timing of antenatal care and results of fetal ultrasonography during pregnancy is available from the pregnancy record books that will be copied after the interview and taken to the research institute. The interviews are conducted by trained project personnel.
The whole study procedure was pre-tested among a small sample of mothers prior to the recruitment phase. All mothers who decline to participate in the study are asked to fill in a short version of the questionnaire containing socio-demographic and certain birth-related data.
Survey among gynecologists
A physician survey among all gynecologists in Bremen and Lower Saxony was conducted from January 2014 up to July 2014. The gynecologists were pre-informed about the survey through newsletters of the Association of Statutory Health Insurance Physicians (Kassenärztliche Vereinigung) in Bremen and Lower Saxony two weeks before the initial survey contact. A total of 1,141 private practice-based gynecologists in the two federal states were asked to participate using a three stage approach including written mail and email contact. The survey comprised a self-administered web-based or paper questionnaire, containing 21 items covering aspects on the gynecologists’ experience and qualification in ultrasonography, as well as the quality of the ultrasonography equipment they use (Table 1).
Expected number of participants during the recruitment phase
According to data from 2012, the annual number of deliveries in the three participating hospitals is approximately 4.935 (=12.339 deliveries in 2½ years). During the course of the recruitment phase, we thus expect approximately 370 to 987 newborns with IUGR (3-8%) (Table 2). Assuming a response rate of 50%, 185 to 494 cases can be included in this study (Table 2).
Table 2.
Expected number of participants with IUGR based on 2012 data
| Hospital 1 | Hospital 2 | Hospital 3 | Total | |
|---|---|---|---|---|
| Number of deliveries within 2½ years | 5.763 | 4.988 | 1.588 | 12.339 |
| IUGR (3-8%) | 173-461 | 150-399 | 48-127 | 370-987 |
| Response (50%) | 87-231 | 75-200 | 24-64 | 185-494 |
Data management and data analyses
At recruitment, each participating woman receives a unique study identifier. This number is used to identify her pseudonymised data and allows the linkage of all collected information across the study, i.e. data from the personal interview, the pregnancy record book and the newborn documentation sheet. The interview data will be directly transferred into the study database after the interview. The study-specific newborn documentation sheet is only transferred to the research institute if the mother has given informed consent. Otherwise all data remain in the hospitals. Data from the pregnancy record book and the newborn documentation sheet are entered into the study database by medical documentation specialists. Immediate automated data completeness and plausibility checks are done. In addition, various strategies such as validation checks for consistency and completeness of routinely collected data, training of study team members and of clinical and project staff are implemented to maximize the quality of data collection.
The web-based responses of the physician survey were automatically entered into the physician survey database, while surveys returned by mail were manually entered into the same software program by a research assistant. The database of the physician survey and the database of maternal interviews will be combined for statistical analyses at group level.
The study data will be analyzed using descriptive and analytical approaches. Differences in socio-demographic, pregnancy and birth related characteristics between cases and controls, as well as between responders and non-responders will be statistically tested using chi-square tests for categorical variables or student’s t-test for continuous variables. Associations between care-related or maternal determinants and non-detection of IUGR will be examined in crude and multiple logistic regression models and presented as odds ratios (OR) with 95% confidence intervals (CI). In sensitivity analyses we will examine differences in the applied method of case–control identification (patient record screening vs. identification by obstetrician at birth) and apply different cut-off limits for IUGR definition (i.e. birth weight <10th, <5th and <3rd percentile for gestational age) to assess any changes in detection rates.
Discussion
This study aims to evaluate antenatal detection-rates of IUGR and to identify possible influencing factors associated with non-detection of IUGR during pregnancy by examining antenatal care routines in Germany, and particularly the performance of fetal ultrasonography. Furthermore, the study aims to identify possible high risk groups for antenatal non-detection of IUGR in terms of different social groups and according to migrant background. To our knowledge, this is one of the few German studies explicitly addressing care-related as well as maternal-related factors influencing the (non-) detection of IUGR by conducting comprehensive interviews with mothers and practice-based gynecologists. Technological advances in ultrasonography equipment have occurred over the last 15 years, and thus there is a need to evaluate whether the detection rates of IUGR in Germany are still as low as previously reported in the late 1990ies. As already mentioned, results from studies on congenital malformations suggest that the sensitivity of antenatal diagnosis is highly correlated with the type of medical institution, quality of the ultrasonography equipment and examiner’s experience and qualification level [22-28]. We will investigate if the same is true for antenatal diagnosis of IUGR. Our study results will contribute to a better understanding of core risk factors for low early detection rates of IUGR and may provide a better evidence basis for quality development in this important health care sector.
