Abstract
Background: Many studies on assisted reproductive technology examine live birth rate per cycle. However, after a cycle fails, couples often want to know what their chances are of having a live birth if they continue treatment. From a patients’ perspective, the cumulative probability of live birth is more informative.
Materials and Methods: This study includes patients who underwent fresh, frozen and non-donor ICSI cycles at our IVF unit between 2006-2012. Patients were divided into two groups; Group 1 represented those who underwent only Day 5 transfers, Group 2 represented only Day 3 transfers. Patients who underwent both were excluded. Cycles were analyzed until the first live birth or the end of the 3rd cycle. Using Kaplan-Meier analysis, we estimated the cumulative live birth rates for each group and according to female age.
Results: The mean age for Group 1 was significantly lower than for Group 2. After 3 cycles, Group 1’s CLBR was 79% versus 66% in Group 2. When analyzing the live births by age and group, there was a significant difference in the CLBR after 3 cycles with the women less than 35 years having the highest CLBR and the women 40 years or older having the lowest CLBR.
Conclusion: In women less than 35 years, excellent CLBR can be achieved irrespective of the transfer day. For women 40 years and above, better results of CLBR are observed with Day 5 transfers. Our findings may impact the counseling of couples considering IVF treatment.
Keywords: IVF, ICSI, ART, cumulative live birth rate, female age, transfer day
Introduction
An important public health issue, it is estimated that between 9% and 14% of couples in the developed world have difficulty conceiving (Walschaerts M et al., 2012). When these couples present for counseling, they want to know the chance of a live birth should they decide to go through the rigors of assisted reproductive technology (ART) (Olivius et al., 2002).
Several studies on ART examine per cycle chance of pregnancy and delivery (Olivius et al., 2002). However, when one ART cycle fails, couples often want to know what their chance is of having a live birth if they continue with ART treatment. Thus from the patients’ perspective, the cumulative probability of live birth is more important (Malizia et al., 2013). Although there have been a few studies that have examined cumulative live birth rate (Engmann et al., 1999; Stern et al., 2010), there is none to our knowledge that has focused on the impact of transfer day by age group. One of these was a large study focusing on Massachusetts; because it is one of a few states in the Unites States that mandate full insurance coverage for ART (Stern et al., 2010). Unfortunately, in many parts of the world and in many states in the United States, there is no insurance mandate to cover any cycles. In France, where the first four cycles are free; 60% of patients returned for further cycles after one failed attempt compared to 30% of patients in the United Kingdom (Engmann et al., 1999). This reflects the financial but also the physical and emotional strain of ART (Malizia et al., 2013). Studies describe increased anxiety, lowered self-esteem, depression and marital problems after in-vitro fertilization (IVF) treatment especially if the couple remains childless (Olivius et al., 2002). Recently, an article examined the impact of several factors on live birth rates. Although this article examined transfer day of the embryo and female age, it did not analyze these factors together (Luke et al., 2012). Our unit moved to day 5 transfers (whenever day 5 transfer is possible) approximately 11 years ago based on data showing higher implantation and delivery rates and fewer multiple pregnancies with day 5 transfers (ASRM Practice Committee Opinion, 2013). If there is a limited number on day 3 though, our policy is to do the transfer on day 3.
We report the cumulative probability of live birth after 3 cycles based on female age and the day of embryo transfer. Our objective is to provide information that can be used for counseling when discussing the impact of age and transfer day on live birth rate.
