Abstract
In this case study we report a fracture of the lateral process of the talus (LPF) in a snowboarder. The fracture is frequently overlooked initially, due to subtle clinical and radiological findings and a low incidence rate. However, LPF are associated with significant morbidity when missed. To address this, we report one case of a patient with a LPF and provide a review of the available literature.
Background
A fracture of the lateral process of the talus (LPF) is thought to be an uncommon injury. The incidence of this fracture has been increasing simultaneously with the growing popularity of snowboarding in the early 90s. The symptoms of a LPF resemble the symptoms of an ankle sprain. Therefore, and because doctors are not aware of this injury due to low incidence rates, the fracture is frequently overlooked initially. LPF are associated with significant morbidity when missed. To address this, we report a case of a patient with a LPF and provide a review of the available literature.
Case presentation
A 29-year-old woman presented to our clinic with pain of her left ankle, after a fall during snowboarding a day earlier. She was able to fully bear weight immediately after the incident. She did not recall the exact movement her ankle made at impact. The algorithm for acute ankle injuries was followed.1 Visual inspection of the foot revealed a distinct swelling and ecchymosis around the lateral malleolus, specifically at the level of the anterior talofibular ligament without an external laesion or deformity. Active and passive range of motion was limited due to pain. Anterior drawer tests were negative. The Ottawa ankle rules were negative, but tenderness at the point of the anterior talofibular ligament was present. This clinical finding in combination with the trauma mechanism made us decide to perform imaging.
Investigations
On the ankle X-rays, a possible fracture line was identified at the anteroposterior view (figure 1A), but not on the lateral view (figure 1B). On CT scan a comminuted intra-articular fracture of the lateral process of the talus with a 2 mm gap in the talocalcaneo joint was seen (figure 1C).
Figure 1.
(A) Anteroposterior view of preoperative radiographs of the initial injury showing possible fracture line. (B) Lateral view of preoperative radiographs of the initial injury. (C) Anteroposterior view from CT scan revealing a comminuted intra-articular fracture of the lateral process of the talus.
Treatment
An open reduction and internal fixation was performed at the operating room using a Kirschner wire to realign the intra-articular comminution and 2.4 mm lag screws for compression and fixation (figures 2A, B and 3A, B). Postoperatively, a non-weight bearing short leg cast was applied for a period of 4 weeks followed by a full-weight bearing short leg cast for another period of 4 weeks.
Figure 2.
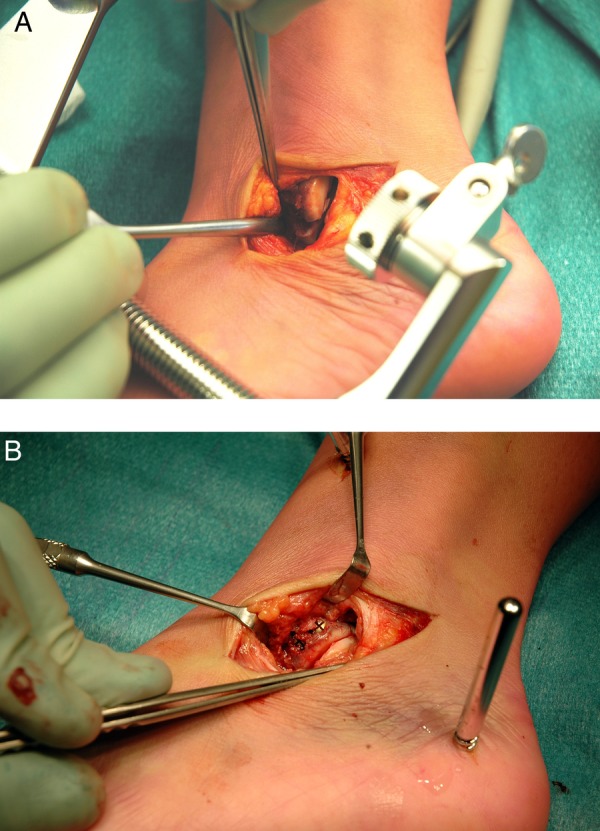
(A) Intraoperative views of the surgical approach showing the fracture of the lateral process of the talus (LPF). (B) Intraoperative views showing the fixation of the fracture of the LPF with screws and a K-wire.
Figure 3.

(A) Early postoperative anteroposterior radiographs of the reduction and fixation. (B) Early postoperative lateral radiographs of the reduction and fixation.