While the term ‘small for gestational age’ refers to neonates with a birth weight below the 10th percentile and is not the same as IUGR, many publications use the terms interchangeably [39,40]. There is no standard definition of IUGR. In some publications it has been defined as a birth weight <2 standard deviations below the median for gestational age, whereas in others a threshold of 3rd or 5th percentile of weight for age for the given population is used [10,41]. For the purpose of our study, we use percentile values for the German population [38] to identify cases and controls. These percentile values do not take the individual fetal growth potential into account to differentiate between physiological and pathological smallness (e.g. considering ethnicity, maternal weight and height) [42]. To our knowledge customized growths charts are not available for Germany so far. In order to deal with this potential limitation, we will conduct sensitivity analyses with different cut-off limits. According to literature, a true IUGR is more likely with lower cut-off [43], thus we can take risk differences between constitutionally SGA neonates and clinically relevant IUGR into consideration.
Due to the relatively low incidence of IUGR (3-8%), the recruitment of cases and controls in this study is a particular challenge. Furthermore, the time available for the recruitment of the individual mothers is very limited as postpartum women usually stay in hospital only for a short observation period. Another factor which might influence response rates is severity of IUGR. It is possible that mothers whose newborns have severe IUGR will decline to participate in the study as they will want to focus their full attention on their infants. In addition, response bias might arise with parents who are more engaged in their child’s health being more willing to take part in the study. In an attempt to address these issues we offer three interview options, either a CAPI directly in the hospital, a CAPI after birth at home or a CATI. We also implemented several reminders and translated the study information and the interview in different languages (i.e. Russian, Turkish) to cater for the main migrant groups living in the study region. A main strength of this study is that it relies on study data from different hospitals that cover diverse socio-economic settings in the federal state-city of Bremen.
The interviews were pretested with mothers of neonates who are diagnosed with SGA or IUGR in one of the participating hospitals to ensure clarity and feasibility of the interview questions, language, structure and time needed.
Conclusions
The present study evaluates the quality of antenatal care and hopes to contribute further information to the discussion of effectiveness of ultrasonography screening in relation to detection-rates of IUGR and to a better understanding of influencing factors regarding non-detection of IUGR. The results will be discussed with the clinical partners, published in scientific journals and presented at national and international conferences.
Acknowledgements
We gratefully acknowledge the cooperation of physicians, obstetricians and midwives of the obstetric units of the three cooperating hospitals in the study region of Bremen City: Klinikum Links der Weser (LdW), St. Joseph Stift Hospital (SJS) and Ev. Diakonie-Krankenhaus (DIAKO). Special thanks to Florence Samkange-Zeeb for proofreading the manuscript and Hande Gencer for her support in the manuscript preparation. The study is funded by the German Federal Ministry of Education and Research (BMBF) (FKZ: 01GY1131).
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AR, JS, and HZ conceived the study. AR, SAE, JS, TB and HZ contributed to the overall design and completion of the study. KP supported the practical implementation of the study with expertise in obstetrics and gynecology. SAE and AR wrote the first draft of the manuscript, with contributions from HZ. All authors read and approved the final manuscript.
Authors’ information
Sinja Alexandra Ernst and Anna Reeske are first author.
Contributor Information
Sinja Alexandra Ernst, Email: ernst@bips.uni-bremen.de.
Anna Reeske, Email: Reeske.Anna@baua.bund.de.
Jacob Spallek, Email: jacob.spallek@uni-bielefeld.de.
Knud Petersen, Email: Knud.Petersen@klinikum-bremen-ldw.de.
Tilman Brand, Email: brand@bips.uni-bremen.de.
Hajo Zeeb, Email: zeeb@bips.uni-bremen.de.