Materials and Methods
This is a retrospective cohort study that included all patients who underwent fresh, non-donor intracytoplasmic sperm injection (ICSI) cycles and may have had subsequent fresh or frozen cycles at our unit between 2006 and 2012. Patients who used gestational carriers were not included in this study. The total number of patients was 3262 and the number of cycles was 4367. The primary outcome was the birth of a live born neonate. Live birth rate was defined as the number of deliveries that resulted in a live born neonate, expressed per 100 embryo transfers (Zegers-Hochschild et al., 2009). Up to 3 cycles were included until the end of IVF treatment or first live birth. We chose 3 cycles because previous research has found that 90% of ART pregnancies are achieved within the first three cycles (Luke et al., 2012) and pregnancy rates are decreased in patients who underwent more than four cycles (Fukuda et al., 2001). Cycles that ended in a miscarriage or stillborn were included in the study. Patients who on day 3 had 4 or more good quality embryos were allocated to a day 5 transfer. Otherwise, patients had day 3 transfers. Patients were divided into two groups; Group 1 included those with day 5 transfers (2184 women with 2758 cycles) and Group 2 included day 3 transfers (1078 women with 1263 cycles). Patients who underwent both day 3 and day 5 transfers in different cycles were excluded (346 cycles).
Fresh and Frozen Embryo Transfer Cycle
Patients received either an antagonist on day 5 of controlled ovarian stimulation (COS) or mid luteal agonist protocol for down regulation. They were stimulated with either recombinant follicle stimulating hormone (rFSH) or a mixed protocol. Down regulation protocol was dependent on the patient’s age, a poor response in a prior cycle and day 3 FSH. Antagonist protocol was used in patients who were greater than 35 years of age, history of poor response and FSH levels approaching the high range of normal (10 mIU/ml or higher). In addition, the majority of PCOS patients received rFSH 150-225 IU starting on day 2 or 3 of their cycle and gonadotropin releasing hormone (GnRH) antagonist starting on day 5 of COS. ICSI was performed on all mature oocytes three to four hours after retrieval.
Embryos were graded based on day 2 blastomere nuclear scoring and day 3 morphologic appearances of cleavage embryos. Blastocysts were graded according to criteria (Gardner et al., 2004). Ultrasound-guided embryo transfer (ET) was performed on either day 3 or day 5. Two top quality embryos/blastocysts were usually transferred and the remaining blastocysts with good quality, frozen. Luteal phase support was started on the second day after retrieval and if pregnancy occurred, the same treatment continued until twelve weeks gestation. Cryopreservation was performed 5 days after oocyte retrieval and included only blastocysts, early blastocysts and morulas that were deemed viable by morphologic criteria. Cycles using cryopreserved embryos were performed in natural cycles if the patient had ovulatory cycles and medicated cycles if the patient had anovulatory cycles.
Data Collection
The demographic and pregnancy outcome data were collected from patient’s charts, while embryology data was collected from our computerized database. Clinical pregnancy was defined as the presence of a gestational sac on transvaginal US scan at six weeks gestation. Miscarriage was defined as a clinical pregnancy that ended in pregnancy loss prior to twenty weeks gestation.
Statistical Analysis
IBM SPSS Statistics version 20 was used for all analysis. CLBR was calculated using Kaplan-Meier survival analysis. Additionally, the CLBR for each group was calculated according to female age (< 35, 35-39, > 39 years). The Mantel-Cox logrank test was used to compare differences in survival distributions between the groups. The independent t-test was used to assess difference in mean age by group. Differences in infertility etiologies were calculated using the chi-square analysis. An alpha of 0.05 was used for all analyses.
Results
During the study period, there were 3262 women who underwent 4367 cycles. The women underwent between 1-3 cycles until the first live birth. The etiology of infertility is presented in Table I. The mean age of group 1 (32. 8 +/- 4.5) was significantly lower than in Group 2 (35.4 +/- 5.1) P < 0.001). While diminished ovarian reserve (demonstrated by day 3 FSH) was more prevalent in the day 3 transfer group, ovulatory disorderslike polycystic ovarian syndrome and unexplained infertility were a more common etiology of infertility in the day 5 group.