Outcome and follow-up
A follow-up CT scan was performed to examine the process of fracture healing. It demonstrated complete bone union and a correct anatomical position (figure 4A, B). After 3 months the patient was able to perform activities of daily living, but was not able to resume her running activities yet. Despite the mobility of the ankle, she reported local pain, which was attributed to the localisation of the osteosynthesis material. Therefore, the patient was scheduled for removal of the screw and wires, and returned to her baseline functional status.
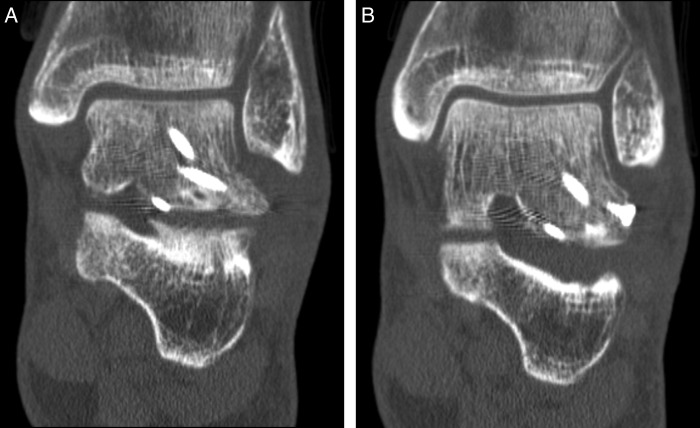
Figure 4.
(A and B) Anteroposterior view from CT scan 2 months postoperatively showing a correct anatomical position and complete bone fusion of the lateral process of the talus.
Discussion
In the past 20 years snowboarding has become an increasingly popular sport. Annually 1500 patients are treated in an emergency department in the Netherlands as a result of snowboard injuries.2 In the past, snowboarding was associated with a high incidence of accidents, but the incidence rates have become similar to skiing over the years,3–6 although the types of injury seen in skiers and snowboarders differ. Less injuries of the lower extremities are present in snowboarders compared with skiers (38% vs 54% respectively), but ankle injuries are more common in snowboarders than skiers (16% vs 6%).6 An explanation for these differences may be the more frequent use of soft boots in snowboarding, because the ability to stabilise the ankle is less compared to hard boots.6
In the literature, conflicting conclusions can be found about the mechanism of trauma. The location of the talus towards its surrounding structures creates a risk of injury. The lateral process of the talus is a wedge-shaped prominence with the articular surfaces often involved. It is important in many complex movements including inversion, eversion, dorsiflexion, plantar flexion and sliding of the articular surfaces in the subtalar articulation. Most authors describe a combination of dorsoflexion and inversion resulting in the fracture.7–9 On the contrary, a number of mechanic studies conclude that the fracture occurs due to eversion, and not inversion, of the ankle.10 Moreover, Boon et al11 suggests external rotation is an essential component in the mechanism of injury. In snowboarding, the fracture is often sustained after a high jump. Falls from height, car accidents and inversion of the ankle are other frequently mentioned causes.69 12 Special attention goes to a fracture of the lateral process of the talus associated with kayaking, described by Yan et al.13 These studies show an important role with regard to axial loading in combination with an out-of-plane orientation of the ankle.10 14
A LPF was rarely seen before the snowboarding era. Only little literature exists from before 1990 describing this injury,8 9 reporting an estimated incidence of LPF of 13 cases on a total of 1500 ankle injuries (0.86%) in the general population.9 However, more recent literature shows a higher incidence and implicates this to be associated with the increasing popularity of the snowboarding. Since the incidence of this fracture is remarkably higher in the snowboarding than in the general population, this injury is also called the ‘snowboarder's ankle’ or ‘snowboarder's fracture’. In two retrospective studies published in 1995 and 1998, the percentage of all ankle injuries among snowboarders was 15.3% to 16%, of which 15% was a LPF,15 16 comprising 2.3% to 6% of all injuries.