References
- 1.Kady S, Gardosi J. Perinatal mortality and fetal growth restriction. Best Pract Res Clin Obstet Gynaecol. 2004;18:397–410. doi: 10.1016/j.bpobgyn.2004.02.009. [DOI] [PubMed] [Google Scholar]
- 2.Figueras F, Gardosi J. Intrauterine growth restriction: new concepts in antenatal surveillance, diagnosis, and management. Am J Obstet Gynecol. 2011;204:288–300. doi: 10.1016/j.ajog.2010.08.055. [DOI] [PubMed] [Google Scholar]
- 3.Mandruzzato G, Antsaklis A, Botet F, Chervenak FA, Figueras F, Grunebaum A, Puerto B, Skupski D, Stanojevic M. Intrauterine restriction (IUGR) J Perinat Med. 2008;36(4):277–281. doi: 10.1515/JPM.2008.050. [DOI] [PubMed] [Google Scholar]
- 4.Jacobsson B, Ahlin K, Francis A, Hagberg G, Hagberg H, Gardosi J. Cerebral palsy and restricted growths status at birth: population-based case–control study. BJOG. 2008;115:1250–1255. doi: 10.1111/j.1471-0528.2008.01827.x. [DOI] [PubMed] [Google Scholar]
- 5.Salam RA, Das JK, Bhutta ZA. Impact of intrauterine growth restriction on long-term health. Curr Opin Clin Nutr Metab Care. 2014;17(3):249–254. doi: 10.1097/MCO.0000000000000051. [DOI] [PubMed] [Google Scholar]
- 6.Crombach G. Intrauterine wachstumsrestriktion. Teil I: klassifikation, pathogenese und diagnose. Gynäkologie. 2007;40(11):891–90. doi: 10.1007/s00129-007-2057-9. [DOI] [Google Scholar]
- 7.Wollmann HA. Intrauterine growth restriction: definition and etiology. Horm Res. 1998;49(2):1–6. doi: 10.1159/000053079. [DOI] [PubMed] [Google Scholar]
- 8.Gembruch U, Baschat AA, Harman CR. Diagnostik und fetale Überwachung bei intrauteriner Wachstumsrestriction. Gynakologe. 2001;34:1128–1137. doi: 10.1007/s001290101089. [DOI] [Google Scholar]
- 9.Manning FA. General Principles and Applications of Ultrasonography. In: Creasy RK, Resnik R, editors. Maternal-Fetal Medicine: Principles and Practice. Philadelphia: Saunders; 2004. [Google Scholar]
- 10.Bakketeig LS. Current growth standards, definitions, diagnosis and classification of fetal growth retardation. Eur J Clin Nutr. 1998;52(Suppl 1):S1–S4. [PubMed] [Google Scholar]
- 11.Stratton JF, Scanaill SN, Stuart B, Turner MJ. Are babies of normal birth weight who fail to reach their growth potential as diagnosed by ultrasound at increased risk? Ultrasound Obstet Gynecol. 1995;5:114–118. doi: 10.1046/j.1469-0705.1995.05020114.x. [DOI] [PubMed] [Google Scholar]
- 12.Sheridan C. Intrauterine growths restriction-diagnosis and management. Aust Fam Physician. 2005;34:717–723. [PubMed] [Google Scholar]
- 13.Vetter K. Therapieoption bei Wachstumsrestriktion des Fetus (IUGR) Gynakologe. 2001;34:1124–1127. doi: 10.1007/s001290101082. [DOI] [Google Scholar]
- 14.Rosendahl H, Kivinen S. Detection of small for gestational age fetuses by the combination of clinical risk factors and ultrasonography. Eur J Obstet Gynecol Reprod Biol. 1991;39(1):7–11. doi: 10.1016/0028-2243(91)90134-7. [DOI] [PubMed] [Google Scholar]
- 15.Neilson JP, Munjana SP, Whitfield CR. Screening for small for date fetuses: a controlled trial. Brit Med J. 1984;289:1179–1182. doi: 10.1136/bmj.289.6453.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jahn A, Razum O, Berle P. Routine screening for intrauterine growth retardation in Germany: low sensitivity and questionable benefit for diagnosed cases. Acta Obstet Gynecol Scand. 1998;77(6):643–648. doi: 10.1034/j.1600-0412.1998.770611.x. [DOI] [PubMed] [Google Scholar]
- 17.Bais JMJ, Eskes M, Pel M, Bonsel GJ, Bleker OP. Effectiveness of detection of intrauterine growth retardation by abdominal palpation as screening test in a low risk population: an observational study. Eur J Obstetrics & Gynecology and Reproductive Biology. 2004;116:164–169. doi: 10.1016/j.ejogrb.2004.01.037. [DOI] [PubMed] [Google Scholar]