Table I. Differences in etiology of infertility are compared by day of transfer.
| Etiology of infertility | |||
| Day 3 | Day 5 | p-value | |
| Male factor | 41.5% (447) | 41.1% (897) | NS |
| Ovulatory disorder | 17.7% (191) | 28.1% (613) | < 0.001 |
| Tubal | 19.0% (205) | 17.3% (378) | NS |
| Endometriosis | 14.7% (158) | 13.4% (293) | NS |
| Uterine | 10.3% (111) | 10.1% (221) | NS |
| Diminished reserves | 30.1% (324) | 12.1% (265) | < 0.001 |
| Unexplained | 5.1% (55) | 3.3% (72) | < 0.05 |
| Other | 9.1% (98) | 15.1% (330) | < 0.001 |
Overall Cumulative Live Birth Rate By Day of Transfer
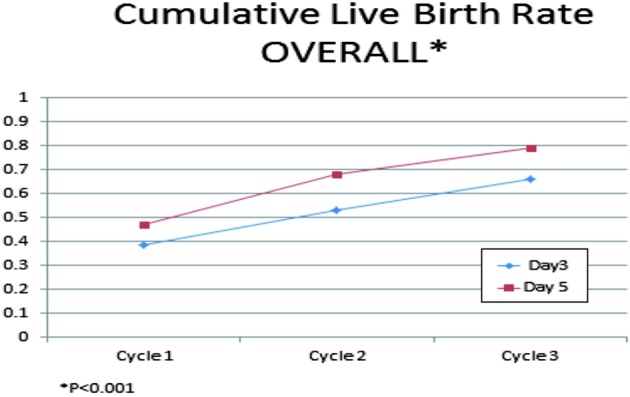
Figure 1 shows the live birth rate per cycle and CLBR after 3 cycles for Day 3 and Day 5 transfers. The overall CLBR for Day 3 transfers was 66.1% and 79.3% for Day 5 transfers. Loss to follow up rate i.e. percentage of women who neither completed three cycles nor had a live birth was 55% for the Day 3 transfer group and 37.5% for the Day 5 group.
Fig. 1. Overall CLBR for cycles 1, 2 and 3 by day of transfer (P < 0.001).
Cumulative Live Birth Rate By Day of Transfer and Age
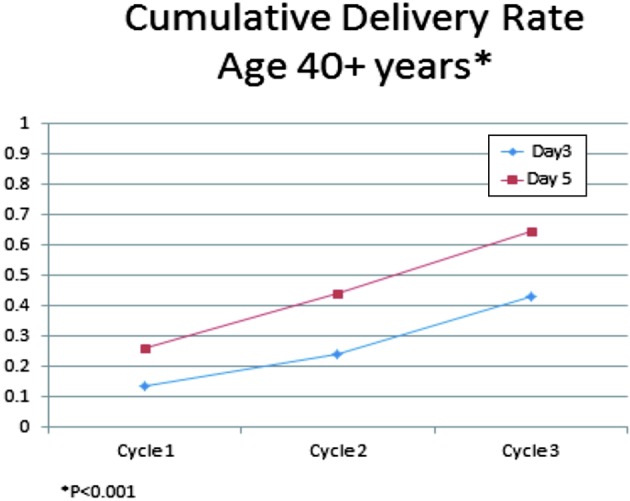
The CLBR at each cycle by day of transfer and stratified by age group is shown in figures 2, 3 and 4. When analyzing the live births by age and group, the live birth rate was noted to decline with advancing age regardless of transfer day (groups 1 and 2). There was a significant difference in the CLBR after 3 cycles; with women less than 35 years having the highest CLBR (78-82%) and women 40 years or older having the lowest CLBR (43%-65%). Stratified according to age, the CLBR also differed significantly between group 1 (Day 5 transfer) and group 2 (Day 3 transfer). Ranging from 82% vs 78% for women less than 35 years, 77% vs 66% in women between 35-39 years to 65% vs 43% in women above 40 years.
Fig. 2. CLBR for women < 35 years by day of transfer (P > 0.05.