LPF are often misdiagnosed because its symptoms resemble the symptoms of an ankle sprain. Thirty-three to 41% of these fractures are missed on initial presentation.9 17 18 Polzer et al1 developed an algorithm for diagnosing and treating acute ankle injuries. The algorithm was designed to simplify clinical decision-making and was implemented in the emergency department. Their recommendations regarding diagnosis included the Ottowa Ankle en Foot rules for reducing X-rays, physical examination (soft tissue damage), functional classification of injuries into stable or unstable, and use of MRI for confirming syndesmosis injuries.1 Specific for a LPF is tenderness inferior and anterior of the lateral malleolus, but the lateral malleolus is usually also painful during palpation. Usually, the Ottawa ankle rules are positive in patients with a LPF, but the fracture is best identified on radiographs using Mortise view (20° endorotation), since standard radiographs have a false-negative rate up to 40% of the cases.9 19 20 The golden standard for diagnosing a LPF is the CT scan, in which also type of fracture, displacement, comminution and involvement of the subtalar joint can be visualised.21 To avoid performing a CT scan on every patient with ankle sprain, we suggest the choice of a CT scan in clinically highly suspected patients after a snowboard injury. This can be defined as patients with positive Ottowa ankle rules and/or pain of the anterior talofibular ligament in combination with a history of a snowboard accident or jump, even when initial radiographs do not show a fracture.
LPF are divided in three subtypes, according to the classification of Hawkins.8 Type 1 is a simple fracture that extends from the talofibular articular surface down to the posterior talocalcaneal articular surface of the subtalar joint. Type 1 can be divided into type 1A; less than 2 mm displacement, and type 1B; more than 2 mm displacement. Type 2 is a comminuted fracture and involves the entire lateral process and both the fibular and the posterior calcaneal articular surfaces. Type 3 is a chip fracture and involves the anterior and inferior part of the lateral process.8 22 Perera et al reported in a review regarding the management and outcome of fractures of the talus that 42% of all LPF were simple and are associated with low energy trauma (type 1), 32% of the LPF were comminuted (type 2) and are associated with moderate to high-energy falls, and 24% were chip fractures (type 3) and are associated with high-energy falls and road traffic accidents. Furthermore, 24% of all patients with a LPF suffered additional foot and ankle pathology.23
The treatment of a LPF is dependent on the classification and the degree of comminution of the fracture. For fractures with displacement less than 2 mm (type 1A or 3), the treatment consists of a non-weight bearing short leg cast for a period of 6 weeks. More than 2 mm displaced, large and/or comminuted fractures should be referred for surgical treatment (open reduction and internal fixation).24 Perera et al23 suggests in a review that type I fractures are best treated with open reduction internal fixation, type II with excision and type III with casting. The review does not distinguish between type 1A and 1B.
The initial treatment is followed by physiotherapy. The incidence of morbidity in LPF in snowboarders appears to be high, although there is a lack of exact epidemiological data from the outcome in this patient group. 80% of patients with a fracture of the lateral process return to preinjury sport level.14 25 Poor prognosis is especially found when the fracture is initially missed or not properly treated.8 9 19 23 Complications that may occur include chronic pain, non-union, mal-union, instability of the ankle and post-traumatic arthritis of the subtalar joint.17 18
We can conclude that a fracture of the lateral process of the talus is rarely seen, but the increased popularity of snowboarding has led to a higher incidence of this fracture, also called the ‘snowboarder's ankle’. The fracture is easily missed due to subtle clinical and radiological findings. Early recognition may reduce the morbidity associated with this fracture. In case of uncertainty about the diagnosis, performing a CT scan is therefore recommended.
Learning points.
The increased popularity of snowboarding has led to a higher incidence of a fracture of the lateral process of the talus, also called the ‘snowboarder's ankle’.
As a result of subtle clinical and radiological findings, this fracture is easily overlooked.
Early recognition may reduce the morbidity associated with a LPF, and therefore performing a CT scan is recommended in patients with a history of a snowboard injury or jump in combination with one or more positive Ottawa ankle rules.
Acknowledgments
The authors would like to thank Mr BHJJ Theunissen, physician assistant trauma surgery, for the help on this article.