- 18.Jahn A, Razum O, Berle P. Routine-Ultraschall in der deutschen Schwangerenvorsorge: Ist die Effektivität gesichert. Geburtshilfe Frauenheilkd. 1999;59(3):97–102. doi: 10.1055/s-1999-14168. [DOI] [Google Scholar]
- 19.Petersen J, Jahn A. Suspicious findings in antenatal care and their implications from the mothers’ perspective: a prospective study in Germany. Birth. 2008;35(1):41–49. doi: 10.1111/j.1523-536X.2007.00210.x. [DOI] [PubMed] [Google Scholar]
- 20.Queisser-Luft A, Stopfkuchen H, Stolz G, Schlaefer K, Merz E. Prenatal diagnosis of major malformations: quality control of routine ultrasound examinations based on a five-year study of 20248 newborn fetuses and infants. Prenat Diagn. 1998;18:567–576. doi: 10.1002/(SICI)1097-0223(199806)18:6<567::AID-PD302>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 21.Behrens O, Steiner C, Böhmer S, Mühlhaus K. Qualität des Ultraschall-Screenings in der Schwangerenvorsorge. Zentralbl Gynakol. 1999;121(5):228–232. [PubMed] [Google Scholar]
- 22.Whitworth M, Bricker L, Neilson JP, Dowswell T. Ultrasound for fetal assessment in early pregnancy. Cochrane Database Syst Rev. 2010;4:Art No. CD007058. doi: 10.1002/14651858.CD007058.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Randall P, Brealey S, Hahn S, Khan KS, Parsons JM. Accuracy of fetal echocardiography in the routine detection of congenital heart disease among unselected and low risk populations: a systematic review. BJOG. 2005;112(1):24–30. doi: 10.1111/j.1471-0528.2004.00295.x. [DOI] [PubMed] [Google Scholar]
- 24.Rosery H, Maxio-Bergemann S, Rosery B, Bergemann R. HTA Bericht Bd. 10: Ultraschall in der Schwangerschaft - Beurteilung der routinemäßigen Schwangerschaftsultraschalluntersuchungen unter Maßgabe der Mutterschaftsrichtlinie. Köln: DIMDI; 2004. [Google Scholar]
- 25.Vos JM, Offringa M, Bilardo CM, Lijmer JG, Barth PG. Sensitive and specific screening for detection of spina bifida by echography in the second trimester: systematic review and meta-analysis. Ned Tijdschr Geneeskd. 2000;144(36):1736–1741. [PubMed] [Google Scholar]
- 26.Levi S, Hyjazi Y, Schaaps JP, Defoort P, Coulon R, Buekens P. Sensitivity and specifity of routine antenatal screening for congenital anomalies by ultrasound. The Belgian multicentric study. Ultrasound Obstet Gynecol. 1991;1:102–110. doi: 10.1046/j.1469-0705.1991.01020102.x. [DOI] [PubMed] [Google Scholar]
- 27.Tegnander E, Eik-Nes SH. The examiner’s ultrasound experience has a significant impact on the detection rate of congenital heart defects at the second-trimester fetal examination. Ultra-sound Obstet Gynecol. 2006;28(1):8–14. doi: 10.1002/uog.2804. [DOI] [PubMed] [Google Scholar]
- 28.Rustico MA, Benettoni A, D’Ottavio G, Fischer-Tamaro L, Conoscenti GC, Meir Y, Natale R, Bussani R, Mandruzzato GP. Early screening for fetal cardiac anomalies by transvaginal echocardiography in an unselected population: the role of operator experience. Ultrasound Obstet Gynecol. 2000;16(7):614–619. doi: 10.1046/j.1469-0705.2000.00291.x. [DOI] [PubMed] [Google Scholar]
- 29.Bernaschek G, Stuempflen I, Deutinger J. The influence of the experience of the investigator on the rate of sonographic diagnosis of fetal malformations in Vienna. Prenat Diagn. 1996;16(9):807–811. doi: 10.1002/(SICI)1097-0223(199609)16:9<807::AID-PD949>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 30.Vial Y, Tran C, Addor MC, Hohlfeld P. Screening for foetal malformations: performance of routine ultrasonography in the population of the Swiss canton of Vaud. Swiss Med Wkly. 2001;131(33–34):490–494. doi: 10.4414/smw.2001.09789. [DOI] [PubMed] [Google Scholar]