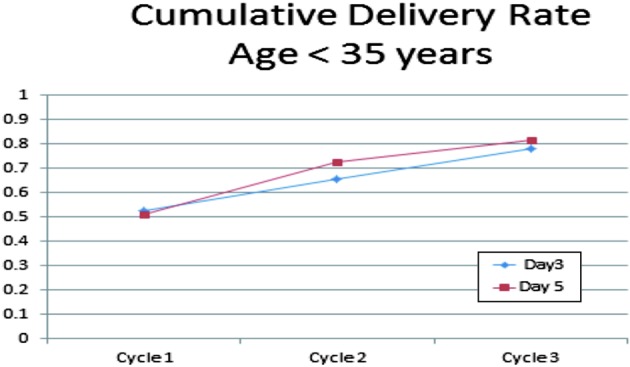
Fig. 3. CLBR for women age 35-39 years by day of transfer (P < 0.05).
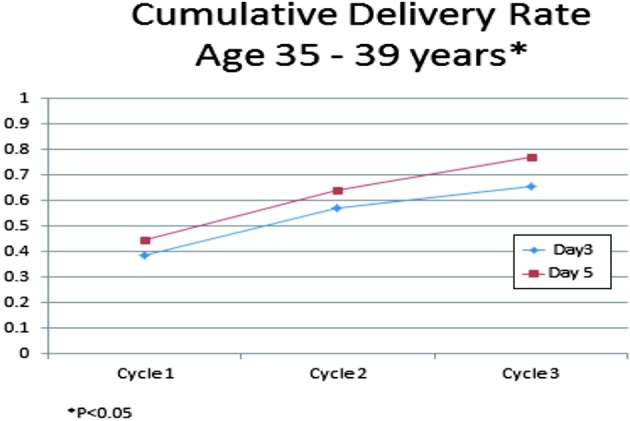
Fig. 4. CLBR for women 40 years or older by day of transfer (P < 0.001).
Discussion
The overall live birth rate after one cycle was 47.4% for Day 5 transfers and 38.5% for Day 3 transfers. After undergoing up to 3 cycles, the overall CLBR in our population of 3262 women showed marked improvement; 79.3% for Day 5 transfers and 66.1% for Day 3 transfers. The CLBR showed no statistically significant difference when stratifying for day of transfer in younger women (women < 35 years); 81.8% for Day 5 transfers and 78% for Day 3 transfers. For women between 35-39 years, the CLBR was significantly higher for Day 5 transfers (76.9%) compared to Day 3 transfers (65.8%). The CLBR was also significantly different for women 40 years and over; 64.6% for Day 5 transfers compared to 43.1% for Day 3 transfers.
Age is the single most important predictor of success with ART (Spandorfer et al., 2007). There is a natural decline in fertility with age as exemplified by our age stratified cumulative live-birth rates. This holds true for the general population as well (Malizia et al., 2009; Spandorfer et al., 2007); with reports of an infertility rate of 10% at 34 years of age and of over 85% at 44 years of age described (Spandorfer et al., 2007). According to a study done in the UK, assuming normal cohabitation and no coital difficulties; the cumulative pregnancy rates in the general population was 32% after 3 months and 54% after 6 months (Tan and Royston, 1992). Our CLBR after up to 3 cycles of between 66.1% and 79.3% depending on the day of transfer compares favorably to this. Amongst women 39 years of age or younger, our CLBR after up to three cycles of ICSI appeared to be similar to or higher than those reported in the general population (Gnoth C et al., 2003; Hull et al., 1992; Liberty G et al., 2013); thus suggesting that IVF/ICSI overcomes infertility in younger women (Malizia et al. 2009). Women 40 years of age or older however, should be counseled that IVF/ICSI might not completely overcome the age-dependent decrease in fertility (Malizia et al., 2009).
This study confirms earlier studies that showed declining per cycle and cumulative live birth rate with advancing age (Engmann et al., 1999; Malizia et al., 2009; Stern et al., 2004). It however shows that the age dependent decline in fertility is somewhat overcome if embryos are transferred on Day 5. It also brings to light a difference in cumulative live birth rates within the age groups depending on the day of transfer. To our knowledge, this is the first study to focus on the impact of day of transfer by age group on cumulative live birth rate.