Footnotes
Contributors: IFK performed literature review, manuscript preparation and editing. LB performed literature review, manuscript preparation and editing. PRGB contributed to the manuscript and provided senior review. MP contributed to the manuscript and provided senior review. IFK and LB are joint first authors.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Polzer H, Kanz KG, Prall WC, et al. Diagnosis and treatment of acute ankle injuries: development of an evidence-based algorithm. Orthop Rev (Pavia) 2012;4:e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Consument, en, veiligheid. Blessures door snowboarden. 2010
- 3.Machold W, Kwasny O, Gassler P, et al. Risk of injury through snowboarding. J Trauma 2000;48:1109–14 [DOI] [PubMed] [Google Scholar]
- 4.Pino EC, Colville MR. Snowboard injuries. Am J Sports Med 1989;17:778–81 [DOI] [PubMed] [Google Scholar]
- 5.Bladin C, McCrory P, Pogorzelski A. Snowboarding injuries: current trends and future directions. Sports Med 2004;34:133–9 [DOI] [PubMed] [Google Scholar]
- 6.Davidson TM, Laliotis AT. Snowboarding injuries, a four-year study with comparison with alpine ski injuries. West J Med 1996;164:231–7 [PMC free article] [PubMed] [Google Scholar]
- 7.Fjeldborg O. Fracture of the lateral process of the talus. Supination-dorsal flexion fracture. Acta Orthop Scand 1968;39:407–12 [DOI] [PubMed] [Google Scholar]
- 8.Hawkins LG. Fractures of the lateral process of the talus. J Bone Joint Surg Am 1965;47:1170–5 [PubMed] [Google Scholar]
- 9.Mukherjee SK, Pringle RM, Baxter AD. Fracture of the lateral process of the talus. A report of thirteen cases. J Bone Joint Surg Br 1974;56:263–73 [PubMed] [Google Scholar]
- 10.Funk JR, Srinivasan SC, Crandall JR. Snowboarder's talus fractures experimentally produced by eversion and dorsiflexion. Am J Sports Med 2003;31:921–8 [DOI] [PubMed] [Google Scholar]
- 11.Boon AJ, Smith J, Zobitz ME, et al. Snowboarder's talus fracture. Mechanism of injury. Am J Sports Med 2001;29:333–8 [DOI] [PubMed] [Google Scholar]
- 12.Ng ES, O'Neill BJ, Cunningham LP, et al. Snowboard, wakeboard, dashboard? Isolated fracture of the lateral process of the talus in a high-speed road traffic accident. BMJ Case Rep 2013;2013:pii: bcr2013200357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yan AY, Mesfin A, Schon LC. Lateral process talus fracture in a kayaking injury. Orthopedics 2011;34:296–9 [DOI] [PubMed] [Google Scholar]
- 14.Valderrabano V, Perren T, Ryf C, et al. Snowboarder's talus fracture: treatment outcome of 20 cases after 3.5 years. Am J Sports Med 2005;33:871–80 [DOI] [PubMed] [Google Scholar]
- 15.Bladin C, McCrory P. Snowboarding injuries. An overview. Sports Med 1995;19:358–64 [DOI] [PubMed] [Google Scholar]
- 16.Kirkpatrick DP, Hunter RE, Janes PC, et al. The snowboarder's foot and ankle. Am J Sports Med 1998;26:271–7 [DOI] [PubMed] [Google Scholar]
- 17.Heckman JD, McLean MR. Fractures of the lateral process of the talus. Clin Orthop Relat Res 1985;199:108–13 [PubMed] [Google Scholar]
- 18.Tucker DJ, Feder JM, Boylan JP. Fractures of the lateral process of the talus: two case reports and a comprehensive literature review. Foot Ankle Int 1998; 19:641–6 [DOI] [PubMed] [Google Scholar]
- 19.Mills HJ, Horne G. Fractures of the lateral process of the talus. Aust N Z J Surg 1987;57:643–6 [DOI] [PubMed] [Google Scholar]
- 20.Noble J, Royle SG. Fracture of the lateral process of the talus: computed tomographic scan diagnosis. Br J Sports Med 1992;26:245–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fortin PT, Balazsy JE. Talus fractures: evaluation and treatment. J Am Acad Orthop Surg 2001;9:114–27 [DOI] [PubMed] [Google Scholar]
- 22.von Knoch F, Reckord U, von Knoch M, et al. Fracture of the lateral process of the talus in snowboarders. J Bone Joint Surg Br 2007;89:772–7 [DOI] [PubMed] [Google Scholar]
- 23.Perera A, Baker JF, Lui DF, et al. The management and outcome of lateral process fracture of the talus. Foot Ankle Surg 2010;16:15–20 [DOI] [PubMed] [Google Scholar]
- 24.Chan GM, Yoshida D. Fracture of the lateral process of the talus associated with snowboarding. Ann Emerg Med 2003;41:854–8 [DOI] [PubMed] [Google Scholar]
- 25.Shakked RJ, Tejwani NC. Surgical treatment of talus fractures. Orthop Clin North Am 2013;44:521–8 [DOI] [PubMed] [Google Scholar]