- 31.Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG) Ultraschallscreening in der Schwangerschaft: Testgüte Hinsichtlich der Entdeckungsrate Fetaler Anomalien. Abschlussbericht S05-03. Köln: IQWiG; 2008. [Google Scholar]
- 32.Reeske A, Kutschmann M, Razum O, Spallek J. Stillbirth differences according to regions of origin: an analysis of the German perinatal database, 2004–2007. BMC Pregnancy Childbirth. 2011;11:63. doi: 10.1186/1471-2393-11-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Koller D, Lack N, Mielck A. Soziale Unterschiede bei der Inanspruchnahme der Schwangerschafts-Vorsorgeuntersuchungen, beim Rauchen der Mutter während der Schwangerschaft und beim Geburtsgewicht des Neugeborenen. Empirische Analyse auf Basis der Bayerischen Perinatal-Studie. Gesundheitswesen. 2009;71:10–18. doi: 10.1055/s-0028-1082310. [DOI] [PubMed] [Google Scholar]
- 34.David M, Pachaly J, Vetter K. Perinatal outcome in Berlin (Germany) among immigrants from Turkey. Arch Gynecol Obstet. 2006;247:271–278. doi: 10.1007/s00404-006-0182-7. [DOI] [PubMed] [Google Scholar]
- 35.Simoes E, Kunz S, Bosing-Schwenkglenks M, Schwoerer P, Schmahl FW. Inanspruchnahme der Schwangerschaftsvorsorge – ein Spiegel gesellschaftlicher Entwicklungen und Aspekte der Effizienz. Untersuchung auf Basis der Perinatalerhebung Baden-Württemberg 1998–2001. Geburtsh Frauenheilk. 2003;61:538–545. [Google Scholar]
- 36.Spallek J, Zeeb H, Razum O. Prevention among immigrants: the example of Germany. BMC Public Health. 2010;10:92. doi: 10.1186/1471-2458-10-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tadesse R, Jahn A, Razum O. How well do doctors document their findings in antenatal care – and are their differences between women of German and non-German nationality? ᅟ. 1999;5:ᅟ. [Google Scholar]
- 38.Voigt M, Schneider KTM, Jährig K. Analyse des Geburtengutes des Jahrgangs 1992 der Bundesrepublik Deutschland. Teil I: Neue Perzentilwerte für die Körpermaße von Neugeborenen. Geburtsh u Frauenheilk. 1996;56:550–558. doi: 10.1055/s-2007-1023283. [DOI] [PubMed] [Google Scholar]
- 39.Bamberg C, Kalache KD. Prenatal diagnosis of fetal growth restriction. Semin Fetal Neonatal Med. 2004;9:387–394. doi: 10.1016/j.siny.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 40.Law TL, Korte JE, Katikaneni LD, Wagner CL, Ebeling MD, Newman RB. Ultrasound assessment of intrauterine growth restriction: relationship to neonatal body composition. Am J Obstet Gynecol. 2011;205:255.e1-6. doi: 10.1016/j.ajog.2011.06.027. [DOI] [PubMed] [Google Scholar]
- 41.Ferro-Luzzi A, Ashworth A, Martorell R, Scrimshaw N. Report of the IDECG Working Group on effects of IUGR on infants, children and adolescents: immunocompetence, mortality, morbidity, body size, body composition, and physical performance. Eur J Clin Nutr. 1998;52(Suppl 1):S97–S99. [PubMed] [Google Scholar]
- 42.Gardosi J, Figueras F, Clausson B, Francis A. The costumised growth potential: an international research tool to study the epidemiology of fetal growth. Paediatr Perinat Epidemiol. 2010;25:2–10. doi: 10.1111/j.1365-3016.2010.01166.x. [DOI] [PubMed] [Google Scholar]
- 43.Gardosi J. Intrauterine growth restriction: new standards for assessing adverse outcome. Best Pract Res Clin Obstet Gynaecol. 2009;23(6):741–749. doi: 10.1016/j.bpobgyn.2009.09.001. [DOI] [PubMed] [Google Scholar]