It is well known that live birth rates using donor oocytes is high and unchanged as a function of age (Stern et al., 2004). A study reported a cumulative live birth rate for donor oocytes after 4 cycles of > 60% in women between 41-42 years (Stern et al., 2004). In this study, we chose to omit donor cycles. A study looked at the cumulative live birth rate with day 3 transfers after three cycles and reported a cumulative live birth rate between 45-53% (Milizia et al., 2009). Another study of Day 3 transfers reported a cumulative live birth rate of 51% after 3 cycles (Neubourg et al., 2010). A third reported a cumulative birth rate of 48.2% after 3 cycles (Engmann et al., 1999) and a Swedish study described a cumulative birth rate between 55.5% and 65.5% after 3 cycles (Olivius et al., 2002). Our results, with a cumulative live birth rate of 66% (Day 3 transfers after 3 cycles) compares favorably to these previous studies. These findings were irrespective of age. Our improved birth rates could simply be a result of improved technology over time (Pinborg et al., 2009). It is therefore difficult to compare our results with earlier studies (Stern et al., 2004).
Our cumulative live birth rates were higher in females < 35 years in agreement with prior publications (Malizia et al., 2009). Overall cumulative birth rates are also higher with day 5 transfers than day 3 transfers. Accordingly, it seems pertinent to consider not only female age but also the day of transfer as an important factor affecting outcomes. Analyses of cumulative cycles and the day of transfer have the advantage of educating physicians and patients alike about the potential outcome of treatment.
The study is subject to a few limitations. It is a retrospective study. The data was analyzed using the Kaplan-Meier analysis which has been criticized because it assumes that subjects that drop out of treatment would have responded similarly to those who continued treatment (Malizia et al., 2009). This study has a relatively high loss to follow up rate, which we believe highlights the financial strains of IVF treatment (Malizia et al, 2009). Michigan does not have an insurance mandate for infertility treatment and as such has a higher dropout rate than states with such coverage (Malizia et al, 2009). A major strength of this study however, is its generalizability; a large cohort of women without exclusion based on ovarian reserve testing, diagnosis or other prognostic factors. We also included fresh and frozen cycles but omitted donor cycles. The large sample size allowed us to stratify by age and day of transfer.
Conclusion
This study showed a significant increase in the probability of a live birth for women who underwent up to three ICSI-cycles. It also described excellent cumulative birth rates women less than 35 years irrespective of the transfer day. For women 40 years or older, the age dependent decline in fertility is somewhat overcome and better results of CLBR are to be expected if embryos are transferred on Day 5. Our findings may impact the counseling of couples considering IVF treatment.
References
- ASRM Practice Committee Opinion. Blastocyst culture and transfer in clinical-assisted reproduction: a committee opinion. Fertil Steril. 2013;99:667–672. doi: 10.1016/j.fertnstert.2013.01.087. [DOI] [PubMed] [Google Scholar]
- Engmann L, Maconochie N, Bekir J, et al. Cumulative probability of clinical pregnancy and live birth after a multiple cycle IVF package: a more realistic assessment of overall and age-specific success rates? Br J Obstet Gynaecol. 1999;106:165–170. doi: 10.1111/j.1471-0528.1999.tb08217.x. [DOI] [PubMed] [Google Scholar]
- Fukuda J, Kumagai J, Kodoma H, et al. Upper limit of the number of IVF-ET treatment cycles in different age groups, predicted by cumulative take-home baby rate. Acta Obstet Gynecol Scand. 2001;80:71–73. doi: 10.1034/j.1600-0412.2001.800114.x. [DOI] [PubMed] [Google Scholar]
- Gardner D, Surrey E, Minjarez D, et al. Single blastocyst transfer: a prospective randomized trial. Fertil Steril. 2004;81:551–555. doi: 10.1016/j.fertnstert.2003.07.023. [DOI] [PubMed] [Google Scholar]
- Gnoth C, Godehardt D, Godehardt E, et al. Time to pregnancy: results of the German prospective study and impact on the management of infertility. Hum Reprod. 2003;18:1959–1966. doi: 10.1093/humrep/deg366. [DOI] [PubMed] [Google Scholar]
- Hull M, Eddowes H, Fahy U. Expectations of assisted conception for infertility. Br Med J. 1992;204:1465–1469. doi: 10.1136/bmj.304.6840.1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberty G, Margalioth E, Meltcer S. Infertility Definitions – Patients’ Perspectives. Int J Gynecol Obst Res. 2013;1:79–83. [Google Scholar]
- Luke B, Brown M, Wantman E, et al. Cumulative Birth Rates with Linked Assisted Reproductive Technology Cycles. N Engl J Med. 2012;366:2483–2491. doi: 10.1056/NEJMoa1110238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malizia B, Hacker M, Penzias A. Cumulative live-birth rates after In Vitro Fertilization. N Engl J Med. 2009;360:236–243. doi: 10.1056/NEJMoa0803072. [DOI] [PubMed] [Google Scholar]
- Malizia B, Dodge L, Penzias A, et al. The cumulative probability of live born multiples after in vitro fertilization: a cohort study of more than 10,000 women. Fertil Steril. 2013;99:393–399. doi: 10.1016/j.fertnstert.2012.10.018. [DOI] [PubMed] [Google Scholar]
- Olivius K, Friden B, Lundin K, et al. Cumulative probability of live birth after three in vitro fertilization/intracytoplasmic sperm injection cycles. Fertil Steril. 2002;77:505–510. doi: 10.1016/s0015-0282(01)03217-4. [DOI] [PubMed] [Google Scholar]
- Neubourg D, Daels C, Elseviers M, et al. Cumulative live-birth delivery after IVF/ICSI since the progressive introduction of single embryo transfer. Reprod Biomed Online. 2010;20:836–842. doi: 10.1016/j.rbmo.2010.02.013. [DOI] [PubMed] [Google Scholar]
- Pinborg A, Hougaard C, Andersen N, et al. Prospective longitudinal cohort study on cumulative 5-year delivery and adoption rates among 1338 couples initiating infertility treatment. Hum Reprod. 2009;24:991–999. doi: 10.1093/humrep/den463. [DOI] [PubMed] [Google Scholar]
- Spandorfer S, Bendikson K, Dragisic K, et al. Outcome of in vitro fertilization in women 45 years and older who use autologous oocytes. Fertil Steril. 2007;87:74–76. doi: 10.1016/j.fertnstert.2006.05.081. [DOI] [PubMed] [Google Scholar]
- Stern J, Brown M, Luke B, et al. Calculating cumulative live-birth rates from linked cycles of assisted reproductive technology (ART): data from the Massachusetts SART CORS. Fertil Steril. 2010;94:1334–1340. doi: 10.1016/j.fertnstert.2009.05.052. [DOI] [PubMed] [Google Scholar]
- Tan S, Royston P. Cumulative conception and livebirth rates after In Vitro Fertilization. Lancet. 1992;339:1390–1394. doi: 10.1016/0140-6736(92)91205-m. [DOI] [PubMed] [Google Scholar]
- Walschaerts M, Bujan L, Isus F, et al. Cumulative parenthood rates in 1735 couples: impact of male factor infertility. Hum Reprod. 2012;27:1184–1190. doi: 10.1093/humrep/der466. [DOI] [PubMed] [Google Scholar]
- Zegers-Hochschild F, Adamson G, De Mouzon J, et al. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART Terminology. Fertil Steril. 2009;92:1520–1524. doi: 10.1016/j.fertnstert.2009.09.009. [DOI] [PubMed] [Google Scholar]


